Effectiveness of the Pfizer-BioNTech Vaccine against COVID-19-Associated Hospitalizations among Lebanese Adults ≥75 Years Old—Lebanon, April–May 2021
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Variables
2.4. Data Management
2.5. Ethical Approval
3. Results
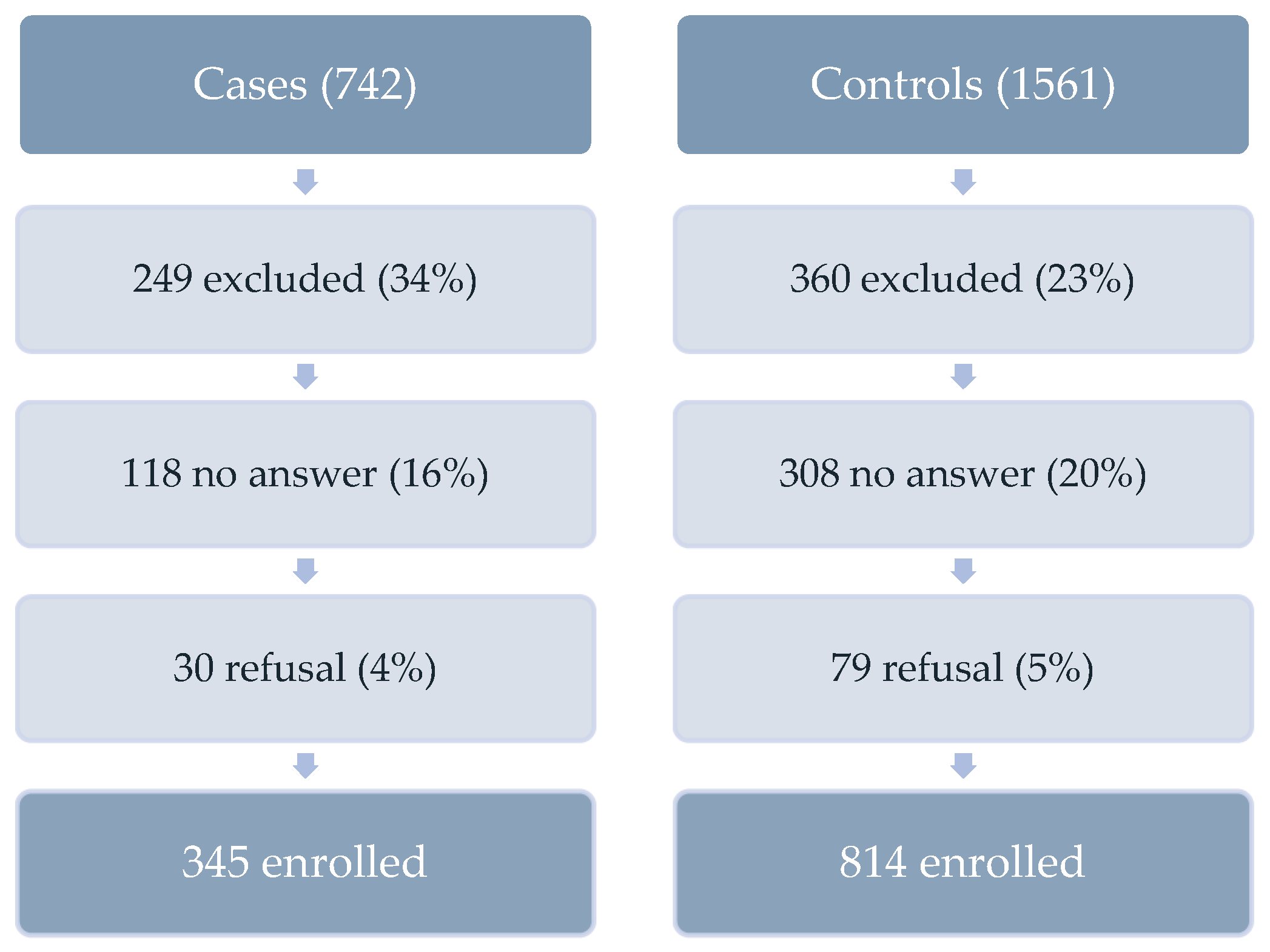
3.1. Study Population
3.2. Hospitalization
3.3. Vaccination Effectiveness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int (accessed on 17 December 2021).
- BBC News, Coronavirus: Greatest Test Since World War Two, Says UN Chief-BBC News, 1 April 2020. Available online: https://www.bbc.com/news/world-52114829 (accessed on 17 December 2021).
- Dong, Y.; Dai, T.; Wei, Y.; Zhang, L.; Zheng, M.; Zhou, F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct. Target. Ther. 2020, 5, 237. [Google Scholar] [CrossRef] [PubMed]
- Meo, S.A.; Bukhari, I.A.; Akram, J.; Meo, A.S.; Klonoff, D.C. COVID-19 vaccines: Comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna Vaccines. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 1663–1669. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Public Health. Monitoring of COVID-19 Infection in Lebanon-Daily Report. 2021. Available online: http://www.moph.gov.lb (accessed on 29 December 2021).
- Ministry of Public Health. Lebanon National Deployment and Vaccination Plan for COVID-19 Vaccines. Available online: https://www.moph.gov.lb/userfiles/files/Prevention/COVID-19%20Vaccine/Lebanon%20NDVP-%20Feb%2016%202021.pdf (accessed on 28 January 2021).
- IMPACT Platform. Impact Open Data: Vaccine Statistics. 2021. Available online: https://impact.cib.gov.lb/home?dashboardName=vaccine (accessed on 17 December 2021).
- World Health Organization. Evaluation of COVID-19 Vaccine Effectiveness: Interim Guidance, 17 March 2021, World Health Organization, WHO/2019-nCoV/Vaccine_Effectiveness/Measurement/2021.1. 2021. Available online: https://apps.who.int/iris/handle/10665/340301 (accessed on 17 December 2021).
- Ammar, Walid, Health System and Reform in Lebanon-2003. 2003. Available online: http://www.moph.gov.lb (accessed on 17 December 2021).
- Tenforde, M.W.; Olson, S.M.; Self, W.H.; Talbot, H.K.; Lindsell, C.J.; Steingrub, J.S.; Shapiro, N.I.; Ginde, A.A.; Douin, D.J.; Prekker, M.E.; et al. Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 among Hospitalized Adults Aged ≥65 Years—United States, January–March 2021. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, M.W.; Patel, M.M.; Ginde, A.A.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; Zepeski, A.; Gaglani, M.; McNeal, T.; et al. Effectiveness of SARS-CoV-2 mRNA Vaccines for Preventing COVID-19 Hospitalizations in the United States. Clin. Infect. Dis. 2022, 74, 1515–1524. [Google Scholar] [CrossRef] [PubMed]
- Bajema, K.L.; Dahl, R.M.; Prill, M.M.; Meites, E.; Rodriguez-Barradas, M.C.; Marconi, V.C.; Beenhouwer, D.O.; Brown, S.T.; Holodniy, M.; Lucero-Obusan, C.; et al. Effectiveness of COVID-19 mRNA Vaccines Against COVID-19–Associated Hospitalization—Five Veterans Affairs Medical Centers, United States, 1 February–6 August 2021. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 1294–1299. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, M.W.; Self, W.H.; Naioti, E.A.; Ginde, A.A.; Douin, D.J.; Olson, S.M.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; Zepeski, A.; et al. Sustained Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Associated Hospitalizations Among Adults—United States, March–July 2021. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 1156–1162. [Google Scholar] [CrossRef] [PubMed]
- Bernal, J.L.; Andrews, N.; Gower, C.; Robertson, C.; Stowe, J.; Tessier, E.; Simmons, R.; Cottrell, S.; Roberts, R.; O’Doherty, M.; et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on COVID-19 related symptoms, hospital admissions, and mortality in older adults in England: Test negative case-control study. BMJ 2021, 373, n1088. [Google Scholar] [CrossRef] [PubMed]
- Lauring, A.S.; Tenforde, M.W.; Chappell, J.D.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Ghamande, S.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; et al. Clinical severity of, and effectiveness of mRNA vaccines against, COVID-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: Prospective observational study. BMJ 2022, 376, e069761. [Google Scholar] [CrossRef] [PubMed]
- Self, W.H.; Tenforde, M.W.; Rhoads, J.P.; Gaglani, M.; Ginde, A.A.; Douin, D.J.; Olson, S.M.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; et al. Comparative Effectiveness of Moderna, Pfizer-BioNTech, and Janssen (Johnson & Johnson) Vaccines in Preventing COVID-19 Hospitalizations Among Adults Without Immunocompromising Conditions—United States, March–August 2021. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 1337–1343. [Google Scholar] [CrossRef] [PubMed]
- Nasreen, S.; Chung, H.; He, S.; Brown, K.A.; Gubbay, J.B.; Buchan, S.A.; Fell, D.B.; Austin, P.C.; Schwartz, K.L.; Sundaram, M.E.; et al. Effectiveness of COVID-19 vaccines against symptomatic SARS-CoV-2 infection and severe outcomes with variants of concern in Ontario. Nat. Microbiol. 2022, 7, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Hyams, C.; Marlow, R.; Maseko, Z.; King, J.; Ward, L.; Fox, K.; Heath, R.; Turner, A.; Friedrich, Z.; Morrison, L.; et al. Effectiveness of BNT162b2 and ChAdOx1 nCoV-19 COVID-19 vaccination at preventing hospitalisations in people aged at least 80 years: A test-negative, case-control study. Lancet Infect. Dis. 2021, 21, 1539–1548. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.; He, S.; Nasreen, S.; Sundaram, M.E.; Buchan, S.A.; Wilson, S.E.; Chen, B.; Calzavara, A.; Fell, D.B.; Austin, P.C.; et al. Effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines against symptomatic SARS-CoV-2 infection and severe COVID-19 outcomes in Ontario, Canada: Test negative design study. BMJ 2021, 374, n1943. [Google Scholar] [CrossRef] [PubMed]
- Merhi, G.; Trotter, A.J.; de Oliveira Martins, L.; Koweyes, J.; Le-Viet, T.; Naja, H.A.; Buaini, M.A.; Prosolek, S.J.; Alikhan, N.F.; Lott, M.; et al. Replacement of the Alpha variant of SARS-CoV-2 by the Delta variant in Lebanon between April and June 2021. Microbial Genom. 2022, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- CDC. COVID-19 Vaccination, Centers for Disease Control and Prevention, 11 February 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html (accessed on 20 December 2021).
| Characteristics | Case Patients (N = 345) * n (%) | Controls (N = 814) * n (%) | p-Value | ||
|---|---|---|---|---|---|
| Socio-demographic characteristics | |||||
| Age (mean ± sd) | 83.1 ± 5.6 | 82.8 ± 5.7 | 0.53 | ||
| Age groups | 75–84 | 236 (68.4) | 559 (68.7) | 0.98 | |
| 85+ | 109 (31.6) | 255 (31.3) | |||
| Gender | Female | 171 (49.6) | 463 (56.9) | 0.03 | |
| Male | 174 (50.4) | 350 (43.1) | |||
| Place of residence (governorate) | Mount Lebanon | 128 (37.1) | 318 (39.0) | 0.33 | |
| Bekaa/Baalbeck-Hermel | 75 (21.7) | 138 (17.0) | |||
| South Nabatieh | 64 (18.6) | 178 (21.9) | |||
| North | 47 (13.6) | 110 (13.5) | |||
| Beirut | 31 (9.0) | 70 (8.6) | |||
| Main income source | Family help | 265 (77.5) | 646 (82.8) | <0.001 | |
| Retirement pension | 38 (11.1) | 19 (2.4) | |||
| Personal savings | 34 (9.9) | 77 (9.9) | |||
| Financial help (not family) | 4 (1.2) | 30 (3.9) | |||
| No income | 1 (0.3) | 8 (1.0) | |||
| Living conditions | |||||
| Number of household members (mean ± sd) | 2.4 ± 1.7 | 2.0 ± 1.9 | <0.001 | ||
| Number of rooms (mean ± sd) | 3.4 ± 1.4 | 3.0 ± 1.2 | <0.001 | ||
| Crowding index (mean ± sd) | 0.8 ± 0.6 | 0.7 ± 0.7 | 0.64 | ||
| Living arrangement | Alone | 24 (7.0) | 122 (15.1) | <0.001 | |
| With Family | 299 (87.1) | 610 (75.5) | |||
| With domestic help | 17 (5.0) | 61 (7.5) | |||
| Long-term facility | 3 (0.9) | 15 (1.9) | |||
| Health conditions (in the 12 month period prior to hospital admission) | |||||
| Perception of general health status | Very good | 61 (17.9) | 51 (6.4) | <0.001 | |
| Good | 151 (44.4) | 290 (36.1) | |||
| Fair | 87 (25.6) | 258 (32.1) | |||
| Poor | 34 (10) | 169 (21.0) | |||
| Very poor | 7 (2.1) | 35 (4.4) | |||
| Ability to walk, climb up or down stairs alone | Yes, without difficulty | 141 (41.2) | 162 (20.4) | ||
| Yes, but with some difficulty | 90 (26.3) | 161 (20.2) | <0.001 | ||
| Yes, but with help or assistance | 73 (21.4) | 202 (25.4) | |||
| No | 38 (11.1) | 271 (34.0) | |||
| Underlying conditions | Hypertension | 221 (69.9) | 549 (75.6) | 0.07 | |
| Heart disease | 150 (50.2) | 448 (66.1) | <0.001 | ||
| Diabetes | 125 (42.7) | 314 (47.0) | 0.24 | ||
| Kidney disease | 34 (12.6) | 76 (13.0) | 0.96 | ||
| Lung disease | 30 (10.9) | 111 (18.3) | 0.007 | ||
| Cancer | 12 (4.4) | 68 (11.3) | 0.002 | ||
| Asthma | 10 (3.7) | 30 (5.2) | 0.46 | ||
| Rheumatological disorders | 6 (2.2) | 45 (7.8) | 0.003 | ||
| Liver disease | 4 (1.5) | 15 (2.6) | 0.44 | ||
| History of cancer | 4 (1.5) | 25 (4.3) | 0.05 | ||
| Immunodeficiency | 4 (1.5) | 6 (1.0) | 0.82 | ||
| Presence of at least one underlying condition | No | 50 (15.1) | 65 (8.4) | 0.001 | |
| Yes | 282 (84.9) | 713 (91.6) | |||
| Cognitive status (in the 12 month period prior to hospital admission) | |||||
| Ability to read and write | Yes, without difficulty | 169 (49.4) | 250 (32.5) | <0.001 | |
| Yes, but with some difficulty | 53 (15.5) | 142 (18.5) | |||
| Yes, but with help or assistance | 28 (8.2) | 48 (6.2) | |||
| No | 92 (26.9) | 329 (42.8) | |||
| Ability to perform calculations | Yes, without difficulty | 184 (53.8) | 233 (31.6) | <0.001 | |
| Yes, but with some difficulty | 50 (14.6) | 91 (12.3) | |||
| Yes, but with help or assistance | 21 (6.1) | 53 (7.2) | |||
| No | 87 (25.5) | 361 (48.9) | |||
| Characteristics | Case Patients (N = 345) § n (%) | Controls (N = 814) § n (%) | p-Value | |
|---|---|---|---|---|
| Month of confirmation/hospital admission * | April | 271 (78.6) | 464 (57.0) | <0.001 |
| May | 74 (21.4) | 350 (43.0) | ||
| Duration of hospitalization (days) | 11.1 ± 9.3 | 6.0 ± 7.0 | <0.001 | |
| Hospital stay | <3 days | 31 (9.6) | 160 (22.3) | <0.001 |
| 3–7 days | 120 (37.0) | 426 (59.5) | ||
| >7 days | 173 (53.4) | 130 (18.2) | ||
| Admission to ICU | Yes | 224 (66.9) | 180 (24.6) | <0.001 |
| No | 111 (33.1) | 551 (75.4) | ||
| Duration of stay in ICU | 8.5 ± 7.9 | 5.8 ± 5.8 | <0.001 | |
| Oxygenotherapy | Yes | 275 (90.2) | 175 (25.8) | <0.001 |
| No | 30 (9.8) | 503 (74.2) | ||
| Mechanical ventilation | Yes | 107 (46.3) | 40 (6.1) | <0.001 |
| No | 124 (53.7) | 611 (93.9) | ||
| Discharge status | Alive | 153 (48.3) | 711 (89.8) | <0.001 |
| Death | 164 (51.7) | 81 (10.2) | ||
| Cause of death ** | COVID-19 | 136 (93.4) | 0 (0) | <0.001 |
| Other causes | 9 (6.2) | 70 (100) |
| Characteristics | Case Patients (N = 337) n (%) | Controls (N = 695) n (%) | p-Value | |
|---|---|---|---|---|
| Number of received doses prior to hospital admission | Two doses | 18 (5.3) | 184 (26.5) | <0.001 |
| One dose | 45 (13.4) | 73 (10.5) | ||
| Zero doses | 274 (81.3) | 438 (63.0) | ||
| Vaccination status prior to confirmation/hospital admission | Fully vaccinated | 14 (4.2) | 143 (20.6) | <0.001 |
| Partially vaccinated | 24 (7.1) | 79 (11.4) | ||
| Within 14 days of first dose | 25 (7.4) | 35 (5.0) | ||
| Unvaccinated | 274 (81.3) | 438 (63.0) | ||
| Adverse events following first dose | No side effects | 41 (66.1) | 210 (81.7) | 0.002 |
| Minor side effects | 10 (16.1) | 34 (13.2) | ||
| Moderate side effects | 5 (8.1) | 10 (3.9) | ||
| Severe | 6 (9.7) | 3 (1.2) | ||
| Adverse events following second dose | No side effects | 12 (66.7) | 145 (80.6) | 0.13 |
| Minor side effects | 3 (16.7) | 26 (14.4) | ||
| Moderate side effects | 2 (11.1) | 5 (2.8) | ||
| Severe | 1 (5.5) | 4 (2.2) |
| Vaccination Status | Case Patients | Controls | Unadjusted OR (95% CI) | VE against COVID-19 Hospitalizations (95% CI) |
|---|---|---|---|---|
| Fully vaccinated | 14 (4.2) | 143 (20.6) | 0.16 (0.09–0.28) | 82 (69–90) * |
| Partially vaccinated | 24 (7.1) | 79 (11.4) | 0.49 (0.30–0.79) | 53 (23–71) ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farah, Z.; Haddad, N.; Abou El Naja, H.; Saleh, M.; Mrad, P.; Ghosn, N. Effectiveness of the Pfizer-BioNTech Vaccine against COVID-19-Associated Hospitalizations among Lebanese Adults ≥75 Years Old—Lebanon, April–May 2021. Epidemiologia 2023, 4, 212-222. https://doi.org/10.3390/epidemiologia4020022
Farah Z, Haddad N, Abou El Naja H, Saleh M, Mrad P, Ghosn N. Effectiveness of the Pfizer-BioNTech Vaccine against COVID-19-Associated Hospitalizations among Lebanese Adults ≥75 Years Old—Lebanon, April–May 2021. Epidemiologia. 2023; 4(2):212-222. https://doi.org/10.3390/epidemiologia4020022
Chicago/Turabian StyleFarah, Zeina, Nadine Haddad, Hala Abou El Naja, Majd Saleh, Pamela Mrad, and Nada Ghosn. 2023. "Effectiveness of the Pfizer-BioNTech Vaccine against COVID-19-Associated Hospitalizations among Lebanese Adults ≥75 Years Old—Lebanon, April–May 2021" Epidemiologia 4, no. 2: 212-222. https://doi.org/10.3390/epidemiologia4020022
APA StyleFarah, Z., Haddad, N., Abou El Naja, H., Saleh, M., Mrad, P., & Ghosn, N. (2023). Effectiveness of the Pfizer-BioNTech Vaccine against COVID-19-Associated Hospitalizations among Lebanese Adults ≥75 Years Old—Lebanon, April–May 2021. Epidemiologia, 4(2), 212-222. https://doi.org/10.3390/epidemiologia4020022






