Awareness, Cultural Beliefs, and Health-Seeking Behavior of Females in Cancer Screening: A Pilot Study in Rural South Africa
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Population
Eligibility Criteria: Inclusion and Exclusion Criteria
2.2. Sample Size Calculation
2.3. Data Collection, Management, and Analysis
2.3.1. Validity and Reliability
2.3.2. Ethical Considerations
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of the Study Population
3.2. Reproductive Characteristics of Study Participants Residing in Lutubeni
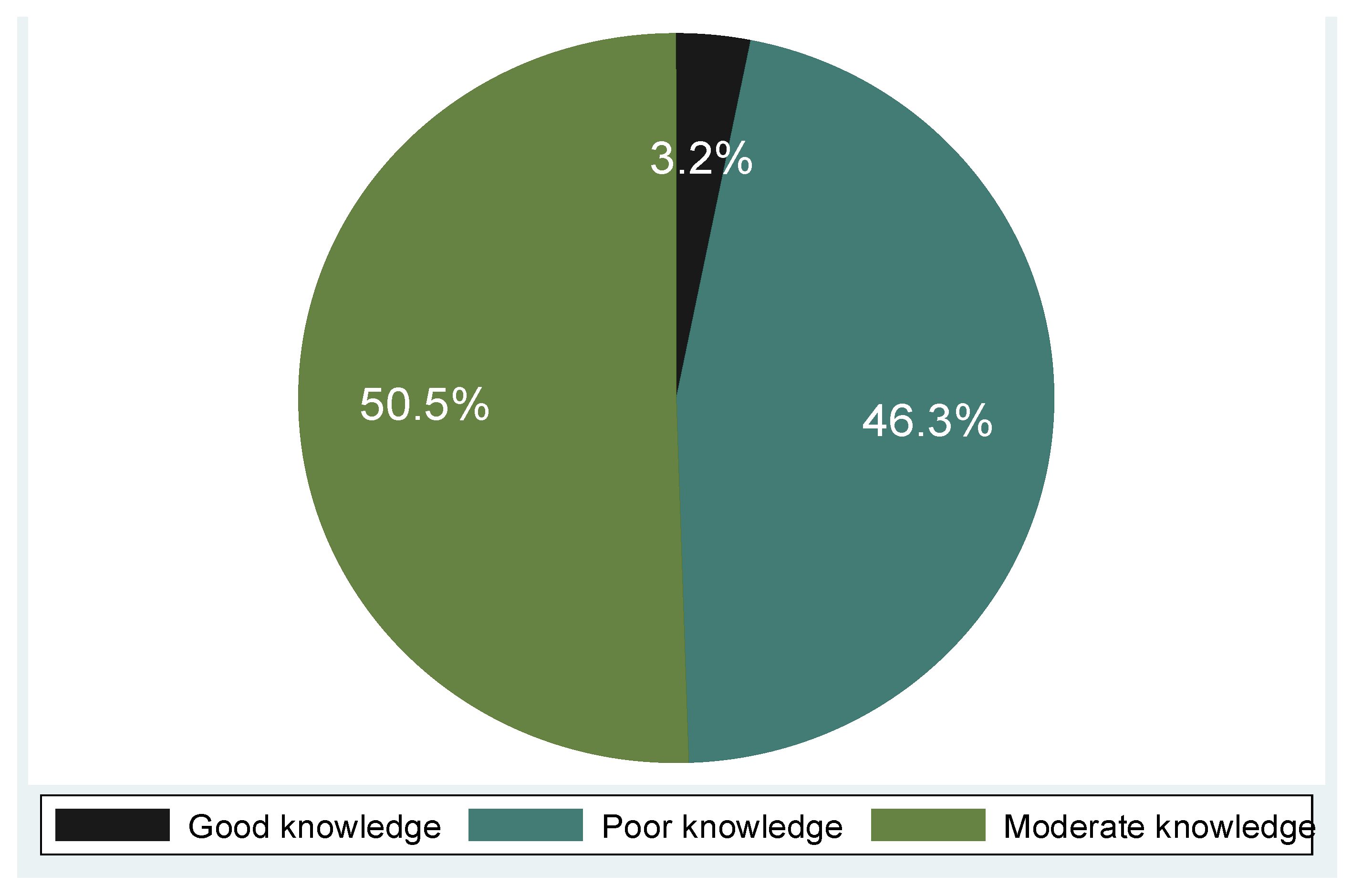
3.3. Knowledge Level About Cervical Cancer and Screening Among the Participants
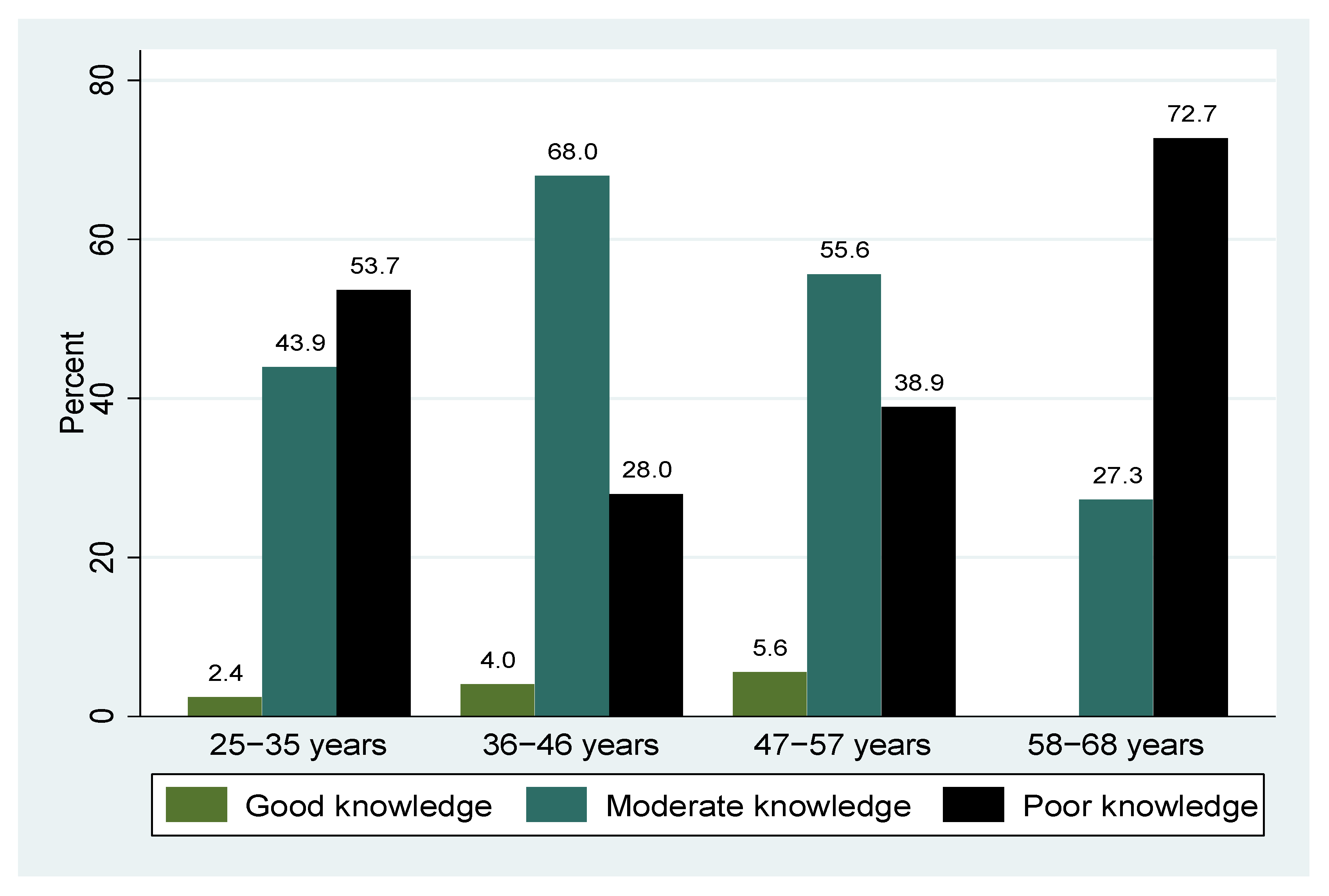
3.4. Overall Knowledge Level and Age Group of the 95 Participants from the Lutubeni Community
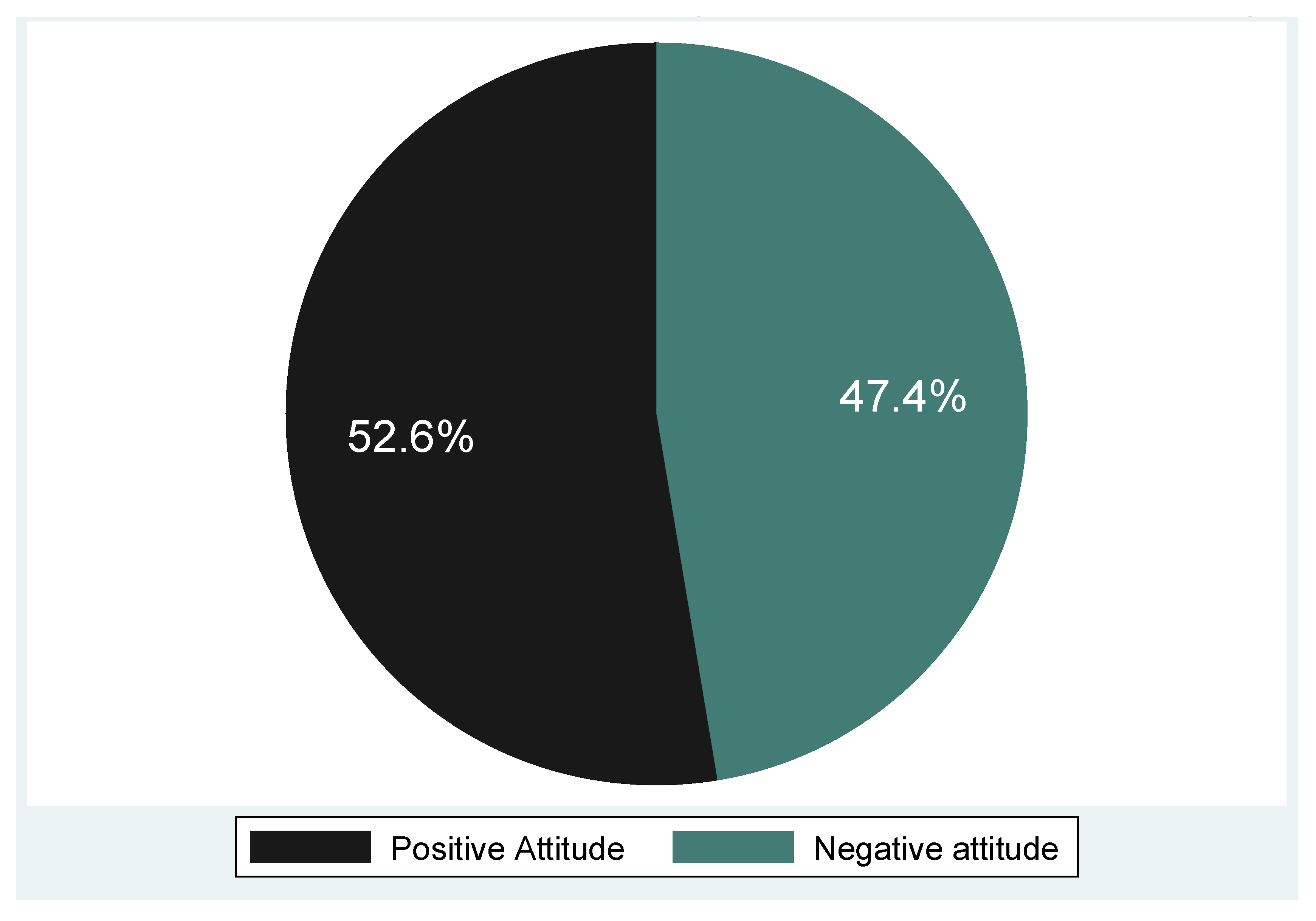
3.5. Attitude of the Participants Towards Cervical Cancer Screening
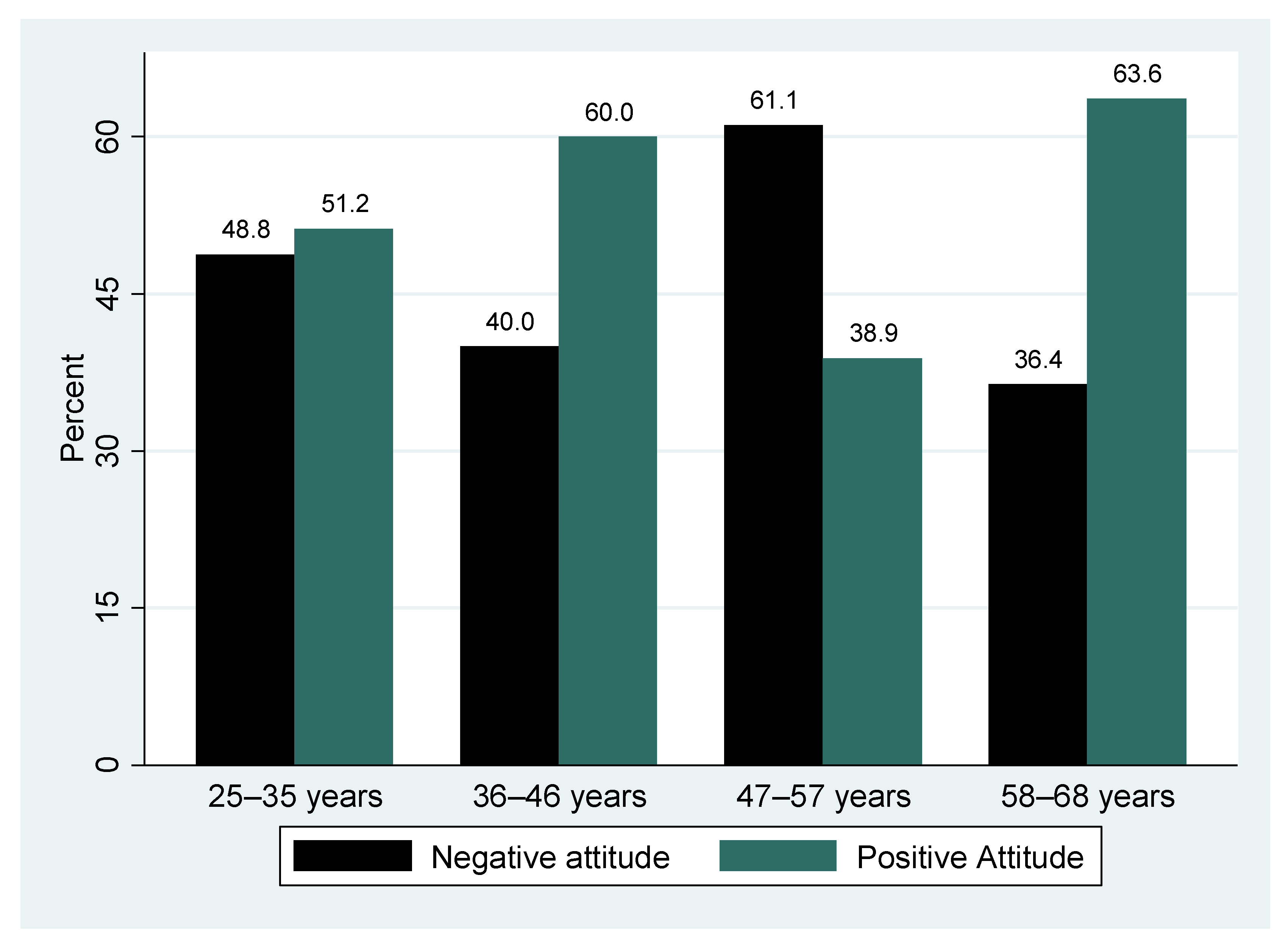
3.6. Overall Attitudes Scores and Age-Stratified Attitudes of Participants
3.7. Cultural Views Regarding Cervical Cancer Among Study Participants
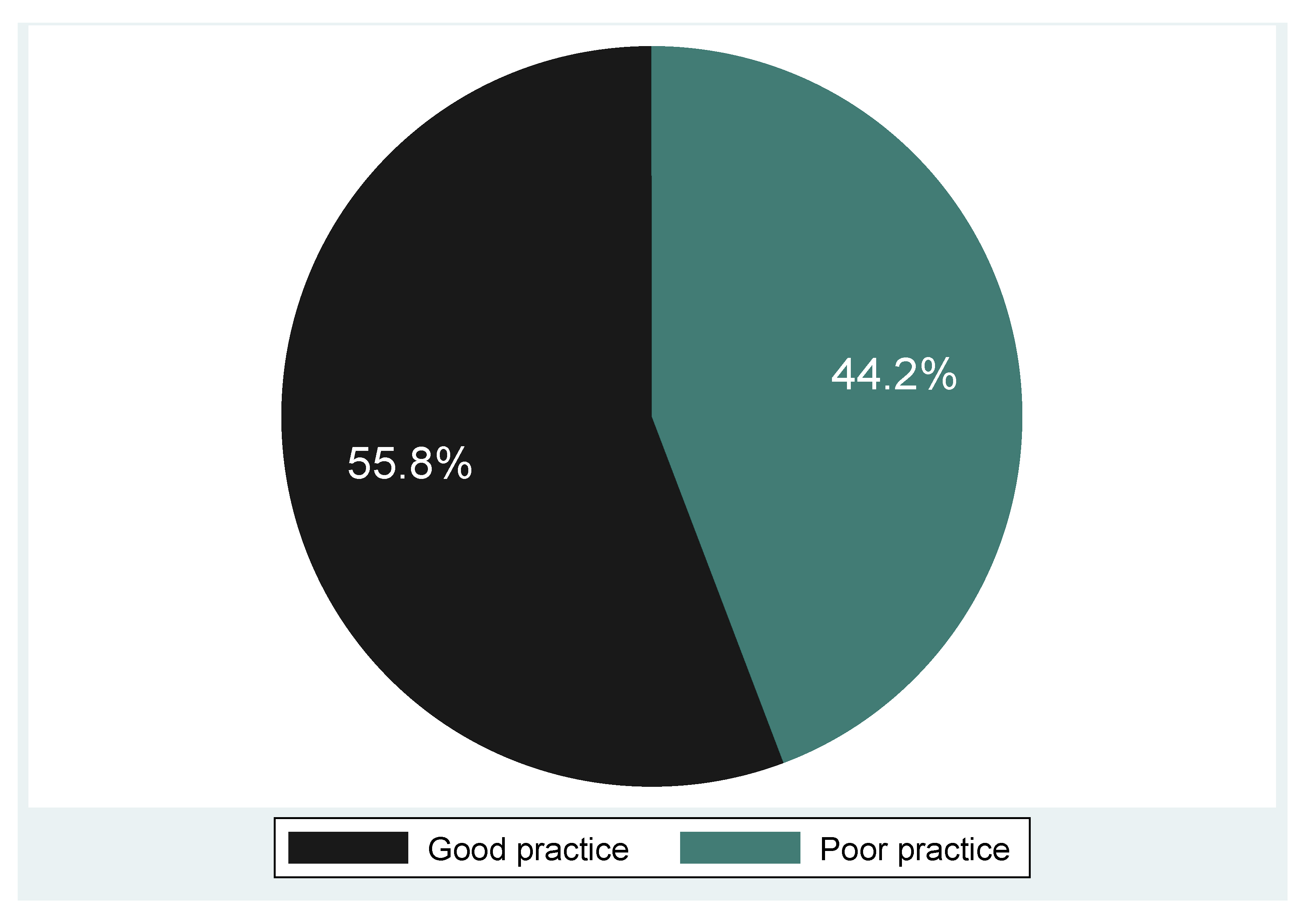
3.8. Cervical Screening Practice and Cervical Screening Experiences of the Participants
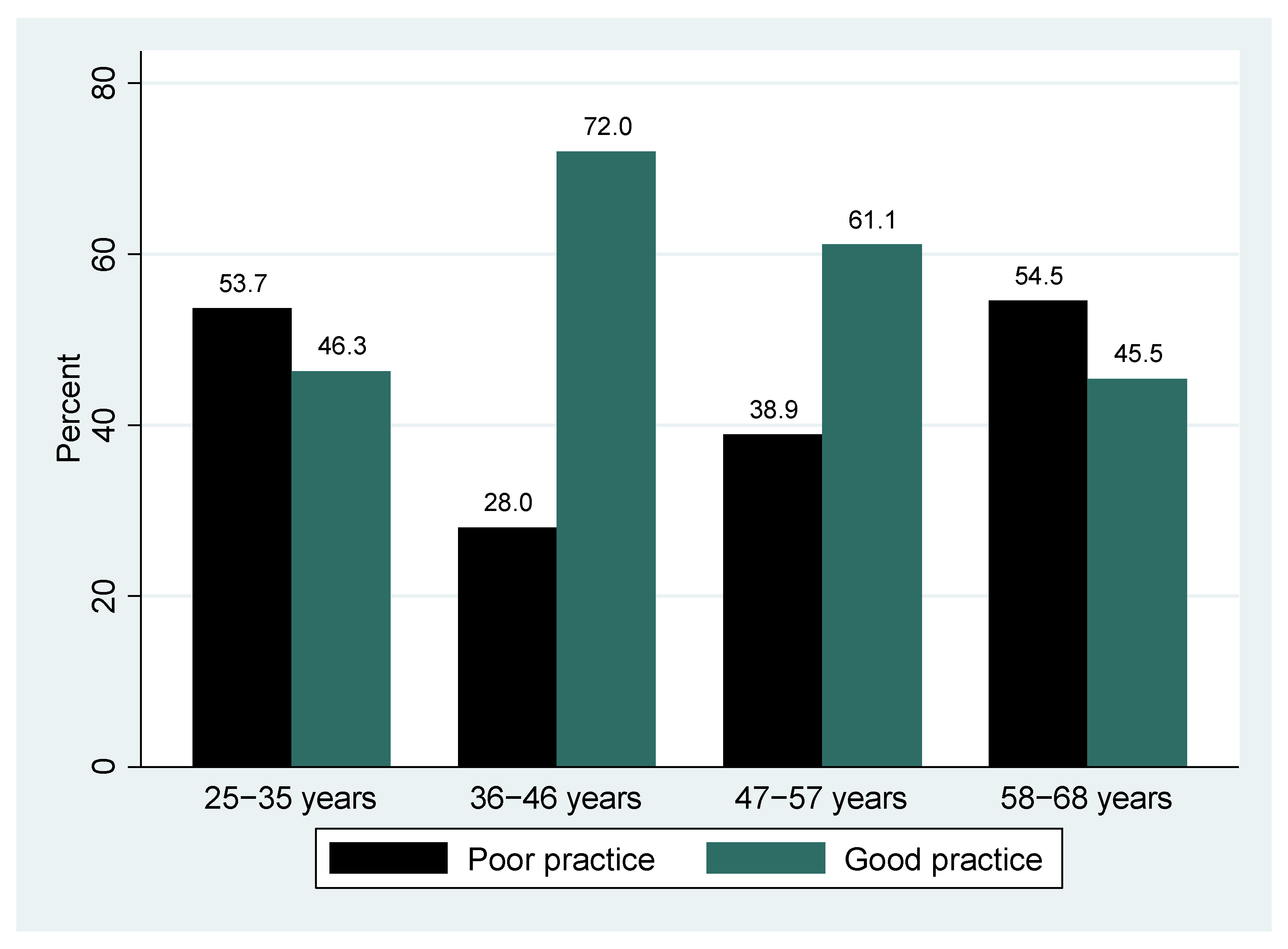
3.9. Age Group by Cervical Cancer Screening Practice
3.10. Factors Associated with Practice Towards Cervical Cancer Screening
3.11. Independent Factors Associated with Poor Screening Practice
4. Discussion
4.1. Limitations
4.2. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SSA | Sub-Saharan Africa |
| OR | Odd Ratio |
| COBES | Community-Based Education and Service |
| LMIC | Low- Middle Income Country |
| HPV | Human papillomavirus |
| VIA | Visual inspection with acetic acid |
| HIV | Human immunodeficiency virus |
| STI | Sexually transmitted infections |
| HIC | High-income countries |
| WHO | World Health Organization |
| hrHPV | High-risk Human papillomavirus |
| ASRS | Age-standardized relative survival |
References
- Mengesha, A.; Messele, A.; Beletew, B. Knowledge and attitude towards cervical cancer among reproductive age group women in Gondar town, North West Ethiopia. BMC Public Health 2020, 20, 209. [Google Scholar] [CrossRef]
- World Health Organization Cervical Cancer 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (accessed on 28 July 2025).
- Gutusa, F.; Roets, L. Early cervical cancer screening: The influence of culture and religion. Afr. J. Prim. Health Care Fam. Med. 2023, 15, a3776. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Jin, Q.; Zhang, Y.; Ji, Y.; Li, J.; Liu, X.; Duan, H.; Feng, Z.; Liu, Y.; Zhang, Y.; et al. Global burden of cervical cancer: Current estimates, temporal trend and future projections based on the GLOBOCAN 2022. J. Natl. Cancer Cent. 2025, 5, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Caruso, G.; Wagar, M.K.; Hsu, H.C.; Hoegl, J.; Valzacchi, G.M.R.; Fernandes, A.; Cucinella, G.; Aker, S.S.; Jayraj, A.S.; Mauro, J.; et al. Cervical cancer: A new era. Int. J. Gynecol. Cancer 2024, 34, 1946–1970. [Google Scholar] [CrossRef] [PubMed]
- Mutambara, J.; Mutandwa, P.; Mahapa, M.; Chirasha, V.; Nkiwane, S.; Shangahaidonhi, T. Knowledge, attitudes and practices of cervical cancer screening among women who attend traditional churches in Zimbabwe. J. Cancer Res. Pr. 2017, 4, 53–58. [Google Scholar] [CrossRef]
- Uchendu, I.; Hewitt-Taylor, J.; Turner-Wilson, A.; Nwakasi, C. Knowledge, attitudes, and perceptions about cervical cancer, and the uptake of cervical cancer screening in Nigeria: An integrative review. Sci. Afr. 2021, 14, e01013. [Google Scholar] [CrossRef]
- Li, Z.; Liu, P.; Yin, A.; Zhang, B.; Xu, J.; Chen, Z.; Zhang, Z.; Zhang, Y.; Wang, S.; Tang, L.; et al. Global landscape of cervical cancer incidence and mortality in 2022 and predictions to 2030: The urgent need to address inequalities in cervical cancer. Int. J. Cancer 2025, 157, 288–297. [Google Scholar] [CrossRef]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef]
- Kussia, B.; Shewangizaw, M.; Abebe, S.; Alemu, H.; Simon, T. Health care seeking behaviour towards cervical cancer screening among women aged 30–49 years in Arbaminch town, Southern Ethiopia, 2023. BMC Cancer 2024, 24, 38. [Google Scholar] [CrossRef]
- Habtu, Y.; Yohannes, S.; Laelago, T. Health seeking behavior and its determinants for cervical cancer among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: Community based cross sectional study. BMC Cancer 2018, 18, 298. [Google Scholar] [CrossRef]
- Moodley, J.; Constant, D.; Mwaka, A.D.; Scott, S.E.; Walter, F.M. Anticipated help seeking behaviour and barriers to seeking care for possible breast and cervical cancer symptoms in Uganda and South Africa. Ecancermedicalscience 2021, 15, 1171. [Google Scholar] [CrossRef]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020; p. 20182020. [Google Scholar]
- Ramaliba, T.M.; Sithole, N.; Ncinitwa, A. Cancer incidence in selected municipalities of the Eastern Cape Province, 2013–2017. In Eastern Cape Cancer Registry Technical Report; South African Medical Research Council: Cape Town, South Africa, 2020. [Google Scholar]
- Jassim, G.; Obeid, A.; Al Nasheet, H.A. Knowledge, attitudes, and practices regarding cervical cancer and screening among women visiting primary health care Centres in Bahrain. BMC Public Health 2018, 18, 128. [Google Scholar] [CrossRef]
- Chitha, W.; Sibulawa, S.; Funani, I.; Swartbooi, B.; Maake, K.; Hellebo, A.; Hongoro, D.; Mnyaka, O.R.; Ngcobo, Z.; Zungu, C.M.; et al. A cross-sectional study of knowledge, attitudes, barriers and practices of cervical cancer screening among nurses in selected hospitals in the Eastern Cape Province, South Africa. BMC Women’s Health 2023, 23, 94. [Google Scholar] [CrossRef]
- Mwaka, A.D.; Orach, C.G.; Were, E.M.; Lyratzopoulos, G.; Wabinga, H.; Roland, M. Awareness of cervical cancer risk factors and symptoms: Cross-sectional community survey in post-conflict northern Uganda. Health Expect. 2016, 19, 854–867. [Google Scholar] [CrossRef]
- Tapera, R.; Manyala, E.; Erick, P.; Maswabi, T.M.; Tumoyagae, T.; Mbongwe, B.; Letsholo, B. Knowledge and attitudes towards cervical cancer screening amongst University of Botswana female students. Asian Pac. J Cancer Prev. 2017, 18, 2445–2450. [Google Scholar] [CrossRef]
- Anyolo, E.; Amakali, K.; Amukugo, H.J. Attitudes of women towards screening, prevention and treatment of cervical cancer in Namibia. Health SA Gesondheid 2024, 29, 9. [Google Scholar] [CrossRef] [PubMed]
- Akokuwebe, M.E.; Idemudia, E.S.; Lekulo, A.M.; Motlogeloa, O.W. Determinants and levels of cervical cancer screening uptake among women of reproductive age in South Africa: Evidence from South Africa Demographic and health survey data, 2016. BMC Public Health 2021, 21, 2013. [Google Scholar] [CrossRef]
- Moeti, C. How Socio-Cultural Factors Affect Cervical Cancer Screening Adherence and Treatment in Disadvantaged Communities in the Greater Cape Town, South Africa; Unpublished Student Thesis; The University of Pretoria: Pretoria, South Africa, 2014. [Google Scholar]
- Tekle, T.; Wolka, E.; Nega, B.; Kumma, W.P.; Koyira, M.M. Knowledge, Attitude and Practice Towards Cervical Cancer Screening Among Women and Associated Factors in Hospitals of Wolaita Zone, Southern Ethiopia. Cancer Manag. Res. 2020, 12, 993–1005. [Google Scholar] [CrossRef] [PubMed]
- Ashebir, W.; Yimer, B.; Alle, A.; Teshome, M.; Teka, Y.; Wolde, A. Knowledge, attitude, practice, and factors associated with prevention practice towards COVID-19 among healthcare providers in Amhara region, northern Ethiopia: A multicenter cross-sectional study. PLoS Glob. Public Health 2022, 2, e0000171. [Google Scholar] [CrossRef] [PubMed]
- Aredo, M.A.; Sendo, E.G.; Deressa, J.T. Knowledge of Cervical Cancer Screening and Associated Factors among Women Attending Maternal Health Services at Aira Hospital, West Wollega, Ethiopia. SAGE Open Med. 2021, 9, 20503121211047063. [Google Scholar] [CrossRef]
- Osei, E.A.; Appiah, S.; Gaogli, J.E.; Oti-Boadi, E. Knowledge on Cervical Cancer Screening and Vaccination among Females at Oyibi Community. BMC Women’s Health 2021, 21, 148. [Google Scholar] [CrossRef]
- Mbaluka, J.H.M. Utilization of Cervical Cancer Screening Services Among Women Aged 30–49 Years in Kitui County, Kenya. Ph.D. Dissertation, Kenyatta University, Nairobi, Kenya, 2020. [Google Scholar]
- Ncane, Z.; Faleni, M.; Pulido-Estrada, G.; Apalata, T.R.; Mabunda, S.A.; Chitha, W.; Nomatshila, S.C. Knowledge on Cervical Cancer Services and Associated Risk Factors by Health Workers in the Eastern Cape Province. Healthcare 2023, 11, 325. [Google Scholar] [CrossRef] [PubMed]
- Tiiti, T.A.; Bogers, J.; Lebelo, R.L. Knowledge of Human Papillomavirus and Cervical Cancer among Women Attending Gynecology Clinics in Pretoria, South Africa. Int. J. Environ. Res. Public Health 2022, 19, 4210. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Narayan, N.; Sinha, R.; Sinha, P.; Sinha, V.P.; Upadhye, J.J. Awareness about Cervical Cancer Risk Factors and Symptoms. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018, 7, 4987–4991. [Google Scholar] [CrossRef]
- Mian, D.B.; Koffi, S.V.; Nsahlai, C.J.; Adjoby, R.; Gbary, E.; N’gUessan, K.; Boni, S. Knowledge, Attitudes and Behaviors of Clients Regarding Cervical Cancer Screening at Gynecology Consultations of the University Hospital of Cocody. J. Obstet. Gynecol. India 2023, 73 (Suppl. S1), 166–171. [Google Scholar] [CrossRef] [PubMed]
- Ken-Amoah, S.; Mensah, L.B.B.; Eliason, S.; Anane-Fenin, B.; Agbeno, E.K.; Essuman, M.A.; Essien-Baidoo, S. Poor Knowledge and Awareness of Human Papillomavirus and Cervical Cancer among Adult Females in Rural Ghana. Front. Trop. Dis. 2022, 3, 971266. [Google Scholar] [CrossRef]
- Mantula, F.; Toefy, Y.; Sewram, V. Barriers to Cervical Cancer Screening in Africa: A Systematic Review. BMC Public Health 2024, 24, 525. [Google Scholar] [CrossRef]
- Munthali, A.C.; Ngwira, B.M.; Taulo, F. Exploring Barriers to the Delivery of Cervical Cancer Screening and Early Treatment Services in Malawi: Some Views from Service Providers. Patient Prefer. Adherence 2015, 9, 501–508. [Google Scholar] [CrossRef]
- Dzobo, M.; Dzinamarira, T. Effective Cervical Cancer Prevention in Sub-Saharan Africa Needs the Inclusion of Men as Key Stakeholders. Front. Oncol. 2025, 15, 1509685. [Google Scholar] [CrossRef]
- Mafiana, J.J.; Dhital, S.; Halabia, M.; Wang, X. Barriers to uptake of cervical cancer screening among women in Nigeria: A systematic review. Afr. Health Sci. 2022, 22, 295–309. [Google Scholar] [CrossRef]
- Yosef, T.; Birhanu, B.; Shifera, N.; Bekele, B.B.; Asefa, A. Determinants of cervical cancer screening uptake among reproductive-age women in southwest Ethiopia: A case-control study. Front. Oncol. 2024, 14, 1424810. [Google Scholar] [CrossRef]
- Lemlem, S.B.; Gary, R.A.; Yeager, K.A.; Sisay, M.M.; Higgins, M.K. Psychometric properties of a modified health belief model for cervical cancer and visual inspection with acetic acid among healthcare professionals in Ethiopia. PLoS ONE 2024, 19, e0295905. [Google Scholar] [CrossRef]
- Xin, T.; Jiang, Y.; Li, C.; Ding, X.; Zhu, Z.; Chen, X. Using planned behavior theory to understand cervical cancer screening intentions in Chinese women. Front. Public Health 2023, 11, 1063694. [Google Scholar] [CrossRef]
- Mirzaei-Alavijeh, M.; Amini, M.; Moradinazar, M.; Eivazi, M.; Jalilian, F. Disparity in cognitive factors related to cancer screening uptake based on the theory of planned behavior. BMC Cancer 2024, 24, 845. [Google Scholar] [CrossRef]
- Dzobo, M.; Dzinamarira, T.; Jaya, Z.; Kgarosi, K.; Mashamba-Thompson, T. Experiences and Perspectives Regarding Human Papillomavirus Self-Sampling in Sub-Saharan Africa: A Systematic Review of Qualitative Evidence. Heliyon 2024, 10, e32926. [Google Scholar] [CrossRef]
- Shahnazi, H.; Ahmadi-Livani, M.; Pahlavanzadeh, B.; Rajabi, A.; Hamrah, M.S.; Charkazi, A. Assessing Preventive Health Behaviors from COVID-19: A Cross Sectional Study with Health Belief Model in Golestan Province, Northern of Iran. Infect. Dis. Poverty 2020, 9, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Srinath, A.; van Merode, F.; Rao, S.V.; Pavlova, M. Barriers to Cervical Cancer and Breast Cancer Screening Uptake in Low- and Middle-Income Countries: A Systematic Review. Health Policy Plan. 2023, 38, 509–527. [Google Scholar] [CrossRef] [PubMed]
- Farajimakin, O. Barriers to Cervical Cancer Screening: A Systematic Review. Cureus 2024, 16, e65555. [Google Scholar] [CrossRef]
- Mengistie, B.A.; Melese, M.; Gebiru, A.M.; Getnet, M.; Getahun, A.B.; Tassew, W.C.; Tilahun, M.M.; Bizuneh, Y.B.; Negash, H.K.; Baykemagn, N.D.; et al. Uptake of Cervical Cancer Screening and Its Determinants in Africa: Umbrella Review. PLoS ONE 2025, 20, e0328103. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, S.; Yang, X.; Chen, M.; Ren, W.; Bao, Y.; Qiao, Y. Knowledge, Willingness, Uptake and Barriers of Cervical Cancer Screening Services among Chinese Adult Females: A National Cross-Sectional Survey Based on a Large E-Commerce Platform. BMC Women’s Health 2023, 23, 435. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Liu, C.; Wei, Y.; Zhang, Q.; Ma, J. Impact of the WHO’s 90-70-90 Strategy on HPV-Related Cervical Cancer Control: A Mathematical Model Evaluation in China. arXiv 2025, arXiv:2506.06405. [Google Scholar]
- Harder, M.T.; Mokete, M.; Chammartin, F.; Lerotholi, M.; Motaboli, L.; Kopo, M.; Kao, M.; Mokebe, M.; Chejane, N.; Mahlatsi, P.; et al. Cervical Cancer Screening Delay and Associated Factors Among Women with HIV in Lesotho: A Mixed-Methods Study. BMC Women’s Health 2024, 24, 543. [Google Scholar] [CrossRef] [PubMed]
| Variable | Category | Frequency (n = 95) | Percentage (%) |
|---|---|---|---|
| Age groups | 25–35 years | 41 | 43.2 |
| 36–46 years | 25 | 26.3 | |
| 47–57 years | 18 | 18.9 | |
| 58–68 years | 11 | 11.6 | |
| Median (IQR): 39 (30–48) years; Min–Max: 25–68 years | |||
| Religion | Christianity | 90 | 94.7 |
| African spirituality | 3 | 3.2 | |
| Zion | 2 | 2.1 | |
| Marital status | Single | 40 | 42.1 |
| Married | 39 | 41.1 | |
| Widowed | 6 | 6.3 | |
| Divorced | 3 | 3.2 | |
| Cohabitation | 2 | 2.1 | |
| Separated | 1 | 1.1 | |
| Decline | 4 | 4.2 | |
| Education Status | Secondary school | 40 | 42.1 |
| Associate degree | 16 | 16.8 | |
| Primary school | 16 | 16.8 | |
| No formal education | 12 | 12.6 | |
| Associate degree /Degree | 8 | 8.4 | |
| Bachelor’s Degree | 3 | 3.2 | |
| Occupation | Unemployed | 29 | 30.5 |
| House wife | 25 | 26.3 | |
| Government | 24 | 25.3 | |
| Self-employed | 11 | 11.6 | |
| Student | 6 | 6.3 | |
| Monthly Income | R < 2000 | 57 | 60.0 |
| R > 2000 | 34 | 35.8 | |
| Sexual Orientation | Heterosexual | 94 | 98.9 |
| Homosexual | 1 | 1.1 | |
| Variable | Category | Frequency (n = 95) | Percentage (%) |
|---|---|---|---|
| Ever had Sex | Yes | 94 | 98.9 |
| No | 1 | 1.1 | |
| Age of First Sex (Years) | 15–18 years | 49 | 51.6 |
| >18 years | 37 | 38.9 | |
| <15 years | 7 | 7.4 | |
| Median (IQR):18 (16–21) years; Min–Max: 10–30 years | |||
| History of Casual Sex | No | 51 | 53.7 |
| Yes | 43 | 45.3 | |
| Never had sex | 1 | 1.1 | |
| Use of Contraceptive pills or injections | Yes | 75 | 78.9 |
| No | 19 | 20.0 | |
| Never had sex | 1 | 1.1 | |
| Duration of Using Oral Contraceptives | 5–9 years | 38 | 40.0 |
| ≥10 years | 20 | 21.1 | |
| <5 years | 16 | 16.8 | |
| Median (IQR): 7 (5–10) years; Min–Max: 1–20 years) | |||
| My mother had cervical cancer | No | 93 | 97.9 |
| Yes | 2 | 2.1 | |
| History of Condom | Yes | 72 | 75.8 |
| No | 22 | 23.2 | |
| Never had sex | 1 | 1.1 | |
| History of Cigarette Smoking | No | 83 | 87.4 |
| Yes | 12 | 12.6 | |
| History of Alcohol Consumption | No | 51 | 53.7 |
| Yes | 44 | 46.3 | |
| Knowledge of Cervical Cancer | Response n (%), n = 95 | |
|---|---|---|
| Yes | No | |
| Knowledge of symptoms of cervical cancer: Poor knowledge 45 (47.4%), Moderate knowledge 27 (28.4%), Good knowledge 23 (24.2%) | ||
| Vaginal bleeding | 57 (60%) | 38 (40%) |
| Vaginal foul-smelling discharges | 48 (50.5%) | 47 (47.9%) |
| Pain during sex | 43 (45.35) | 52 (54.7%) |
| Knowledge related to the risk factor of Cervical cancer: Poor knowledge 58 (61.1%), Moderate knowledge 26 (27.4%), Good knowledge 11 (11.6%) | ||
| Acquiring HPV | 23 (24.2%) | 72 (75. 8%) |
| Multiple sex partners | 45 (47.4%) | 50 (52.6%) |
| Multi parity | 26 (27.4%) | 69 (72.6%) |
| Early sexual intercourse | 29 (30.5%) | 66 (69.5%) |
| Long-term oral contraceptive use | 30 (31.6%) | 65 (68.4%) |
| Cigarette smoking | 39 (41.1%) | 56 (58.9%) |
| Do not know the risk factors | 31 (32.6%) | 64 (67.4%) |
| Knowledge related to prevention: Poor knowledge 52 (54.7%), Moderate knowledge 4 (4.2%), Good knowledge 39 (41.1%) | ||
| Vaccination for HPV | 38 (40%) | 57 (60%) |
| Avoid multiple sexual partners | 61 (64.2%) | 34 (35. 8%) |
| Avoid long-term use of oral contraceptives | 40 (42.1%) | 55 (57.9%) |
| Early screening | 65 (68.4%) | 30 (31.6%) |
| No smoking | 44 (46.3%) | 51 (53.7%) |
| Do not know the prevention | 14 (14.7%) | 81 (85.3%) |
| Knowledge related to the treatment of cervical cancer: Poor knowledge 42 (44.2%), Moderate knowledge 41 (43.2%), Good knowledge 12 (12.6%) | ||
| Surgery | 68 (71.6%) | 27 (28.4%) |
| Chemotherapy | 57 (60%) | 38 (40%) |
| Radiotherapy | 15 (15. 8%) | 80 (84.2%) |
| Do not know | 20 (21.1%) | 75 (78.9%) |
| Knowledge of cervical cancer screening: Poor knowledge 8 (8.4%), Moderate knowledge 4 (4.2%), Good knowledge 83 (87.4%) | ||
| Is there screening for cervical cancer | 86 (90.5%) | 9 (9.5%) |
| Screening service is available at the local clinic | 84 (88.4%) | 11 (11.6%) |
| Knowledge related to screening interval: Poor knowledge 66 (69.5%), Moderate knowledge 27 (28.4%), Good knowledge 2 (2.1%) | ||
| Every year | 31 (32.6%) | 64 (67.4%) |
| Every three years | 22 (23.2%) | 73 (76.8%) |
| Every five years | 12 (12.6%) | 83 (87.4%) |
| Do not know | 28 (29.5%) | 67 (70.5%) |
| Knowledge related to screening eligibility: Poor knowledge 48 (50.5%), Moderate knowledge 28 (29.5%), Good knowledge 19 (20.0%) | ||
| Women 30 years of age and older | 58 (61.1%) | 37 (38.9%) |
| Prostitute | 47 (45.5%) | 48 (50.5%) |
| Elderly women | 44 (46.3%) | 51 (53.7%) |
| Do not know | 21 (22.1%) | 74 (77.9%) |
| Knowledge related to cervical cancer screening procedures | ||
| VIA | 1 (1.1%) | 94 (98.9%) |
| PAP smear | 84 (88.4%) | 11 (11.6%) |
| Do not know | 11 (11.6%) | 84 (88.4%) |
| Composite Knowledge score | ||
| Poor Knowledge | 44 (46.3%) | |
| Good knowledge | 3 (3.2%) | |
| Moderate knowledge | 48 (50.5%) | |
| Age Group (Years) | WHO Target (≥70%) | Study Coverage (%) | Shortfall vs. Target |
|---|---|---|---|
| 25–35 | 70 | 46.3 | −23.7 |
| 36–46 | 70 | 72.0 | +2.0 (met target) |
| 47–57 | 70 | 61.1 | −8.9 |
| 58–68 | 70 | 45.5 | −24.5 |
| Variables Used to Measure Attitude | SA | A | NADA | DA |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Cervical cancer is a highly prevalent disease among women in South Africa | 64 (67.4) | 20 (21.1) | 6 (6.3) | 5 (5.3) |
| Cervical cancer is the leading cause of cancer-related death among women in South Africa | 30 (31.6) | 38 (40.0) | 14 (14.7) | 13 (13.7) |
| Any adult woman, including you, can acquire cervical cancer | 35 (36.8) | 41 (43.2) | 16 (16.8) | 3 (3.2) |
| Cervical cancer cannot be transmitted from one person to another | 26 (27.4) | 44 (46.3) | 13 (13.7) | 12 (12.6) |
| Screening helps in the prevention of cervical cancer | 29 (30.5) | 48 (50.5) | 12 (12.6) | 6 (6.3) |
| Screening causes no harm to the client | 30 (31.6) | 37 (38.9) | 17 (17.9) | 11 (11.6) |
| Variables of Interest | True n (%) | False n (%) |
|---|---|---|
| Sexual organs are not a topic for discussion | 84 (88.4) | 11 (11.6) |
| A diagnosis with cervical cancer is associated with death | 28 (29.5) | 67 (70.5) |
| A diagnosis of cervical cancer means you are having multiple sexual partners | 16 (16.8) | 79 (83.2) |
| A diagnosis of cervical cancer means you are promiscuous | 18 (18.9) | 77 (81.1) |
| Fear of cervical cancer | 21 (22.1) | 74 (77.9) |
| Cervical cancer is perceived to be caused by indecent behavior | 31 (32.6) | 64 (67.4) |
| Need approval from the partner for cervical cancer screening | 11 (11.6) | 84 (88.4) |
| Cultural views around cervical cancer screening influence my decision to screen | 7 (7.4) | 88 (92.6) |
| Traditional medicines are the primary healthcare-seeking option | 11 (11.6) | 84 (88.4) |
| Views around cervical cancer screening are the primary reason why I have never been screened for cervical cancer | 4 (4.2) | 91 (95.8) |
| One’s sexual organs are private and not supposed to be exposed or touched | 87 (91.6) | 8 (8.4) |
| Variable | Category | Frequency (n = 95) | Percent (%) |
|---|---|---|---|
| Have you ever been screened for cervical cancer | Yes | 53 | 55.8 |
| No | 42 | 44.2 | |
| Where did you screen | Never screened | 42 | 44.2 |
| Clinic | 32 | 33.7 | |
| Hospital | 20 | 21.1 | |
| Others | 1 | 1.1 | |
| How many times did you screen | Once | 41 | 43.2 |
| Twice | 8 | 8.4 | |
| Thrice | 2 | 2.1 | |
| Four times | 1 | 1.1 | |
| Five times | 1 | 1.1 | |
| When was the last time you screened | Last year | 28 | 29.4 |
| >3 years | 12 | 12.6 | |
| Within the past 3 years | 9 | 9.5 | |
| <3 years | 4 | 4.2 | |
| Who initiated you to be screened | Health professional | 39 | 41.1 |
| Self-initiated | 13 | 13.7 | |
| Others | 1 | 1.1 | |
| Have you ever made use of reproductive health services, like HIV or STI testing | Yes | 88 | 92.6 |
| No | 7 | 7.4 |
| Associate Factors | Cervical Cancer Screening Practice | X2 p-Value | |
|---|---|---|---|
| Poor Practice (N = 42) | Good Practice (N = 53) | ||
| Educational status | 0.047 * | ||
| Bachelor’s Degree | 1 (33.3) | 2 (66.7) | |
| Associate degree | 3 (18.8) | 13 (81.2) | |
| Associate degree/Degree | 1 (12.5) | 7 (87.5) | |
| No formal education | 7 (58.3) | 5 (41.7) | |
| Primary school | 9 (56.2) | 7 (43.8) | |
| Secondary | 21 (52.5) | 19 (47.5) | |
| Knowledge of the symptoms of cervical cancer | 0.04 | ||
| Good | 7 (30.4) | 16 (69.6) | |
| Moderate | 9 (33.3) | 18 (66.7) | |
| Poor | 26 (57.8) | 19 (42.2) | |
| Knowledge related to the risk factor of Cervical cancer | <0.0001 * | ||
| Good | 1 (9.1) | 10 (90.9) | |
| Moderate | 5 (19.2) | 21 (80.8) | |
| Poor | 36 (62.1) | 22 (37.9) | |
| Knowledge related to prevention | <0.0001 * | ||
| Good | 4 (10.3) | 35 (89.7) | |
| Moderate | 2 (50.0) | 2 (50.0) | |
| Poor | 36 (69.2) | 16 (30.8) | |
| Knowledge related to the treatment of cervical cancer | 0.001 | ||
| Good | 1 (8.3) | 11 (91.7) | |
| Moderate | 14 (34.1) | 27 (65.9) | |
| Poor | 27 (64.3) | 15 (35.7) | |
| Knowledge of screening availability | <0.0001 * | ||
| Good | 31 (37.3) | 52 (62.7) | |
| Moderate | 3 (75.0) | 1 (25.0) | |
| Poor | 8 (100.0) | 0 (0.0) | |
| Knowledge related to the Cervical screening procedure | 0.002 * | ||
| Good | 0 (0.0) | 1 (100.0) | |
| Moderate | 32 (38.6) | 51 (61.4) | |
| Poor | 10 (90.9) | 1 (9.1) | |
| Composite Knowledge | <0.0001 * | ||
| Good | 0 (0.0) | 3 (100.0) | |
| Moderate | 11 (22.9) | 37 (77.1) | |
| Poor | 31 (70.5) | 13 (29.5) | |
| Attitude towards cervical cancer and screening | <0.0001 | ||
| Negative attitude | 29 (82.9) | 6 (17.1) | |
| Positive Attitude | 13 (21.7) | 47 (78.3) | |
| Independent Factors Associated with Poor Screening Practice | B | OR (95% CI) |
|---|---|---|
| Held an associate degree | −3.278 | 0.04 (0.002–0.894) |
| Good knowledge related to prevention | −3.905 | 0.02 (0.001–0.424) |
| Negative attitude towards cervical cancer and screening | 3.590 | 36.22 (2.9–453.6) |
| Model: X2 = 85.3; Nagelkerke R2 =79.3%; B = Regression coefficient, OR = Odd Ratio | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akapo, O.O.; Hosu, M.C.; Nanjoh, M.K.-K. Awareness, Cultural Beliefs, and Health-Seeking Behavior of Females in Cancer Screening: A Pilot Study in Rural South Africa. Epidemiologia 2025, 6, 90. https://doi.org/10.3390/epidemiologia6040090
Akapo OO, Hosu MC, Nanjoh MK-K. Awareness, Cultural Beliefs, and Health-Seeking Behavior of Females in Cancer Screening: A Pilot Study in Rural South Africa. Epidemiologia. 2025; 6(4):90. https://doi.org/10.3390/epidemiologia6040090
Chicago/Turabian StyleAkapo, Olufunmilayo Olukemi, Mojisola Clara Hosu, and Mirabel Kah-Keh Nanjoh. 2025. "Awareness, Cultural Beliefs, and Health-Seeking Behavior of Females in Cancer Screening: A Pilot Study in Rural South Africa" Epidemiologia 6, no. 4: 90. https://doi.org/10.3390/epidemiologia6040090
APA StyleAkapo, O. O., Hosu, M. C., & Nanjoh, M. K.-K. (2025). Awareness, Cultural Beliefs, and Health-Seeking Behavior of Females in Cancer Screening: A Pilot Study in Rural South Africa. Epidemiologia, 6(4), 90. https://doi.org/10.3390/epidemiologia6040090






