The Frequent Use of Emergency Departments Among the Pediatric Population: A Retrospective Analysis in Rome, Italy
Abstract
1. Introduction
1.1. Background
1.2. The Child Healthcare System in Italy
2. Materials and Methods
2.1. Study Design, Population, and Data Sources
- Demographic characteristics: The gender was classified as binary (male or female) according to the LHA registry; age was classified according to the age stages of the National Institute of Child Health and Human Development: “infancy” (birth to 12 months); “toddler” (13 to 24 months); “early childhood” (25 months to 5 years); “middle childhood” (6 to 12 years); and “adolescent” (12 to 15 years) [22].
- Arrival mode: Emergency Medical Services (EMS) or not EMS;
- Triage code: Color codes (1, 2, 3, 4, 5—from the most urgent to the least) [23];
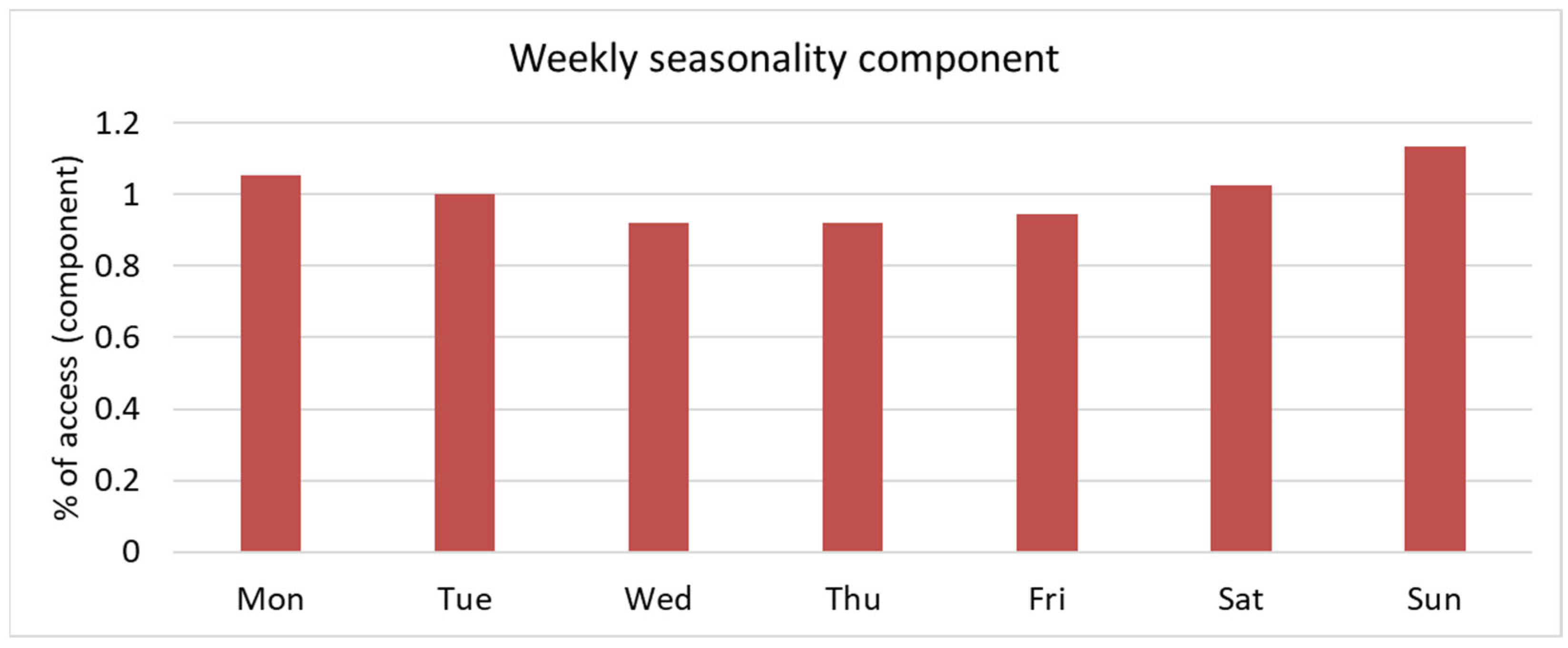
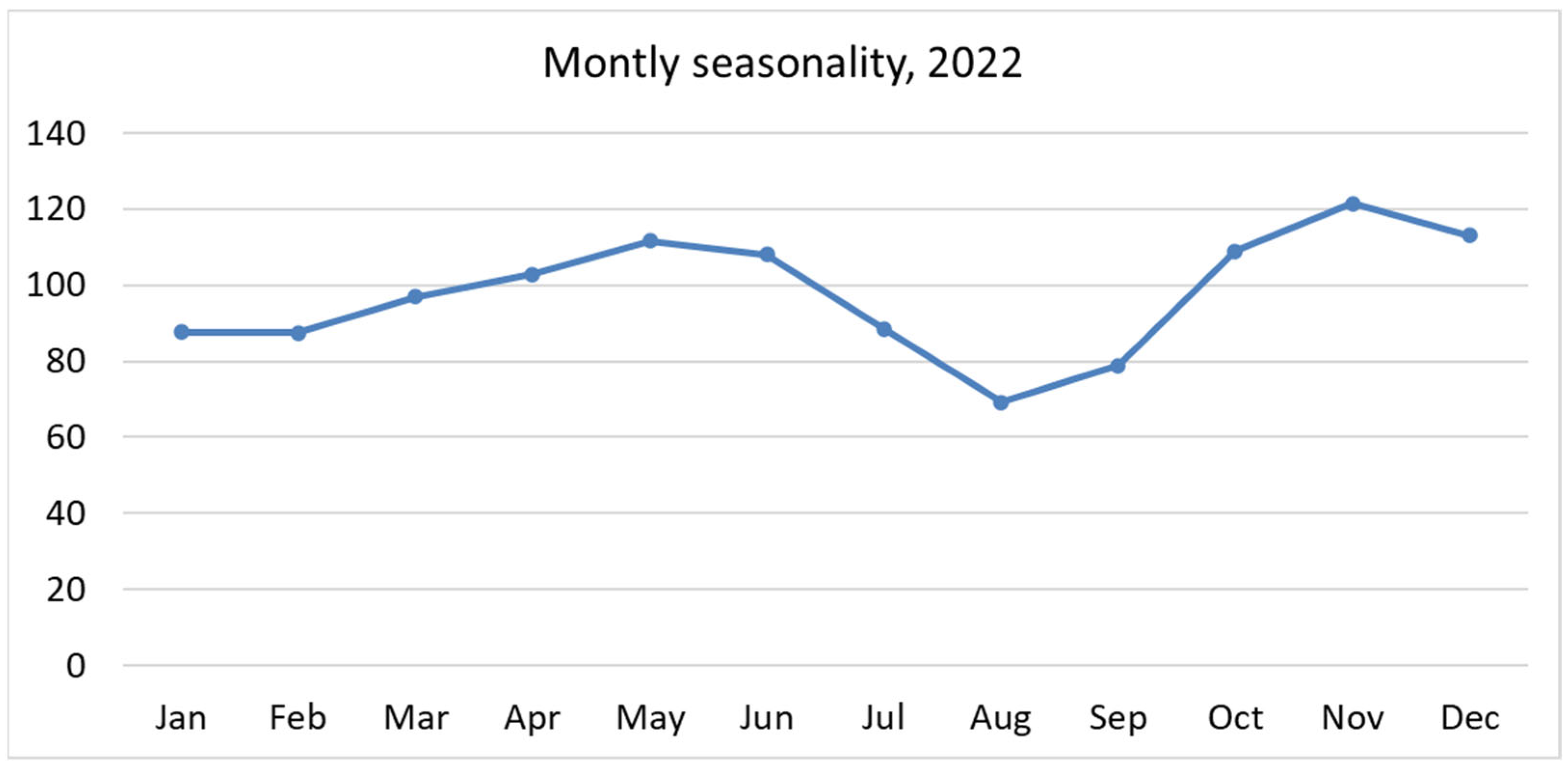
- Festivity or workday: During weekends and holidays, primary care services are not available;
- Appropriateness of attendance: According to 2019 Italian Ministry of Health’s priority code triage system, ED attendances are considered “inappropriate” when it meets one of the following criteria: triage code “white” (noncritical, nonurgent patients) or “green” (low urgency and priority) and outcome “home discharge” or “leave during medical examinations” or “leave without being seen by the physician” [5,23];
- Patient’s PCP/GP (only doctors associated with at least one patient’s access to EDs were selected);
- Patient’s LHD.
2.2. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ED | Emergency Department |
| EMS | Emergency Medical Service |
| FU | Frequent User |
| GP | General Practitioner |
| PCP | Primary Care Pediatrician |
| LHA | Local Health Authority |
| LHD | Local Health District |
| NHS | National Health Service |
References
- Alele, F.O.; Emeto, T.I.; Callander, E.J.; Watt, K. Non-urgent paediatric emergency department presentation: A systematic review. J. Paediatr. Child. Health 2019, 55, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Giannouchos, T.V.; Washburn, D.J.; Gary, J.C.; Foster, M.J. Frequent emergency department use in the paediatric population: A systematic literature review. J. Eval. Clin. Pract. 2021, 27, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, G.; Blair, M.; Aylin, P.P.; Saxena, S.; Majeed, A.; Hoffman, M.; Bottle, A. Frequent attendances at emergency departments in England. Emerg. Med. J. EMJ 2020, 37, 597–599. [Google Scholar] [CrossRef] [PubMed]
- Liguoro, I.; Beorchia, Y.; Castriotta, L.; Rosso, A.; Pedduzza, A.; Pilotto, C.; Cogo, P. Analysis of factors conditioning inappropriate visits in a paediatric emergency department. Eur. J. Pediatr. 2023, 182, 5427–5437. [Google Scholar] [CrossRef]
- Vedovetto, A.; Soriani, N.; Merlo, E.; Gregori, D. The burden of inappropriate emergency department pediatric visits: Why Italy needs an urgent reform. Health Serv. Res. 2014, 49, 1290–1305. [Google Scholar] [CrossRef]
- Furia, G.; Vinci, A.; Colamesta, V.; Papini, P.; Grossi, A.; Cammalleri, V.; Chierchini, P.; Maurici, M.; Damiani, G.; De Vito, C. Appropriateness of frequent use of emergency departments: A retrospective analysis in Rome, Italy. Front. Public. Health 2023, 11, 1150511. [Google Scholar] [CrossRef]
- Doan, Q.; Wong, H.; Meckler, G.; Johnson, D.; Stang, A.; Dixon, A.; Sawyer, S.; Principi, T.; Kam, A.J.; Joubert, G.; et al. The impact of pediatric emergency department crowding on patient and health care system outcomes: A multicentre cohort study. CMAJ 2019, 191, E627–E635. [Google Scholar] [CrossRef]
- Cunningham, A.; Mautner, D.; Ku, B.; Scott, K.; LaNoue, M. Frequent emergency department visitors are frequent primary care visitors and report unmet primary care needs. J. Eval. Clin. Pract. 2017, 23, 567–573. [Google Scholar] [CrossRef]
- Berry, A.; Brousseau, D.; Brotanek, J.M.; Tomany-Korman, S.; Flores, G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambul. Pediatr. 2008, 8, 360–367. [Google Scholar] [CrossRef]
- Pethe, K.; Baxterbeck, A.; Rosenthal, S.L.; Stockwell, M.S. Why Parents Use the Emergency Department Despite Having a Medical Home. Clin. Pediatr. 2019, 58, 95–99. [Google Scholar] [CrossRef]
- Bezzina, A.J.; Smith, P.B.; Cromwell, D.; Eagar, K. Primary care patients in the emergency department: Who are they? A review of the definition of the ‘primary care patient’ in the emergency department. Emerg. Med. Australas. 2005, 17, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Fieldston, E.S.; Alpern, E.R.; Nadel, F.M.; Shea, J.A.; Alessandrini, E.A. A qualitative assessment of reasons for nonurgent visits to the emergency department: Parent and health professional opinions. Pediatr. Emerg. Care 2012, 28, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Vinci, A.; Furia, G.; Cammalleri, V.; Colamesta, V.; Chierchini, P.; Corrado, O.; Mammarella, A.; Ingravalle, F.; Bardhi, D.; Malerba, R.M.; et al. Burden of delayed discharge on acute hospital medical wards: A retrospective ecological study in Rome, Italy. PLoS ONE 2024, 19, e0294785. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, G.; Okoli, O.; Quezada-Yamamoto, H.; Blair, M.; Saxena, S.; Majeed, A.; Hayhoe, B. Characteristics of frequently attending children in hospital emergency departments: A systematic review. BMJ Open 2021, 11, e051409. [Google Scholar] [CrossRef]
- Pol, A.; Biagioli, V.; Adriani, L.; Fadda, G.; Gawronski, O.; Cirulli, L.; Stelitano, R.; Federici, T.; Tiozzo, E.; Dall’oglio, I. Non-urgent presentations to the paediatric emergency department: A literature review. Emerg. Nurse 2023, 31, 35–41. [Google Scholar] [CrossRef]
- Corsello, G.; Ferrara, P.; Chiamenti, G.; Nigri, L.; Campanozzi, A.; Pettoello-Mantovani, M. The Child Health Care System in Italy. J. Pediatr. 2016, 177, S116–S126. [Google Scholar] [CrossRef]
- Sapienza, M.; Furia, G.; La Regina, D.P.; Grimaldi, V.; Tarsitano, M.G.; Patrizi, C.; Capelli, G.; Rome OMCeO Group; Magi, A.; De Lillo, S.; et al. Primary care pediatricians and job satisfaction: A cross sectional study in the Lazio region. Ital. J. Pediatr. 2023, 49, 104. [Google Scholar] [CrossRef]
- Sintesi Stato di Salute. Available online: https://www.opensalutelazio.it/salute/stato_salute.php?stato_salute (accessed on 23 April 2025).
- Poku, B.A.; Hemingway, P. Reducing repeat paediatric emergency department attendance for non-urgent care: A systematic review of the effectiveness of interventions. Emerg. Med. J. 2019, 36, 435–442. [Google Scholar] [CrossRef]
- Gibson, N.P.; Jelinek, G.A.; Jiwa, M.; Lynch, A.-M. Paediatric frequent attenders at emergency departments: A linked-data population study. J. Paediatr. Child. Health 2010, 46, 723–728. [Google Scholar] [CrossRef]
- Riva, B.; Clavenna, A.; Cartabia, M.; Bortolotti, A.; Fortino, I.; Merlino, L.; Biondi, A.; Bonati, M. Emergency department use by paediatric patients in Lombardy Region, Italy: A population study. BMJ Paediatr. Open 2018, 2, e000247. [Google Scholar] [CrossRef]
- Williams, K.; Thomson, D.; Seto, I.; Contopoulos-Ioannidis, D.G.; Ioannidis, J.P.; Curtis, S.; Constantin, E.; Batmanabane, G.; Hartling, L.; Klassen, T. Standard 6, age groups for pediatric trials. Pediatrics 2012, 129 (Suppl. S3), S153–S160. [Google Scholar] [CrossRef] [PubMed]
- Repertorio atto n. 143/CSR. Conf. Perm. Rapp. Tra Lo Stato Reg. E Prov. Auton. Trento E Bolzano. Available online: https://www.statoregioni.it/it/conferenza-stato-regioni/sedute-2019/seduta-del-01082019/atti/repertorio-atto-n-143csr (accessed on 25 April 2025).
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef] [PubMed]
- Merlo, J.; Chaix, B.; Ohlsson, H.; Beckman, A.; Johnell, K.; Hjerpe, P.; Råstam, L.; Larsen, K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health 2006, 60, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Pongiglione, B.; Torbica, A.; Gusmano, M.K. Inequalities in avoidable hospitalisation in large urban areas: Retrospective observational study in the metropolitan area of Milan. BMJ Open 2020, 10, e042424. [Google Scholar] [CrossRef]
- Bianco, A.; Pileggi, C.; Angelillo, I.F. Non-urgent visits to a hospital emergency department in Italy. Public Health 2003, 117, 250–255. [Google Scholar] [CrossRef]
- McHale, P.; Wood, S.; Hughes, K.; Bellis, M.A.; Demnitz, U.; Wyke, S. Who uses emergency departments inappropriately and when—A national cross-sectional study using a monitoring data system. BMC Med. 2013, 11, 258. [Google Scholar] [CrossRef]
- Carret, M.L.V.; Fassa, A.C.G.; Domingues, M.R. Inappropriate use of emergency services: A systematic review of prevalence and associated factors. Cad. Saude Publica 2009, 25, 7–28. [Google Scholar] [CrossRef]
- Calikoglu, E.O.; Aras, A. Defensive medicine among different surgical disciplines: A descriptive cross-sectional study. J. Forensic Leg. Med. 2020, 73, 101970. [Google Scholar] [CrossRef]
- di Luca, A.; Vetrugno, G.; Pascali, V.L.; Oliva, A.; Ozonoff, A. Perspectives on Patient Safety and Medical Malpractice: A Comparison of Medical and Legal Systems in Italy and the United States. J. Patient Saf. 2019, 15, e78–e81. [Google Scholar] [CrossRef]
- Krieg, C.; Hudon, C.; Chouinard, M.-C.; Dufour, I. Individual predictors of frequent emergency department use: A scoping review. BMC Health Serv. Res. 2016, 16, 594. [Google Scholar] [CrossRef]
- Wahl, H.; Banerjee, J.; Manikam, L.; Parylo, C.; Lakhanpaul, M. Health information needs of families attending the paediatric emergency department. Arch. Dis. Child. 2011, 96, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Hendry, S.J.; Beattie, T.F.; Heaney, D. Minor illness and injury: Factors influencing attendance at a paediatric accident and emergency department. Arch. Dis. Child. 2005, 90, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Betz, M.G.; Grunfeld, A.F. ‘Fever phobia’ in the emergency department: A survey of children’s caregivers. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2006, 13, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Zickafoose, J.S.; DeCamp, L.R.; Prosser, L.A. Association between enhanced access services in pediatric primary care and utilization of emergency departments: A national parent survey. J. Pediatr. 2013, 163, e1–e6. [Google Scholar] [CrossRef]
- Sturm, J.J.; Hirsh, D.; Weselman, B.; Simon, H.K. Reconnecting patients with their primary care provider: An intervention for reducing nonurgent pediatric emergency department visits. Clin. Pediatr. 2014, 53, 988–994. [Google Scholar] [CrossRef]
- Yoffe, S.J.; Moore, R.W.; Gibson, J.O.; Dadfar, N.M.; McKay, R.L.; A McClellan, D.; Huang, T.-Y. A reduction in emergency department use by children from a parent educational intervention. Fam. Med. 2011, 43, 106–111. [Google Scholar]
- Salami, O.; Salvador, J.; Vega, R. Reasons for nonurgent pediatric emergency department visits: Perceptions of health care providers and caregivers. Pediatr. Emerg. Care 2012, 28, 43–46. [Google Scholar] [CrossRef]
- Ismail, S.A.; Gibbons, D.C.; Gnani, S. Reducing inappropriate accident and emergency department attendances: A systematic review of primary care service interventions. Br. J. Gen. Pract. 2013, 63, e813–e820. [Google Scholar] [CrossRef]
- Carini, E.; Villani, L.; Pezzullo, A.M.; Gentili, A.; Barbara, A.; Ricciardi, W.; Boccia, S. The Impact of Digital Patient Portals on Health Outcomes, System Efficiency, and Patient Attitudes: Updated Systematic Literature Review. J. Med. Internet Res. 2021, 23, e26189. [Google Scholar] [CrossRef]
- Pietrantonio, F.; on behalf of FADOI-OdC Group; Vinci, A.; Maurici, M.; Ciarambino, T.; Galli, B.; Signorini, A.; La Fazia, V.M.; Rosselli, F.; Fortunato, L.; et al. Intra- and Extra-Hospitalization Monitoring of Vital Signs—Two Sides of the Same Coin: Perspectives from LIMS and Greenline-HT Study Operators. Sensors 2023, 23, 5408. [Google Scholar] [CrossRef]
- Bozzola, E.; Caffarelli, C.; Santamaria, F.; Corsello, G. Year 2022, exploring COVID-19 pandemic in children. Ital. J. Pediatr. 2023, 49, 128. [Google Scholar] [CrossRef] [PubMed]
| Cumulative Attendance | N° Patients (0–18) | % Patients (0–18) | N° Attendances | % Attendances |
|---|---|---|---|---|
| 1 | 17,817 | 71.8% | 17,817 | 49.9% |
| 2 | 4731 | 19.1% | 9462 | 26.5% |
| 3 | 1418 | 5.7% | 4254 | 11.9% |
| 4 | 481 | 1.9% | 1924 | 5.4% |
| 5 | 218 | 0.9% | 1090 | 3.1% |
| 6 | 85 | 0.3% | 510 | 1.4% |
| 7 | 29 | 0.1% | 203 | 0.6% |
| 8 | 23 | 0.1% | 184 | 0.5% |
| 9 | 7 | 0.1% | 63 | 0.2% |
| 10 | 4 | 0.1% | 40 | 0.1% |
| >10 | 11 | 0.1% | 144 | 0.4% |
| Total | 24,824 | 100% | 35,691 | 100% |
| Grouping Variable | Groups (N) | Cumulative Patients per Group | Cumulative Attendances per Group | ||||
|---|---|---|---|---|---|---|---|
| Min | Avg | Max | Min | Avg | Max | ||
| LHD | 6 | 2995 | 4137.3 | 5175 | 4072 | 5948.5 | 7626 |
| PCP/GP | 904 | 1 | 27.5 | 261 | 1 | 39.5 | 422 |
| Patient | 24,824 | - | - | - | 1 | 1.4 | 21 |
| Variable | Population | |||
|---|---|---|---|---|
| Total Patients (N = 24,824) | Non-FU (N = 23,966) | FU (N = 858) | p-Value | |
| Gender | ||||
| Male | 14,040 (56.6%) | 13,549 (56.5%) | 491 (57.2%) | 0.688 * |
| Female | 10,784 (43.4%) | 10,417 (43.5%) | 367 (42.8%) | |
| Mean age (SD) | 7.6 (5.5) | 7.7 (5.5) | 5.3 (5.5) | <0.001 ° |
| Age group | ||||
| Infants (<1) | 2491 (10.0%) | 2288 (9.5%) | 203 (23.7%) | <0.001 * |
| Toddlers (1) | 2017 (8.1%) | 1905 (7.9%) | 112 (13.1%) | |
| Early childhood (2–5) | 5996 (24.2%) | 5775 (24.1%) | 221 (25.8%) | |
| Middle childhood (6–12) | 8143 (32.8%) | 7966 (33.2%) | 177 (20.6%) | |
| Adolescents (13–15) | 3746 (15.1%) | 3651 (15.2%) | 95 (11.1%) | |
| Young adults (>15) | 2431 (9.8%) | 2381 (9.9%) | 50 (5.8%) | |
| Attendances | ||||
| Total attendance (N = 35,691) | Non-FU (N = 31,533) | FU (N = 4158) | ||
| Gender | ||||
| Male | 15,372 (43.1%) | 17,934 (56.9%) | 2385 (57.4%) | 0.552 * |
| Female | 20,319 (56.9%) | 13,559 (43.1%) | 1773 (42.6%) | |
| Age group | ||||
| Infancy (<1) | 3830 (10.7%) | 3078 (9.8%) | 752 (18.1%) | <0.001 * |
| Toddler (1) | 3439 (9.6%) | 2799 (8.9%) | 640 (15.4%) | |
| Early childhood (2–5) | 9114 (25.5%) | 7929 (25.1%) | 1185 (28.5%) | |
| Middle childhood (6–12) | 10,962 (30.7%) | 10,111 (32.1%) | 851 (20.5%) | |
| Adolescent (13–15) | 5036 (14.1%) | 4591 (14.6%) | 445 (10.7%) | |
| Young adults (>15) | 3310 (9.3%) | 3025 (9.6%) | 285 (6.9%) | |
| Triage code | ||||
| 1 | 2010 (5.6%) | 1724 (5.5%) | 286 (6.9%) | <0.001 * |
| 2 | 22,391 (62.7%) | 19,966 (63.3%) | 2425 (58.3%) | |
| 3 | 8503 (23.8%) | 7502 (23.8%) | 1001 (24.1%) | |
| 4 | 2411 (6.8%) | 2058 (6.5%) | 353 (8.5%) | |
| 5 | 376 (1.1%) | 283 (0.9%) | 93 (2.2%) | |
| Arrival mode | ||||
| EMS | 33,797 (94.7%) | 29,872 (94.7%) | 3925 (94.4%) | 0.363 * |
| NO EMS | 1894 (5.3%) | 1661 (5.3%) | 233 (5.6%) | |
| Day of the week | ||||
| Working day | 11,089 (31.1%) | 21,705 (68.8%) | 2897 (69.7%) | 0.271 * |
| Festivity | 24,602 (68–9%) | 9828 (31.2%) | 1261 (30.3%) | |
| Appropriateness | ||||
| Not appropriate | 22,295 (62.5%) | 19,823 (62.9%) | 2472 (59.5%) | <0.001 * |
| Appropriate | 13,396 (37.5%) | 11,710 (37.1%) | 1686 (40.6%) | |
| Variables | Median Odds Ratio | p-Value | 95% Confidence Interval |
|---|---|---|---|
| Gender | |||
| Female | - | - | - |
| Male | 1.06 | 0.040 | 1.00–1.13 |
| Age Group | |||
| Infancy (<1) | 3.05 | <0.001 | 2.73–3.41 |
| Toddler (1) | 1.12 | 0.050 | 0.99–1.26 |
| Early childhood (2–5) | - | - | - |
| Middle childhood (6–12) | 1.29 | <0.001 | 1.18–1.40 |
| Adolescent (13–15) | 2.27 | <0.001 | 2.05–2.51 |
| Young adult (>15) | 3.32 | <0.001 | 2.94–3.75 |
| Day of the Week | |||
| Workday | - | - | - |
| Vacation day | 0.08 | 0.007 | 0.02–0.14 |
| Arrival Mode | |||
| Not by EMS | - | - | - |
| By EMS | 5.65 | <0.001 | 4.99–6.38 |
| Frequent Usage | |||
| Non-frequent user | - | - | - |
| Frequent user | 1.24 | <0.001 | 1.10–1.39 |
| Constant Value | 0.28 | <0.001 | 0.21–0.37 |
| Variables | Variance | p-Value | 95% Confidence Interval |
|---|---|---|---|
| District | 0.12 | - | 0.04–0.38 |
| PCP/GP > District | 0.03 | - | 0.02–0.05 |
| Patient > PCP/GP > District | 1.41 | - | 1.24–1.61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Furia, G.; Ingravalle, F.; Vinci, A.; Papini, P.; Barbara, A.; Chierchini, P.; Damiani, G.; Maurici, M.; De Vito, C. The Frequent Use of Emergency Departments Among the Pediatric Population: A Retrospective Analysis in Rome, Italy. Epidemiologia 2025, 6, 31. https://doi.org/10.3390/epidemiologia6030031
Furia G, Ingravalle F, Vinci A, Papini P, Barbara A, Chierchini P, Damiani G, Maurici M, De Vito C. The Frequent Use of Emergency Departments Among the Pediatric Population: A Retrospective Analysis in Rome, Italy. Epidemiologia. 2025; 6(3):31. https://doi.org/10.3390/epidemiologia6030031
Chicago/Turabian StyleFuria, Giuseppe, Fabio Ingravalle, Antonio Vinci, Paolo Papini, Andrea Barbara, Patrizia Chierchini, Gianfranco Damiani, Massimo Maurici, and Corrado De Vito. 2025. "The Frequent Use of Emergency Departments Among the Pediatric Population: A Retrospective Analysis in Rome, Italy" Epidemiologia 6, no. 3: 31. https://doi.org/10.3390/epidemiologia6030031
APA StyleFuria, G., Ingravalle, F., Vinci, A., Papini, P., Barbara, A., Chierchini, P., Damiani, G., Maurici, M., & De Vito, C. (2025). The Frequent Use of Emergency Departments Among the Pediatric Population: A Retrospective Analysis in Rome, Italy. Epidemiologia, 6(3), 31. https://doi.org/10.3390/epidemiologia6030031







