Future Strategic Priorities of the Swiss Decentralized Healthcare System: A COVID-19 Case Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
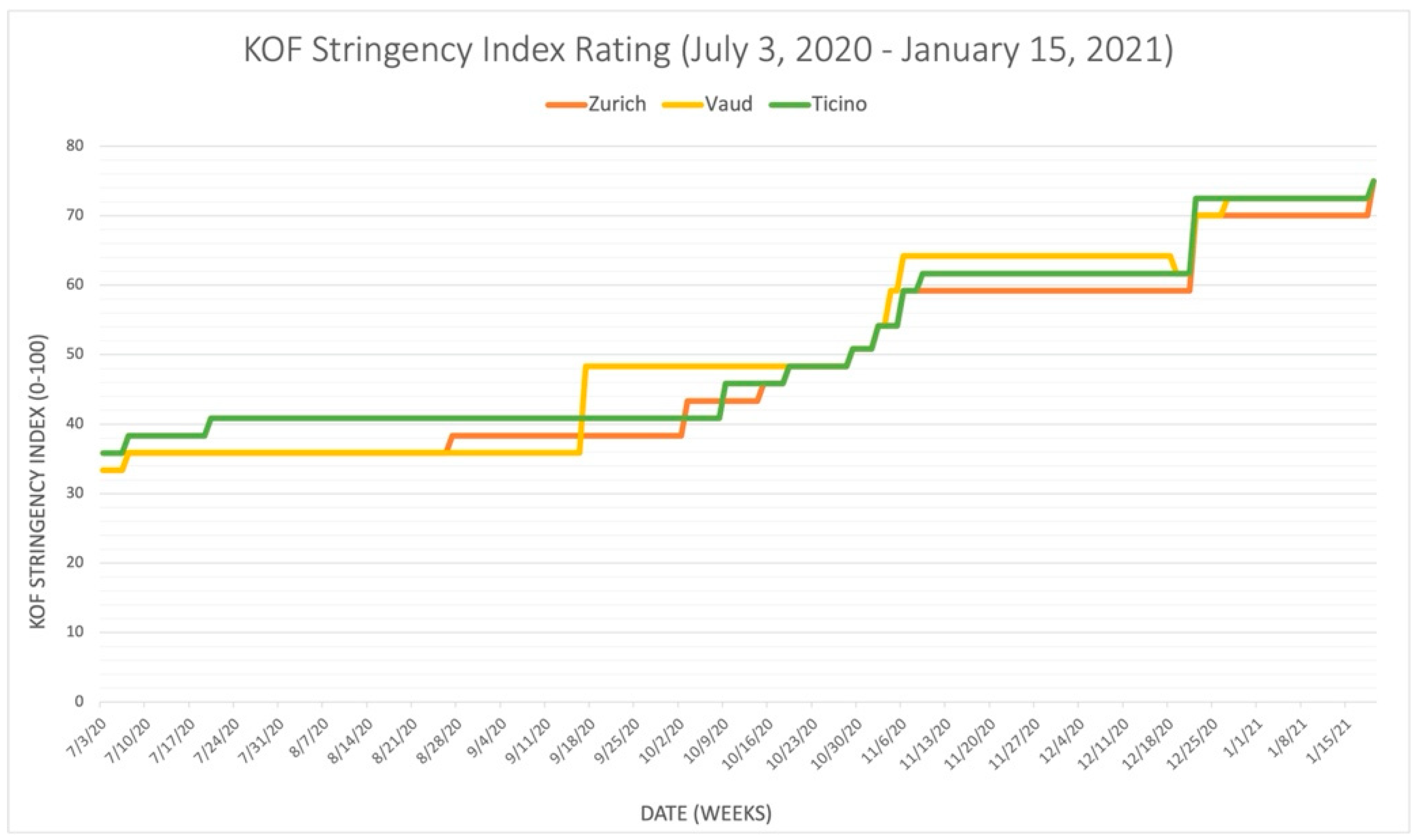
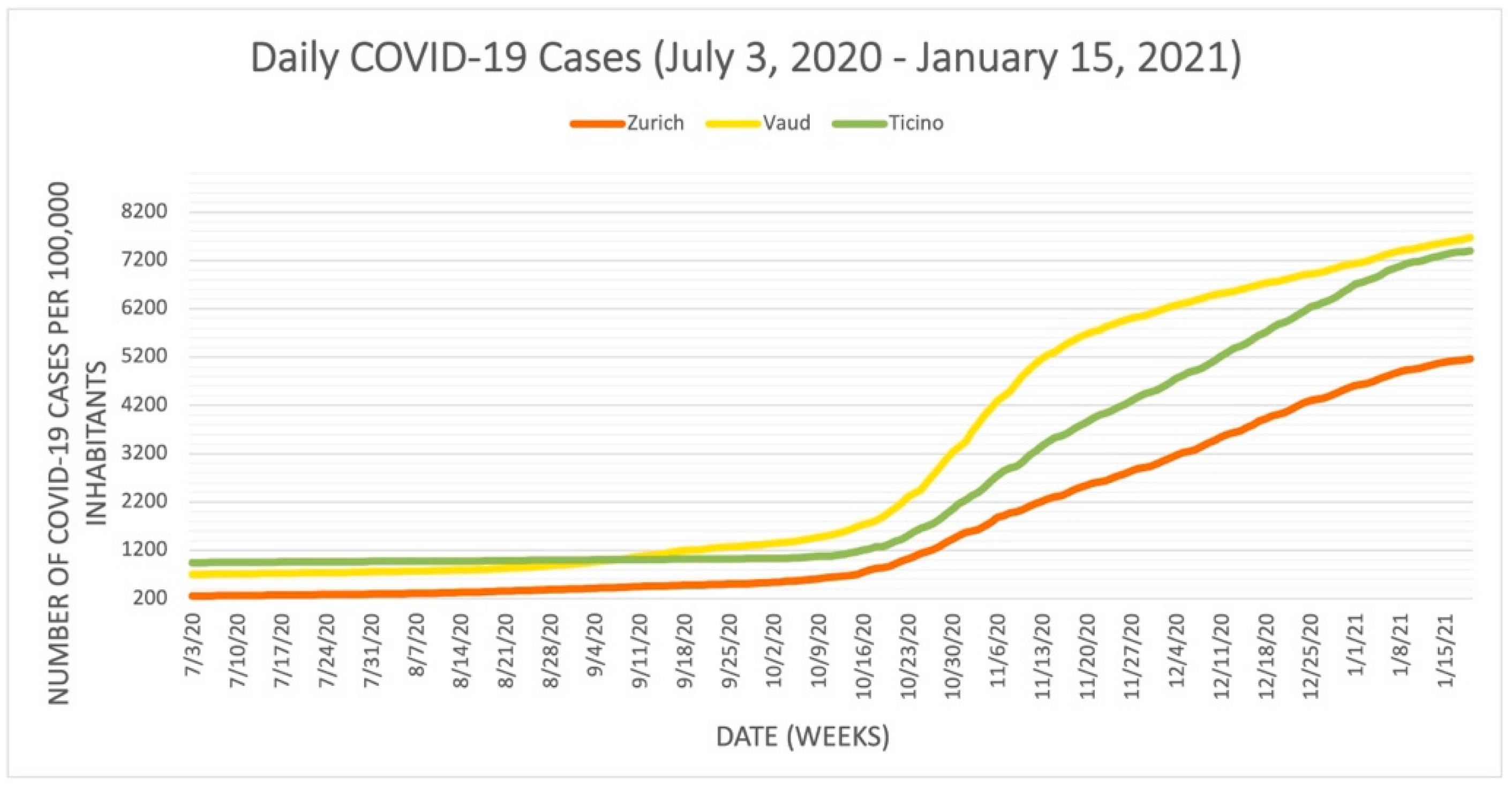
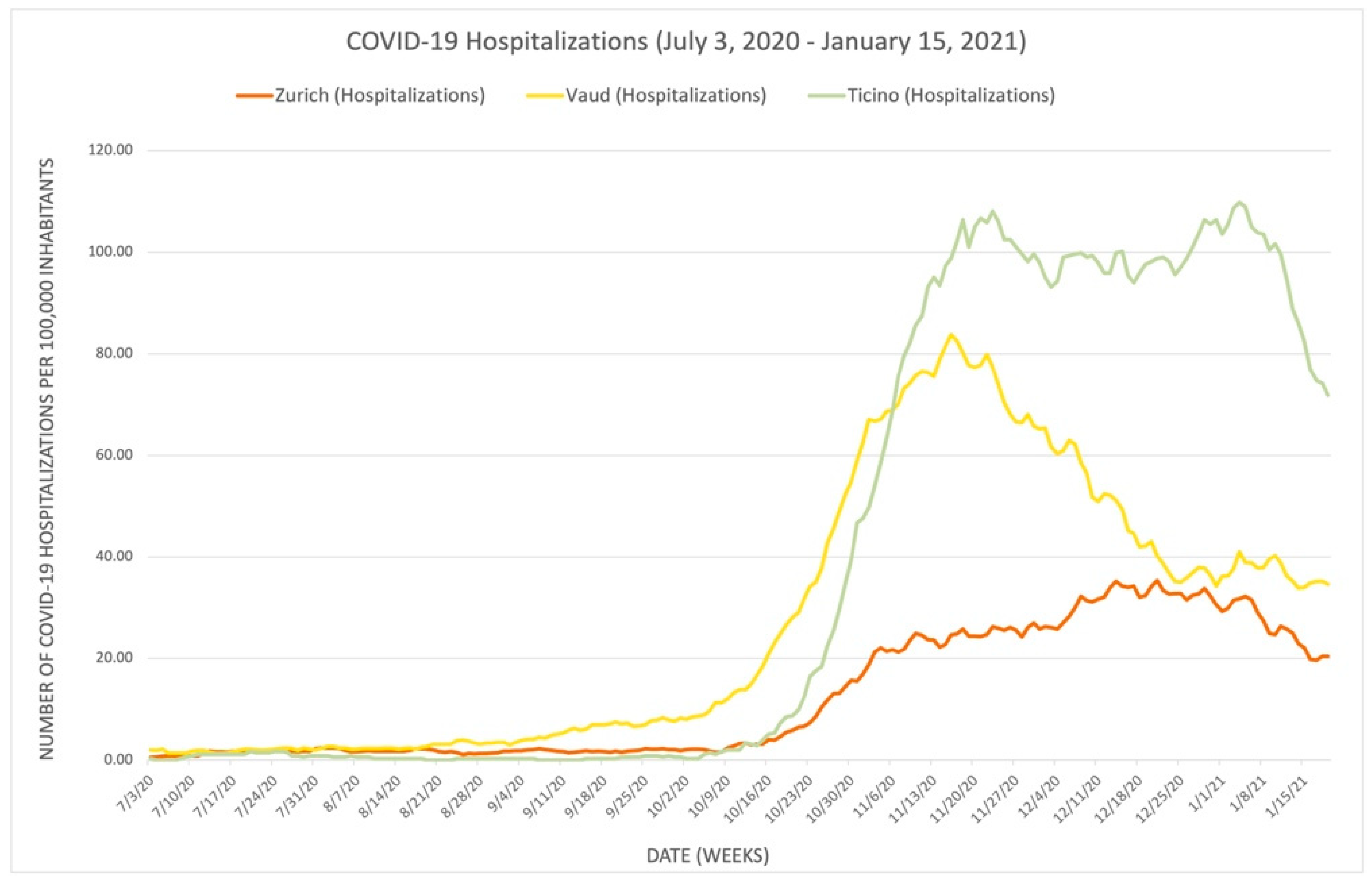
3.1. Disjointed Response: Zurich, Vaud, Ticino
3.1.1. Overview of the Pandemic Situation in Switzerland
3.1.2. Comparison of Zurich, Vaud, and Ticino
- Closure of schools, closure of workplaces, cancelation of public events, restriction of meetings, closure of public transportation, house arrest, restriction of domestic movement, international travel controls, public information campaigns, and face coverings. The nine sub-indices represented by the stringency index provide the correlation between the severity of pandemics in the cantons and the value of the index data.
3.2. Private Sectors in the Healthcare System: Challenges or Advantages?
3.2.1. The Importance of the Private Sector in the Swiss Healthcare System
3.2.2. Development of Private–Public Collaboration in Testing, Tracing, and Vaccination Policies
Contact Tracing: The SwissCovid App
Testing
Vaccination
3.2.3. Challenges in the Provision of Health Care Service during the Pandemic
3.3. Capacity of Central Authority
3.3.1. Decentralization in the Swiss Healthcare System
3.3.2. Advantages of a Central Authority during COVID-19 and Future Pandemics
3.3.3. Disadvantages of a Central Authority during COVID-19 and Future Pandemics
4. Discussion
5. Conclusions
6. Recommendations
- Greater emphasis on the collaboration between the public and private sectors, particularly between health care providers and health insurers. Greater collaboration would benefit both population health and disease prevention immensely by leading to a more equitable sharing of the risks associated with poor health and the benefits associated with good health and healthy lifestyles. This would require a solutions-based approach that considers health care resources and the better distribution, accessibility, and execution of health care services. Intelligent technologies alone can provide significant opportunities in decentralized systems, but trust in the respective government and citizen participation is a prerequisite for the long-term success of future health care challenges. Synergies should not be compromised by government involvement in the network of political parties, associations, interest groups, and lobbyists.
- Improved communication channels between governments, the public and private sectors, and the public. Different sectors operate under different constraints and regulations and approach problems in different ways, which can lead to impaired communication. Therefore, pandemic preparedness plans should establish direct communication channels between scientists and government agencies and between decision-makers and health care providers at different levels of government. This would enable active and comprehensive scientific communication that would improve timely decision-making and efficiency.
- Optimization of the healthcare value chain. To improve health care at all system levels, it is imperative to reduce the costs associated with care. This may seem counterintuitive, but it calls for the right incentives rather than emphasizing the wrong incentives. However, if risks and benefits are shared between providers and health insurers, providers could improve care—for example, by including more health-promoting services inside and outside hospitals—and reduce the number of disease services that the current system overwhelmingly provides. Prioritizing preventive care models and long-term cost-saving initiatives would not only reduce morbidity and mortality and save money later but would also start building strong provider–recipient relationships earlier and strengthen personal health accountability. Examples of trust-building structures could include college curricula with a preventive care focus or the provision of low-threshold community frameworks and health services that support long-term health behavior change [48]. In this sense, understanding and optimizing the healthcare value chain could help reduce patient admissions, prevent ICU overcrowding, provide sufficient treatment capacity, and reduce overall costs for hospitals and emergency departments.
- Promotion of the role of social determinants and health literacy. Prevention and basic health literacy should be more widely funded and promoted throughout society. Population compliance is greatly influenced by the level of health literacy that individuals bring to community discussions. Health literacy encompasses comprehension, numeracy, critical media literacy, and digital literacy and can contribute to a more comprehensive understanding of lifestyle or health choices and their impact on mental health, chronic disease management, substance use disorders, pregnancy, parenting, and younger population behaviors. Promoting health literacy could support overall confidence in and acceptance of public health interventions but may also increase demand for health care services.
- Application of the United Nations Sustainable Development Goals as a project catalyst and future-directed vessel. The SDGs provide powerful conceptual guidance for greater collaboration across sectors and more rigorous global standards for a sustainable future in all areas of work and life, particularly health, business, and policy. Given the unmet need to develop a pandemic preparedness plan, the context of the SDGs could be an opportunity to combine sustainable, long-term national programs with powerful requirements for emergency situations.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| GDP | Gross domestic product |
| NPI | Non-pharmaceutical intervention |
| SFG | Swiss Federal Government |
| P1–P6 | Interview participants No. (n = 1–6) |
| SFC | Swiss Federal Council |
| ETH | Swiss Federal Institute of Technology in Zürich |
| MHI | Mandatory health insurance |
| THE | Total health expenditure |
| NCS-TF | Swiss National COVID-19 Science Task Force |
| FOPH | Federal Office of Public Health |
| EPFL | École Polytechnique Fédérale de Lausanne |
| GP | General practitioner |
| SDGs | Sustainable Development Goals |
References
- Isabelle Sturny International Health Care System Profiles: Switzerland. Available online: https://www.commonwealthfund.org/international-health-policy-center/countries/switzerland (accessed on 8 December 2021).
- James, C.; Beazley, I.; Penn, C.; Philips, L.; Dougherty, S. Decentralisation in the Health Sector and Responsibilities across Levels of Government: Impact on Spending Decisions and the Budget. OECD J. Budg. 2019, 18–20. [Google Scholar] [CrossRef] [Green Version]
- Harvard, T.H.; Chan School of Public Health Decentralization. International Health Systems Program. Available online: https://www.hsph.harvard.edu/international-health-systems-program/decentralization/ (accessed on 29 November 2021).
- KOF Stringency Indices. Available online: https://kof.ethz.ch/en/forecasts-and-indicators/indicators/kof-stringency-index.html (accessed on 17 November 2021).
- COVID-19 Switzerland|Coronavirus|Dashboard. Available online: https://www.covid19.admin.ch/en/overview (accessed on 15 January 2022).
- Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups|The EQUATOR Network. Available online: https://www.equator-network.org/reporting-guidelines/coreq/ (accessed on 15 January 2022).
- European Comission Population: Demographic Situation, Languages and Religions: Switzerland. Available online: https://eacea.ec.europa.eu/national-policies/eurydice/content/population-demographic-situation-languages-and-religions-115_en (accessed on 17 November 2021).
- The Federal Assembly of the Swiss Confederation SR 818.101—Federal Act of 28 September 2012 on Controlling Communicable Human Diseases (Epidemics Act, EpidA). Available online: https://www.fedlex.admin.ch/eli/cc/2015/297/en (accessed on 1 May 2022).
- Wyss, K.; Lorenz, N. Decentralization and Central and Regional Coordination of Health Services: The Case of Switzerland. Int. J. Health Plan. Manag. 2000, 15, 103–114. [Google Scholar] [CrossRef]
- Federal Office of Public Health FOPH: Coronavirus: Vaccination. Available online: https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/impfen.html (accessed on 11 November 2021).
- Johns Hopkins University & Medicine Switzerland—COVID-19 Overview—Johns Hopkins. Available online: https://coronavirus.jhu.edu/region/switzerland (accessed on 17 November 2021).
- Office, F.S. Marked Decline in GDP in 2020 Following COVID-19—Swiss National Accounts 2020|Press Release. Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/catalogues-databases/press-releases.assetdetail.18344126.html (accessed on 17 November 2021).
- Burci, G.L. Jennifer Hasselgard-Rowe Switzerland’s Response to the COVID-19 Pandemic|IHEID. Available online: https://www.graduateinstitute.ch/communications/news/switzerlands-response-covid-19-pandemic (accessed on 17 November 2021).
- Clarke, D. Technical Series on Primary Health Care. The Private Sector, Universal Health Coverage and Primary Care. World Health Organization 2018. Available online: https://www.who.int/docs/default-source/primary-health-care-conference/private-sector.pdf?sfvrsn=36e53c69_2 (accessed on 21 November 2021).
- World Health Organization, Regional Office for Europe; European Observatory on Health Systems and Policies. Switzerland: Health System Review 2015; De Pietro, C., Camenzind, P., Sturny, I., Crivelli, L., Edwards-Garavoglia, S., Spranger, A., Wittenbecher, F., Quentin, W., Eds.; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- Desson, Z.; Lambertz, L.; Peters, J.W.; Falkenbach, M.; Kauer, L. Europe’s COVID-19 outliers: German, Austrian and Swiss policy responses during the early stages of the 2020 pandemic. Health Policy Technol. 2020, 9, 405–418. [Google Scholar] [CrossRef]
- Federal Office of Public Health. FOPH COVID-19 Task Force. Available online: https://www.bag.admin.ch/bag/en/home/das-bag/organisation/direktionsbereiche-abteilungen/krisenorganisation-covid-19.html (accessed on 2 December 2021).
- Guenduez, A. Wie Smarte Städte Pandemien Bekämpfen Können. Available online: www.ncbi.nlm.nih.gov/pmc/articles/PMC7481040/pdf/35114_2020_Article_272.pdf (accessed on 21 November 2021).
- Swiss Tracing App Goes on Trial|ETH Zurich. Available online: https://ethz.ch/en/news-and-events/eth-news/news/2020/05/swiss-covid-app.html (accessed on 16 November 2021).
- Longchamp, C. How to Make the Federal Council More Weatherproof. Available online: https://www.swissinfo.ch/eng/politics/how-to-make-the-federal-council-more-weatherproof/46208704 (accessed on 2 December 2021).
- Canton of Zurich, General Secretariat: Erweiterte Teststrategie: Umsetzung im Kanton Zürich. Available online: https://www.zh.ch/de/news-uebersicht/medienmitteilungen/2021/02/erweiterte-teststrategie-umsetzung-im-kanton-zuerich.html (accessed on 25 November 2021).
- Kanton Graubünden: Graubünden Beweist: Wiederholtes Testen Senkt Corona-Ansteckungen Deutlich. Available online: https://www.tagblatt.ch/news-service/leben-wissen/auswertung-der-massentests-graubuenden-beweist-wiederholtes-testen-senkt-corona-ansteckungen-deutlich-ld.2134271 (accessed on 25 November 2021).
- Kanton Glarus: Corona-Flächentests Erfolgreich Gestartet. Available online: https://www.gl.ch/public-newsroom/details.html/31/news/21499 (accessed on 25 November 2021).
- Fehr, E. Test the World to Make It Safer Place. Available online: https://testtheworld.org (accessed on 15 October 2021).
- Riachi, I. Available online: https://towardsdatascience.com/8-key-points-you-might-want-to-think-about-before-sharing-that-next-covid-19-stat-with-your-friends-812c134de124 (accessed on 12 November 2021).
- Fehr, E. Neue Zürcher Zeitung: Economist Ernst Fehr Accuses Policymakers of Making Decisions Based on Insufficient Data—And He Makes a Suggestion (Video). Available online: https://www.nzz.ch/panorama/coronavirus-oekonom-fordert-repraesentatives-testing-ld.1548239?reduced=true (accessed on 20 November 2021).
- University of Zurich, Department of Global Health, Zentrum für Reisemedizin. 2021. Available online: https://coronazentrum.uzh.ch/de/testen (accessed on 23 November 2021).
- Ab Heute Sind Coronatests Nicht Mehr Gratis. Available online: https://www.srf.ch/news/schweiz/neues-testregime-ab-heute-sind-coronatests-nicht-mehr-gratis (accessed on 16 November 2021).
- Federal Office of Public Health. Coronavirus: Health Insurance Arrangements. Available online: https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/regelung-krankenversicherung.html (accessed on 5 November 2021).
- Giachino, M.; Valera, C.B.G.; Velásquez, S.R.; Dohrendorf-Wyss, M.A.; Rozanova, L.; Flahault, A. Understanding the Dynamics of the COVID-19 Pandemic: A Real-Time Analysis of Switzerland’s First Wave. Int. J. Environ. Res. Public Health 2020, 17, 8825. [Google Scholar] [CrossRef]
- Cohidon, C.; El Hakmaoui, F.; Senn, N. The role of general practitioners in managing the COVID-19 pandemic in a private healthcare system. Fam. Pr. 2021, cmab112. [Google Scholar] [CrossRef] [PubMed]
- Giezendanner, S.; Fischer, R.; Hernandez, L.D.; Zeller, A. The use of health care during the SARS-CoV-2 pandemic: Repeated cross-sectional survey of the adult Swiss general population. BMC Public Health 2021, 21, 853. [Google Scholar] [CrossRef] [PubMed]
- Westerhoff, C.; Kuhlen, R.; Schmithausen, D.; Graf, R.; Winklmair, C. Effekte der COVID-19 Pandemie auf Die Stationre Versorgung. Available online: https://doi.emh.ch/saez.2021.19616 (accessed on 10 October 2021).
- PWC: Whitepaper 3.0 zur Berechnung des Finanziellen Schadens für Schweizer Spitäler und Kliniken Infolge von COVID-19. Available online: https://www.pwc.ch/de/publications/2020/20201216_COVID19_Whitepaper_3.0.pdf (accessed on 26 November 2021).
- Tikkanen, R.; Osborn, R. International Profiles of Health Care Systems. Available online: https://www.researchgate.net/publication/347011106_International_Profiles_of_Health_Care_Systems_2020/link/5fd7897292851c13fe865e6a/download (accessed on 8 December 2021).
- Bruhin, E.; Wüthrich, A. Spectra—Gesundheitsförderung und Prävention; Bundesamt für Gesundheit BAG: Bern, Switzerland, 2014.
- Belser, E.M.; Mazidi, S. Does Swiss Federalism Need Oxygen Treatment after Been Hit by the COVID-19 Crisis? Available online: https://uacesterrpol.wordpress.com/2020/06/02/does-swiss-federalism-need-oxygen-treatment-after-been-hit-by-the-covid-19-crisis/ (accessed on 11 October 2021).
- Gaskel, J.; Stoker, G. Centralised or Multi-Level: Which Governance Systems Are Having a ‘Good’ Pandemic? Available online: https://blogs.lse.ac.uk/politicsandpolicy/governance-systems-covid19/ (accessed on 10 October 2021).
- Morton, C. The Merits of a Centralized System of Government. Available online: https://www.virtualkollage.com/2016/12/the-merits-of-centralization-system-of-government.html (accessed on 16 November 2021).
- The Local: Why Did It Take Switzerland so Long to Make Masks Compulsory? Available online: https://www.thelocal.ch/20200701/why-are-coronavirus-masks-still-not-required-in-switzerland/ (accessed on 16 November 2021).
- Klaunzer, P. Cantons Threaten Rebellion against Swiss Mini-Lockdown Plans. Available online: https://www.swissinfo.ch/eng/cantons-threaten-rebellion-against-swiss-mini-lockdown-plans/46213134 (accessed on 16 November 2021).
- Hitchman, S. Reasons for Not Getting Vaccinated against COVID-19 in German-Speaking Switzerland: An Online Survey among Vaccine Hesitant 16–60 Year Olds. Available online: https://psyarxiv.com/hnzke/ (accessed on 30 November 2021).
- Tschannen, P. Pflegeinitiative: Es Braucht Mehr Als Nur Mehr Ausbildung. Neue Zürcher Zeitung. Available online: https://www.nzz.ch/meinung/pflegeinitiative-es-braucht-mehr-als-nur-mehr-ausbildung-ld.1651964 (accessed on 28 November 2021).
- Pflegeinitiative. 2021. Available online: https://www.pflegeinitiative.ch (accessed on 15 November 2021).
- Riou, J.; Panczak, R.; Althaus, C.L.; Junker, C.; Perisa, D.; Schneider, K.; Criscuolo, N.G.; Low, N.; Egger, M. Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: A population-based analysis. Lancet Public Health 2021, 6, e683–e691. [Google Scholar] [CrossRef]
- Geiser, U. How the Virus Puts the Swiss Political System to Test. Available online: https://www.swissinfo.ch/eng/federalism-and-covid-19_how-the-virus-puts-the-swiss-political-system-to-test/45646244 (accessed on 13 November 2021).
- Simonian, H. How the Private Sector Could Help to Fight the Next Pandemic. Available online: https://www.avenir-suisse.ch/en/how-the-private-sector-could-help-to-fight-the-next-pandemic/ (accessed on 21 November 2021).
- Global Social Prescribing Alliance. Available online: https://whis.world/gspa (accessed on 15 November 2021).

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burger, M.M.-R.L.; Large, K.E.; Liu, Y.; Coyle, M.C.; Gamanya, C.T.; Etter, J.-F. Future Strategic Priorities of the Swiss Decentralized Healthcare System: A COVID-19 Case Study. Epidemiologia 2022, 3, 250-268. https://doi.org/10.3390/epidemiologia3020020
Burger MM-RL, Large KE, Liu Y, Coyle MC, Gamanya CT, Etter J-F. Future Strategic Priorities of the Swiss Decentralized Healthcare System: A COVID-19 Case Study. Epidemiologia. 2022; 3(2):250-268. https://doi.org/10.3390/epidemiologia3020020
Chicago/Turabian StyleBurger, Miriam Mi-Rim Lee, Kaitlin Elizabeth Large, Yiqi Liu, Melissa Cigdem Coyle, Cherish Tariro Gamanya, and Jean-François Etter. 2022. "Future Strategic Priorities of the Swiss Decentralized Healthcare System: A COVID-19 Case Study" Epidemiologia 3, no. 2: 250-268. https://doi.org/10.3390/epidemiologia3020020
APA StyleBurger, M. M.-R. L., Large, K. E., Liu, Y., Coyle, M. C., Gamanya, C. T., & Etter, J.-F. (2022). Future Strategic Priorities of the Swiss Decentralized Healthcare System: A COVID-19 Case Study. Epidemiologia, 3(2), 250-268. https://doi.org/10.3390/epidemiologia3020020







