The Impact of Preoperative Education on Knee and Hip Replacement: A Systematic Review
Abstract
1. Introduction
Preoperative Education
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Study Inclusion Criteria
- Studies involving employed individuals of all ages with no restrictions.
- Studies that measure outcomes of patients who have undergone total hip arthroplasty (THA) and total knee arthroplasty (TKA) using generic scales administered to specific groups or at specific times, such as before and after preoperative education, and studies that report scores related to functionality and psychological aspects.
- Score (WOMAC, LOS, SF-36, NRS, AIMS, HAD, OKS, STAI, HR, HADS, NHP, SACL, OHS, PHWSUQ, VAS, RSES, NEADL, OPKQ, MEQ, KSS, KRES, HHS, ADL, APAIS, BPI-I).
- Only articles written in English were included.
2.1.2. Study Exclusion Criteria
- We excluded case reports, technical notes, letters to editors, instructional courses, in vitro and cadaver studies, protocol studies, reviews, validation studies, and books.
- We excluded patients who had not undergone osteoarthritis prostheses, who thus might have had infections, fractures, or tumors.
2.2. Search Strategy
2.3. Study Selection and Data Collection
2.4. Quality Assessment
2.5. Data Synthesis and Analysis
3. Results
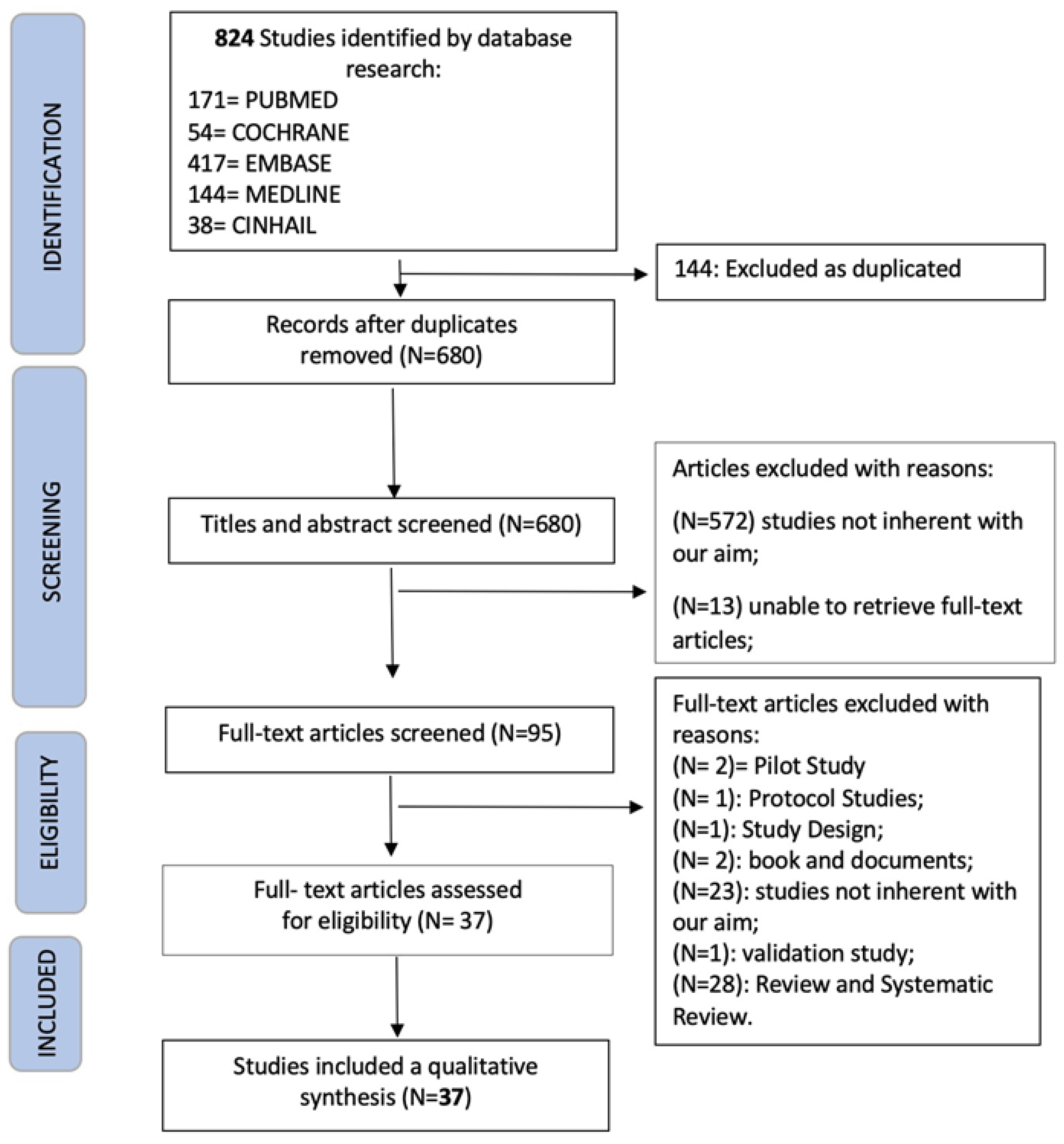
3.1. Study Selection
3.2. Study Characteristics
3.3. Results of Individual Studies
3.3.1. Outcome: Pain
3.3.2. Outcome: Satisfaction
3.3.3. Outcome: Anxiety
3.3.4. Outcome: LOS
3.4. Quality Assessment
3.4.1. Risk of Bias Assessment with MINOR for Non-Randomized Studies
3.4.2. Risk of Bias Assessment with MINOR for Randomized Studies
3.5. Synthesis of Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neogi, T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1145–1153. [Google Scholar] [CrossRef] [PubMed]
- Loeser, R.F. The Role of Aging in the Development of Osteoarthritis. Trans. Am. Clin. Climatol. Assoc. 2017, 128, 44–54. [Google Scholar]
- Longo, U.G.; De Salvatore, S.; Santamaria, G.; Indiveri, A.; Piergentili, I.; Salvatore, G.; De Marinis, M.G.; Bandini, B.; Denaro, V. Total Hip Replacement: Psychometric Validation of the Italian Version of Forgotten Joint Score (FJS-12). J. Clin. Med. 2023, 12, 1525. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Margiotti, K.; Longo, U.G.; Loppini, M.; Fazio, V.M.; Denaro, V. The genetics of sports injuries and athletic performance. Muscles Ligaments Tendons J. 2013, 3, 173–189. [Google Scholar] [CrossRef] [PubMed]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- McDonald, S.; Page, M.J.; Beringer, K.; Wasiak, J.; Sprowson, A. Preoperative education for hip or knee replacement. Cochrane Database Syst. Rev. 2014, 2014, CD003526. [Google Scholar] [CrossRef]
- Franceschi, F.; Longo, U.G.; Ruzzini, L.; Rizzello, G.; Denaro, V. Arthroscopic management of calcific tendinitis of the subscapularis tendon. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 1482–1485. [Google Scholar] [CrossRef]
- Longo, U.G.; Loppini, M.; Denaro, L.; Maffulli, N.; Denaro, V. Conservative management of patients with an osteoporotic vertebral fracture: A review of the literature. J. Bone Jt. Surg. Br. 2012, 94, 152–157. [Google Scholar] [CrossRef]
- Grappiolo, G.; Loppini, M.; Longo, U.G.; Traverso, F.; Mazziotta, G.; Denaro, V. Trabecular Metal Augments for the Management of Paprosky Type III Defects without Pelvic Discontinuity. J. Arthroplast. 2015, 30, 1024–1029. [Google Scholar] [CrossRef]
- Khanna, A.; Gougoulias, N.; Longo, U.G.; Maffulli, N. Minimally invasive total knee arthroplasty: A systematic review. Orthop. Clin. N. Am. 2009, 40, 479–489. [Google Scholar] [CrossRef]
- Moyer, R.; Ikert, K.; Long, K.; Marsh, J. The Value of Preoperative Exercise and Education for Patients Undergoing Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev. 2017, 5, e2. [Google Scholar] [CrossRef] [PubMed]
- Bravi, M.; Longo, U.G.; Laurito, A.; Greco, A.; Marino, M.; Maselli, M.; Sterzi, S.; Santacaterina, F. Supervised versus unsupervised rehabilitation following total knee arthroplasty: A systematic review and meta-analysis. Knee 2023, 40, 71–89. [Google Scholar] [CrossRef] [PubMed]
- Berge, D.J.; Dolin, S.J.; Williams, A.C.; Harman, R. Pre-operative and post-operative effect of a pain management programme prior to total hip replacement: A randomized controlled trial. Pain 2004, 110, 33–39. [Google Scholar] [CrossRef]
- Biau, D.J.; Porcher, R.; Roren, A.; Babinet, A.; Rosencher, N.; Chevret, S.; Poiraudeau, S.; Anract, P. Neither pre-operative education or a minimally invasive procedure have any influence on the recovery time after total hip replacement. Int. Orthop. 2015, 39, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Birch, S.; Stilling, M.; Mechlenburg, I.; Hansen, T.B. No effect of cognitive behavioral patient education for patients with pain catastrophizing before total knee arthroplasty: A randomized controlled trial. Acta Orthop. 2020, 91, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Bondy, L.R.; Sims, N.; Schroeder, D.R.; Offord, K.P.; Narr, B.J. The effect of anesthetic patient education on preoperative patient anxiety. Reg. Anesth. Pain Med. 1999, 24, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Butler, G.S.; Hurley, C.A.; Buchanan, K.L.; Smith-VanHorne, J. Prehospital education: Effectiveness with total hip replacement surgery patients. Patient Educ. Couns. 1996, 29, 189–197. [Google Scholar] [CrossRef]
- Clode-Baker, E.; Draper, E.; Raymond, N.; Haslam, C.; Gregg, P. Preparing patients for total hip replacement: A randomized controlled trial of a preoperative educational intervention. J. Health Psychol. 1997, 2, 107–114. [Google Scholar] [CrossRef]
- Daltroy, L.H.; Morlino, C.I.; Eaton, H.M.; Poss, R.; Liang, M.H. Preoperative education for total hip and knee replacement patients. Arthritis Care Res. 1998, 11, 469–478. [Google Scholar] [CrossRef]
- Doering, S.; Katzlberger, F.; Rumpold, G.; Roessler, S.; Hofstoetter, B.; Schatz, D.S.; Behensky, H.; Krismer, M.; Luz, G.; Innerhofer, P.; et al. Videotape preparation of patients before hip replacement surgery reduces stress. Psychosom. Med. 2000, 62, 365–373. [Google Scholar] [CrossRef]
- O’Connor, M.I.; Brennan, K.; Kazmerchak, S.; Pratt, J. YouTube Videos to Create a “Virtual Hospital Experience” for Hip and Knee Replacement Patients to Decrease Preoperative Anxiety: A Randomized Trial. Interact. J. Med. Res. 2016, 5, e10. [Google Scholar] [CrossRef] [PubMed]
- Gammon, J.; Mulholland, C.W. Effect of preparatory information prior to elective total hip replacement on post-operative physical coping outcomes. Int. J. Nurs. Stud. 1996, 33, 589–604. [Google Scholar] [CrossRef]
- Gammon, J.; Mulholland, C.W. Effect of preparatory information prior to elective total hip replacement on psychological coping outcomes. J. Adv. Nurs. 1996, 24, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Giraudet-Le Quintrec, J.S.; Coste, J.; Vastel, L.; Pacault, V.; Jeanne, L.; Lamas, J.P.; Kerboull, L.; Fougeray, M.; Conseiller, C.; Kahan, A.; et al. Positive effect of patient education for hip surgery: A randomized trial. Clin. Orthop. Relat. Res. 2003, 414, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.; Sung, C.C.; Wang, W.S.; Wang, B.H. The effects of the empowerment education program in older adults with total hip replacement surgery. J. Adv. Nurs. 2017, 73, 1848–1861. [Google Scholar] [CrossRef]
- Jepson, P.; Sands, G.; Beswick, A.D.; Davis, E.T.; Blom, A.W.; Sackley, C.M. A feasibility randomised controlled trial of pre-operative occupational therapy to optimise recovery for patients undergoing primary total hip replacement for osteoarthritis (PROOF-THR). Clin. Rehabil. 2016, 30, 156–166. [Google Scholar] [CrossRef]
- Johansson, K.; Salanterä, S.; Katajisto, J. Empowering orthopaedic patients through preadmission education: Results from a clinical study. Patient Educ. Couns. 2007, 66, 84–91. [Google Scholar] [CrossRef]
- Kearney, M.; Jennrich, M.K.; Lyons, S.; Robinson, R.; Berger, B. Effects of preoperative education on patient outcomes after joint replacement surgery. Orthop. Nurs. 2011, 30, 391–396. [Google Scholar] [CrossRef]
- Kennedy, D.; Wainwright, A.; Pereira, L.; Robarts, S.; Dickson, P.; Christian, J.; Webster, F. A qualitative study of patient education needs for hip and knee replacement. BMC Musculoskelet. Disord. 2017, 18, 413. [Google Scholar] [CrossRef]
- Leal-Blanquet, J.; Alentorn-Geli, E.; Ginés-Cespedosa, A.; Martínez-Díaz, S.; Cáceres, E.; Puig, L. Effects of an educational audiovisual videodisc on patients’ pre-operative expectations with total knee arthroplasty: A prospective randomized comparative study. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2595–2602. [Google Scholar] [CrossRef]
- Lewis, C. Value of an orthopaedic pre-admission clinic for total knee and hip replacements in a rural health service. Aust. J. Rural Health 1997, 5, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, R.; Semaan, S.; Marmar, E.C. Development and impact of a hospital-based perioperative patient education program in a joint replacement center. Orthop. Nurs. 1993, 12, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Lilja, Y.; Rydén, S.; Fridlund, B. Effects of extended preoperative information on perioperative stress: An anaesthetic nurse intervention for patients with breast cancer and total hip replacement. Intensive Crit. Care Nurs. 1998, 14, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, C.A.; Graziano, S.; Briskie, L.M.; Peterson, M.G.; Pellicci, P.M.; Salvati, E.A.; Sculco, T.P. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin. Orthop. Relat. Res. 2008, 466, 424–431. [Google Scholar] [CrossRef] [PubMed]
- McDonald, D.D.; Freeland, M.; Thomas, G.; Moore, J. Testing a preoperative pain management intervention for elders. Res. Nurs. Health 2001, 24, 402–409. [Google Scholar] [CrossRef]
- McGregor, A.H.; Rylands, H.; Owen, A.; Doré, C.J.; Hughes, S.P. Does preoperative hip rehabilitation advice improve recovery and patient satisfaction? J. Arthroplast. 2004, 19, 464–468. [Google Scholar] [CrossRef]
- Medina-Garzón, M. Effectiveness of a Nursing Intervention to Diminish Preoperative Anxiety in Patients Programmed for Knee Replacement Surgery: Preventive Controlled and Randomized Clinical Trial. Investig. Educ. Enferm. 2019, 37. [Google Scholar] [CrossRef][Green Version]
- Orr, P.M. An educational program for total hip and knee replacement patients as part of a total arthritis center program. Orthop. Nurs. 1990, 9, 61–69. [Google Scholar] [CrossRef]
- Pelt, C.E.; Gililland, J.M.; Erickson, J.A.; Trimble, D.E.; Anderson, M.B.; Peters, C.L. Improving Value in Total Joint Arthroplasty: A Comprehensive Patient Education and Management Program Decreases Discharge to Post-Acute Care Facilities and Post-Operative Complications. J. Arthroplast. 2018, 33, 14–18. [Google Scholar] [CrossRef]
- Prouty, A.; Cooper, M.; Thomas, P.; Christensen, J.; Strong, C.; Bowie, L.; Oermann, M.H. Multidisciplinary patient education for total joint replacement surgery patients. Orthop. Nurs. 2006, 25, 257–261. [Google Scholar] [CrossRef]
- O’ Reilly, M.; Mohamed, K.; Foy, D.; Sheehan, E. Educational impact of joint replacement school for patients undergoing total hip and knee arthroplasty: A prospective cohort study. Int. Orthop. 2018, 42, 2745–2754. [Google Scholar] [CrossRef] [PubMed]
- Roach, J.A.; Tremblay, L.M.; Bowers, D.L. A preoperative assessment and education program: Implementation and outcomes. Patient Educ. Couns. 1995, 25, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Santavirta, N.; Lillqvist, G.; Sarvimäki, A.; Honkanen, V.; Konttinen, Y.T.; Santavirta, S. Teaching of patients undergoing total hip replacement surgery. Int. J. Nurs. Stud. 1994, 31, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Siggeirsdottir, K.; Olafsson, O.; Jonsson, H.; Iwarsson, S.; Gudnason, V.; Jonsson, B.Y. Short hospital stay augmented with education and home-based rehabilitation improves function and quality of life after hip replacement: Randomized study of 50 patients with 6 months of follow-up. Acta Orthop. 2005, 76, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Sisak, K.; Darch, R.; Burgess, L.C.; Middleton, R.G.; Wainwright, T.W. A preoperative education class reduces length of stay for total knee replacement patients identified at risk of an extended length of stay. J. Rehabil. Med. 2019, 51, 788–796. [Google Scholar] [CrossRef]
- Sjöling, M.; Nordahl, G.; Olofsson, N.; Asplund, K. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ. Couns. 2003, 51, 169–176. [Google Scholar] [CrossRef]
- Wilson, R.A.; Watt-Watson, J.; Hodnett, E.; Tranmer, J. A Randomized Controlled Trial of an Individualized Preoperative Education Intervention for Symptom Management after Total Knee Arthroplasty. Orthop. Nurs. 2016, 35, 20–29. [Google Scholar] [CrossRef]
- Wong, J.; Wong, S. A randomized controlled trial of a new approach to preoperative teaching and patient compliance. Int. J. Nurs. Stud. 1985, 22, 105–115. [Google Scholar] [CrossRef]
- Yoon, R.S.; Nellans, K.W.; Geller, J.A.; Kim, A.D.; Jacobs, M.R.; Macaulay, W. Patient education before hip or knee arthroplasty lowers length of stay. J. Arthroplast. 2010, 25, 547–551. [Google Scholar] [CrossRef]
- Buonanno, P.; Laiola, A.; Palumbo, C.; Spinelli, G.; Terminiello, V.; Servillo, G. Italian validation of the Amsterdam Preoperative Anxiety and Information Scale. Minerva Anestesiol. 2017, 83, 705–711. [Google Scholar] [CrossRef]
- Aronson, J.K. Compliance, concordance, adherence. Br. J. Clin. Pharmacol. 2007, 63, 383–384. [Google Scholar] [CrossRef] [PubMed]
| Author | Year | Country | Study Design | Sample Size | Aim |
|---|---|---|---|---|---|
| Berge [13] | 2004 | United Kingdom | RCT | 40 (19, 21) | Measure the effects of PMP on patients’ pain and function after hip replacement surgery |
| Biau [14] | 2015 | France | RCT | 209 (105, 102) | Evaluate preoperative education versus no education |
| Birch [15] | 2020 | Denmark | RCT | 60 (31/29) | Investigate the effectiveness of patient education in pain coping among patients with moderate to high pain catastrophizing score before TKA. Secondary outcomes were physical function, quality of life, self-efficacy, and pain catastrophizing |
| Bondy [16] | 1999 | USA | RCT | 134 (65/69) | Evaluate the effects that materials mailed to the home relating to anesthetic-focused patient education may have on preoperative patient anxiety |
| Butler [17] | 1996 | Canada | RCT | 80 (32, 48) | Evaluate pre-hospital education and compare with anxiety, ability to adapt, and length of stay |
| Clode-Baker [18] | 1997 | United Kingdom | RCT | 78 (41, 37) | Verify that providing adequate information to patients before surgery brings many benefits |
| Daltroy [19] | 1998 | USA | RCT | 222 (168, 54) | Test two common psychoeducational procedures |
| Doering [20] | 2001 | Austria | RCT | 100 (46, 54) | Prepare patients before surgery with the aim of reducing stress and improving outcome |
| O’Connor [21] | 2016 | USA | RCT | 65 (36, 29) | Evaluate the potential impact of viewing this playlist on preoperative anxiety |
| Gammon [22] | 1996A | Great Britain | Not RTC | 82 (41, 41) | Evaluate the effect of preparatory information on a patient’s postoperative physical coping results following total hip replacement (THR) |
| Gammon [23] | 1996B | United Kingdom | Not RTC | 82 (41, 41) | Evaluate the effects of preparatory information on psychological coping outcomes among patients with total hip replacement (THR) |
| Giraudet-lequintrec [24] | 2003 | France | RCT | 100 (48, 52) | Compare patient education prior to total hip arthroplasty with the usual verbal information |
| Huang [25] | 2017 | Taiwan | RCT | 116 (59, 57) | Measure the effectiveness of an education empowerment program |
| Jepson [26] | 2016 | United Kingdom | RCT | 90 | Assess the feasibility of a pre-operative occupational therapy intervention |
| Johansson [27] | 2007 | Finland | RCT | 123 (62,61) | Determine if additional preoperative education is more effective than standard pre-education |
| Kearney [28] | 2011 | USA | Descriptive comparative study | 150 | Compare the results of patients who have attended and have not attended a hospital preoperative education class |
| Kennedy [29] | 2017 | Canada | Qualitative Study | 32 | Assess satisfaction with the educational material provided |
| Leal-Blanquet [30] | 2013 | Spain | RCT | 92 (42, 50) | Hypothesize that patients receiving standard information plus additional medical information through audiovisual video discs would modify their preoperative expectations more than those only receiving the standard information through medical interviews |
| Lewis [31] | 1997 | Australia | Not RTC | 87 (38, 49) | Determine the value of orthopaedical education in a pre-admission clinic for patients who were undergoing total knee and total hip replacements. |
| Lichtenstein [32] | 1993 | USA | Qualitative Study | 535 | Describe the development and impact of a hospital-based education program for patients undergoing knee or hip replacement surgery |
| Lilja [33] | 1998 | Sweden | RCT | 50 (22, 28) | Evaluate the effects of extended preoperative information |
| Mancuso [34] | 2008 | USA | RCT | 324 (160, 160) | Evaluate the importance of expectations and associations between expectations and function |
| McDonald [35] | 2001 | USA | RCT | 31 (13, 18) | Test a Preoperative Pain Management Intervention for Elders |
| McGregor [36] | 2004 | United Kingdom | RCT | 35 (15, 16) | Investigate if preoperative rehabilitation advice with an information booklet can help recovery |
| Medina-Garzon [37] | 2019 | Colombia | RCT | 56 (28, 28) | Determine the effectiveness of a nursing intervention to diminish preoperative anxiety |
| Montgomery Orr [38] | 1990 | USA | Not RCT | 203 | Use the program to attempt to prevent complications, decrease anxiety, and decrease pain and hospital length of stay |
| Pelt [39] | 2018 | USA | Cohort Study | 462 | Assess the exposure of the pathway on discharge disposition as well as institutional 30-day and 90-day readmissions and reoperations |
| Prouty [40] | 2006 | USA | Qualitative Study | 2066 | Evaluate a preoperative educational program through surveys |
| O’Reilly [41] | 2018 | United Kingdom | Cohort Study | 57 | Assess patient understanding to ensure a sustained, high level of patient care, quality assurance, and educational standards |
| Roach [42] | 1995 | USA | Not RCT | 463 | Highlight the effectiveness of preoperative assessment and educational programs |
| Santavirta [43] | 1994 | Finland | RCT | 60 (27, 33) | Analyze the patients’ needs and study the results of intensified patient teaching |
| Siggeirsdottir [44] | 2005 | USA | RCT | 50 (27, 23) | Study the effectiveness of preoperative education during a shorter hospital stay |
| Sisak [45] | 2019 | United Kingdom | Cohort Study | 1233 (1018, 215) | Establish whether attendance at an education class prior to total hip or knee replacement surgery as part of an enhanced recovery after surgery pathway could decrease length of hospital stay |
| Sjoling [46] | 2003 | Sweden | RCT | 60 (30, 30) | Study the impact of preoperative information on state and trait anxiety |
| Wilson [47] | 2016 | Canada | RCT | 143 | Determine the effect of a preoperative educational intervention |
| Wong [48] | 1985 | Canada | RCT | 98 (51, 47) | Evaluate the effects of a new approach to preoperative teaching |
| Yoon [49] | 2010 | USA | Cohort Study | 261 | Study how education programs influence hospital length of stay |
| Author | Mean Age | Female/Male | Joint | Education Program for Intervention Group | Outcome Measures | Conclusion |
|---|---|---|---|---|---|---|
| Berge [13] | i: 71.6 (S.D. = 6) c: 71 (S.D. = 6.1) | 12/15 | Hip | Pain management education for one to two mornings/week for 6 week | NRS, AIMS | PAIN+ * SLEEP+ * ANALGESIC INTAKE = IMPROVED FUNCTIONS = |
| Biau [14] | 66 (range 60–74) | 121/209 | Hip | Small group education on postoperative exercises and pain management with practical demonstration. One session 4 week before to surgery | NRS, LOS | PAIN = LOS = |
| Birch [15] | 66 (range 47–82) | 40/20 | Knee | Two physiotherapists followed a manual describing in detail the content in each of the seven sessions | VAS, OKS, KOOS, EQ-5D, PSEQ, PCS. | PAIN (catastrophizing) = IMPROVED FUNCTION = QUALITY OF LIFE = SELF EFFICACY = |
| Bondy [16] | i: 65.3 (S.D. = 12.0) c: 64.9 (S.D. = 11.3) | 109/81 | Both | Two pamphlets and a video describing general and regional anesthesia | STAI | ANXIETY+ * |
| Butler [17] | 62.6 (S.D. 12.95) | 41/39 | Hip | Booklet about biophysiological, functional, experiential, and social information related to THA | STAI, purpose-designed questionnaire, HR | ANXIETY (preoperative and postoperative)+ * SATISFACTION RATING = LOS = ADHERENCE TO EXERCISES+ * OCCUPATIONAL THERAPY+ * |
| Clode-Baker [18] | - | 52/26 | Hip | Video, booklet, and plastic models for patients undergoing total hip replacement | HADS, NHP, and Stress Arousal Checklist. | SATISFACTION RATING+ * CAREGIVER SATISFACTION+ * PAIN = SLEEP = LOS MANAGEMENT+ * |
| Daltroy [19] | 64.0 (S.D. = 12) | 147/75 | Both | Audiotape slide program presented the day before surgery | Speilberger’s Zo-item anxiety, Wilson’s three-item scale, LOS, MMSE | PAIN (postoperative) = ANXIETY+ * ANALGESIC INTAKE+ * LOS+ * POSTOPERATIVE MENTAL STATE+ * |
| Doering [20] | i: 58.7 (S.D. = 10.8) c: 60.4 (S.D. = 8.7) | 38/62 | Hip | Educational video (1 day) | VAS, STAI | ANXIETY (properative and postoperative)+ * INTRAOPERATIVE VITAL SIGNS+ * PAIN = ANALGESIC INTAKE+ * CORTISOL LEVELS+ * |
| O’Connor [21] | c: 63.1 (S.D. = 10.7) i: 67.4 (S.D. = 10.3) | 31/22 | Both | Sixteen YouTube videos aimed at creating a virtual hospital experience for primary total hip and knee joint replacement patients | GAD | ANXIETY (preoperatory)+ SATISFACTION RATING+ * |
| Gammon [22] | 44–82 | 56/24 | Hip | Booklet with information of a sensory and procedural nature and suggestions on possible coping methods and strategies | VAS and purpose designed by postoperative pain analgesia, ability to mobilize, performing exercises, complications, LOS | ANALGESIC INTAKE = ANALGESIC INTAKE (intramuscular)+ * IMPROVED FUNCTIONS+ * ADHERENCE TO EXERCISES+ * COMPLICATIONS–(not statistically significant) LOS+ * COPING+ * |
| Gammon [23] | 44–82 | 56/24 | Hip | Booklet with information of a sensory and procedural nature and suggestions on possible coping methods and strategies | HADS, Healt Illness Questionnaire, Linear Analogue Coping scale | COPING+ * ANXIETY+ * PAIN+ * POSTOPERATIVE MENTAL STATE+ * SELF ESTEEM+ * SENSE OF CONTROL+ * |
| Giraudet-lequintrec [24] | i: 62.7 (S.D. = 8.8) c: 64.3 (S.D. = 9.5) | 56/44 | Hip | Collective multidisciplinary information session 2 to 6 weeks before surgery | STAI, VAS, LOS | ANXIETY+ * PAIN (pre-operative and postoperative)+ * IMPROVED FUNCTIONS+ * |
| Huang [25] | 66.05 (S.D. = 9.46) | 53/63 | Knee | Intervention program for educational empowerment (five meetings in 12 weeks) | THR Self-efficacy Scale, ADL, Barthel, GDS, SF-36 | SELF-EFFICACY+ * COMPLIANCE+ * POSTOPERATIVE MENTAL STATE+ * IMPROVED FUNCTIONS = |
| Jepson [26] | 66 (S.D. = 10.8) | 33/57 | Hip | In-home education by an occupational therapist | LOS, NEADL, HADS, WOMAC | PAIN+ * IMPROVED FUNCTIONS+ * ANXIETY+ * |
| Johansson [27] | 62.4 (range and SD not found) | 63/60 | Hip | Educational concept maps by biophysiological, functional, experiential, ethical, social, and financial issues related to care for 30–60 min, 2 week prior | OPKQ, MEQ | KNOWLEDGE+ * |
| Kearney [28] | i: 67.25 (S.D. = 10.8) c: 64.5 (S.D. = 11.2) | 90/60 | Both | Structured online course including book; brochure; CD from MD; and information from hospital, family, friend, joint class, mailing, and neighbor prior to surgery. | Research questions, NRS | SATISFACTION RATING+ * PAIN = LOS = IMPROVED FUNCTIONS = COMPLICATION RATE = |
| Leal-Blanquet [30] | i: 72.1 (S.D. = 7.4) c: 73.4 (S.D. = 6.5) | 69/23 | Knee | Ten-minute DVD with the process from admission to surgical intervention, recovery room, immediate postoperative care, and outpatient care | KSS, KRES | SATISFACTION RATING = IMPROVED FUNCTIONS = |
| Lewis [31] | (34–87) | 42/45 | Both | Multidisciplinary team show a video of the type of joint replacement surgery. They instruct on the use of analgesics, devices, and physical exercises | LOS | LOS+ * |
| Lilja [33] | 65 (range and SD not found) | 17/33 | Hip | Information by the anesthetic nurse about what was going to happen to the patient. This information was given for half an hour on the day before surgery | HADS, VAS, S-Cortisol | PAIN = CORTISOL LEVELS = ANXIETY = |
| Mancuso [34,35] | THA i: 71 c: 70 (S.D. 6) TKA i: 72 c: 71 (S.D. = 8) | 181/139 | Both | Educational modules that address recovery over 12 months to make patients’ expectations more effective | WOMAC, SF-36 | EXPECTATIONS+ * |
| McDonald [35] | 74 (S.D. = 6.16) | 8/23 | Both | PowerPoint slide shown to teach basic pain management and pain communication skills. | MPQ-SF, PPI | PAIN+ * |
| McGregor [36] | 71.9 (S.D. = 9.3) | 25 /10 | Hip | Education, gait aid instruction, and exercise for 2–4 week | WOMAC, HHS, ADL | SATISFACTION RATING+ * LOS+ * IMPROVED FUNCTIONS = PAIN = |
| Medina-Garzon [37] | i: 76.32 (S.D. = 16.1) c: 73.7 (S.D. = 16.6) | 26 /29 | Knee | Three sessions of motivational interview, each lasting 40 min, during the 6 weeks prior to surgery | APAIS | ANXIETY (preoperative) + |
| Montgomery Orr [38] | - | Both | Five different classes that started in an outpatient setting and continued in the inpatient unit. The program bridged the gap between the scheduling of surgery, admission to the hospital, surgery, and discharge | LOS, questionnaire | LOS+ * ANXIETY+ * | |
| Pelt [39] | i: 63 (range = 15–87) c: 62 (range = 24–92) | 265/197 | Both | Nine short videos about what the patient should be learning and doing before surgery and what to expect on the day of surgery, during the hospital stay, and when they return home + “joint academy” class | PAC | COMPLICATION RATE+ * |
| O’Reilly [41] | 64.5 (range and SD not found) | 30/27 | Both | Combination of PowerPoint presentations, educational videos, and model demonstrations | Kruskal–Wallis H-test | KNOWLEDGE+ * |
| Roach [42] | - | - | Both | Four-hour multidisciplinary program offered twice a week in the orthopedic unit for patients and their families for 2–4 weeks with written information support | LOS | LOS+ * IMPROVED FUNCTIONS+ * EFFICIENCY+ * CAREGIVER SATISFACTION+ * |
| Santavirta [43] | 58.9 (S.D. = 5.64) | 38/22 | Hip | Illustrated patient guide | Mann–Whitney U-test, McNemar’s test, Wilcoxon signed-rank test | ADHERENCE TO EXERCISES+ * KNOWLEDGE = SATISFACTION+ * COMPLICATION RATE = |
| Siggeirsdottir [44] | 68 (range = 28–86) | 26/24 | Hip | Preoperative program 1 month before surgery with illustrated brochure and consultancy with specialists: familiarization with exercises and devices | OHS, LOS | LOS+ * PAIN+ * IMPROVED FUNCTIONS+ * SLEEP = |
| Sisak [45] | THR i: 69.87 (S.D. = 9.7) c: 70.96 (S.D. = 10.63) TKR i: 70.90 (S.D. = 8.22) c: 72.15 (S.D. = 8.73) | 629/389 | Both | Preoperative education class (range 2–21 days before surgery) | LOS | LOS+ * |
| Sjoling [46] | 71 (range = 54–86) | 36/24 | Knee | Information class (20–40 min) 1–4 days before surgery | VAS, LOS | PAIN+ * ANXIETY+ * SATISFACTION RATING+ * ANALGESIC INTAKE = LOS = |
| Wilson [47] | i: 67 (S.D. = 8) c: 66 (S.D. = 8) | 89/54 | Knee | Three components: the booklet, an individual teaching session, and a follow-up support telephone call | BPI-I, MPQ-SF | PAIN = NAUSEA = ANALGESIC INTAKE = |
| Wong [48] | (range = 50–89) | 67/31 | Hip | LAP that included five learning-activity packages | MW (Mann–Whitney) | SATISFACTION RATING+ * ADHERENCE TO EXERCISES+ * |
| Yoon [49] | 66.3 (S.D. = 11.2) | 95/163 | Both | One-on-one education session via phone regarding the specifics of their scheduled procedure, hospital stay, and recovery | LOS | LOS+ * |
| Author | Outcome Results | |
|---|---|---|
| Berge [13] | Intervention group reported significantly less average pain intensity (means for PMP and control groups = 4.47, 6.65, respectively, t (1.34) = −2,99; p = 0.005), less average pain distress (means = 4.11, 6.12, t (1.34) = −2,22; p = 0.033), and less sleep disturbance from hip pain (means =3.37, 5.29, t (1.34) = −2,04; p = 0.05) than waiting list controls. There were no statistically significant differences between groups for the following variables: weak opioid use, NSAID use (x2, p > 0.1), paracetamol use, or any drug use (Fisher’s p >0.1); pain interference; AIMS total or subscales of mobility, depression, and anxiety; meters walked in 4 min (t (1.34) = −1:37–1,19; p > 0.1); and AIMS physical activity (U = 145.5; p > 0.1). | |
| Biau [14] | 65 | The median time to reach complete independence was five days in all groups. There was no significant effect of either education (HR: 1.1; 95% CI: 0.76–1.5; p = 0.77). NRS: Recovery i: 2 (1–5) c: 2 (0–6) (p = 0.95). Day 1 i: 2 (1–4) c: 2 (1–4) (p = 0.43). Day 3 i: 1 (0–3) c: 2 (0–3) (p = 0.26). |
| Birch [15] | - | VAS during activity Baseline 48 (41–55) 31 49 (42–57) 29, 12 months 12 (5–18) 24 9 (3–15) 26 VAS during rest; Baseline 19 (13–24) 31 25 (19–30) 29, 12 months 7 (1–12) 24 6 (1–12) 26 Oxford Knee Score; Baseline 21 (19–23) 31 22 (20–24) 29, 12 months 33 (29–37) 24 37 (33–41) 24 KOOS pain; Baseline 40 (35–45) 31 37 (32–43) 27, 12 months 75 (67–82) 24 83 (75– 90) 23 EQ-5D; Baseline 0.58 (0.52–0.66) 29 0.62 (0.54–0.70) 26, 12 months 0.78 (0.70–0.86) 24 0.86 (0.81–0.91) 24 PSEQ; Baseline 33 (30–36) 31 34 (31–38) 29, 12 months 49 (44–53) 23 52 (48–57) 25 PCS; Baseline 30 (28–32) 31 31 (29–33) 29, 12 months 11 (7–16) 23 9 (5–14) 25 6 min walk test; Baseline 387 (350–424) 31 334 (296–372) 29, 12 months 441 (402–480) 24 406 (367–446) 26 sit-to-stand; Baseline 10 (9–11) 31 9 (8–10) 29, 12 months 12 (11–14) 24 11 (10–13) 26 (p < 0.05). |
| Bondy [16] | STAI State Score Baseline i: 34.8 ± 13.5 (33.0) c: 30.7 − 12.3 (30.0) Presurgery i: 35.0 ± I5.2 (36.0) c: 34.6 − 11.4 (35.0); Trait Score Baseline i: 33.5 + 10.8 (32.0) c: 30.2 ± 10.4 (30,0); Presurgery i: 31.5 ± 10.8 (30.0) c: 29.3 ± 10.i (29.0) p i: 0.031 c: 0.073. | |
| Butler [17] | Patients in the Booklet Group (N = 30) had a mean percentile score of 27.93 (S.D. = 25.24) at time of hospital admission, and a mean percentile score of 21.57 (S.D. = 18.44) the day prior to discharge. Means for the No-Booklet Group (N = 40) were 42.65 (S.D. = 29.06) at admission and 31.15 (S.D. = 22.93) at discharge. Patients in the Booklet Group were far more likely to practice breathing and coughing exercises (55% of Booklet patients compared to 15% of No-Booklet patients), log rolling (39% vs. 6%); and leg exercises (65% vs. 24%). Despite the differences in anxiety and rates of engaging in prehospital preparatory exercises, there were no significant differences for length of hospital stay between the Booklet (mean = 10.28 days, S.D. = 4.74) and No-Booklet (mean = 10.38 days, S.D. = 5.53) groups. Physioterapy i: 7.29 (2.79) c: 9.24 (4.34) p < 0.05. Occupational terapy i: 2.21 (1.35) c: 3.07 (1.99) p = 0.045. Deep breathing and coughing exercises i: 55% c: 15% (p < 0.001). Leg rolling i: 39% c: 6% (p < 0.001). Leg exercises i: 65% c: 24% (p < 0.001). | |
| Clode-Baker [18] | Stress Score median i: 5, median c: 3 (p = 0.31). Arousal score median i: 4 median C:5 (p = 0.13). HAD Anxiety score preoperative. Median i: 6 median c: 8 (p = 0.1). Anxiety score postoperative median i: 5 median C:5 (p = 0.7). Depression score preoperative median i: 7, median c: 7 (p = 1). Depression score postoperative median i: 4, median c: 4 (p = 0.99). NHP preoperative median i: 19, median c: 17.5 (p = 0.89), postoperative median i: 10, median c: 9 (p = 0.33). | |
| Daltroy [19] | LOS: patients who received information had shorter LOS than controls (0.67 days less, on average); patients in the bottom quartile (least denial) who received information had greater length of stay (1.94 days) than controls. The average anxiety level 4 days postoperatively was 1.9 (scaled 1 = low to 4 = high; SD 0.56). The average pain level 4 days postoperatively was 2.4 (scaled 1 to 5; SD 0.85). General linear models analysis indicated that 24% of the variance in pain was explained by the covariates and intervention effects (F = 6.55, 10,207 df; p < 0.0001). The average patient used the equivalent of 9.9 units of morphine during the first 4 days postoperatively (range 0.0–62.1; median 8.0; SD 8.3). Neither the information intervention (p = 0.059) nor the relaxation intervention (p = 0.52) nor their interaction (p = 0.51) was associated with better mental status, although the trend was favorable for information provision. | |
| Doering [20] | Trait anxiety (stanine value) 5.0 ± 1.9 5.3 ± 1.9. Depression (stanine value) 6.1 ± 1.7 6.2 ± 1.9. Pain during previous week (VAS 0–100 mm) 57 ± 25.4 62.1 ± 21.5 (p > 0.05). | |
| O’Connor [21] | GAD Median (range) c: 0.0 (−7, 4) i: −1.0 (−12,7) p = 0.53. | |
| Gammon [22] | Oral analgesia c: 22.5 i: 18.8 (p > 0.05), intramuscular analgesia c: 4 i: 2 (p < 0.01), Mobilization Zimmer c: 3 i: 2 (p < 0.05), Mobilization Stick c: 5 i: 3 (p < 0.05), Breathing exercises c: > 15 i: 1 (p < 0.05), Foot/ leg exercises c: > 5 i: 1 (p < 0.01), Postoperative complication c: 2.5 i: 2.9 (p > 0.05), Length of stay c: 17 i: 14 (p < 0.001). The mean number of complications for the experimental group was 2.5 (range G3), and 2.9 (range O-4) for the control. Although the experimental groups had fewer complications, this was not statistically significant. (p < 0.05). LOS i: 14 (range 10–22 days) c: 17 (range 12–25) (p< 0.001). COPING i;6.6 c: 4.1 (p < 0.001) | |
| Gammon [23] | Anxiety observed i: 42 c: 44 (p < 0.001). Depression i: 42 c: 68 (p < 0.001). Self-esteem i: 19 c: 174 (p < 0.001). Sense of control i: 199 c: 112 (p < 0.01). Patient assesment of coping i: 66 c: 43 (p < 0.001). | |
| Giraudet-lequintrec [24] | Preoperative VAS i: 24 c: 35 (p 0.04). Postoperative VAS i: 21 c: 28 (p 0.07). Preoperative anxiety i: −1.74 c: + 1.81 (p 0.08). Postoperative anxiety i: -4.16 c: -2.53 (p 0.5). | |
| Huang [25] | S-E (T4) i: 2.87 c: 2.66 competence (T4) K i: 14.94 c: 14.59 B i: 21.20 c: 17.33 ADL (T4) i: 99.07 c: 98.33 GDS-15 (T4) i: 2.02 c: 2.87 QOL (T4) i: 69.08 c: 66.74 All (p < 0.05). | |
| Jepson [26] | WOMAC c: 61.41 i: 56.50 WOMAC 26 WEEKS c: 15.67 i: 9.95 HADS 6.56 (4.58) 6.71 (5.33) HADS 26 WEEKS 3.52 (3.66) 2.87 (3.62) NEADL 49.26 (10.32) 47.28 (14.67 NEADL 26 WEEKS 57.34 (16.18) 62.53 (6.95). | |
| Johansson [27] | Time for discussions on admission A: M = 13.25 min, B: M = 33.36 min, p < 0.001 OPKQ at discharge i: 4.3 c: 4.03 (p < 0.022). | |
| Kearney [28] | Patients who had attended the structured preoperative class felt significantly better prepared for surgery (mean 1.2 vs. 1.4, p 0.002, where 1 corresponded to very much so and 2 to somewhat) and they also felt better able to control their pain after surgery (mean 1.4 vs. 1.7, p 0.001, where 1 corresponded to very much so and 2 to somewhat). | |
| Leal-Blanquet [30] | Knee ROM c: 0.1 i: 0 (p = 0.04). Going up the stairs c: -0.04 i: 0.1 (p = 0.03). Going down the stairs c: −0.02 i: 0.2 (p = 0.03). Other result p = n.s. | |
| Lilja [33] | HADS Day0 i: 5 c: 3 (p < 0.01) S-Cortisol Day0 i: 370 c: 368 VAS Day3 i: 1.3 c: 2.5 | |
| Mancuso [34,35] | WOMAC. Pain i (THA)51 ± 17 c (THA) 49 ± 20 (p = 0.20) i (TKA)45 ± 19 c (TKA)48 ± 21 (p = 0.40). Stiffness i (THA)54 ± 18 c (THA) 51 ± 19 0.40 i (TKA)50 ± 19 c (TKA)55 ± 19 (p = 0.20). Function i (THA)57 ± 16 c (THA)55 ± 18 0.30 i (TKA)52 ± 16 c (TKA)54 ± 19 (p = 0.60). SF-36 Physical function i (THA)17 ± 20 c (THA)20 ± 22 0.40 i (TKA)18 ± 18 c (TKA)17 ± 20 (p = 0.60). Pain i (THA)39 ± 15 c (THA)43 ± 19 0.20 i (TKA)43 ± 16 c (TKA)40 ± 19 (p = 0.20). | |
| McDonald [35] | PPI Intensity DOS i: 2.6 (SD:1.39) c: 2.2 (SD:1.06) POD2 i: 1.6 (SD:0.77) c: 2.2 (SD:1.47) Affective DOS i: 2.3 (SD:1.97) c: 3.8 (SD:2.50) POD2 i: 2.2 (SD:2.28) c: 2.6 (SD:3.00). Sensory DOS i: 9.9 (SD:5.58) c: 7.7 (SD:5.29). POD2 i: 6.1 (SD:4.66) c: 7.6 (SD:6.21). | |
| McGregor [36] | i: Admission Pain 7.8, Womac Pain 10.2, Womac Stiffness 4.3, Womac Function 35.8, HHS 45.4, Barthel Index 19.2. c: Admission Pain: 7.6, Womac Pain 10.3, Womac Stiffness 4.1, Womac Function 41.0, HHS 43.2, Barthel Index 19 i: 3-Month Review Pain 2.1 Womac Pain 2.7, Womac Stiffness 1.1, Womac Function 15.9, HHS 74.2, Barthel Index 19.9 c: 3-Month Review Pain 3.1 Womac Pain 0.05, Womac Stiffness 1.6, Womac Function 18.4, HHS 68.8, Barthel Index 19.6 (p < 0.005). | |
| Medina-Garzon [37] | The mean score of preoperative anxiety was equal in the pre-intervention evaluation in both groups (19.76 in the experimental versus 22.02 in the control = 22.02; p < 0.226), while during the post-intervention, the anxiety score was lower in the intervention group compared with the control group (15.56 and 20.30, respectively; p < 0.013). | |
| Montgomery Orr [38] | −8/23. | |
| Pelt [39] | There was a 20% absolute reduction in discharges to PACs (<0.001). The frequency of 30-day readmissions was greater in patients who underwent TJA before implementation (incidence rate ratio [IRR]. 1.93, 95% confidence interval [CI]. 1.01–3.69). The risk for 90-day readmissions (IRR 1.70, 95% CI 1.20–2.40) and reoperations (IRR 1.67, 95% CI 1.12–2.53) was greater prior to implementation. Discharge to PACs was associated with 2.4 and 3.10 times greater risk for 30-day readmissions (95% CI 1.28–4.56) and 30-day reoperations (95% CI 1.40–7.0), respectively. Patients discharged to PACs were also at greater risk for both 90-day readmissions (IRR 1.59, 95% CI 1.08–2.32) and 90-day reoperations (IRR 1.75, 95% CI 1.12–2.73), p < 0.001. | |
| O’Reilly [41] | Anesthetic type 0.00210 p = 0.963 Anesthetic complications 30.48084 p < 0.001. Items required on admission 60.58557 p < 0.001 Length of stay 18.07776 p < 0.001. Physiotherapy requirements 3.82730 p = 0.050 Walking aid requirements 7.37168 p = 0.007. Understanding of procedure/operation 36.59683 p < 0.001. Smoking-related complications 14.21220 p < 0.00. | |
| Roach [42] | Average LOS i: 8.0 days, c: 8.7 days. | |
| Santavirta [43] | The experimental group had followed the instructions for the exercise program more often than the control group (p = 0.02, Chi-square). Patients who received information increased fruit consumption (p = 0.05, McNemar test). The intervention group’s knowledge of symptoms and complications were not statistically better than that of the controls (p = 0.2, Mann–Whitney U-test). The experimental group showed more satisfied with the information they had received. There was no statistical difference in the number of early complications and the two- to three-month rehabilitation results between the two groups. Confusing or controversial information from different health care professionals/groups t: 422.5 p: 0.2519. Teaching and verbal information presented clearly t: 475.0 p: 0.0913. Teaching and information always adjusted to individual situation t: 305.0 p: 0.3132. At home, many items remained unclear t: 332.5 p: 0.3293. | |
| Siggeirsdottir [44] | Mean hospital stay was shorter for the SG than for the CG (6.4 days and 10 days, respectively; p < 0.001). During the 6-month study period, there were nine non-fatal complications in the SG and 12 in the CG (p = 0.3). The difference in Oxford Hip Score between the groups was not statistically significant before the operation, but was better for the SG at 2 months (p = 0.03), and this difference remained more or less constant throughout the study. | |
| Sisak [45] | Mean length of stay was reduced by 0.37 days for patients who had received total hip replacement surgery (95% CI –0.74, –0.01, p = 0.05) and by 0.77 days for patients who had undergone total knee replacement (95% CI –1.23, –0.31, p = 0.001). | |
| Sjoling [46] | State anxiety i: 29 (96.7) c: 30 (100) p = 0.009 VAS (Day 2) i: 0.28 c: 0.41 p < 0.05. Satisfaction i: 100% c: 87% p < 0.05. | |
| Wilson [47] | Analgesic intake Day 3 i: 40 (45) c: 40 (42) BPI-I i: 24.4 (14.4) c: 22.4 (15.1) p = 0.45 MPQ-SF. Pain right now at rest Day3 i: 2.8 c: 2.8 p = 0.7. Pain right now when moving Day3 i: 5.4 c: 6.1 p = 0.2 Worst pain last 24 h i: 7.0 c: 7.0 p = 0.87. | |
| Wong [48] | Satisfaction, willingness and regularity, accuracy, and deep breathing. MW E > C p < 0.001. | |
| Yoon [49] | LOS: total hip arthroplasty 3.1 ± 0.8 days vs. 3.9 ± 1.4 days; p = 0.0001; total knee arthroplasty 3.1 ± 0.9 days vs. 4.1 ± 1.9 days; p = 0.001. | |
| Author | Mean Age | Female/Male | Joint | Education Program for Intervention Group | Follow-Up | Outcome Results | Conclusion |
|---|---|---|---|---|---|---|---|
| Kennedy [29] | 67.9 (S.D. = 7.82) | 16/16 | Both | A focus group guide to address four specific aspects of the patient’s experience with educational material and a preoperative education class | 12 months | One of the key themes that emerged was a need for more education concerning pain management postoperatively. Poorly managed pain decreases patient satisfaction and the ability to progress functionally | PAIN= |
| Lichtenstein [32] | 65 | - | Both | A 1 h education session conducted by a case manager providing information on what to expect from the procedure | 2 months, 6 months, 12 months | More than 90 percent of the patients that responded to the questionnaire indicated that the program was helpful in preparing them for their surgical experience and for their home discharge needs. Additionally, the rate of compliance of the patient with medical advice was high, as demonstrated by their adherence to the physical exercise regimen | SATISFACTION RATING+ * COMPLICATION RATE+ * |
| Prouty [40] | - | - | Both | HOPE educational program: 2 h for 3 week of educational program for the patient and the caregiver | - | Evaluations indicated that patients’ expectations of the program were met, they were less anxious about their surgery as a result of attending the classes, and the preoperative teaching by the multidisciplinary team was effective | ANXIETY+ * SELF-EFFICACY+ * SATISFACTION RATING+ * |
| Author | Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Data Collection | Endpoints Appropriate to Study Aim | Unbiased Assessment of Study Endpoint | Follow-Up Period Appropriate to Study Aim | <5% Lost to Follow-Up | Prospective Calculation of Study Size | Adequate Control Group | Contemporary Groups | Baseline Equivalence of Groups | Adequate Statistical Analyses | Total Score (…/24) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gammon [22], 1996A | 2 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | 15/24 |
| Gammon [23], 1996B | 2 | 1 | 2 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | 15/24 |
| Kearney [28], 2011 | 2 | 1 | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 20/24 |
| Kennedy [29], 2017 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | NA | 0 | 0 | 2 | 16/24 |
| Lewis [31] | 2 | 2 | 0 | 1 | 1 | 1 | 0 | 2 | 2 | 2 | 0 | 0 | 13/24 |
| Lichtenstein [32], 1993 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 13/24 |
| Montgomery Orr [38] | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7/24 |
| Pelt [39], 2018 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 1 | 1 | 0 | 0 | 14/24 |
| Prouty [40], 2006 | 2 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 5/24 |
| O’Reilly [41], 2018 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | NA | 0 | 1 | 2 | 18/24 |
| Sisak [45]2019 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 0 | 2 | 18/24 |
| Yoon [49], 2010 | 2 | 0 | 1 | 2 | 1 | 2 | 2 | 0 | NA | 0 | 0 | 0 | 10/24 |
| Title Article | Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Outcome Reporting | Other Sources of Bias | Punteggio Totale (Overall Score) |
|---|---|---|---|---|---|---|---|---|
| Berge [13], 2004 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 3 |
| Birch [15], 2020 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 2 |
| Biau [14], 2015 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bondy [16], 1999 | 0 | 0 | 2 | 2 | 1 | 2 | 2 | 9 |
| Butler [17], 1996 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
| Clode-Baker [18], 1997 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| Daltroy [19], 1998 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Doering [20], 2000 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Giraudet-Lequintrec [24], 2003 | 0 | 0 | 2 | 1 | 0 | 2 | 0 | 5 |
| Huang [25], 2017 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Jepson [26], 2016 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Johansson [27], 2007 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 4 |
| Leal-Blanquet [30], 2012 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 4 |
| Lilja [33], 1998 | 0 | 0 | 2 | 2 | 1 | 0 | 0 | 5 |
| Mancuso [34,35], 2008 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| McDonald [35], 2001 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| McGregor [36], 2004 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 3 |
| Medina-Garzon [37], 2019 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| O’Connor [21], 2016 | 0 | 1 | 2 | 2 | 0 | 0 | 1 | 6 |
| Roach [42], 1995 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 5 |
| Santavirta [43], 1994 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 4 |
| Siggeirsdottir [44], 2005 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 4 |
| Sjoling [46], 2003 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Wilson [47],2016 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Wong [48], 1985 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; De Salvatore, S.; Rosati, C.; Pisani, I.; Ceccaroli, A.; Rizzello, G.; De Marinis, M.G.; Denaro, V. The Impact of Preoperative Education on Knee and Hip Replacement: A Systematic Review. Osteology 2023, 3, 94-112. https://doi.org/10.3390/osteology3030010
Longo UG, De Salvatore S, Rosati C, Pisani I, Ceccaroli A, Rizzello G, De Marinis MG, Denaro V. The Impact of Preoperative Education on Knee and Hip Replacement: A Systematic Review. Osteology. 2023; 3(3):94-112. https://doi.org/10.3390/osteology3030010
Chicago/Turabian StyleLongo, Umile Giuseppe, Sergio De Salvatore, Chiara Rosati, Irene Pisani, Alice Ceccaroli, Giacomo Rizzello, Maria Grazia De Marinis, and Vincenzo Denaro. 2023. "The Impact of Preoperative Education on Knee and Hip Replacement: A Systematic Review" Osteology 3, no. 3: 94-112. https://doi.org/10.3390/osteology3030010
APA StyleLongo, U. G., De Salvatore, S., Rosati, C., Pisani, I., Ceccaroli, A., Rizzello, G., De Marinis, M. G., & Denaro, V. (2023). The Impact of Preoperative Education on Knee and Hip Replacement: A Systematic Review. Osteology, 3(3), 94-112. https://doi.org/10.3390/osteology3030010









