Reshaping Emergency Care: Dynamics of OHCA and STEMI in a Three-Year Analysis
Abstract
1. Introduction
2. Materials and Methods
3. Results
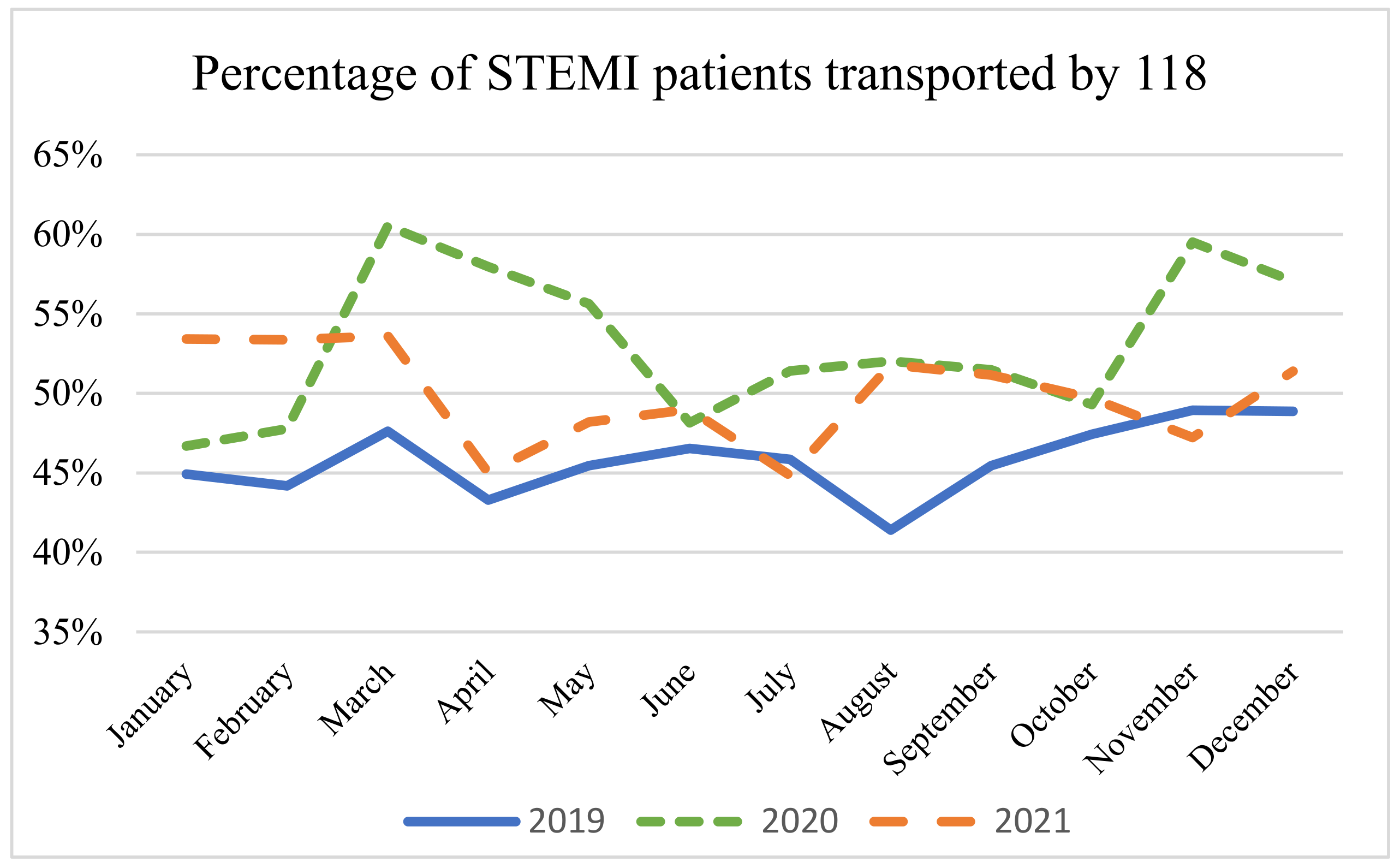
3.1. STEMI
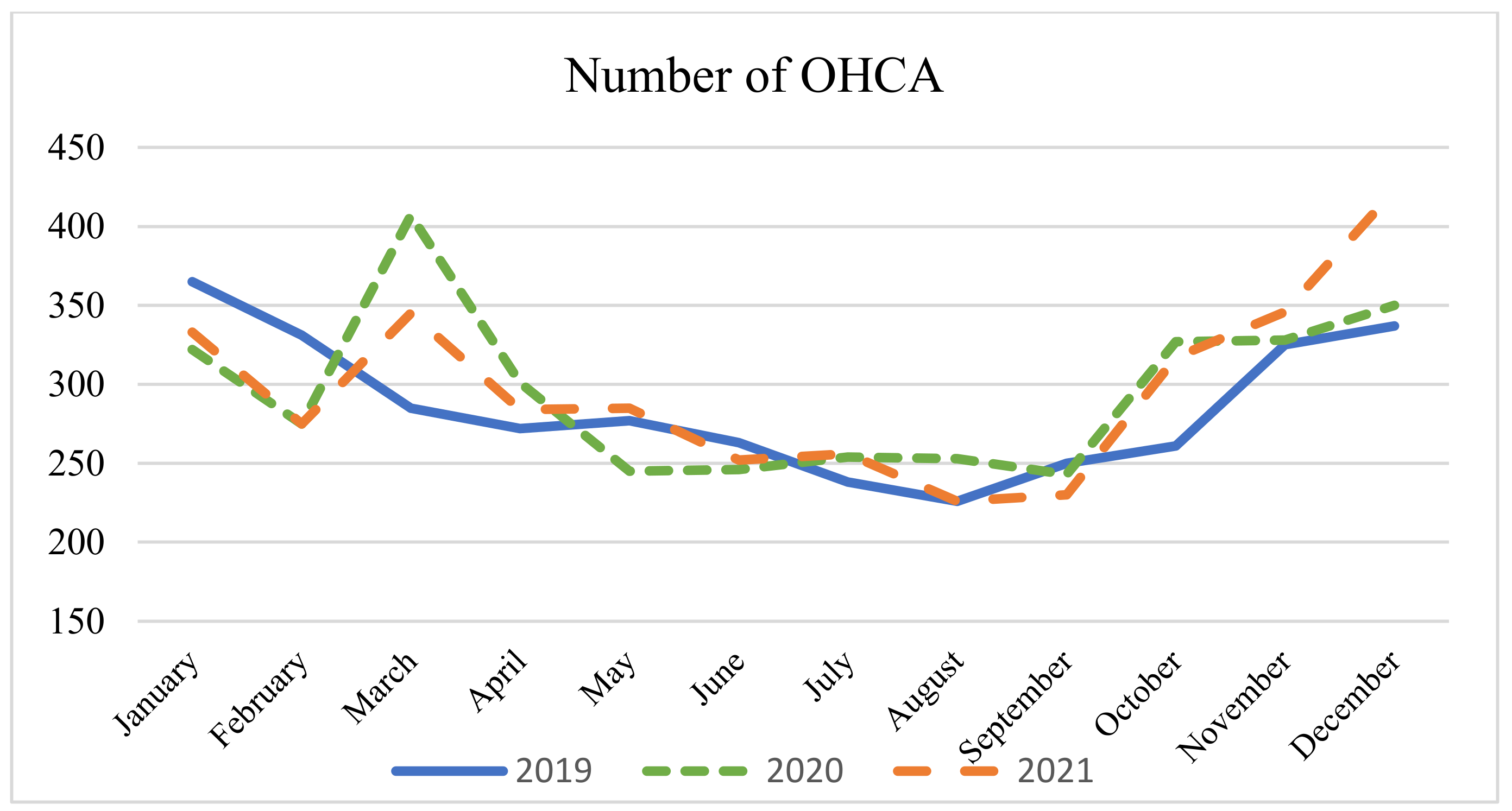
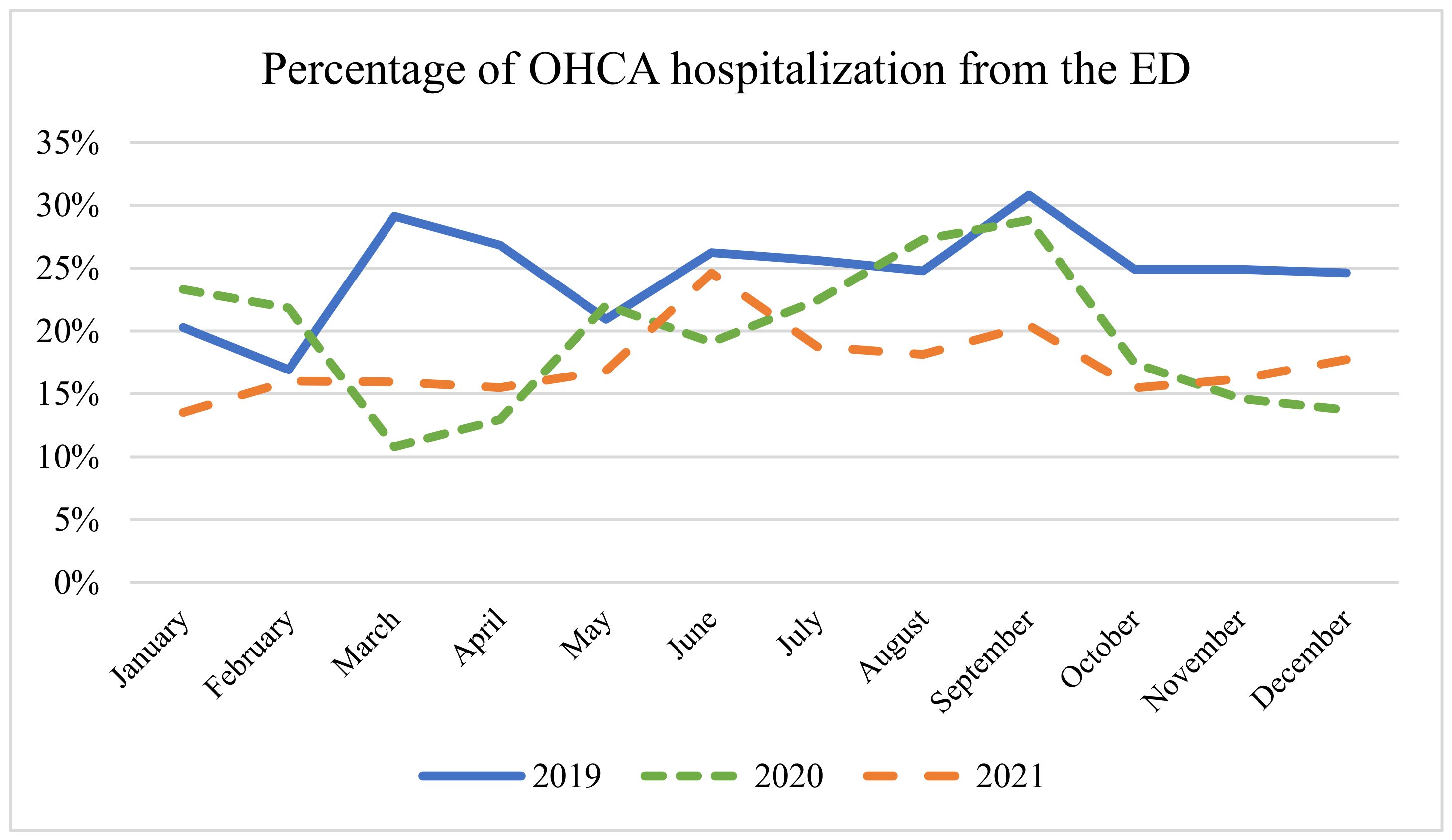
3.2. OHCA
4. Discussion
4.1. STEMI
4.2. OHCA
4.3. EMS
4.4. Relationship between OHCA and STEMI
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sartor, G.; Del Riccio, M.; Dal Poz, I.; Bonanni, P.; Bonaccorsi, G. COVID-19 in Italy: Considerations on Official Data. Int. J. Infect. Dis. 2020, 98, 188–190. [Google Scholar] [CrossRef]
- Ciminelli, G.; Garcia-Mandicó, S. COVID-19 in Italy: An Analysis of Death Registry Data. J. Public. Health 2020, 42, 723–730. [Google Scholar] [CrossRef] [PubMed]
- Fagoni, N.; Perone, G.; Villa, G.F.G.F.; Celi, S.; Bera, P.; Sechi, G.M.; Mare, C.; Zoli, A.; Botteri, M. The Lombardy Emergency Medical System Faced with COVID-19: The Impact of Out-of-Hospital Outbreak. Prehospital Emerg. Care 2020, 25, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Zedde, M.; Pezzella, F.R.; Paciaroni, M.; Corea, F.; Reale, N.; Toni, D.; Caso, V. Stroke Care in Italy: An Overview of Strategies to Manage Acute Stroke in COVID-19 Time. Eur. Stroke J. 2020, 5, 222–229. [Google Scholar] [CrossRef]
- Baracchini, C.; Pieroni, A.; Viaro, F.; Cianci, V.; Cattelan, A.M.; Tiberio, I.; Munari, M.; Causin, F. Acute Stroke Management Pathway during Coronavirus-19 Pandemic. Neurol. Sci. 2020, 41, 1003–1005. [Google Scholar] [CrossRef] [PubMed]
- Comelli, I.; Scioscioli, F.; Cervellin, G. Impact of the COVID-19 Epidemic on Census, Organization and Activity of a Large Urban Emergency Department. Acta Biomed. 2020, 91, 45–49. [Google Scholar] [CrossRef]
- Giuseppe, S.; Bellini, L.; Fagoni, N.; Compatti, S.; Botteri, M.; Villa, G.F.; Sironi, S.; Signorelli, C.; Sechi, G.M.; Zoli, A. Missed Training, Collateral Damage from COVID 19? Disaster Med. Public. Health Prep. 2022, 16, 1–8. [Google Scholar] [CrossRef]
- Stirparo, G.; Oradini-Alacreu, A.; Signorelli, C.; Sechi, G.M.; Zoli, A.; Fagoni, N. Smart-working policies during COVID-19 pandemic: A way to reduce work-related traumas? Intern. Emerg. Med. 2022, 17, 2427–2430. [Google Scholar] [CrossRef] [PubMed]
- Diegoli, H.; Magalhães, P.S.C.; Martins, S.C.O.; Moro, C.H.C.; Franca, P.H.C.; Safanelli, J.; Nagel, V.; Venancio, V.G.; Liberato, R.B.; Longo, A.L. Decrease in Hospital Admissions for Transient Ischemic Attack, Mild, and Moderate Stroke during the COVID-19 Era. Stroke 2020, 51, 2315–2321. [Google Scholar] [CrossRef]
- Rose, D.Z.; Burgin, W.S.; Renati, S. Untreated Stroke as Collateral Damage of COVID-19: “Time Is Brain” Versus “Stay at Home”. Neurohospitalist 2020, 10, 291–292. [Google Scholar] [CrossRef]
- Mosites, E.; Parker, E.M.; Clarke, K.E.N.; Gaeta, J.M.; Baggett, T.P.; Imbert, E.; Sankaran, M.; Scarborough, A.; Huster, K.; Hanson, M.; et al. Assessment of SARS-CoV-2 Infection Prevalence in Homeless Shelters—Four U.S. Cities, March 27–April 15, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 521–522. [Google Scholar] [CrossRef]
- Raitio, A.; Ahonen, M.; Jääskelä, M.; Jalkanen, J.; Luoto, T.T.; Haara, M.; Nietosvaara, Y.; Salonen, A.; Pakkasjärvi, N.; Laaksonen, T.; et al. Reduced Number of Pediatric Orthopedic Trauma Requiring Operative Treatment during COVID-19 Restrictions: A Nationwide Cohort Study. Scand. J. Surg. 2020, 110, 1457496920968014. [Google Scholar] [CrossRef] [PubMed]
- Stirparo, G.; Gambolò, L.; Bellini, L.; Medioli, F.; Bertuol, M.; Guasconi, M.; Sulla, F.; Artioli, G.; Sarli, L. Satisfaction Evaluation for ACLS Training. Acta Biomed. 2022, 93, e2022260. [Google Scholar] [CrossRef]
- Gentile, F.R.; Primi, R.; Baldi, E.; Compagnoni, S.; Mare, C.; Contri, E.; Reali, F.; Bussi, D.; Facchin, F.; Currao, A.; et al. Out-of-Hospital Cardiac Arrest and Ambient Air Pollution: A Dose-Effect Relationship and an Association with OHCA Incidence. PLoS ONE 2021, 16, e0256526. [Google Scholar] [CrossRef] [PubMed]
- Villa, G.F.; Kette, F.; Balzarini, F.; Riccò, M.; Manera, M.; Solaro, N.; Pagliosa, A.; Zoli, A.; Migliori, M.; Sechi, G.M.; et al. Out-of-Hospital Cardiac Arrest (OHCA) Survey in Lombardy: Data Analysis through Prospective Short Time Period Assessment. Acta Biomed. 2019, 90, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Stirparo, G.; Fagoni, N.; Bellini, L.; Oradini-Alacreu, A.; Migliari, M.; Villa, G.F.; Botteri, M.; Signorelli, C.; Sechi, G.M.; Zoli, A. Cardiopulmonary Resuscitation Missed by Bystanders: Collateral Damage of Coronavirus Disease 2019. Acta Anaesthesiol. Scand. 2022, 66, 1124–1129. [Google Scholar] [CrossRef]
- Mathew, S.; Harrison, N.; Chalek, A.D.; Gorelick, D.; Brennan, E.; Wise, S.; Gandolfo, L.; O’Neil, B.; Dunne, R. Effects of the COVID-19 Pandemic on out-of-Hospital Cardiac Arrest Care in Detroit. Am. J. Emerg. Med. 2021, 46, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Borkowska, M.J.; Jaguszewski, M.J.; Koda, M.; Gasecka, A.; Szarpak, A.; Gilis-Malinowska, N.; Safiejko, K.; Szarpak, L.; Filipiak, K.J.; Smereka, J. Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis. J. Clin. Med. 2021, 10, 1209. [Google Scholar] [CrossRef]
- Pessoa-Amorim, G.; Camm, C.F.; Gajendragadkar, P.; De Maria, G.L.; Arsac, C.; Laroche, C.; Zamorano, J.L.; Weidinger, F.; Achenbach, S.; Maggioni, A.P.; et al. Admission of Patients with STEMI since the Outbreak of the COVID-19 Pandemic: A Survey by the European Society of Cardiology. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 210–216. [Google Scholar] [CrossRef]
- Rattka, M.; Dreyhaupt, J.; Winsauer, C.; Stuhler, L.; Baumhardt, M.; Thiessen, K.; Rottbauer, W.; Imhof, A. Effect of the COVID-19 Pandemic on Mortality of Patients with STEMI: A Systematic Review and Meta-Analysis. Heart 2020, 107, 482–487. [Google Scholar] [CrossRef]
- Little, C.D.; Kotecha, T.; Candilio, L.; Jabbour, R.J.; Collins, G.B.; Ahmed, A.; Connolly, M.; Kanyal, R.; Demir, O.M.; Lawson, L.O.; et al. COVID-19 Pandemic and STEMI: Pathway Activation and Outcomes from the Pan-London Heart Attack Group. Open Heart 2020, 7, e001432. [Google Scholar] [CrossRef]
- D’Ascenzi, F.; Cameli, M.; Forni, S.; Gemmi, F.; Szasz, C.; Di Fabrizio, V.; Mechi, M.T.; Nocci, M.; Mondillo, S.; Valente, S. Reduction of Emergency Calls and Hospitalizations for Cardiac Causes: Effects of Covid-19 Pandemic and Lockdown in Tuscany Region. Front. Cardiovasc. Med. 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Leor, O.; Cid-Alvarez, B.; Ojeda, S.; Martin-Moreiras, J.; Ramon Rumoroso, J.; Lopez-Palop, R.; Serrador, A.; Cequier, A.; Romaguera, R.; Cruz, I.; et al. Impact of the COVID-19 Pandemic on Interventional Cardiology Activity in Spain. REC: Interv. Cardiol. 2020, 2, 82–89. [Google Scholar] [CrossRef]
- Stirparo, G.; Bellini, L.; Ristagno, G.; Bonora, R.; Pagliosa, A.; Migliari, M.; Andreassi, A.; Signorelli, C.; Sechi, G.M.; Fagoni, N. The Impact of COVID-19 on Lombardy Region ST-Elevation Myocardial Infarction Emergency Medical System Network-A Three-Year Study. J. Clin. Med. 2022, 11, 5718. [Google Scholar] [CrossRef] [PubMed]
- Prezant, D.J.; Lancet, E.A.; Zeig-Owens, R.; Lai, P.H.; Appel, D.; Webber, M.P.; Braun, J.; Hall, C.B.; Asaeda, G.; Kaufman, B.; et al. System Impacts of the COVID-19 Pandemic on New York City’s Emergency Medical Services. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1205–1213. [Google Scholar] [CrossRef]
- Goldberg, S.A.; Cash, R.E.; Peters, G.; Weiner, S.G.; Greenough, P.G.; Seethala, R. The Impact of COVID-19 on Statewide EMS Use for Cardiac Emergencies and Stroke in Massachusetts. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12351. [Google Scholar] [CrossRef] [PubMed]
- AREU Sistema AREU. Available online: https://www.areu.lombardia.it/web/home/sistema-emergenza-urgenza (accessed on 1 July 2021).
- Perlini, S.; Canevari, F.; Cortesi, S.; Sgromo, V.; Brancaglione, A.; Contri, E.; Pettenazza, P.; Salinaro, F.; Speciale, F.; Sechi, G.; et al. Emergency Department and Out-of-Hospital Emergency System (112-AREU 118) Integrated Response to Coronavirus Disease 2019 in a Northern Italy Centre. Intern. Emerg. Med. 2020, 15, 825–833. [Google Scholar] [CrossRef]
- Spina, S.; Marrazzo, F.; Migliari, M.; Stucchi, R.; Sforza, A.; Fumagalli, R. The Response of Milan’s Emergency Medical System to the COVID-19 Outbreak in Italy. Lancet 2020, 395, e49–e50. [Google Scholar] [CrossRef]
- Marrazzo, F.; Spina, S.; Pepe, P.E.; D’Ambrosio, A.; Bernasconi, F.; Manzoni, P.; Graci, C.; Frigerio, C.; Sacchi, M.; Stucchi, R.; et al. Rapid Reorganization of the Milan Metropolitan Public Safety Answering Point Operations during the Initial Phase of the COVID-19 Outbreak in Italy. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1240–1249. [Google Scholar] [CrossRef]
- Spina, S.; Gianquintieri, L.; Marrazzo, F.; Migliari, M.; Sechi, G.M.; Migliori, M.; Pagliosa, A.; Bonora, R.; Langer, T.; Caiani, E.G.; et al. Detection of Patients with COVID-19 by the Emergency Medical Services in Lombardy through an Operator-Based Interview and Machine Learning Models. Emerg. Med. J. 2023, 40, 810–820. [Google Scholar] [CrossRef]
- Astir. Available online: https://www.astir.com/soluzioni/euol-emergenza-urgenza-online/ (accessed on 30 April 2024).
- EuMed. Available online: https://www.eumed.it/icd9cm/index.php?scelta=diagnosi&queryutente=4379&ok=cerca (accessed on 30 April 2024).
- Lorenzo, G.; Antonia, B.M.; Maria, B.P.; Andrea, P.; Francesco, V.G.; Gianluca, C.E. Development of a Novel Framework to Propose New Strategies for Automated External Defibrillators Deployment Targeting Residential Out-Of-Hospital Cardiac Arrests: Application to the City of Milan. ISPRS Int. J. Geo-Inf. 2020, 9, 491. [Google Scholar] [CrossRef]
- Bellini, L.; Fagoni, N.; Andreassi, A.; Sechi, G.M.; Bonora, R.; Stirparo, G. Effectiveness of Cardiopulmonary Resuscitation at the Workplace. Med. Lav. 2023, 114, e2023010. [Google Scholar] [CrossRef] [PubMed]
- Gianni, A.; Botteri, M.; Stirparo, G.; Mattesi, G.; Zorzi, A.; Villa, G.F. The impact of the Italian law mandating an automatic external defibrillator in all sports venues on sudden cardiac arrest resuscitation rates. Eur. J. Prev. Cardiol. 2024, 31, e16–e18. [Google Scholar] [CrossRef]
- Patocka, C.; Lockey, A.; Lauridsen, K.G.; Greif, R. Impact of Accredited Advanced Life Support Course Participation on In-Hospital Cardiac Arrest Patient Outcomes: A Systematic Review. Resusc. Plus 2023, 14, 100389. [Google Scholar] [CrossRef]
- Wang, H.; Paulson, K.R.; Pease, S.A.; Watson, S.; Comfort, H.; Zheng, P.; Aravkin, A.Y.; Bisignano, C.; Barber, R.M.; Alam, T.; et al. Estimating Excess Mortality Due to the COVID-19 Pandemic: A Systematic Analysis of COVID-19-Related Mortality, 2020–2021. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef] [PubMed]
- Zińczuk, A.; Rorat, M.; Jurek, T. COVID-19-Related Excess Mortality—An Overview of the Current Evidence. Arch. Med. Sadowej Kryminol. 2023, 73, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Ballin, M.; Bergman, J.; Kivipelto, M.; Nordström, A.; Nordström, P. Excess Mortality after COVID-19 in Swedish Long-Term Care Facilities. J. Am. Med. Dir. Assoc. 2021, 22, 1574–1580.e8. [Google Scholar] [CrossRef] [PubMed]
- Godshall, C.E.; Banach, D.B. Pandemic Preparedness. Infect. Dis. Clin. N. Am. 2021, 35, 1077–1089. [Google Scholar] [CrossRef]
- Stratton, S.J. Post-Pandemic Emergency Medical Services. Prehosp. Disaster Med. 2021, 36, 249–250. [Google Scholar] [CrossRef] [PubMed]
- Vuilleumier, S.; Spichiger, T.; Dénéréaz, S.; Fiorentino, A. Not only COVID-19 disease impacts ambulance emergency demands but also lockdowns and quarantines. BMC Emerg. Med. 2023, 23, 4. [Google Scholar] [CrossRef]
- Stirparo, G.; Di Fronzo, P.; Solla, D.; Bottignole, D.; Gambolò, L. Are Italian Newly Licensed Nurses Ready? A Study on Self-Perceived Clinical Autonomy in Critical Care Scenarios. Healthcare 2024, 12, 809. [Google Scholar] [CrossRef] [PubMed]
- Pek, J.H.; Quah, L.J.J.; Valente, M.; Ragazzoni, L.; Della Corte, F. Use of Simulation in Full-Scale Exercises for Response to Disasters and Mass-Casualty Incidents: A Scoping Review. Prehosp. Disaster Med. 2023, 38, 792–806. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bottega, F.; Kacerik, E.; Perotti, G.; Signorelli, C.; Ristagno, G. Reshaping Emergency Care: Dynamics of OHCA and STEMI in a Three-Year Analysis. Epidemiologia 2024, 5, 362-370. https://doi.org/10.3390/epidemiologia5030026
Bottega F, Kacerik E, Perotti G, Signorelli C, Ristagno G. Reshaping Emergency Care: Dynamics of OHCA and STEMI in a Three-Year Analysis. Epidemiologia. 2024; 5(3):362-370. https://doi.org/10.3390/epidemiologia5030026
Chicago/Turabian StyleBottega, Francesca, Erika Kacerik, Gabriele Perotti, Carlo Signorelli, and Giuseppe Ristagno. 2024. "Reshaping Emergency Care: Dynamics of OHCA and STEMI in a Three-Year Analysis" Epidemiologia 5, no. 3: 362-370. https://doi.org/10.3390/epidemiologia5030026
APA StyleBottega, F., Kacerik, E., Perotti, G., Signorelli, C., & Ristagno, G. (2024). Reshaping Emergency Care: Dynamics of OHCA and STEMI in a Three-Year Analysis. Epidemiologia, 5(3), 362-370. https://doi.org/10.3390/epidemiologia5030026






