Abstract
Objectives: The aim of this study was to determine the epidemiological characteristics of bicycling-related maxillofacial fractures in a defined population and to identify factors contributing to these injuries. Methods: An 8-year cohort study was carried out, including all patients presenting with bicycling-related maxillofacial fractures at a tertiary care center from 2017 through 2024. Data recorded for each patient included age, gender, date and cause of injury, contributing factors, type of facial fractures, other injuries, hospital stay, and helmet use. Statistical analysis was performed. Continuous variables were assessed for normality (Shapiro–Wilk test) and compared using the Mann–Whitney test. Categorical variables were analyzed with chi-square tests. A p-value ≤ 0.05 was considered statistically significant. Results: Out of 899 cycling accident patients seeking medical treatment, 122 (13%) sustained facial fractures, accounting for 4% of all facial fracture cases in our department during the study period. In our cohort, the male–female ratio was 2.6:1, and the mean age was 29.5 years (SD 12.8, range 13–77). Collision with another object/vehicle was the most common cause (64%), followed by isolated falls (36%). A total of 135 facial fractures were recorded (some patients had multiple fractures). Mandibular fractures were most frequent (49% of patients), followed by zygomatic (32%), orbital (13%), nasal (7%), maxillary (2%) and frontal (2%) fractures. Among mandibular injuries, condylar fractures were the most common subtype (63%). Dental injuries were found in 27% of patients. The most common dental trauma was tooth fracture (43% of those with dental injuries), followed by tooth luxation (32%) and tooth avulsion (25%). In 80% of cases involving dental injuries, the upper anterior teeth were involved. Concomitant injuries were present in 20% of patients, most often orthopedic limb injuries. Only 27% of patients reported always wearing a helmet, whereas 43% reported never having worn one. Conclusions: Bicycling-related facial injuries are a noteworthy subset of facial trauma. Missed or delayed diagnosis can lead to lasting deformities and functional issues. Preventive strategies—especially promoting helmet use and improving helmet design—along with broader safety measures are important to reduce the incidence and severity of these injuries.
1. Introduction
Traffic injuries remain a major public health problem and a leading cause of injury and disability around the world. The social, economic and health losses resulting from traffic injuries are not inevitable. There is substantial evidence confirming that traffic accidents can be prevented. A number of factors have been identified as increasing the risk of traffic-related injuries, including poorly designed or insufficiently maintained road infrastructure, excess speed, drinking and driving or vehicles that are not well maintained or that lack safety features. Regulatory and other actions that address those contributing factors have led to dramatic decreases in traffic crashes in many countries. The provision of emergency trauma care services has also been shown to be very important in mitigating the negative impacts of traffic accidents [1,2].
Maxillofacial trauma often requires multidisciplinary care and can result from a variety of causes, including traffic accidents, falls, assaults, and sports. The epidemiology of facial fractures varies by geographic region and time period. Different trauma mechanisms are associated with different injury patterns (in terms of patient age, gender, fracture site, and injury severity); understanding these patterns can help guide more effective prevention and treatment strategies [3,4,5].
Bicycling is a popular form of transportation and exercise across all ages; however, it carries a risk of injury. Traffic accidents—including bicycle crashes—are among the most common causes of maxillofacial fractures, with bicycle accidents reportedly responsible for roughly 2–18% of facial fractures in published cases [6,7,8]. Seville, Spain, provides a pertinent context. The city has witnessed rapid expansion of its bicycle infrastructure. Before 2005, bicycle use in Seville was minimal and primarily for recreational purposes. In 2006, an ambitious plan resulted in the addition of more than 80 km of bike lanes in one year, with the introduction of a public bike-share program. Bicycle modal share increased from 0.5% in 2006 to 7% in 2013. The Copenhagenize Index ranks Seville among the top ten bicycle-friendly cities worldwide.
Vulnerable bicycle infrastructure users, who lack the protective shell of a car and who have been overlooked in many traffic safety strategies, are particularly at risk and in need of protection. The surge in cycling activity has been accompanied by an increase in bicycle-related accidents [9,10,11,12,13]. The objective of this study was to characterize the epidemiology of bicycling-related maxillofacial fractures in Seville since 2017 to identify key risk factors contributing to these injuries and to propose countermeasures to improve cyclist safety.
2. Materials and Methods
2.1. Standard Protocol Approvals and Patient Consent
This study was approved by the Institutional Research and Clinical Ethics Committee (Internal Code: 0975-N-21) and was conducted in accordance with the principles of the Declaration of Helsinki on medical protocols and ethics. All the participants were informed of the nature of the study and their written consent was obtained.
2.2. Study Design and Subjects
This study is a single-center cohort study of acute maxillofacial fractures sustained in bicycling-related accidents, treated at the Department of Oral and Maxillofacial Surgery between January 2017 and October 2024. Bicycling-related injury was defined as any trauma occurring while the patient was riding a bicycle. The information was collected exclusively from the analysis of police and medical reports. A number of factors were identified as increasing the risk of bicycling-related injuries, including insufficiently maintained bicycle infrastructure, excess speed, drinking and driving, cycling with headphones, non-use of helmets or bicycles that are not well maintained or that lack safety features. The presence or absence of such factors was recorded by emergency services during their response to an incident or inferred from their location of the accident. The study cases were patients of both sexes, aged between 10 and 80 years, who were referred to our center after traffic accidents. Data were collected by the same observer (C.A.-D.) and the personal information of the patients was anonymized to protect their privacy; this process included the removal of all personal data such as names, date of birth, address, and other identifiable information from images. The inclusion criteria were: a history of maxillofacial trauma after bicycling-related accident, and imaging studies consistent with signs of facial bone fracture. We reviewed hospital records, including clinical notes and imaging, for all patients meeting these criteria. Data collected included age, gender, date of injury, cause/mechanism of the crash (collision or fall, and specific circumstances), presumed contributing factors, type and location of facial fractures, injuries to other body regions, length of hospitalization, and helmet use pattern. Individuals with one or more of the following conditions were excluded: incomplete patient records and minor superficial injuries (abrasions or contusions) without any facial fracture.
2.3. Statistical Analysis
Data analysis was performed using IBM SPSS Statistics 20 (IBM Corp., Armonk, NY, USA). Continuous variables were tested for normal distribution with the Shapiro–Wilk test. As most continuous data were non-normal, comparisons between groups were made using the Mann–Whitney U test. Categorical variables were analyzed with chi-square tests. A p-value ≤ 0.05 was considered statistically significant.
3. Results
During the 8-year study period, 899 patients were evaluated for cycling-related accidents. Bicycle-related facial fractures were diagnosed in 122 of these cases, representing 13% of cycling accident patients and approximately 4% of all patients with facial fractures seen at our institution in this timeframe. Our study cohort included 88 male and 34 female patients (male–female ratio 2.6:1), and the mean age was 29.5 years (SD 12.8, range 13–77 years). The number of male and female patients admitted each year with bicycle-related facial fractures is summarized in Table 1.

Table 1.
The number of admitted patients with bicycle-related maxillofacial fractures per year.
By age group, young adults were most frequently affected. Patients aged 20–29 years formed the largest group (43 patients, 35%), followed by those aged 10–19 years old (31 patients, 25%). The age distribution by decade and gender is shown in Table 2.

Table 2.
Gender and age-group distribution of patients.
The incidence of bicycle-related maxillofacial injuries by month is illustrated in Figure 1. The number of cases was highest from April through September (spring and summer months). There was no significant difference in incidence across different days of the week.
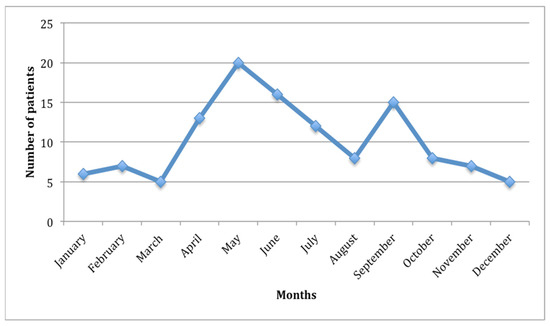
Figure 1.
The number of admitted patients with bicycle-related maxillofacial fractures by month of occurrence over an 8-year period.
Contributing factors in traffic accidents were identifiable in 83 patients (68%). Some patients were noted as having multiple contributing factors. The following key contributing factors observed were: not wearing a helmet: 33 patients (27%); involvement of a motor vehicle: 25 patients (20%); cycling with headphones (music/earpieces): 23 patients (19%); riding during early evening (dusk): 21 patients (17%); unsafe road conditions (e.g., rain, road works): 15 patients (12%); mechanical failure of the bicycle: 14 patients (11%); alcohol use by the cyclist: 11 patients (9%); and competitive or high-speed cycling (racing): 10 patients (8%). The contributing factors observed in our series are shown in Figure 2a.
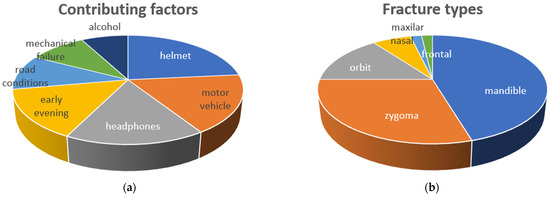
Figure 2.
(a) Contributing factors for injury. Understanding these factors is crucial for promoting safe cycling practices and reducing the likelihood of accidents and injuries. (b) Distribution of facial fracture types in our series. Mandibular fractures were the most common type.
Most patients (93%) sustained a single facial fracture, with the remaining patients (7%) suffering multiple facial fractures. The distribution of fracture types is as follows: mandible in 60 patients (49%), zygomatic complex in 39 (32%), orbital in 16 (13%), nasal in 9 (7%), maxillary in 2 (2%), and frontal in 2 (2%). The distribution of fracture types in our series is shown in Figure 2b. Mandibular fractures were the most common type of injury, and among them, the condylar region was by far the most frequently fractured site (seen in 63% of patients with mandibular fractures).
The majority of patients did not require prolonged hospitalization. For patients who suffered no other injuries than the facial fracture, the average hospital stay was 4 days (SD 1.2 days). Self-reported helmet use among the cohort was low: 43% of patients reported never having worn a bicycle helmet, and 32% reported inconsistent or occasional helmet use. Only 26% of patients stated that they always wore a helmet while cycling.
Associated injuries (outside of the facial region) were documented in 24 patients (20%). Among these concomitant injuries, orthopedic trauma to the limbs was most common (42% of those with associated injuries). Dental injuries were also frequent, found in 33 patients (27% of all cases). The most common dental trauma was tooth fracture (43% of those with dental injuries), followed by tooth luxation (32%) and tooth avulsion (25%). In 80% of cases involving dental injuries, the upper anterior teeth were involved. Traumatic brain injuries (e.g., intracranial injuries or concussions) were noted in seven patients (6%). These head injuries were associated with a significantly longer hospital stay (mean 30 ± 7 days). Importantly, none of the patients who sustained a concomitant cranial injury were wearing a helmet at the time of their bicycle crash.
4. Discussion
Overall, the incidence of automobile-related trauma has declined in recent years due to improved safety measures such as seatbelts and airbags. However, injuries sustained while using other modes of transport—such as bicycles—have increased in frequency as these activities grow in popularity. This trend is evident in Seville following the expansion of its cycling network in 2006. Seville is a flat city in southern Spain with a mild climate for the majority of the year, making it well-suited to cycling. The metropolitan area comprises roughly 1.5 million inhabitants. The dramatic increase in cycling infrastructure and usage (from virtually zero daily cyclists in 2005 to a 7% modal share by 2013) has been accompanied by a rise in bicycle accidents. Several factors have likely contributed to the spike in accidents. Firstly, the design and layout of some new bike lanes have led to conflict points with motor vehicle traffic and pedestrians. In certain areas, bicycle lanes intersect with roads and areas where drivers have limited visibility, resulting in collisions. Secondly, there was a lack of public education on safe cycling practices when the infrastructure was introduced. Many new cyclists were unfamiliar with how to safely share the road or bike paths with cars and pedestrians, leading to improper use of the lanes.
Bicycling-related injuries have become an important etiological factor in maxillofacial trauma. Notably, differences in maxillofacial injury rates across regions can be explained by differences in exposure to cycling, local habits, and demographic characteristics of cyclists [13,14,15,16,17]. It is also recognized that injuries to cyclists are under-reported in official road traffic data, because single-bicycle crashes (falls without collision) are often not reported to the police. Hospital-based data therefore provide crucial insight into the true burden of cycling injuries [8,11].
Boffano et al. conducted a comprehensive study on bicycle-related maxillofacial injuries in two European centers (Turin, Italy, and Amsterdam, the Netherlands) between 2001 and 2010 [18]. Their findings on the proportion of facial fractures caused by cycling accidents and the associated injury patterns are comparable to those in our series. In our study, bicycle-related fractures consistently represented a measurable subset of all facial fractures each year from 2017 to 2024. However, it is possible that we may have underestimated the total number of cycling-related facial injuries in the community. Some cases might have been classified differently (for example, attributed to a simple fall rather than a “bicycle accident” in records) or not brought to the attention of medical specialists at all (especially if the fracture was nondisplaced and symptoms were mild). Cyclists who crash without serious symptoms may not seek treatment, and thus their injuries would not be captured in our dataset. Of note, our series includes the COVID pandemic period. During the first year of the pandemic, there was a 35.2% reduction in maxillofacial fractures was noted, including those from bicycle-related accidents, compared to the year before the pandemic. A significant decrease was detected, compared to the pre-pandemic year. A significant decrease was detected during the period of total home confinement (15 March to 21 June 2020) [19].
The demographic profile of our patients aligns with trends reported in other studies [8,9,10,11]. Young male adults constituted the majority of bicyclist trauma patients. Individuals in their teens through their thirties are more likely to cycle frequently (often as a mode of transport in our city) and may exhibit higher risk-taking behavior, which increases their injury risk. We also observed that the most severe facial fractures tended to occur in scenarios involving motor vehicles. Of note, maxillofacial injuries are roughly three times more likely in crashes that involve a motor vehicle compared to bicycle-only incidents [1,2,18]. This fact may partially explain why the risk of facial fracture appears to decrease as impact speed decreases (in purely bicycle falls), although this correlation is complex and confounded by factors such as the cyclist’s experience and caution levels. It is also worth noting that categorizing an injury as “motor vehicle involved” does not in itself explain the mechanism. Some bicycle-motor vehicle collisions occur because of cyclist error (e.g., losing control or mechanical failure leading the cyclist into traffic), while others are due to driver error (e.g., a car turning into a cyclist’s path). In the study by Juhra et al., the authors combined police reports with hospital records to gain a more comprehensive picture of bicycle accidents, highlighting the fact that many minor bicycle incidents do not end up being included in hospital data and vice versa [14]. Such combined data provide a more accurate statistical pool for understanding cycling accidents.
Consistent with prior reports, the mandible was found to be the most commonly fractured facial bone in bicycle accidents [20,21,22,23]. In our series, nearly half of the patients suffered a mandibular fracture, and among them, the condylar process was the most frequent fracture site. Falls from a bicycle often result in the rider landing on the chin—the most prominent and exposed part of the face—which transmits force to the mandibular condyles, leading to fracture of the condylar neck. The mandible’s biomechanical properties explain this fact: the mandibular symphysis and body are relatively thick and robust; in comparison, the condylar neck is a thinner, more fragile area that serves as a stress point. Clinically, a patient with a condylar fracture may present with preauricular swelling and pain, limited jaw opening, and malocclusion. In our management protocol for bicycle trauma, careful examination of mandibular movement (jaw opening, lateral excursions, and bite alignment) is essential to detect condylar injuries that might otherwise be overlooked upon initial assessment.
Facial fractures in cyclists can be accompanied by other traumatic injuries, thus highlighting the importance of a multidisciplinary evaluation. In our study, 20% of patients suffered injuries beyond the facial region. Orthopedic injuries (particularly to the arms and legs) were the most common concomitant trauma. This finding emphasizes that bicycle trauma patients benefit from thorough trauma protocols and imaging (such as whole-body computed tomography when indicated) to identify all injuries, rather than focusing only on obvious facial wounds.
There are multiple opportunities to reduce the risk of severe injuries for cyclists. One of the most effective measures is the use of safety helmets. The results of previous studies have demonstrated that bicycle helmets can prevent between 65 and 88% of serious head injuries [8,9]. Helmets provide a substantial protective effect by absorbing impact energy and shielding the skull and upper face. Indeed, they are particularly effective in crashes that do not involve high-speed motor vehicles—for example, when a cyclist falls or in low-speed collisions—as they can prevent direct head impact. In our series, we found that none of the patients who sustained serious head injuries were wearing helmets, underscoring the protective value of helmet use.
Despite the known benefits of helmets, their usage varies widely. Richard et al. reported that in France the rate of helmet wearing among cyclists increased significantly from 2000 to 2010 (roughly 7% to 22%), yet this rise did not correspond to a measurable decrease in overall bicycle accidents [24]. This finding suggests that while a greater number of people wore helmets during this period, other factors may have influenced the total number of accidents (such as increased cycling exposure or risk compensation). In California, Castle et al. found almost no change in helmet usage or head injury rates among cyclists in Los Angeles County after the introduction of a mandatory helmet law for minors [25]. In contrast, in New South Wales, Australia, a mandatory helmet law was associated with a significant and sustained reduction in head injuries among cyclists; Olivier et al. documented a steady decline in head injury rates following the law’s implementation [26]. These differing outcomes indicate that legislation and public health campaigns around helmet use can have varying effectiveness depending on enforcement and the public’s response.
In Spain, current law requires cyclists under 16 years old to wear a helmet when riding in urban areas; in contrast, helmet use for adults in cities is only recommended, not mandatory. Our findings strongly support promoting helmet use for riders of all ages, not just children. It is important to acknowledge, however, that standard bicycle helmets (which comply with the European EN-1078 standard) do not cover the entire face—they primarily protect the cranium and upper part of the face, leaving the lower face (especially the jaw and chin) exposed [27,28,29,30,31]. It is clear that even with a helmet, a cyclist can sustain facial injuries, particularly in high-impact crashes involving vehicles. Some critics of helmet promotion have pointed out potential limitations and biases in helmet effectiveness studies (for example, suggesting that riskier riders are less likely to wear helmets, or that helmets might not help in certain high-severity impacts). We do not suggest that simply not wearing a helmet causes accidents—the decision to wear a helmet likely does not affect whether a crash occurs—but helmet use does mitigate the severity of injuries when accidents happen. Improving helmet design to offer more facial coverage and better impact absorption could further reduce injury severity. For instance, innovative helmet technologies, such as inflatable “airbag” helmets, have been developed to provide enhanced protection for cyclists’ heads and are an area of active interest for injury prevention [32,33].
Ample evidence supports the injury-prevention benefits of helmets. The results of other studies have demonstrated that wearing a helmet significantly reduces the risk of head and brain injuries, and conversely that not wearing a helmet is strongly associated with sustaining severe head trauma in a crash [34]. Our study’s findings are consistent with this evidence: patients who did not wear helmets had a markedly higher risk of head injury and were more likely to require hospital admission for head trauma, indicating greater injury severity. This finding aligns with other reports in the literature that link helmet non-use to more serious injury outcomes [35,36]. Besides helmets, other technological interventions may improve cyclist safety in the near future. For example, Anagnostopoulos et al. have developed a system in which traffic signals can detect an approaching cyclist by communicating with the cyclist’s smartphone, allowing traffic lights to adjust and give cyclists priority or additional crossing time [37]. Similarly, various vehicle-to-vehicle and vehicle-to-cyclist communication systems (using ad hoc wireless networks) are being tested to alert drivers and cyclists to each other’s presence. Such innovations could help prevent collisions by providing early warnings and adapting traffic control to protect cyclists.
It should be noted that while bicycle-related maxillofacial injuries have been studied extensively, the emergence of electric scooters (e-scooters) as a popular form of urban transport has introduced new patterns of craniofacial injuries. At present, research on e-scooter-related injuries is limited, despite the increasing number of users in cities across Europe and other regions. This gap in knowledge will be addressed in future investigations, in which we plan to compare the characteristics of facial injuries from e-scooter accidents with those from bicycle accidents. Understanding any differences in injury patterns between these two transport modalities will be crucial for developing effective safety measures and public health interventions tailored to each situation [38].
Our study has several limitations that must be addressed. Firstly, the study was conducted at a single tertiary referral hospital in Andalusia. As a major regional center, our hospital tends to receive more severe craniofacial trauma cases, which may not be fully representative of all bicycle injuries in the community. Minor facial injuries (for example, uncomplicated nasal fractures or tooth injuries) might be managed at smaller clinics or possibly be left untreated, leading to underestimation of less severe cases. Consequently, the true incidence of bicycle-related facial injuries is likely higher than that reported herein, as many cyclists with milder injuries would likely not present to our department. Secondly, some fractures—particularly condylar fractures of the mandible—can be easily missed if they are not displaced and the patient’s symptoms are mild. It is common for a subset of patients with condylar fractures to be managed conservatively (with rest, soft diet, and analgesics) without referral to specialist care. We have encountered patients who presented later with chronic temporomandibular joint dysfunction, only to discover a past history of an untreated condylar fracture. Thus, our series may under-represent certain injury types due to these diagnostic challenges. Lastly, the sample size (122 patients over a period of 8 years) is relatively small for extensive subgroup analysis, reflecting the fact that serious maxillofacial injuries suffered during cycling accidents are still infrequent at the population level.
5. Conclusions
Maxillofacial trauma is a common injury caused by a variety of factors. In this study, we focused on bicycle-related facial injuries in an urban setting with a high adoption of cycling. In our series, mandibular fractures were the most frequent type of injury, with condylar fractures being the predominant subtype, often resulting from direct impacts to the chin during falls. Although bicycling-related maxillofacial fractures are relatively rare, awareness of their frequency, causes, contributing factors, and anatomical distribution is important for emergency and trauma teams who are the first to assess these patients. Early recognition and timely management are crucial, as missed diagnoses or delayed treatment can lead to permanent facial deformities and functional impairments.
We identified several key contributing factors in these injuries, notably the lack of helmet use, involvement of motor vehicles, distraction (such as headphone use), and riding during the early evening hours. These insights can inform targeted public health strategies and injury prevention programs. Efforts to make cycling safer should include promoting the use of protective helmets—since helmets can significantly reduce the risk of head and facial injuries—while also recognizing that helmets alone cannot prevent all injuries. Improving infrastructure design, enforcing traffic laws, educating both cyclists and drivers, and advancing helmet technology are all necessary components of a comprehensive approach to reducing the occurrence and severity of bicycling-related facial trauma. By combining these strategies, urban areas can work towards safer, sustainable transport systems that protect cyclists from serious injuries.
Author Contributions
Conceptualization, L.M.G.-P. and J.W.; methodology, L.M.G.-P. and J.W.; software, L.M.G.-P., J.W. and C.A.-D.; validation, L.M.G.-P. and J.W.; formal analysis, L.M.G.-P., J.W. and C.A.-D.; investigation, L.M.G.-P. and J.W.; resources, L.M.G.-P., J.W. and C.A.-D.; data curation, L.M.G.-P., J.W. and C.A.-D.; writing—original draft preparation, L.M.G.-P. and J.W.; writing—review and editing, L.M.G.-P., J.W. and C.A.-D.; visualization, L.M.G.-P. and J.W.; supervision, L.M.G.-P., J.W. and C.A.-D.; project administration, L.M.G.-P. and J.W.; funding acquisition, L.M.G.-P. and J.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Virgen del Rocio University Hospital, Seville, Spain (IRB 2014PI/083) on 14 December 2021.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon reasonable request by contacting the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bachani, A.M.; Ahsan, H.; Jagnoor, J.; Kobusingye, O.; Tran, N.; Peden, M. Time for action: The critical role of research and data in achieving the targets of the second UN Decade of Action for Road Safety. BMJ Glob. Health 2025, 10, e017488. [Google Scholar] [CrossRef]
- Peden, M.; Scurfield, R.; Sleet, D.; Mohan, D.; Hyder, A.A.; Jarawan, E.; Mathers, C. World Report on Road Traffic Injury Prevention; World Health Organization: Geneva, Switzerland, 2004; pp. 88–94. [Google Scholar]
- Bicsak, A.; Topcuoglu, F.; Hassfeld, S.; Lefering, R.; Bonitz, L.; Stahl, J.P. Concomitant body-wide trauma patterns in patients with head and neck injuries: A comparison based on the trauma register DGU® by the German trauma society and the Dortmund maxillofacial trauma registry. Eur. J. Med. Res. 2025, 30, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Kostakis, G.; Stathopoulos, P.; Dais, P.; Gkinis, G.; Jgoumenakis, D.; Mezitis, M.; Rallis, G. An epidemiologic analysis of 1142 maxillofacial fractures and concomitant injuries. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Van Hout, W.M.M.T.; Van Cann, E.M.; Abbink, J.H.; Koole, R. An epidemiological study of maxillofacial fractures requiring surgical treatment at a tertiary trauma centre between 2005 and 2010. Br. J. Oral Maxillofac. Surg. 2013, 51, 416–420. [Google Scholar] [CrossRef]
- Bourdet, N.; Deck, C.; Serre, T.; Perrin, C.; Llari, M.; Willinger, R. In-depth real-world bicycle accident reconstructions. Int. J. Crashworthiness 2013, 19, 222–232. [Google Scholar] [CrossRef]
- Lee, K.H.; Chou, H.J. Facial fractures in road cyclists. Aust. Dent. J. 2008, 53, 246–249. [Google Scholar] [CrossRef]
- Palmer, A.J.; Si, L.; Gordon, J.M.; Saul, T.; Hitchens, P.L. Accident rates amongst regular bicycle riders in Tasmania. Accid. Anal. Prev. 2014, 72, 376–381. [Google Scholar] [CrossRef]
- Goerke, D.; Zolfaghari, E.; Marek, A.P.; Endorf, F.W.; Nygaard, R.M. Incidence and profile of severe cycling injuries after bikeway infrastructure changes. J. Community Health 2020, 45, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Farkkila, E.M.; Oksanen, E.; Kormi, E.; Suojanen, J. What is the relationship between maxillofacial injury location and associated injuries? J. Oral Maxillofac. Surg. 2024, 82, 800–805. [Google Scholar] [CrossRef]
- Lawson, A.R.; Pakrashi, V.; Ghosh, B.; Szeto, W.Y. Perception of safety of cyclists in Dublin City. Accid. Anal. Prev. 2013, 50, 499–511. [Google Scholar] [CrossRef]
- Vandenbulcke, G.; Thomas, I.; De Geus, B.; Degraeuwe, B.; Torfs, R.; Meeusen, R.; Int Panis, L. Mapping bicycle use and the risk of accidents for commuters who cycle to work in Belgium. Transp. Policy 2009, 16, 77–87. [Google Scholar] [CrossRef]
- Weber, T.; Scaramuzza, G.; Schmitt, K.U. Evaluation of e-bike accidents in Switzerland. Accid. Anal. Prev. 2014, 73, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Juhra, C.; Wieskotter, B.; Chu, K.; Trost, L.; Weiss, U.; Messerschmidt, M.; Malczyk, A.; Heckwolf, M.; Raschke, M. Bicycle accidents: Do we only see the tip of the iceberg? A prospective multi-centre study in a large German city combining medical and police data. Injury 2012, 43, 2026–2034. [Google Scholar] [CrossRef]
- Vandenbulcke, G.; Thomas, I.; Int Panis, L. Predicting cycling accident risk in Brussels: A spatial case-control approach. Accid. Anal. Prev. 2014, 62, 341–357. [Google Scholar] [CrossRef]
- Yamamoto, K.; Matsusue, Y.; Horita, S.; Murakami, K.; Sugiura, T.; Kirita, T. Maxillofacial fractures sustained in bicycle accidents. J. Oral Maxillofac. Surg. 2011, 69, 155–160. [Google Scholar] [CrossRef]
- Wusiman, P.; Maimaitituerxun, B.; Guli, X.; Saimaiti, A.; Moming, A. Epidemiology and pattern of oral and of maxillofacial trauma. J. Craniofac. Surg. 2020, 31, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Gallesio, C.; Karagozoglu, K.H.; Forouzanfar, T. Bicycle-related maxillofacial injuries: A double-center study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Infante-Cossio, P.; Fernandez-Mayoralas, M.; Gonzalez-Perez, L.M.; Martinez-de-Fuentes, R.; Rollon-Mayordomo, A.; Torres-Carranza, E. Impact of the coronavirus pandemic on maxillofacial trauma: A retrospective study in southern Spain. Med. Oral Patol. Oral Cir. Bucal. 2022, 27, 223–229. [Google Scholar] [CrossRef]
- Thomas, B.; Derobertis, M. The safety of urban cycle tracks: A review of the literature. Accid. Anal. Prev. 2013, 52, 219–227. [Google Scholar] [CrossRef]
- Van der Horst, A.R.; De Goede, M.; De Hair-Buijssen, S.; Methorst, R. Traffic conflicts on bicycle paths: A systematic observation of behaviour from video. Accid. Anal. Prev. 2014, 62, 358–368. [Google Scholar] [CrossRef]
- Syed, S.H.; Willing, R.; Jenkyn, T.R.; Yazdani, A. Video analysis of the biomechanics of a bicycle accident resulting in significant facial fractures. J. Craniofac. Surg. 2013, 24, 2023–2029. [Google Scholar] [CrossRef]
- Haworth, N.; Debnath, A.K. How similar are two-unit bicycle and motorcycle crashes? Accid. Anal. Prev. 2013, 58, 15–25. [Google Scholar] [CrossRef]
- Richard, J.B.; Thelot, B.; Beck, F. Evolution of bicycle helmet use and its determinants in France: 2000–2010. Accid. Anal. Prev. 2013, 60, 113–120. [Google Scholar] [CrossRef]
- Castle, S.L.; Burke, R.V.; Arbogast, H.; Upperman, J.S. Bicycle helmet legislation and injury patterns in trauma patients under age 18. J. Surg. Res. 2012, 173, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Olivier, J.; Walter, S.R.; Grzebieta, R.H. Long-term bicycle related head injury trends for New South Wales, Australia following mandatory helmet legislation. Accid. Anal. Prev. 2013, 50, 1128–1134. [Google Scholar] [CrossRef][Green Version]
- EN 1078; Helmets for Pedal Cyclist and for Users of Skateboards and Roller Skates. European Committee for Standardization: Brussels, Belgium, 1997.[Green Version]
- Thai, K.T.; McIntosh, A.S.; Pang, T.Y. Bicycle helmet size, adjustment, and stability. Traffic Inj. Prev. 2014, 16, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Cummings, P.; Rivara, F.P.; Thompson, D.C.; Thompson, R.S. Misconception regarding case-control studies of bicycle helmets and head injury. Accid. Anal. Prev. 2006, 38, 636–643. [Google Scholar] [CrossRef]
- Hansen, K.; Dau, N.; Feist, F.; Deck, C.; Willinger, R.; Madey, S.M.; Bottlang, M. Angular Impact Mitigation system for bicycle helmets to reduce head acceleration and risk of traumatic brain injury. Accid. Anal. Prev. 2013, 59, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Milne, G.; Deck, C.; Bourdet, N.; Carreira, R.P.; Allinne, Q.; Gallego, A.; Willinger, R. Bicycle helmet modelling and validation under linear and tangential impacts. Int. J. Crashworthiness 2013, 19, 323–333. [Google Scholar] [CrossRef]
- Rizzi, M.; Stigson, S.; Krafft, M. Cyclist injuries leading to permanent medical impairment in Sweden and the effect of bicycle helmets. In Proceedings of the International Research Council on the Biomechanics of Injury Conference, Gothenburg, Sweden, 11–13 September 2013; pp. 412–423. [Google Scholar]
- Cripton, P.A.; Dressler, D.M.; Stuart, C.A.; Dennison, C.R. Bicycle helmets are highly effective at preventing head injury during head impact: Head-form accelerations and injury criteria for helmeted and unhelmeted impacts. Accid. Anal. Prev. 2014, 70, 1–7. [Google Scholar] [CrossRef]
- Farkkila, E.M.; Kaban, L.B.; Boos-Lima, F.; Peacock, Z.S. Association of craniomaxillofacial fractures and blunt cerebrovascular injuries. Int. J. Oral Maxillofac. Surg. 2023, 52, 847–853. [Google Scholar] [CrossRef]
- Galteland, P.; Doving, M.; Naess, I.; Sehic, A.; Utheim, T.P.; Eken, T.; Skaga, N.O.; Helseth, E.; Ramm-Pettersen, J. The association between head injury and facial fracture treatment: An observational study of hospitalized bicyclists from a level 1 trauma centre. Acta Neurochirurgica 2024, 166, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Goh, E.Z.; Beech, N.; Johnson, N.R. Traumatic maxillofacial and brain injuries: A systematic review. Int. J. Oral Maxillofac. Surg. 2021, 50, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Anagnostopoulos, T.; Ferreira, D.; Samodelkin, A.; Ahmed, M.; Kostakos, V. Cyclist-aware traffic lights through distributed smartphone sensing. Pervasive Mob. Comput. 2016, 31, 22–36. [Google Scholar] [CrossRef]
- Dudde, F.; Revend, L.; Revend, D.; Schuck, O.; Giese, M. Facial trauma in e-scooter vs. bicycle accidents: A retrospective comparative analysis in a metropolitan setting. Dent. Traumatol. 2025, 41, 641–648. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).