Outbreak Investigation of Typhoid Fever in the District of Gabes, South of Tunisia
Abstract
1. Introduction
2. Methods
2.1. Epidemiological Investigation
2.2. Bacteriological and Environmental Investigation
2.3. Ethical Considerations
3. Results
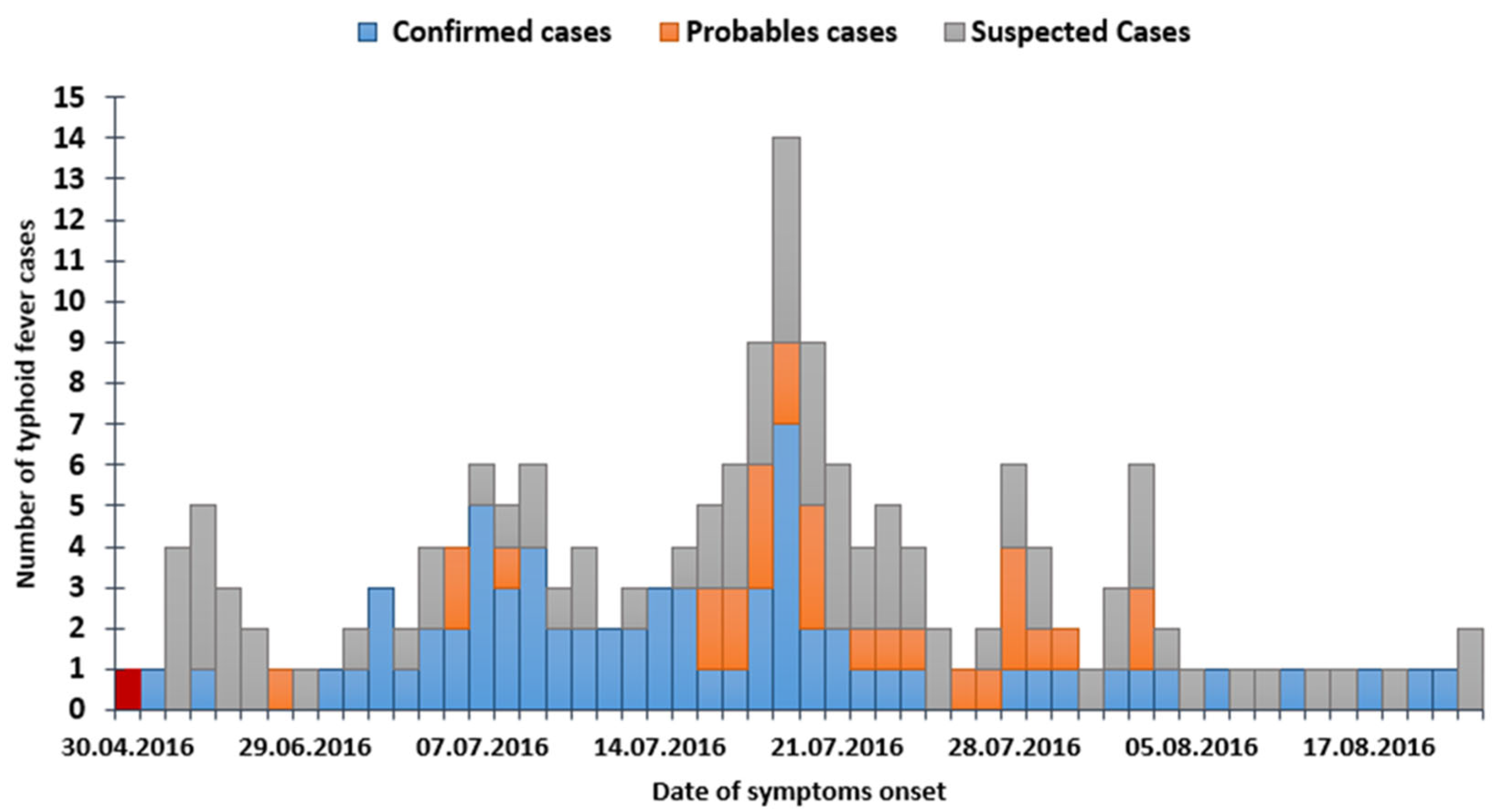
3.1. Descriptive Epidemiology
3.1.1. Description of the Study Population
3.1.2. Description of the Outbreak
3.2. Analytical Epidemiology
3.2.1. Main Risk Factors for Typhoid Fever
3.2.2. Laboratory Investigation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mahmud, A.K.; Chowdhury, A.J.; Sarker, Z.M.; Miah, R.A.; Saleh, A.A.; Mandal, R.M.; Dhakal, G.P. Typhoid Fever. Mymensingh Med. J. 2008, 17, 236–244. [Google Scholar] [PubMed]
- Colebunders, R.L. Review of Control of Communicable Diseases Manual, 19th Edition, edited by D. L. Heymann. Clin. Infect. Dis. 2009, 49, 1292–1293. [Google Scholar] [CrossRef]
- WHO Background Document: The Diagnosis, Treatment and Prevention of Typhoid Fever. Available online: http://apps.who.int/iris/handle/10665/68122 (accessed on 14 August 2018).
- Crump, J.A.; Luby, S.P.; Mintz, E.D. The Global Burden of Typhoid Fever. Bull. World Health Organ. 2004, 82, 346–353. [Google Scholar]
- Mogasale, V.; Maskery, B.; Ochiai, R.L.; Lee, J.S.; Mogasale, V.V.; Ramani, E.; Kim, Y.E.; Park, J.K.; Wierzba, T.F. Burden of typhoid fever in low-income and middle-income countries: A systematic, literature-based update with risk-factor adjustment. Lancet Glob. Health 2014, 2, e570–e580. [Google Scholar] [CrossRef] [PubMed]
- How Do Water Softeners Work? Scientific American. Available online: https://www.scientificamerican.com/article/how-do-water-softeners-wo/ (accessed on 20 September 2018).
- Desenclos, J.-C.; Vaillant, V.; Delarocque Astagneau, E.; Campèse, C.; Che, D.; Coignard, B.; Bonmarin, I.; Lévy Bruhl, D.; de Valk, H. Les principes de l’investigation d’une épidémie dans une finalité de santé publique. Méd. Mal. Infect. 2007, 37, 77–94. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.; Brunette, K.; Rybka, T.P.; Alexander, L.; Mejia, G.C.; MacDonald, P.D. Focus on field epidemiology Cohort Studies for Outbreak Investigations North Carolina Center for Public Health Preparedness. Available online: https://nciph.sph.unc.edu/focus/vol3/issue1/3-1Cohort_issue.pdf (accessed on 20 September 2018).
- Polonsky, J.A.; Martínez-Pino, I.; Nackers, F.; Chonzi, P.; Manangazira, P.; Van Herp, M.; Maes, P.; Porten, K.; Luquero, F.J. Descriptive Epidemiology of Typhoid Fever during an Epidemic in Harare, Zimbabwe, 2012. PLoS ONE 2014, 9, e114702. [Google Scholar] [CrossRef] [PubMed]
- Cherian, J.; Sampath, S.; Sunderamurthy, B.; Chavada, V.; Vasudevan, K.; Govindasamy, A. An outbreak investigation of typhoid fever in Pondicherry, South India, 2013. Int. J. Med. Sci. Public Health 2015, 4, 256–261. [Google Scholar] [CrossRef]
- Anand, P.K.; Ramakrishnan, R. Investigation of the outbreak of typhoid in a village of Thar Desert Rajasthan, India. Indian J. Med. Res. 2010, 131, 799–803. [Google Scholar] [PubMed]
- Noire, M. d’Afrique Epidémie de fièvre typhoïde à Gassa, extrême-nord Cameroun en 2011. Méd. D’Afr. Noire 2015, 62, 258. [Google Scholar]
- Toprak, D.; Erdorgan, S. Spatial analysis of the distribution of typhoid fever in Turkey. Int. Arch. Photogramm. Remote Sens. Spat. Inf. Sci. 2008, 37, 1367–1371. [Google Scholar]
- Vollaard, A.M.; Ali, S.; van Asten, H.A.G.H.; Widjaja, S.; Visser, L.G.; Surjadi, C.; van Dissel, J.T. Risk factors for typhoid and paratyphoid fever in Jakarta, Indonesia. JAMA 2004, 291, 2607–2615. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.H.; Bjune, G.; Nguyen, B.M.; Rottingen, J.A.; Grais, R.F.; Guerin, P.J. Risk factors associated with typhoid fever in Son La province, northern Vietnam. Trans. R. Soc. Trop. Med. Hyg. 2005, 99, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Gasem, M.H.; Dolmans, W.M.V.W.M.V.; Keuter, M.M.; Djokomoeljanto, R.R. Poor food hygiene and housing as risk factors for typhoid fever in Semarang, Indonesia. Trop. Med. Int. Health 2001, 6, 484–490. [Google Scholar] [CrossRef]
- Siddiqui, F.J.; Haider, S.R.; Bhutta, Z.A. Risk factors for typhoid fever in children in squatter settlements of Karachi: A nested case–control study. J. Infect. Public Health 2008, 1, 113–120. [Google Scholar] [CrossRef]
- Muti, M.; Gombe, N.; Tshimanga, M.; Takundwa, L.; Bangure, D.; Mungofa, S.; Chonzi, P. Typhoid outbreak investigation in Dzivaresekwa, suburb of Harare City, Zimbabwe, 2011. Pan. Afr. Med. J. 2014, 18, 309. [Google Scholar] [CrossRef]
- Kabwama, S.N.; Bulage, L.; Nsubuga, F.; Pande, G.; Oguttu, D.W.; Mafigiri, R.; Kihembo, C.; Kwesiga, B.; Masiira, B.; Okullo, A.E.; et al. A large and persistent outbreak of typhoid fever caused by consuming contaminated water and street-vended beverages: Kampala, Uganda, January–June 2015. BMC Public Health 2017, 17, 23. [Google Scholar]
- Saha, S.; Saha, S.; Das, R.C.; Faruque, A.S.G.; Salam, M.A.; Islam, M.; Saha, S.K. Enteric Fever and Related Contextual Factors in Bangladesh. Am. J. Trop. Med. Hyg. 2018, 99 (Suppl. S3), 20–25. [Google Scholar] [CrossRef]
- Abaidoo, R.C.; Keraita, B.; Drechsel, P.; Dissanayake, P.; Maxwell, A.S. Soil and Crop Contamination Through Wastewater Irrigation and Options for Risk Reduction in Developing Countries. In Soil Biology and Agriculture in the Tropics; Dion, P., Ed.; Springer: Berlin/Heidelberg, Germany, 2010; pp. 275–297. [Google Scholar]
- Kouamé, P.K.; Dongo, K.; Nguyen-Viet, H.; Zurbrügg, C.; Lüthi, C.; Hattendorf, J.; Utzinger, J.; Biémi, J.; Bonfoh, B. Ecohealth Approach to Urban Waste Management: Exposure to Environmental Pollutants and Health Risks in Yamoussoukro, Côte d’Ivoire. Int. J. Environ. Res. Public Health 2014, 11, 10292–10309. [Google Scholar] [CrossRef]
- Suleman, Y.; Darko, E.T.; Agyemang-Duah, W. Solid Waste Disposal and Community Health Implications in Ghana: Evidence from Sawaba, Asokore Mampong Municipal Assembly. J. Civ. Environ. Eng. 2015, 5, 202. [Google Scholar] [CrossRef]
- Alba, S.; Bakker, M.I.; Hatta, M.; Scheelbeek, P.F.D.; Dwiyanti, R.; Usman, R.; Sultan, A.R.; Sabir, M.; Tandirogang, N.; Amir, M.; et al. Risk Factors of Typhoid Infection in the Indonesian Archipelago. PLoS ONE 2016, 11, e0155286. [Google Scholar] [CrossRef]
- Bouallegue, O.; Grimont, F.; Salem, Y.B.; Letaief, A.; Mzoughi, R. Bactériologie. Bull. Soc. Pathol. Exot. 2004, 97, 173–174. [Google Scholar] [PubMed]
- Available online: https://covid19.onmne.tn/WebClientNew/Browser/%2FTyphoid%20fever%20outbreak%20investigation%20Gabes%202016 (accessed on 2 March 2022).

| Sub Groups | Exposed Population | Number of TF Cases (Proportional Distribution of Cases (%)) | Attack Rate (%) (CI95%) |
|---|---|---|---|
| Age (years) | p < 10−3 | ||
| <10 | 102 | 39 (38.24) | 38.23 (28.9–47.7) |
| 10–20 | 137 | 29 (28.43) | 21.16 (14.5–27.8) |
| 20–30 | 117 | 14 (13.73) | 11.96 (6.5–18.1) |
| 30–40 | 93 | 9 (8.82) | 9.67 (4.3–16.3) |
| 40–50 | 88 | 7 (6.86) | 7.95 (3.1–14.3) |
| 50–60 | 58 | 3 (2.94) | 5.17 (0.0–11.3) |
| ≥60 | 33 | 1 (0.98) | 3.03 (0.0–10.7) |
| Gender | NS | ||
| Male | 317 | 58 (56.86) | 18.29 (14.0–22.7) |
| Female | 311 | 44 (43.14) | 14.14 (10.6–18.2) |
| Level of education | p < 10−3 | ||
| Illiterate | 42 | 4 (3.92) | 9.52 (2.2–20.0) |
| out-of-school | 64 | 35 (34.31) | 54.68 (37.1–61.0) |
| Primary | 209 | 41 (40.20) | 19.61 (14.8–26.0) |
| Secondary | 244 | 17 (16.67) | 6.96 (4.0–10.3) |
| University | 69 | 5 (4.90) | 7.24 (1.6–14.1) |
| Housing type | p < 10−3 | ||
| Arab or rudimentary house | 234 | 80 (78.43) | 34.18 (26.3–37.8) |
| Villa or apartment | 394 | 22 (21.57) | 5.58 (4.6–10.6) |
| Total | 628 | 102 (100) | 16.24 (13.2–19.3) |
| Clinical Signs | Number N = 102 | Percentage (%) |
|---|---|---|
| Fever | 97 | 95.1 |
| Diarrhea | 58 | 56.9 |
| Abdominal pain | 48 | 47.1 |
| Vomiting | 47 | 46.1 |
| Asthenia | 43 | 42.2 |
| Constipation | 10 | 9.8 |
| Tuphos or neurological signs | 4 | 3.9 |
| Skin rash | 3 | 2.9 |
| Lenticular rosy spots | 2 | 2.0 |
| Socio-Demographic Factors Associated with Typhoid Fever | Crude OR | CI 95% | p |
|---|---|---|---|
| Age groups (years) | |||
| <10 | 19.81 | (2.60–150.83) | 0.004 |
| (10–20) | 8.59 | (1.12–65.56) | 0.038 |
| (20–30) | 4.35 | (0.55–34.37) | 0.163 |
| (30–40) | 3.42 | (0.41–28.16) | 0.251 |
| (40–50) | 2.76 | (0.32–23.38) | 0.35 |
| (50–60) | 1.74 | (0.17–17.49) | 0.636 |
| ≥60 (ref) | 1 | ||
| Level of education | |||
| Illiterate | 1.34 | (0.34–5.32) | 0.671 |
| Out-of-school | 12.10 | (4.36–33.60) | <10−3 |
| Primary | 3.28 | (1.24–8.67) | 0.017 |
| Secondary | 0.95 | (0.34–2.70) | 0.936 |
| University (ref) | 1 | ||
| Housing type | |||
| Arab or rudimentary house | 7.55 | (4.55–12.52) | <10−3 |
| Villa or apartment (ref) | 1 | ||
| Environmental factors associated with typhoid fever | Crude OR | CI 95% | p |
| Type of drinking water | |||
| Softened water | 3.80 | (1.80–8.05) | 0.001 |
| Private tank | 1.20 | (0.24–6.05) | 0.818 |
| Mineral water | 1.24 | (0.31–4.93) | 0.757 |
| Other (wells. cisterns. natural source) | 1.03 | (0.120–8.90) | 0.974 |
| Public tap water (National Water Supply and Distribution Company) (ref) | 1 | ||
| Exposure to softened water/type of use | |||
| For drinking | |||
| Yes | 3.50 | (1.93–6.31) | <10−3 |
| No (ref) | 1 | ||
| Washing of raw vegetables | |||
| Yes | 2.24 | (1.22–4.12) | 0.009 |
| No (ref) | 1 | ||
| Cooking | |||
| Yes | 2.37 | (1.54−3.65) | <10−3 |
| No (ref) | 1 | ||
| Conditions of water storage | |||
| Covered | |||
| No | 79.05 | (30.14–207.26) | <10−3 |
| Yes (ref) | 1 | ||
| Disinfected | |||
| Yes | 5.25 | (2.60–10.66) | <10−3 |
| No (ref) | 1 | ||
| Exposed to sunlight | |||
| Yes | 7.62 | (4.76–12.20) | <10−3 |
| No (ref) | |||
| Controlled bacteriologically | |||
| No | 2.92 | (1.15–7.45) | 0.0024 |
| Yes (ref) | 1 | ||
| Sanitation & household waste management | |||
| Connection to the public sanitation system | |||
| No | 2.14 | (1.38–3.32) | 0.001 |
| Yes (ref) | 1 | ||
| Using cesspools | |||
| Yes | 2.46 | (1.58–3.82) | <10−3 |
| No (ref) | 1 | ||
| Household waste management | |||
| Uncontrolled waste disposal | 5.30 | (3.27–8.60) | <10−3 |
| By the municipal departments (ref) | 1 | ||
| Fruit & vegetable supplies | |||
| Family garden | 8.11 | (5.10–12.91) | 0.001 |
| local market | 1 | ||
| Factors | AOR | 95% CI | p |
|---|---|---|---|
| Age | 0.95 | 0.93–0.97 | <10−3 |
| Education level | 0.001 | ||
| Illiterate | 2.55 | 0.49–13.10 | 0.263 |
| Out-of-school | 4.76 | 1.34–16.81 | 0.015 |
| Primary | 2.16 | 0.72–6.48 | 0.168 |
| Secondary | 0.75 | 0.24–2.34 | 0.622 |
| Living in arab or rudimentary house | 4.93 | 2.61–8.27 | <10−3 |
| Drinking softened water | 2.64 | 1.16–4.82 | 0.018 |
| Fruit and vegetables from family garden | 6.13 | 3.66–11.06 | <10−3 |
| Uncontrolled dumping of household waste | 3.52 | 2.03–6.94 | <10−3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hechaichi, A.; Bouguerra, H.; Letaief, H.; Safer, M.; Missaoui, L.; Cherif, A.; Farah, S.; Jabrane, H.; Atawa, T.; Yahia, H.; et al. Outbreak Investigation of Typhoid Fever in the District of Gabes, South of Tunisia. Epidemiologia 2023, 4, 223-234. https://doi.org/10.3390/epidemiologia4030023
Hechaichi A, Bouguerra H, Letaief H, Safer M, Missaoui L, Cherif A, Farah S, Jabrane H, Atawa T, Yahia H, et al. Outbreak Investigation of Typhoid Fever in the District of Gabes, South of Tunisia. Epidemiologia. 2023; 4(3):223-234. https://doi.org/10.3390/epidemiologia4030023
Chicago/Turabian StyleHechaichi, Aicha, Hind Bouguerra, Hajer Letaief, Mouna Safer, Lamia Missaoui, Amal Cherif, Saffar Farah, Houcine Jabrane, Taoufik Atawa, Hamdi Yahia, and et al. 2023. "Outbreak Investigation of Typhoid Fever in the District of Gabes, South of Tunisia" Epidemiologia 4, no. 3: 223-234. https://doi.org/10.3390/epidemiologia4030023
APA StyleHechaichi, A., Bouguerra, H., Letaief, H., Safer, M., Missaoui, L., Cherif, A., Farah, S., Jabrane, H., Atawa, T., Yahia, H., Hamdouni, H., Zitoun, K., Chahed, K., Laamouri, R., Daaboub, J., Rabhi, M., Salah, A. B., Chahed, M. K., & Bouafif Ben Alaya, N. (2023). Outbreak Investigation of Typhoid Fever in the District of Gabes, South of Tunisia. Epidemiologia, 4(3), 223-234. https://doi.org/10.3390/epidemiologia4030023






