Use of Complementary and Alternative Medicine and Its Relationship with Health-Related Quality of Life (HRQOL) in Patients with Type 2 Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. CAM
2.3. HRQOL
2.4. Clinical Parameters
2.5. Statistical Analysis
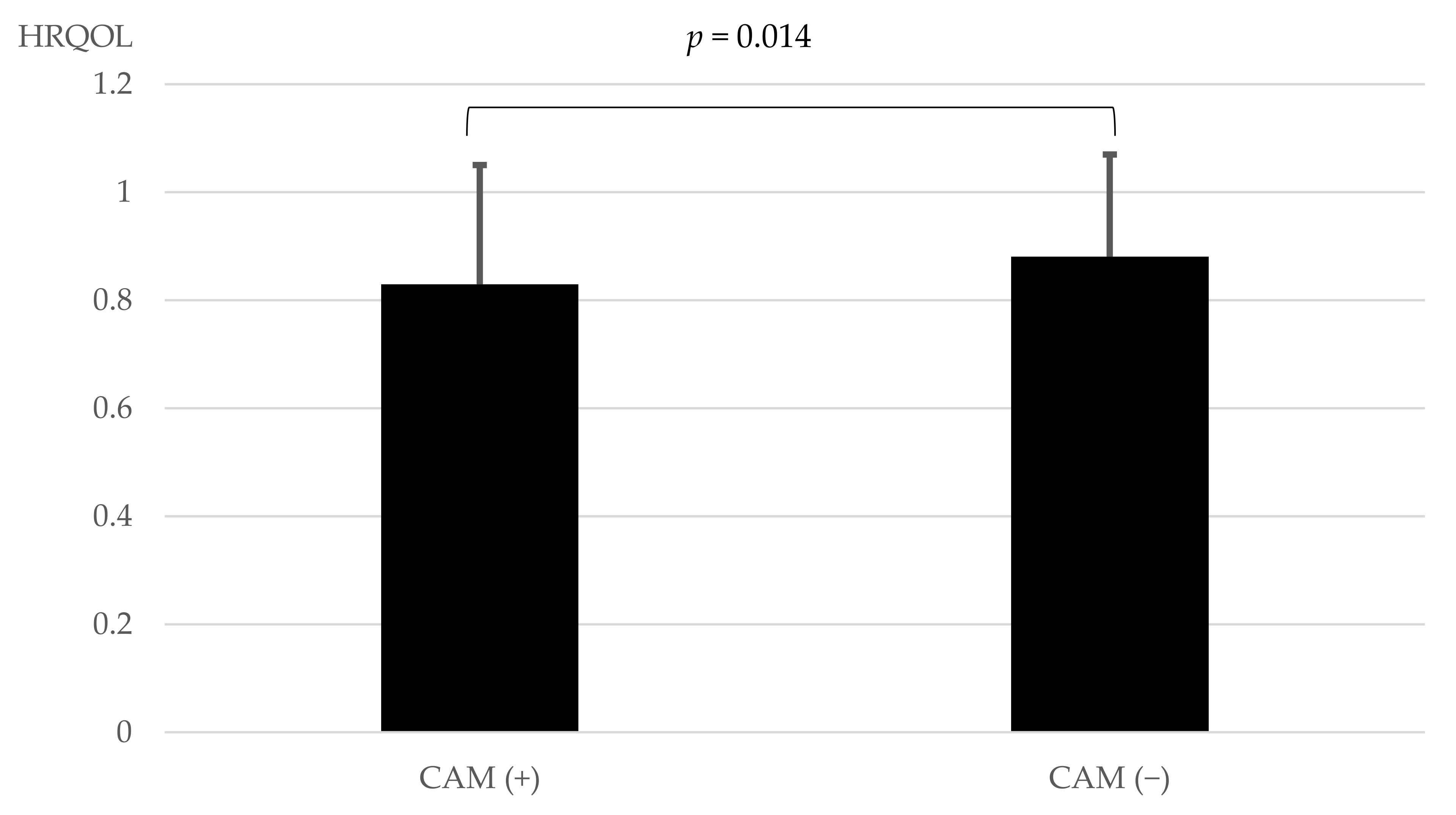
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health, Labor and Welfare in 2019, Japan. Available online: https://www.mhlw.go.jp/stf/newpage_14156.html (accessed on 1 October 2022). (In Japanese)
- The Japan Diabetes Society. Fourth Five-Year Strategic Plan Against Diabetes Mellitus. Available online: http://www.fa.kyorin.co.jp/jds/uploads/plan_5years_4th.pdf (accessed on 1 October 2022). (In Japanese).
- National Cancer Institute at the National Institutes of Health. Complementary and Alternative Medicine. Available online: https://www.cancer.gov/about-cancer/treatment/cam. (accessed on 1 October 2022).
- Zhang, L.; Cheng, Y.; Li, H.; Zhou, Y.; Sun, B.; Xu, L. Meta-analysis of randomized controlled trials on the efficacy of daikenchuto on improving intestinal dysfunction after abdominal surgery. Ann. Surg. Treat. Res. 2018, 95, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Kono, T.; Shimada, M.; Nishi, M.; Morine, Y.; Yoshikawa, K.; Katsuno, H.; Maeda, K.; Koeda, K.; Morita, S.; Watanabe, M.; et al. Daikenchuto accelerates the recovery from prolonged postoperative ileus after open abdominal surgery: A subgroup analysis of three randomized controlled trials. Surg. Today 2019, 49, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Ishizuka, M.; Shibuya, N.; Nagata, H.; Takagi, K.; Iwasaki, Y.; Hachiya, H.; Aoki, T.; Kubota, K. Perioperative administration of traditional Japanese medicine daikenchuto relieves postoperative ileus in patients undergoing surgery for gastrointestinal cancer: A systemic review and meta-analysis. Anticancer Res. 2017, 37, 5967–5974. [Google Scholar] [PubMed]
- Matsunaga, S.; Kishi, T.; Iwata, N. Yokukansan in the treatment of behavioral and psychological symptoms of dementia: An updated meta-analysis of randomized controlled trials. J. Alzheimer’s Dis. 2016, 54, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Imai, H.; Takeshima, N.; Oda, H.; Chen, P.; Sawada, E.; Furukawa, T.A. Choto-san versus placebo for patients with dementia: Systematic review and meta-analysis. Psychogeriatrics 2017, 17, 466–478. [Google Scholar] [CrossRef]
- Matsuda, Y.; Kishi, T.; Shibayama, H.; Iwata, N. Yokukansan in the treatment of behavioral and psychological symptoms of dementia: A systematic review and meta-analysis of randomized controlled trials. Hum. Psychopharmacol. 2013, 28, 80–86. [Google Scholar] [CrossRef]
- Shimoichi, Y.; Haruki, J.; Wakayama, I. Acupuncture for patients with lower back pain -Systematic review of randomized trials conducted in Japan. J. Jpn. Soc. Acupunct. Moxibustion 2014, 64, 37–53. [Google Scholar]
- Eisenberg, D.M.; Davis, R.B.; Ettner, S.L.; Appel, S.; Wilkey, S.; Van Rompay, M.; Kessler, R.C. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA 1998, 280, 1569–1575. [Google Scholar] [CrossRef]
- Clarke, T.C.; Black, L.I.; Stussman, B.J.; Barnes, P.M.; Nahin, R.L. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl. Health Stat. Rep. 2015, 79, 1–16. [Google Scholar]
- Misawa, J. Influence of psychosocial factors on the use of complementary and alternative medicine. J. Health Welf. Stat. 2011, 58, 1–7. [Google Scholar]
- Ishibashi, Y.; Horiguti, I.; Kawaminami, K.; Kigawa, M.; Marui, E. Use of Integrative Medicine in Japan. J. Health Welf. Stat. 2016, 63, 25–30. [Google Scholar]
- Yamashita, H.; Tsukayama, H.; Sugishita, C. Popularity of complementary and alternative medicine in Japan: A telephone survey. Complement. Ther. Med. 2002, 10, 84–92. [Google Scholar] [CrossRef]
- Fukuda, S.; Watanabe, E.; Ono, N.; Tsubouchi, M.; Shirakawa, T. Use of complementary and alternative medicine and health problems. Jpn. J. Public Health 2006, 53, 293–300. [Google Scholar]
- Mukai, J.; Kanamori, A.; Hiratsuka, Y.; Shimada, K.; Otori, K.; Koichiro Atsuda, K. Overview of Complementary and Alternative Medicine in Diabetes Patients and Clinical Factors Affecting the Adoption of Food for Specified Health Uses: A Questionnaire-Based Survey. J. Jpn. Diab. Soc. 2017, 60, 65–74. [Google Scholar]
- Ministry of Health, Labor and Welfare in 2019, Japan. Survey and Research on the Need for the Dissemination of Information on Integrative Medicine. Available online: https://www.mhlw.go.jp/stf/shingi/2r9852000002vsub-att/2r9852000002vsy2.pdf (accessed on 1 October 2022). (In Japanese)
- Japanese EuroQol Translation Team. The development of the Japanese EuroQol Instrument. J. Health Soc. 1998, 8, 109–123. (In Japanese) [Google Scholar]
- Yapp, L.Z.; Scott, C.E.H.; Howie, C.R.; MacDonald, D.J.; Simpson, A.H.R.W.; Clement, N.D. Meaningful values of the EQ-5D-3L in patients undergoing primary knee arthroplasty. Bone Jt. Res. 2022, 11, 619–628. [Google Scholar] [CrossRef]
- Zare, F.; Ameri, H.; Madadizadeh, F.; Aghaei, M.R. Validity and reliability of the EQ-5D-3L (a generic preference-based instrument used for calculating quality-adjusted life-years) for patients with type 2 diabetes in Iran. Diabetes Metab. Syndr. 2021, 15, 319–324. [Google Scholar] [CrossRef]
- Yokoyama, H.; Hishida, A. Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar]
- Radwan, H.; Hasan, H.; Hamadeh, R.; Hashim, M.; AbdulWahid, Z.; Hassanzadeh Gerashi, M.; Al Hilali, M.; Naja, F. Complementary and alternative medicine use among patients with type 2 diabetes living in the United Arab Emirates. BMC Complement. Ther. Med. 2020, 20, 216. [Google Scholar] [CrossRef]
- Yıldırım, D.İ.; Marakoğlu, K. Complementary and alternative medicine use amongst Turkish type 2 diabetic patients: A cross-sectional study. Complement. Ther. Med. 2018, 41, 41–46. [Google Scholar] [CrossRef]
- Huo, N.; Ray, G.E.; Mehta, S.; LoBello, S.G. Complementary and alternative medicine use among people with asthma and health-related quality of life. J. Asthma 2015, 52, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Opheim, R.; Lie Høivik, M.; Bernklev, T.; Jelsness-Jørgensen, L.P.; Moum, B. The Use of Complementary and Alternative Medicine among Patients with Inflammatory Bowel Disease Is Associated with Reduced Health-Related Quality of Life. Gastroenterol. Res. Pract. 2016, 6, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Rhee, T.G.; Pawloski, P.A.; Parsons, H.M. Health-related quality of life among US adults with cancer: Potential roles of complementary and alternative medicine for health promotion and well-being. Psychooncology 2019, 28, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Beatty, L.J.; Adams, J.; Sibbritt, D.; Wade, T.D. Evaluating the impact of cancer on complementary and alternative medicine use, distress and health related QoL among Australian women: A prospective longitudinal investigation. Complement. Med. Ther. 2012, 20, 61–69. [Google Scholar] [CrossRef]
- Lu, C.L.; Liu, X.H.; Stub, T.; Kristoffersen, A.E.; Liang, S.B.; Wang, X.; Bai, X.; Norheim, A.J.; Musial, F.; Alræk, T.; et al. Complementary and alternative medicine for patients with chronic fatigue syndrome: A systematic review. BMC Complement. Altern. Med. 2018, 18, 260. [Google Scholar]
| Total | |||
|---|---|---|---|
| Mean ± SD | Minimum | Maximum | |
| Number of subjects | 421 | ||
| Age (years) | 67.3 ± 12.8 | 17.0 | 92.0 |
| Height (cm) | 161.8 ± 9.6 | 134.2 | 190.0 |
| Body weight (kg) | 66.7 ± 15.3 | 38.4 | 138.0 |
| Body mass index (kg/m2) | 25.3 ± 4.6 | 16.1 | 46.4 |
| Duration of diabetes (day) | 5863.9 ± 3711.7 | 0.0 | 17,854.0 |
| Albumin (g/mL) | 4.1 ± 0.5 | 2.0 | 5.3 |
| Triglycerides (mg/dL) | 190.4 ± 144.3 | 34.0 | 1630.0 |
| LDL cholesterol (mg/dL) | 103.9 ± 30.9 | 25.0 | 195.0 |
| HDL cholesterol (mg/dL) | 54.4 ± 15 | 9.0 | 105.0 |
| HbA1c (%) | 7.5 ± 1.5 | 4.0 | 13.5 |
| Blood glucose (mg/dL) | 165.9 ± 62.3 | 54.0 | 428.0 |
| Serum creatinine (mg/dL) | 1.0 ± 0.7 | 0.5 | 10.5 |
| eGFR (mL/min/1.73m2) | 61.3 ± 19.6 | 4.4 | 115.4 |
| HRQOL | 0.860 ± 0.200 | −0.290 | 1.000 |
| Use of Insulin (the number of subjects) | 195 (46.3%) | ||
| Use of oral hypoglycemic agents (the number of subjects) | 342 (81.2%) | ||
| Oral hypoglycemic agents: 1 Tablet | 126 | ||
| Oral hypoglycemic agents: 2 Tablets | 119 | ||
| Oral hypoglycemic agents: 3 Tablets | 70 | ||
| Oral hypoglycemic agents: ≥4 Tablets | 27 | ||
| I Have Used and Still Use. | I Have Used, but I Do Not Use It Now. | I Have Never Used It. | I Do Not Remember and/or Do Not Know. | |||||
|---|---|---|---|---|---|---|---|---|
| Subjects | % | Subjects | % | Subjects | % | Subjects | % | |
| Supplements and/or Health Foods | 112 | 26.6 | 56 | 13.3 | 248 | 58.9 | 5 | 1.2 |
| Massage | 49 | 11.6 | 68 | 16.2 | 299 | 71.0 | 5 | 1.2 |
| Osteopathy | 36 | 8.6 | 67 | 15.9 | 315 | 74.8 | 3 | 0.7 |
| Spa therapy | 19 | 4.5 | 11 | 2.6 | 386 | 91.7 | 5 | 1.2 |
| Aromatherapy | 6 | 1.4 | 8 | 1.9 | 402 | 95.5 | 5 | 1.2 |
| Kampo | 33 | 7.8 | 34 | 8.1 | 347 | 82.4 | 7 | 1.7 |
| Acupuncture and/or Moxibustion | 12 | 2.9 | 38 | 9.0 | 366 | 86.9 | 5 | 1.2 |
| Yoga | 10 | 2.4 | 14 | 3.3 | 393 | 93.3 | 4 | 1.0 |
| Bone grafting | 13 | 3.1 | 40 | 9.5 | 366 | 86.9 | 2 | 0.5 |
| Chiropractic therapy | 4 | 1.0 | 21 | 5.0 | 388 | 92.2 | 8 | 1.9 |
| Magnetic therapy | 9 | 2.1 | 10 | 2.4 | 396 | 94.1 | 6 | 1.4 |
| Forest therapy | 1 | 0.2 | 5 | 1.2 | 408 | 96.9 | 7 | 1.7 |
| Music therapy | 2 | 0.5 | 4 | 1.0 | 409 | 97.1 | 6 | 1.4 |
| Thermotherapy | 3 | 0.7 | 5 | 1.2 | 406 | 96.4 | 7 | 1.7 |
| Qigong | 2 | 0.5 | 2 | 0.5 | 410 | 97.4 | 7 | 1.7 |
| Fasting therapy | 3 | 0.7 | 6 | 1.4 | 407 | 96.7 | 5 | 1.2 |
| Ayurveda | 1 | 0.2 | 1 | 0.2 | 408 | 96.9 | 11 | 2.6 |
| Homeopathy | 2 | 0.5 | 1 | 0.2 | 408 | 96.9 | 10 | 2.4 |
| CAM (+) | CAM (−) | p | |||
|---|---|---|---|---|---|
| Subjects | Mean ± SD | Subjects | Mean ± SD | ||
| Supplements and/or Health Foods | 112 | 0.838 ± 0.217 | 309 | 0.869 ± 0.198 | 0.141 |
| Massage | 49 | 0.811 ± 0.235 | 372 | 0.868 ± 0.198 | 0.080 |
| Osteopathy | 36 | 0.825 ± 0.230 | 385 | 0.864 ± 0.201 | 0.273 |
| Spa therapy | 19 | 0.779 ± 0.221 | 402 | 0.865 ± 0.202 | 0.029 |
| Aromatherapy | 6 | 0.846 ± 0.122 | 415 | 0.861 ± 0.204 | 0.345 |
| Kampo | 33 | 0.780 ± 0.212 | 388 | 0.868 ± 0.201 | 0.001 |
| Acupuncture and/or Moxibustion | 12 | 0.849 ± 0.158 | 409 | 0.861 ± 0.205 | 0.470 |
| Yoga | 10 | 0.849 ± 0.175 | 411 | 0.861 ± 0.204 | 0.580 |
| Bone grafting | 13 | 0.756 ± 0.267 | 408 | 0.864 ± 0.200 | 0.094 |
| Chiropractic therapy | 4 | 0.673 ± 0.108 | 417 | 0.863 ± 0.203 | 0.008 |
| Magnetic therapy | 9 | 0.679 ± 0.255 | 412 | 0.865 ± 0.201 | 0.007 |
| Forest therapy | 1 | 0.796 ± − | 420 | 0.861 ± 0.204 | – |
| Music therapy | 2 | 0.692 ± 0.105 | 419 | 0.862 ± 0.203 | 0.083 |
| Thermotherapy | 3 | 0.559 ± 0.273 | 418 | 0.863 ± 0.202 | 0.016 |
| Qigong | 2 | 0.898 ± 0.144 | 419 | 0.861 ± 0.204 | 0.998 |
| Fasting therapy | 3 | 0.617 ± 0.497 | 418 | 0.863 ± 0.200 | 0.280 |
| Ayurveda | 1 | 0.796 ± − | 420 | 0.861 ± 0.204 | – |
| Homeopathy | 2 | 0.708 ± 0.124 | 419 | 0.862 ± 0.203 | 0.093 |
| CAM (+) | CAM (−) | p | |
|---|---|---|---|
| Total | 161 | 260 | |
| Men | 81 | 166 | 0.006c |
| Women | 80 | 94 | |
| Age (years) * | 66.6 ± 13.1 * | 67.7 ± 12.5 * | 0.398 b |
| Body mass index (kg/m2) * | 25.5 ± 4.8 * | 25.3 ± 4.5 * | 0.709 b |
| Duration of diabetes (day) * | 5807.0 ± 3412.6 * | 5899.2 ± 3352.3 * | 0.846 b |
| Albumin (g/mL) * | 4.1 ± 0.5 * | 4.1 ± 0.4 * | 0.488 b |
| HbA1c (%) * | 7.5 ± 1.6 * | 7.5 ± 1.4 * | 0.421 b |
| eGFR (mL/min/1.73m2) * | 59.8 ± 20.4 * | 62.3 ± 19.0 * | 0.212 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mori, Y.; Daikuhara, H.; Oshima, T.; Suzuki, H.; Okada, S.; Miyatake, N. Use of Complementary and Alternative Medicine and Its Relationship with Health-Related Quality of Life (HRQOL) in Patients with Type 2 Diabetes Mellitus. Epidemiologia 2023, 4, 53-59. https://doi.org/10.3390/epidemiologia4010005
Mori Y, Daikuhara H, Oshima T, Suzuki H, Okada S, Miyatake N. Use of Complementary and Alternative Medicine and Its Relationship with Health-Related Quality of Life (HRQOL) in Patients with Type 2 Diabetes Mellitus. Epidemiologia. 2023; 4(1):53-59. https://doi.org/10.3390/epidemiologia4010005
Chicago/Turabian StyleMori, Yoshiro, Hiroyuki Daikuhara, Tomie Oshima, Hiromi Suzuki, Setsuo Okada, and Nobuyuki Miyatake. 2023. "Use of Complementary and Alternative Medicine and Its Relationship with Health-Related Quality of Life (HRQOL) in Patients with Type 2 Diabetes Mellitus" Epidemiologia 4, no. 1: 53-59. https://doi.org/10.3390/epidemiologia4010005
APA StyleMori, Y., Daikuhara, H., Oshima, T., Suzuki, H., Okada, S., & Miyatake, N. (2023). Use of Complementary and Alternative Medicine and Its Relationship with Health-Related Quality of Life (HRQOL) in Patients with Type 2 Diabetes Mellitus. Epidemiologia, 4(1), 53-59. https://doi.org/10.3390/epidemiologia4010005





