Restrictions on Hospital Referrals from Long-Term Care Homes in Madrid and COVID-19 Mortality from March to June 2020: A Systematic Review of Studies Conducted in Spain
Abstract
:1. Introduction
1.1. The First Two Months of the COVID-19 Pandemic in Long-Term Care Homes in the Community of Madrid (Spain)
1.2. The Context of Healthcare for the LTCH Population in Spain in 2020
1.3. CoM Health Policy on LTCHs during the First Two Months of the COVID-19 Pandemic
1.4. Rationale and Aim of the Study
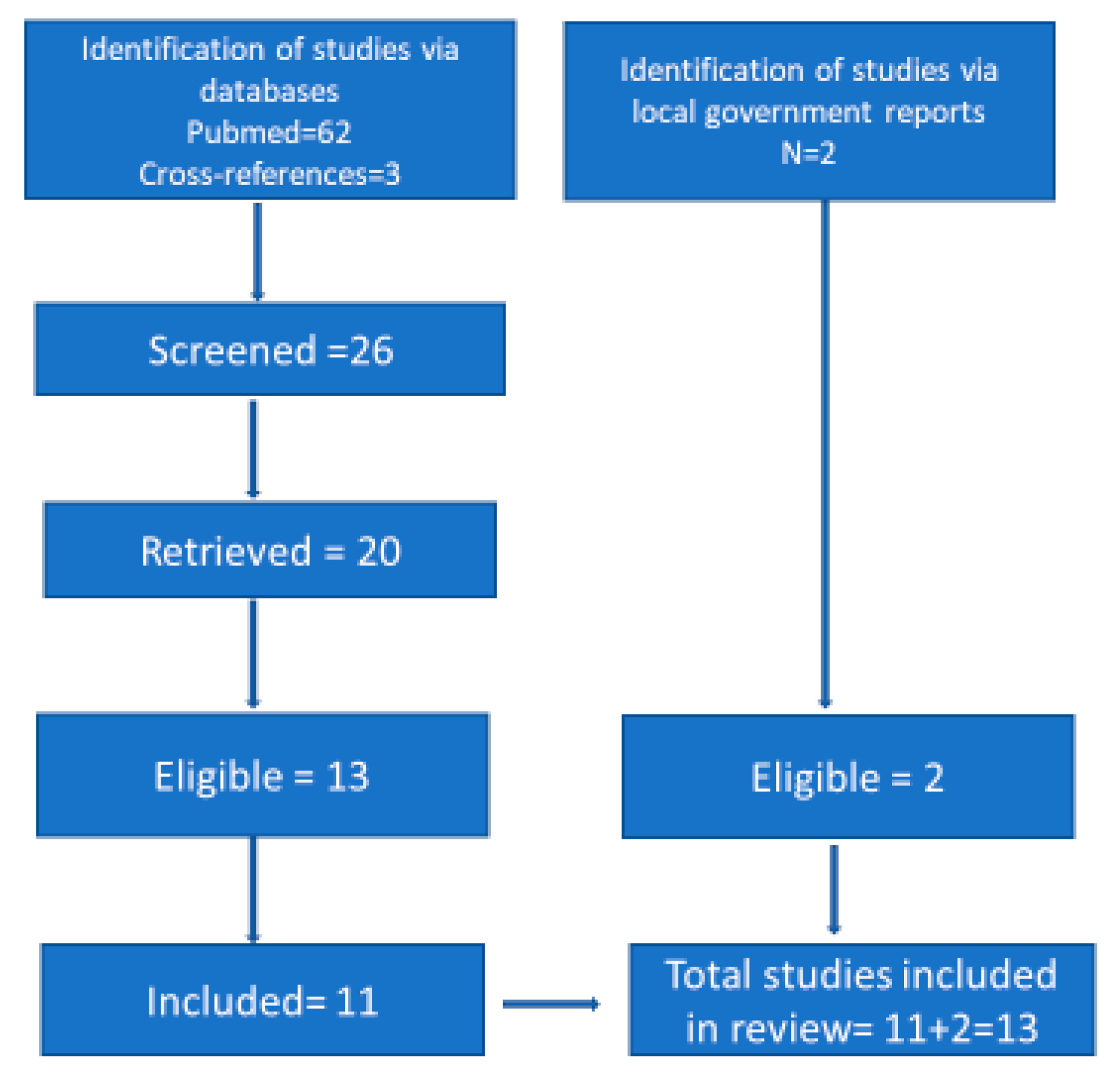
2. Materials and Methods
3. Results
3.1. Characteristics of the Studies
3.2. Hospital Referrals
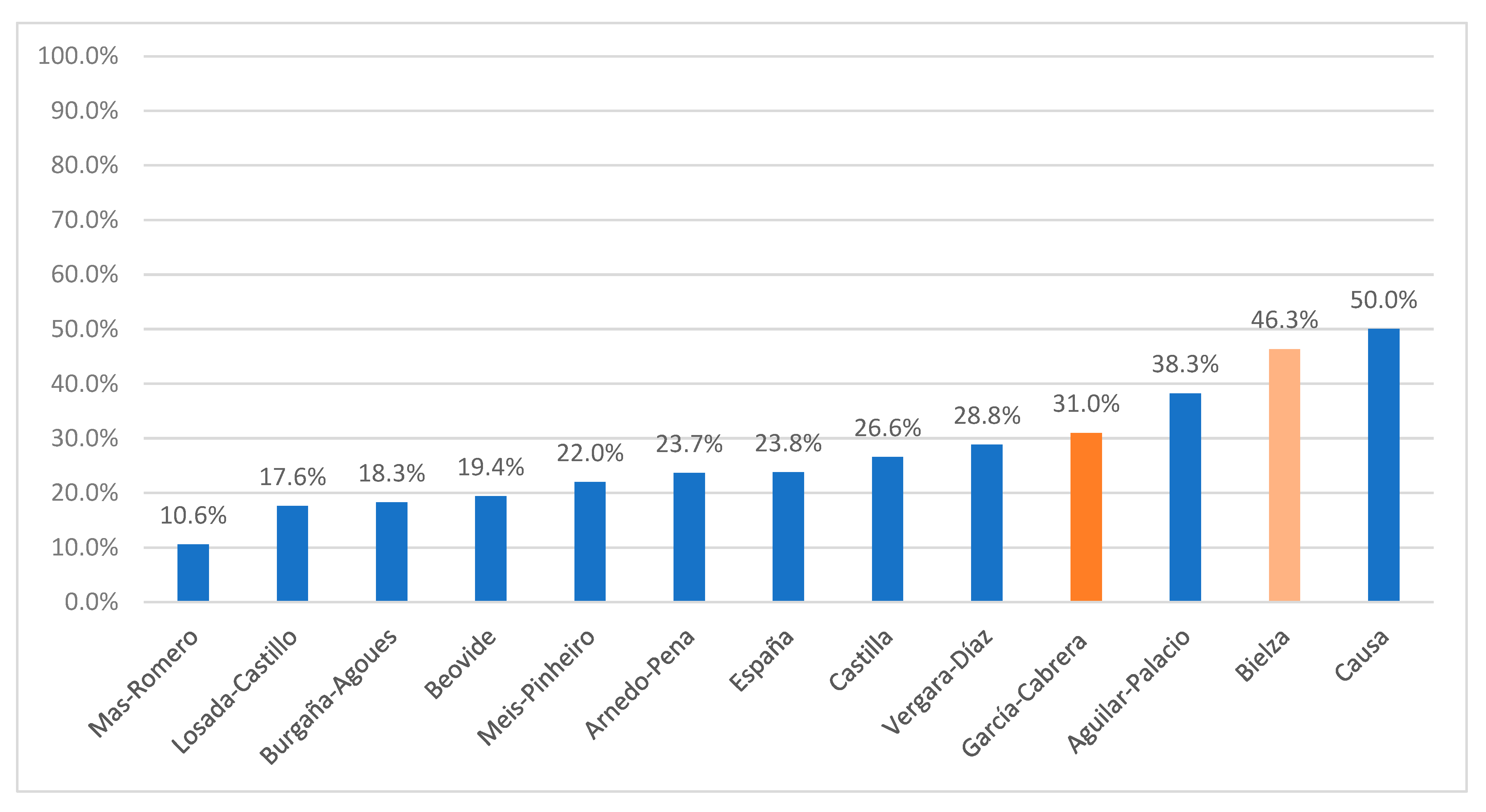
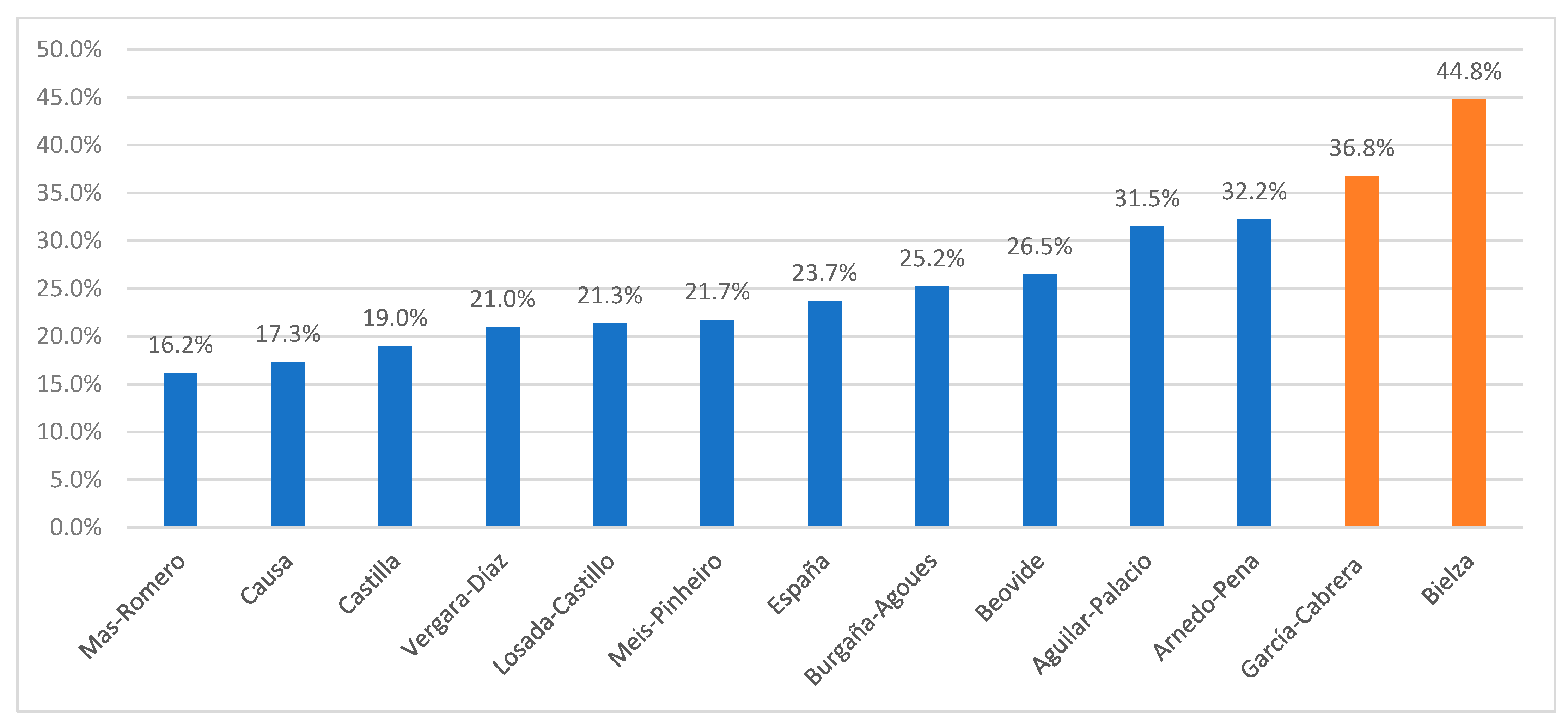
3.3. Total Mortality
3.4. Mortality among Residents Who Remained at an LTCH
3.5. In-Hospital Mortality
3.6. In-Hospital Mortality vs. In-LTCH Mortality
4. Discussion
4.1. Summary of Results
4.2. Comparison with International Literature and Interpretation of Results
4.3. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zunzunegui, M.V.; Rico, M.; Béland, F.; García-López, F.J. The Impact of Long-Term Care Home Ownership and Administration Type on All-Cause Mortality from March to April 2020 in Madrid, Spain. Epidemiologia 2022, 3, 323–336. [Google Scholar] [CrossRef] [PubMed]
- Condes, E.; Arribas, J.R. Impact of COVID-19 on Madrid hospital system. Enferm. Infecc. Microbiol. Clin. 2021, 39, 256–257. [Google Scholar] [CrossRef] [PubMed]
- La Comunidad de Madrid Pone en Marcha un Plan Histórico que Unirá la Sanidad Pública y Privada Bajo una Única Coordinación. Available online: https://www.comunidad.madrid/notas-prensa/2020/03/12/comunidad-madrid-pone-marcha-plan-historico-unira-sanidad-publica-privada-unica-coordinacion (accessed on 5 June 2023).
- Rico, M. Los Seis Documentos que Demuestran que Ayuso Miente Sobre la Orden de no Trasladar Enfermos de Residencias a Hospitales. Infolibre. 2020. Available online: https://www.infolibre.es/politica/seis-documentos-demuestran-ayuso-miente-orden-no-trasladar-enfermos-residencias-hospitales_1_1183785.html (accessed on 5 June 2023).
- Reyero Zubiri, A. Morirán de Forma Indigna; K.O. Ediciones: Madrid, Spain, 2022. [Google Scholar]
- Rico, M. Verguenza: El Escándalo de las Residencias; Planeta: Barcelona, Spain, 2021. [Google Scholar]
- Guzmán-García, M.B.; Mohedano-Moriano, A.; González-González, J.; Morales-Cano, J.M.; Campo-Linares, R.; Lozano-Suárez, C.; Estrada-Álvarez, T.P.; Romero-Fernández, M.M.; Aguilar-Galán, E.V.; Criado-Álvarez, J.J. Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia. J. Clin. Med. 2022, 11, 6420. [Google Scholar] [CrossRef] [PubMed]
- Bielza, R.; Sanz, J.; Zambrana, F.; Arias, E.; Malmierca, E.; Portillo, L.; Thuissard, I.J.; Lung, A.; Neira, M.; Moral, M.; et al. Clinical Characteristics, Frailty, and Mortality of Residents With COVID-19 in Nursing Homes of a Region of Madrid. J. Am. Med. Dir. Assoc. 2021, 22, 245–252.e2. [Google Scholar] [CrossRef] [PubMed]
- García-Cabrera, L.; Pérez-Abascal, N.; Montero-Errasquín, B.; Rexach Cano, L.; Mateos-Nozal, J.; Cruz-Jentoft, A. Characteristics, hospital referrals and 60-day mortality of older patients living in nursing homes with COVID-19 assessed by a liaison geriatric team during the first wave: A research article. BMC Geriatr. 2021, 21, 610. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Palacio, I.; Maldonado, L.; Marcos-Campos, I.; Castel-Feced, S.; Malo, S.; Aibar, C.; Rabanaque, M. Understanding the COVID-19 Pandemic in Nursing Homes (Aragón, Spain): Sociodemographic and Clinical Factors Associated with Hospitalization and Mortality. Front. Public Health 2022, 10, 928174. [Google Scholar] [CrossRef] [PubMed]
- Arnedo-Pena, A.; Romeu-García, M.A.; Gascó-Laborda, J.C.; Meseguer-Ferrer, N.; Safont-Adsuara, L.; Prades-Vila, L.; Flores-Medina, M.; Rusen, V.; Tirado-Balaguer, M.D.; Sabater-Vidal, S.; et al. Incidence, Mortality, and Risk Factors of COVID-19 in Nursing Homes. Epidemiologia 2022, 3, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Beobide Telleria, I.; Ferro Uriguen, A.; Laso Lucas, E.; Sannino Menicucci, C.; Enriquez Barroso, M.; López de Munain Arregui, A. Risk factors associated with COVID-19 infection and mortality in nursing homes. Aten. Primaria 2022, 54, 102463. [Google Scholar] [CrossRef]
- Burgaña Agoües, A.; Serra Gallego, M.; Hernández Resa, R.; Joven Llorente, B.; Lloret Arabi, M.; Ortiz Rodriguez, J.; Acebal, H.P.; Hernández, M.C.; Ayala, I.C.; Calero, P.P.; et al. Risk factors for COVID-19 morbidity and mortality in institutionalised elderly people. Int. J. Environ. Res. Public Health 2021, 18, 10221. [Google Scholar] [CrossRef] [PubMed]
- Causa, R.; Nievas, D.A.; Bermúdez Tamayo, C. COVID-19 y dependencia funcional: Análisis de un brote en un centro sociosanitario de personas mayores. Rev. Esp. Salud Pública 2021, 95, e1–e12. [Google Scholar]
- España, P.P.; Bilbao, A.; García-Gutiérrez, S.; Lafuente, I.; Anton-Ladislao, A.; Villanueva, A.; Uranga, A.; Legarreta, M.J.; Aguirre, U.; Quintana, J.M.; et al. Predictors of mortality of COVID-19 in the general population and nursing homes. Intern. Emerg Med. 2021, 16, 1487–1496. [Google Scholar] [CrossRef] [PubMed]
- Losada-Castillo, I.; Santiago-Pérez, M.I.; Naveira-Barbeito, G.; Otero-Barros, M.T.; Pérez-Martínez, O.; Zubizarreta-Alberdi, R. Impact of COVID-19 pandemic in terms of incidence and lethality in nursing homes in Galicia (Spain). Rev. Esp. Geriatr. Gerontol. 2022, 57, 337. [Google Scholar] [CrossRef]
- Mas Romero, M.; Avendaño Céspedes, A.; Tabernero Sahuquillo, M.T.; Cortés Zamora, E.B.; Gómez Ballesteros, C.; Sánchez-Flor Alfaro, V.; Bru, R.L.; Utiel, M.L.; Cifuentes, S.C.; Longobardo, L.M.P.; et al. COVID-19 outbreak in long-term care facilities from Spain. Many lessons to learn. PLoS ONE 2020, 15, e0241030. [Google Scholar] [CrossRef] [PubMed]
- Meis-Pinheiro, U.; Lopez-Segui, F.; Walsh, S.; Ussi, A.; Santaeugenia, S.; García-Navarro, J.A.; San-Jose, A.; Andreu, A.L.; Campins, M.; Almirante, B. Clinical characteristics of COVID-19 in older adults. A retrospective study in long-term nursing homes in Catalonia. PLoS ONE 2021, 16, e0255141. [Google Scholar] [CrossRef] [PubMed]
- Vergara-Diaz, A.; Forcada Falcón, M. Análisis de Brotes Declarados en Residencias de Mayores por Coronavirus SARS-CoV-2 en Andalucía 2020. Sistema de Vigilancia Epidemiológica de Andalucía 2020, 25. Available online: https://www.repositoriosalud.es/handle/10668/3138 (accessed on 5 June 2023).
- Castilla, J. Vigilancia Epidemiológica en Navarra. 2020. Available online: http://www.navarra.es/NR/rdonlyres/3855C06B-B6A2-4E05-BA57-034AB7947A04/477682/InformesEpidemiologicos_2020pp.pdf (accessed on 27 January 2023).
- Zhang, X.S.; Charland, K.; Quach, C.; Nguyen, Q.D.; Zinszer, K. Institutional, therapeutic, and individual factors associated with 30-day mortality after COVID-19 diagnosis in Canadian long-term care facilities. J. Am. Geriatr. Soc. 2022, 70, 3210–3220. [Google Scholar] [CrossRef] [PubMed]
- Marin-Gomez, F.X.; Mendioroz-Peña, J.; Mayer, M.A.; Méndez-Boo, L.; Mora, N.; Hermosilla, E.; Coma, E.; Vilaseca, J.-M.; Leis, A.; Medina, M.; et al. Comparing the clinical characteristics and mortality of residential and non-residential older people with COVID-19: Retrospective observational study. Int. J. Environ. Res. Public Health 2022, 19, 483. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Precision shielding for COVID-19: Metrics of assessment and feasibility of deployment. BMJ Glob. Health 2021, 6, e004614. [Google Scholar] [CrossRef] [PubMed]
- Fernández, M. Pelea por Dinero en la Sanidad Privada. Available online: https://elpais.com/economia/2020-04-17/pelea-por-dinero-en-la-sanidad-privada.html (accessed on 24 May 2023).
- Peinado, F. Los Días Más Duros de los Geriatras de Madrid. Available online: https://elpais.com/espana/madrid/2020-06-12/los-dias-mas-duros-de-los-geriatras-de-madrid.html (accessed on 24 May 2023).
- Guide Pour la Prise en Charge des Résidents en Centres D’hébergement et de Soins de Longue Durée (CHSLD) Dans le Contexte de la Pandémie de la COVID-19. Available online: https://santesaglac.gouv.qc.ca/medias/2020/04/20-MS-02502-61_Guide_CHSLD_13_avril.pdf (accessed on 24 May 2023).
- Rueda, J. Ageism in the COVID-19 pandemic: Age-based discrimination in triage decisions and beyond. Hist. Philos. Life Sci. 2021, 43, 91. [Google Scholar] [CrossRef] [PubMed]
- Scully, J.L. Disability, Disablism, and COVID-19 Pandemic Triage. Bioethical Inq. 2020, 17, 601–605. [Google Scholar] [CrossRef] [PubMed]
| Criteria for Hospital Referral of Patients with Respiratory Conditions: | |
|---|---|
| March 18 | Hospital referral will proceed if the patient fulfills the following criteria: |
| |
| March 20 | Exclusion criteria for hospital referral of patients with respiratory conditions: |
| |
| March 24 | Exclusion recommendations for hospital referral of patients with a respiratory condition: |
| |
| March 25 | Recommendations for hospital referral of patients with a respiratory condition: |
Taking into account the presence of symptoms, assessment of emergency care availability at the hospital, and prioritization of care at the LTCH, the patient should be transferred if they fulfill the following criteria after clinical assessment:
|
| First Author | Geographical Area | Confirmed/Clinical Cases | Period | No. of Hospitals in Geographical Area (GA) | Dependency | Cognitive Impairment |
|---|---|---|---|---|---|---|
| Bielza | CoM | Confirmed/clinical | 20 March–1 June 2020 | One | 75% | 50% |
| García Cabrera | CoM | Confirmed/clinical | 30 March–30 April 2020 | One | 64% | 44% |
| Aguilar-Palacio | Aragon | Confirmed | March 2020–March 2021 | All in GA | UNK | 36% dementia |
| Arnedo Pena | Castellon | Confirmed | March–May 2020 | Two | 78% | UNK |
| Beobide-Tellería | Guipuzcoa | Confirmed | March–December 2020 | All in GA | 75% | 55% |
| Burgaña-Agoues | Cugat del Valles | Confirmed | 15 March–15 May 2020 | One | 64% | 72% |
| Causa | Granada | Confirmed | 13 March–20 June 2020 | One | 60% | 61% |
| España | Basque Country | Confirmed | February–22 May 2020 | All in GA | UNK | 33% dementia |
| Losada-Castillo | Galicia | Confirmed | 1 March–12 June 2020 | All in GA | UNK | UNK |
| Mas-Romero | Albacete | Confirmed/Clinical | 6 March–5 April 2020 | One | 50% | 22% dementia |
| Meis-Pinheiro | Catalonia | Confirmed | March–May 2020 | Several | UNK | 59% dementia |
| Vergara- Díaz | Andalusia | Confirmed | 28 February–May 2020 | All in GA | UNK | UNK |
| Castilla | Navarre | Confirmed | March–15 May 2020 | All in GA | UNK | UNK |
| First Author | Geographical Area | COVID-19 Cases | Mortality N (%) | Hospitalization N (%) | In-Hospital Mortality N (%) | In-LTCH Mortality N (%) | Mortality Ratio (Hospital/ LTCH) (95% CI) |
|---|---|---|---|---|---|---|---|
| Bielza | CoM | 630 | 282 (44.8%) | 292 (46.3%) | 124 (42.5%) | 158 (46.7%) | 0.9 (0.8; 1.1) |
| García-Cabrera | 419 | 154 (36.7%) | 130 (31.0%) | 36 (27.7%) | 118 (40.8%) | 0.68 (0.5; 0.9) | |
| Arnedo-Pena | Castellon | 304 | 98 (32.2%) | 72 (23.7%) | 38 (52.8%) | 60 (25.9%) | 2.0 (1.5; 2.8) |
| Burgaña-Agoues | Sant Cugat del Valles | 345 | 87 (25.0%) | 63 (18.2%) | 21 (33.3%) | 66 (23.4%) | 1.4 (0.9; 2.1) |
| Meis-Pinheiro | Catalonia | 2092 | 455 (21.7%) | 460 (22.0) | 148 (32.1%) | 307 (18.8%) | 1.7 (1.4; 2.0) |
| Aguilar-Palacios ** | Aragon | 4632 | 1458 (31.5%) | 1772 (38.3%) | 935 (52.8%) | 523 (18.3%) | 2.9 (2.6; 3.2) |
| Beobide ** | Guipuzcoa | 170 | 45 (26.4%) | 33 (19.4%) | 22 (66.6%) | 23 (16.8%) | 4.0 (2.5; 6.2) |
| España | Basque Country | 2140 | 507 (23.7%) | 510 (23.8%) | 257 (50.4%) | 250 (15.3%) | 3.3 (2.8; 3.8) |
| Castilla | Navarre | 1483 | 301 (20.3%) | 429 (28.9%) | 155 (36.1) | 146 (13.8%) | 2.6 (2.1; 3.2) |
| Mas-Romero | Albacete | 198 | 32 (16.2%) | 21 (10.1%) | 11 (52.4%) | 21 (11.9%) | 4.4 (2.5; 7.8) |
| Losada- Castillo | Galicia | 1276 | 272 (21.3%) | 225 (17.6%) | 141 (62.7%) | 131 (12.5%) | 5.0 (4.2; 6.1) |
| Vergara- Díaz | Andalusia | 2581 | 541 (21.0%) | 744 (28.8%) | 340 (45.7%) | 201 (10.9%) | 4.2 (3.6; 4.9) |
| Causa | Granada | 52 | 9 (17.3) | 26 (50%) | 7 (26.9%) | 2 (7.7%) | 3.5 (0.8; 15.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zunzunegui, M.V.; Béland, F.; García López, F.J. Restrictions on Hospital Referrals from Long-Term Care Homes in Madrid and COVID-19 Mortality from March to June 2020: A Systematic Review of Studies Conducted in Spain. Epidemiologia 2023, 4, 176-187. https://doi.org/10.3390/epidemiologia4020019
Zunzunegui MV, Béland F, García López FJ. Restrictions on Hospital Referrals from Long-Term Care Homes in Madrid and COVID-19 Mortality from March to June 2020: A Systematic Review of Studies Conducted in Spain. Epidemiologia. 2023; 4(2):176-187. https://doi.org/10.3390/epidemiologia4020019
Chicago/Turabian StyleZunzunegui, Maria Victoria, François Béland, and Fernando J. García López. 2023. "Restrictions on Hospital Referrals from Long-Term Care Homes in Madrid and COVID-19 Mortality from March to June 2020: A Systematic Review of Studies Conducted in Spain" Epidemiologia 4, no. 2: 176-187. https://doi.org/10.3390/epidemiologia4020019
APA StyleZunzunegui, M. V., Béland, F., & García López, F. J. (2023). Restrictions on Hospital Referrals from Long-Term Care Homes in Madrid and COVID-19 Mortality from March to June 2020: A Systematic Review of Studies Conducted in Spain. Epidemiologia, 4(2), 176-187. https://doi.org/10.3390/epidemiologia4020019






