Decoding Diabetes Nutritional Guidelines for Physicians in Underserved American Populations
Abstract
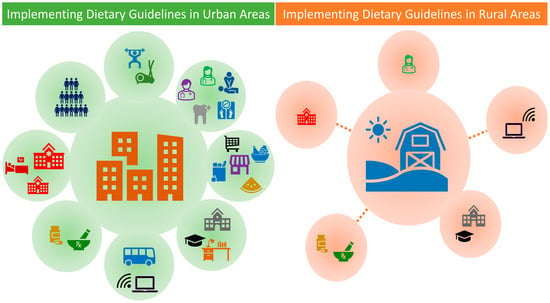
1. Introduction
2. Nutritional Guidelines under a Rural Lens
3. Dietary Intakes of People with Diabetes
4. Initiating Nutritional Therapy in Rural Environments
4.1. Estimating Energy Intake
4.2. Macronutrient Distribution
4.3. Protein and Fat
4.4. Carbohydrate
4.5. Water
4.6. Micronutrients
4.7. Non-Nutritive Sweeteners
4.8. Alcohol
4.9. Dietary Patterns/Quality
5. Cultural Preferences
6. Summary and Conclusions
- The process must be supportive and positive, and include cultural preferences.
- Screen for malnutrition;
- For weight loss, the 3500 kcal rule is a good starting point but has limitations.
- Focus on improving diet quality, especially carbohydrate quality, to reduce micronutrient insufficiencies;
- Limit sugar-sweetened beverages;
- Focus on modifying snacks to help reduce energy intake, refined carbohydrates, and added sugars;
- Increase plant foods and whole foods in the diet;
- Decrease processed meat consumption, and reduce processed food where possible to reduce sodium;
- Maintain good hydration;
- Assess B12 status at least annually for those on metformin.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bennett, K.J.; Borders, T.F.; Holmes, G.M.; Kozhimannil, K.B.; Ziller, E. What Is Rural? Challenges And Implications Of Definitions That Inadequately Encompass Rural People And Places. Health Aff. 2019, 38, 1985–1992. [Google Scholar] [CrossRef]
- Rutledge, S.A.; Masalovich, S.; Blacher, R.J.; Saunders, M.M. Diabetes Self-Management Education Programs in Nonmetropolitan Counties—United States, 2016. Surveill. Summ. 2017, 66, 1–6. [Google Scholar] [CrossRef]
- O’Connor, A.; Wellenius, G. Rural–urban disparities in the prevalence of diabetes and coronary heart disease. Public Health 2012, 126, 813–820. [Google Scholar] [CrossRef]
- Bolin, J.N.; Bellamy, G.R.; Ferdinand, A.O.; Vuong, A.M.; Kash, B.A.; Schulze, A.; Helduser, J.W. Rural Healthy People 2020: New Decade, Same Challenges. J. Rural Health 2015, 31, 326–333. [Google Scholar] [CrossRef]
- Rosenblatt, R.A.; Hart, L.G. Physicians and rural America. West. J. Med. 2000, 173, 348–351. [Google Scholar] [CrossRef]
- Feng, W.; Page, E.T.; Cash, S.B. Dollar Stores and Food Access for Rural Households in the United States, 2008–2020. Am. J. Public Health 2023, 113, 331–336. [Google Scholar] [CrossRef]
- Li, Y.; Kou, C.; Bai, W.; Hua, W.; Yu, W.; Song, Y.; Liu, X.; Li, W. Trends in Diabetes Mortality by Gender in Urban and Rural Areas in China From 2003 to 2012: An Age-Period-Cohort Analysis. Asia Pac. J. Public Health 2019, 31, 238–245. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Jayawardena, R.; Gamage, N.; Sivanandam, N.; Misra, A. Prevalence and trends of the diabetes epidemic in urban and rural India: A pooled systematic review and meta-analysis of 1.7 million adults. Ann. Epidemiol. 2021, 58, 128–148. [Google Scholar] [CrossRef]
- Loccoh, E.C.; Maddox, K.E.J.; Wang, Y.; Kazi, D.S.; Yeh, R.W.; Wadhera, R.K. Rural-Urban Disparities in Outcomes of Myocardial Infarction, Heart Failure, and Stroke in the United States. J. Am. Coll. Cardiol. 2022, 79, 267–279. [Google Scholar] [CrossRef]
- Hammond, G.; Luke, A.A.; Elson, L.; Towfighi, A.; Joynt Maddox, K.E. Urban-Rural Inequities in Acute Stroke Care and In-Hospital Mortality. Stroke 2020, 51, 2131–2138. [Google Scholar] [CrossRef]
- Chen, X.; Orom, H.; Hay, J.L.; Waters, E.A.; Schofield, E.; Li, Y.; Kiviniemi, M.T. Differences in Rural and Urban Health Information Access and Use. J. Rural Health 2019, 35, 405–417. [Google Scholar] [CrossRef]
- Kozhimannil, K.B.; Interrante, J.D.; Henning-Smith, C.; Admon, L.K. Rural-Urban Differences In Severe Maternal Morbidity And Mortality In The US, 2007–2015. Health Aff. 2019, 38, 2077–2085. [Google Scholar] [CrossRef]
- Cyr, M.E.; Etchin, A.G.; Guthrie, B.J.; Benneyan, J.C. Access to specialty healthcare in urban versus rural US populations: A systematic literature review. BMC Health Serv. Res. 2019, 19, 974. [Google Scholar] [CrossRef]
- Evert, A.B.; Dennison, M.; Gardner, C.D.; Garvey, W.T.; Lau, K.H.K.; MacLeod, J.; Mitri, J.; Pereira, R.F.; Rawlings, K.; Robinson, S.; et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care 2019, 42, 731–754. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46, S10–S18. [Google Scholar] [CrossRef]
- Diabetes Canada Clinical Practice Guidelines Expert Committee; Sievenpiper, J.L.; Chan, C.B.; Dworatzek, P.D.; Freeze, C.; Williams, S.L. Nutrition Therapy. Can. J. Diabetes 2018, 42 (Suppl. S1), S64–S79. [Google Scholar] [CrossRef]
- Dyson, P.A.; Twenefour, D.; Breen, C.; Duncan, A.; Elvin, E.; Goff, L.; Hill, A.; Kalsi, P.; Marsland, N.; McArdle, P.; et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet. Med. 2018, 35, 541–547. [Google Scholar] [CrossRef]
- Gray, A.; Rebecca, J. Nutritional Recommendations for Individuals with Diabetes; Mdtext Com, Inc.: South Dartmouth, MA, USA, 2019. [Google Scholar]
- Rosik, P.; Stępniak, M.; Wiśniewski, R. Delineation of health care deserts using accessibility measures: The case of Poland. Eur. Plan. Stud. 2020, 29, 1151–1173. [Google Scholar] [CrossRef]
- Lucas-Gabrielli, V.; Chevillard, G. Medical deserts” and accessibility to care: What are we talking about? Med. Sci. 2018, 34, 599–603. [Google Scholar] [CrossRef]
- Delk, J.A.; Singleton, B.A.; Al-Dahir, S.; Kirchain, W.; Bailey-Wheeler, J. The effect of food access on type 2 diabetes control in patients of a New Orleans, Louisiana, clinic. J. Am. Pharm. Assoc. 2022, 62, 1675–1679. [Google Scholar] [CrossRef]
- Berkowitz, S.A.; Karter, A.J.; Corbie-Smith, G.; Seligman, H.K.; Ackroyd, S.A.; Barnard, L.S.; Atlas, S.J.; Wexler, D.J. Food Insecurity, Food “Deserts,” and Glycemic Control in Patients With Diabetes: A Longitudinal Analysis. Diabetes Care 2018, 41, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Look, A.R.G.; Wing, R.R.; Bolin, P.; Brancati, F.L.; Bray, G.A.; Clark, J.M.; Coday, M.; Crow, R.S.; Curtis, J.M.; Egan, C.M.; et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N. Engl. J. Med. 2013, 369, 145–154. [Google Scholar] [CrossRef]
- Smith, J.G.; Plover, C.M.; McChesney, M.C.; Lake, E.T. Isolated, small, and large hospitals have fewer nursing resources than urban hospitals: Implications for rural health policy. Public Health Nurs. 2019, 36, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Harrington, R.A.; Califf, R.M.; Balamurugan, A.; Brown, N.; Benjamin, R.M.; Braund, W.E.; Hipp, J.; Konig, M.; Sanchez, E.; Joynt Maddox, K.E. Call to Action: Rural Health: A Presidential Advisory From the American Heart Association and American Stroke Association. Circulation 2020, 141, e615–e644. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Clary, C.; Johnson, J.A.; Berman, A.; Heboyan, V.; Benevides, T.; Moore, J.; George, V. Continuing Challenges in Rural Health in the United States. J. Environ. Health Sci. 2019, 5, 90–92. [Google Scholar]
- Dao, M.C.; Subar, A.F.; Warthon-Medina, M.; Cade, J.E.; Burrows, T.; Golley, R.K.; Forouhi, N.G.; Pearce, M.; Holmes, B.A. Dietary assessment toolkits: An overview. Public Health Nutr. 2019, 22, 404–418. [Google Scholar] [CrossRef]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Athinarayanan, S.J.; Roberts, C.G.P.; Adams, R.N.; Volk, B.M.; Phinney, S.D.; Volek, J.; McKenzie, A.L. 410-P: Two-Year (2y) eGFR Slope in People with Type 2 Diabetes (T2D) Receiving a Very Low Carbohydrate Diet (VLCD) Intervention. Diabetes 2023, 72, 410-P. [Google Scholar] [CrossRef]
- Asano, M.; Fukuda, T.; Fukui, M.; Hashimoto, Y.; Oyabu, C.; Tanaka, M.; Yamazaki, M. Impact of low-carbohydrate diet on renal function: A meta-analysis of over 1000 individuals from nine randomised controlled trials. Br. J. Nutr. 2016, 116, 632–638. [Google Scholar] [CrossRef]
- de Las Hazas, M.-C.L.; Dávalos, A. Individualization, Precision Nutrition Developments for the 21st Century. In Advances in Precision Nutrition, Personalization and Healthy Aging; Haslberger, A.G., Ed.; Springer International Publishing: Cham, Switzerland, 2022; pp. 25–50. [Google Scholar]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Heitman, K.; Thomas, S.E.; Kelly, O.; Fanelli, S.M.; Krok-Schoen, J.L.; Luo, M.; Taylor, C.A. Snacks contribute considerably to total dietary intakes among adults stratified by glycemia in the United States. PLoS Glob. Public Health 2023, 3, e0000802. [Google Scholar] [CrossRef] [PubMed]
- Fanelli, S.M.; Kelly, O.J.; Krok-Schoen, J.L.; Taylor, C.A. Low Protein Intakes and Poor Diet Quality Associate with Functional Limitations in US Adults with Diabetes: A 2005–2016 NHANES Analysis. Nutrients 2021, 13, 2582. [Google Scholar] [CrossRef] [PubMed]
- Kelly, O.; Krok-Schoen, J.L.; Luo, M.; Taylor, C.A. Evaluation of Dietary Intakes of Macronutrients in Adults with Different A1C Levels. Diabetes 2018, 67, 763-P. [Google Scholar] [CrossRef]
- Fanelli, S.; Kelly, O.; Luo, M.; Krok-Schoen, J.; Taylor, C. Differences in Micronutrient Intakes by Levels of Glycemic Control in US Adults. J. Acad. Nutr. Diet. 2018, 118, A133. [Google Scholar] [CrossRef]
- Kelly, O.; Fanelli, S.M.; Krok-Schoen, J.L.; Taylor, C.A. 1577-P: Dietary Intake Trends Associated with Breakfast Skipping in U.S. Adults by Diabetes Status. Diabetes 2019, 68, 1577-P. [Google Scholar] [CrossRef]
- Fanelli, S.M.; Jonnalagadda, S.S.; Pisegna, J.L.; Kelly, O.J.; Krok-Schoen, J.L.; Taylor, C.A. Poorer Diet Quality Observed Among US Adults With a Greater Number of Clinical Chronic Disease Risk Factors. J. Prim. Care Community Health 2020, 11, 2150132720945898. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Dietary Reference Intakes for Energy; The National Academies Press: Washington, DC, USA, 2023; p. 460. [Google Scholar]
- Hall, K.D.; Sacks, G.; Chandramohan, D.; Chow, C.C.; Wang, Y.C.; Gortmaker, S.L.; Swinburn, B.A. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011, 378, 826–837. [Google Scholar] [CrossRef]
- Thomas, D.M.; Gonzalez, M.C.; Pereira, A.Z.; Redman, L.M.; Heymsfield, S.B. Time to correctly predict the amount of weight loss with dieting. J. Acad. Nutr. Diet. 2014, 114, 857–861. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture. MyPlate Plan. Available online: https://www.myplate.gov/myplate-plan (accessed on 1 January 2024).
- Fleming, S.; Arensberg, M.B.; Kerr, K.; Blancato, R. The Opportunity for Quality Malnutrition Care to Improve Rural Health Outcomes and Health Equity for Older Americans. OBM Geriatr. 2023, 07, 227. [Google Scholar] [CrossRef]
- Saunders, J.; Smith, T. Malnutrition: Causes and consequences. Clin. Med. 2010, 10, 624–627. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46, S68–S96. [Google Scholar] [CrossRef] [PubMed]
- Medicine, I.O. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; The National Academies Press: Washington, DC, USA, 2005; p. 1358. [Google Scholar]
- Guzman, J.R.; Lyra, R.; Aguilar-Salinas, C.A.; Cavalcanti, S.; Escano, F.; Tambasia, M.; Duarte, E.; Group, A.C. Treatment of type 2 diabetes in Latin America: A consensus statement by the medical associations of 17 Latin American countries. Latin American Diabetes Association. Rev. Panam. Salud Publica 2010, 28, 463–471. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mann, J.I.; De Leeuw, I.; Hermansen, K.; Karamanos, B.; Karlstrom, B.; Katsilambros, N.; Riccardi, G.; Rivellese, A.A.; Rizkalla, S.; Slama, G.; et al. Evidence-based nutritional approaches to the treatment and prevention of diabetes mellitus. Nutr. Metab. Cardiovasc. Dis. 2004, 14, 373–394. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Sharma, R.; Gulati, S.; Joshi, S.R.; Sharma, V.; Ghafoorunissa; Ibrahim, A.; Joshi, S.; Laxmaiah, A.; Kurpad, A.; et al. Consensus dietary guidelines for healthy living and prevention of obesity, the metabolic syndrome, diabetes, and related disorders in Asian Indians. Diabetes Technol. Ther. 2011, 13, 683–694. [Google Scholar] [CrossRef] [PubMed]
- Sinska, B.; Kucharska, A. Dietary guidelines in diabetes—Why are they so difficult to follow? Pediatr. Endocrinol. Diabetes Metab. 2023, 29, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Hershon, K.S.; Hirsch, B.R.; Odugbesan, O. Importance of Postprandial Glucose in Relation to A1C and Cardiovascular Disease. Clin. Diabetes 2019, 37, 250–259. [Google Scholar] [CrossRef]
- Ramsden, C.E.; Zamora, D.; Majchrzak-Hong, S.; Faurot, K.R.; Broste, S.K.; Frantz, R.P.; Davis, J.M.; Ringel, A.; Suchindran, C.M.; Hibbeln, J.R. Re-evaluation of the traditional diet-heart hypothesis: Analysis of recovered data from Minnesota Coronary Experiment (1968–73). BMJ 2016, 353, i1246. [Google Scholar] [CrossRef]
- Carson, J.A.S.; Lichtenstein, A.H.; Anderson, C.A.M.; Appel, L.J.; Kris-Etherton, P.M.; Meyer, K.A.; Petersen, K.; Polonsky, T.; Van Horn, L.; American Heart Association Nutrition Committee of the Council; et al. Dietary Cholesterol and Cardiovascular Risk: A Science Advisory From the American Heart Association. Circulation 2020, 141, e39–e53. [Google Scholar] [CrossRef]
- Ludwig, D.S. Lowering the Bar on the Low-Fat Diet. JAMA 2016, 316, 2087–2088. [Google Scholar] [CrossRef]
- Harcombe, Z. US dietary guidelines: Is saturated fat a nutrient of concern? Br. J. Sports Med. 2019, 53, 1393–1396. [Google Scholar] [CrossRef]
- Kaur, D.; Tallman, D.A.; Khosla, P. The health effects of saturated fats—The role of whole foods and dietary patterns. Diabetes Metab. Syndr. 2020, 14, 151–153. [Google Scholar] [CrossRef]
- Derosa, G.; Maffioli, P. alpha-Glucosidase inhibitors and their use in clinical practice. Arch. Med. Sci. 2012, 8, 899–906. [Google Scholar] [CrossRef]
- Rehani, P.R.; Iftikhar, H.; Nakajima, M.; Tanaka, T.; Jabbar, Z.; Rehani, R.N. Safety and Mode of Action of Diabetes Medications in comparison with 5-Aminolevulinic Acid (5-ALA). J. Diabetes Res. 2019, 2019, 4267357. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Barquera, S.; Duhamel, J.F.; Hardinsyah, R.; Haslam, D.; Lafontan, M. Recommendations for healthier hydration: Addressing the public health issues of obesity and type 2 diabetes. Clin. Obes. 2012, 2, 115–124. [Google Scholar] [CrossRef]
- Janbozorgi, N.; Allipour, R.; Djafarian, K.; Shab-Bidar, S.; Badeli, M.; Safabakhsh, M. Water intake and risk of type 2 diabetes: A systematic review and meta-analysis of observational studies. Diabetes Metab. Syndr. 2021, 15, 102156. [Google Scholar] [CrossRef]
- Vanhaecke, T.; Perrier, E.T.; Melander, O. A Journey through the Early Evidence Linking Hydration to Metabolic Health. Ann. Nutr. Metab. 2020, 76 (Suppl. S1), 4–9. [Google Scholar] [CrossRef]
- Johnson, E.C.; Bardis, C.N.; Jansen, L.T.; Adams, J.D.; Kirkland, T.W.; Kavouras, S.A. Reduced water intake deteriorates glucose regulation in patients with type 2 diabetes. Nutr. Res. 2017, 43, 25–32. [Google Scholar] [CrossRef]
- Wolfsdorf, J.; Glaser, N.; Sperling, M.A.; American Diabetes, A. Diabetic ketoacidosis in infants, children, and adolescents: A consensus statement from the American Diabetes Association. Diabetes Care 2006, 29, 1150–1159. [Google Scholar] [CrossRef]
- Gosmanov, A.R.; Gosmanova, E.O.; Dillard-Cannon, E. Management of adult diabetic ketoacidosis. Diabetes Metab. Syndr. Obes. 2014, 7, 255–264. [Google Scholar] [CrossRef]
- Medicine, I.O. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate; The National Academies Press: Washington, DC, USA, 2005; p. 638. [Google Scholar]
- Begg, D.P. Disturbances of thirst and fluid balance associated with aging. Physiol. Behav. 2017, 178, 28–34. [Google Scholar] [CrossRef]
- Kavouras, S.A. Assessing hydration status. Curr. Opin. Clin. Nutr. Metab. Care 2002, 5, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Kostelnik, S.B.; Davy, K.P.; Hedrick, V.E.; Thomas, D.T.; Davy, B.M. The Validity of Urine Color as a Hydration Biomarker within the General Adult Population and Athletes: A Systematic Review. J. Am. Coll. Nutr. 2021, 40, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, L.E.; Maresh, C.M.; Castellani, J.W.; Bergeron, M.F.; Kenefick, R.W.; LaGasse, K.E.; Riebe, D. Urinary indices of hydration status. Int. J. Sport. Nutr. 1994, 4, 265–279. [Google Scholar] [CrossRef] [PubMed]
- Wardenaar, F.C.; Thompsett, D.; Vento, K.A.; Pesek, K.; Bacalzo, D. Athletes’ Self-Assessment of Urine Color Using Two Color Charts to Determine Urine Concentration. Int. J. Environ. Res. Public Health 2021, 18, 4126. [Google Scholar] [CrossRef] [PubMed]
- Wardenaar, F.C.; Thompsett, D.; Vento, K.A.; Bacalzo, D. A lavatory urine color (LUC) chart method can identify hypohydration in a physically active population. Eur. J. Nutr. 2021, 60, 2795–2805. [Google Scholar] [CrossRef]
- MedlinePlus. Urine—Abnormal Color. Available online: https://medlineplus.gov/ency/article/003139.htm (accessed on 30 December 2023).
- National Institutes of Health. Nutrient Recommendations and Databases. Available online: https://ods.od.nih.gov/HealthInformation/nutrientrecommendations.aspx (accessed on 30 December 2023).
- Chehade, J.M.; Sheikh-Ali, M.; Mooradian, A.D. The Role of Micronutrients in Managing Diabetes. Diabetes Spectr. 2009, 22, 214–218. [Google Scholar] [CrossRef]
- Shearer, J.; Swithers, S.E. Artificial sweeteners and metabolic dysregulation: Lessons learned from agriculture and the laboratory. Rev. Endocr. Metab. Disord. 2016, 17, 179–186. [Google Scholar] [CrossRef]
- Tey, S.L.; Salleh, N.B.; Henry, J.; Forde, C.G. Effects of aspartame-, monk fruit-, stevia- and sucrose-sweetened beverages on postprandial glucose, insulin and energy intake. Int. J. Obes. 2017, 41, 450–457. [Google Scholar] [CrossRef]
- Mejia, E.; Pearlman, M. Natural Alternative Sweeteners and Diabetes Management. Curr. Diabetes Rep. 2019, 19, 142. [Google Scholar] [CrossRef]
- Purohit, V.; Mishra, S. The truth about artificial sweeteners—Are they good for diabetics? Indian Heart J. 2018, 70, 197–199. [Google Scholar] [CrossRef]
- Nettleton, J.A.; Lutsey, P.L.; Wang, Y.; Lima, J.A.; Michos, E.D.; Jacobs, D.R., Jr. Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 2009, 32, 688–694. [Google Scholar] [CrossRef]
- Imamura, F.; O’Connor, L.; Ye, Z.; Mursu, J.; Hayashino, Y.; Bhupathiraju, S.N.; Forouhi, N.G. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: Systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 2015, 351, h3576. [Google Scholar] [CrossRef] [PubMed]
- van de Wiel, A. Diabetes mellitus and alcohol. Diabetes Metab. Res. Rev. 2004, 20, 263–267. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. What Is the Diabetes Plate Method? Available online: https://www.diabetesfoodhub.org/articles/what-is-the-diabetes-plate-method.html (accessed on 30 December 2023).
- Gardner, C.D.; Landry, M.J.; Perelman, D.; Petlura, C.; Durand, L.R.; Aronica, L.; Crimarco, A.; Cunanan, K.M.; Chang, A.; Dant, C.C.; et al. Effect of a ketogenic diet versus Mediterranean diet on glycated hemoglobin in individuals with prediabetes and type 2 diabetes mellitus: The interventional Keto-Med randomized crossover trial. Am. J. Clin. Nutr. 2022, 116, 640–652. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, K.D. Food, Culture, and Diabetes in the United States. Clin. Diabetes 2004, 22, 190–192. [Google Scholar] [CrossRef]
- Woodside, J.; Young, I.S.; McKinley, M.C. Culturally adapting the Mediterranean Diet pattern—A way of promoting more ‘sustainable’ dietary change? Br. J. Nutr. 2022, 128, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report Website. Available online: https://www.cdc.gov/diabetes/data/statistics-report/index.html (accessed on 12 December 2023).
- Marshall, M.C., Jr. Diabetes in African Americans. Postgrad. Med. J. 2005, 81, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Kittler, P.G.; Sucher, K.P.; Nelms, M. Food and Culture, 7th ed.; Cengage Learning: Boston, MA, USA, 2017. [Google Scholar]
- James, D.C. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: Application of a culturally sensitive model. Ethn. Health 2004, 9, 349–367. [Google Scholar] [CrossRef]
- Anderson-Loftin, W.; Barnett, S.; Bunn, P.; Sullivan, P.; Hussey, J.; Tavakoli, A. Soul food light: Culturally competent diabetes education. Diabetes Educ. 2005, 31, 555–563. [Google Scholar] [CrossRef]
- Bullock, A.; Sheff, K.; Hora, I.; Burrows, N.R.; Benoit, S.R.; Saydah, S.H.; Hardin, C.L.; Gregg, E.W. Prevalence of diagnosed diabetes in American Indian and Alaska Native adults, 2006–2017. BMJ Open Diabetes Res. Care 2020, 8, e001218. [Google Scholar] [CrossRef]
- Indian Health Service. Disparities. Available online: https://www.ihs.gov/newsroom/factsheets/disparities/ (accessed on 12 December 2023).
- Stotz, S.; Brega, A.G.; Lockhart, S.; Hebert, L.E.; Henderson, J.N.; Roubideaux, Y.; Moore, K. An online diabetes nutrition education programme for American Indian and Alaska Native adults with type 2 diabetes: Perspectives from key stakeholders. Public Health Nutr. 2021, 24, 1449–1459. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Diabetes Prevention Program. Available online: https://www.cdc.gov/diabetes/prevention/resources/curriculum.html (accessed on 30 December 2023).
- OMH. American Indian/Alaska Native. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=62 (accessed on 12 December 2023).
- Indian Health Service. My Native Plate. Available online: https://www.ihs.gov/diabetes/education-materials-and-resources/index.cfm?module=productDetails&productID=2468 (accessed on 30 December 2023).
- Indian Health Service. Food Insecurity Assessment Tool and Resource List. Available online: https://www.ihs.gov/diabetes/education-materials-and-resources/index.cfm?module=productDetails&productID=332 (accessed on 30 December 2023).
- Dias, J.; Echeverria, S.; Mayer, V.; Janevic, T. Diabetes Risk and Control in Multi-ethnic US Immigrant Populations. Curr. Diabetes Rep. 2020, 20, 73. [Google Scholar] [CrossRef] [PubMed]
- Payton, C.; Kimball, S.; Ahrenholz, N.C.; Wieland, M.L. Preventive Care and Management of Chronic Diseases in Immigrant Adults. Prim. Care 2021, 48, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Attridge, M.; Creamer, J.; Ramsden, M.; Cannings-John, R.; Hawthorne, K. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2014, 9, CD006424. [Google Scholar] [CrossRef] [PubMed]
- McConatha, J.T.; Kumar, V.K.; Raymond, E.; Akwarandu, A. Cultural Dimensions of Diabetes Management: A Qualitative Study of Middle Eastern Immigrants in the U.S. J. Cross-Cult. Gerontol. 2020, 35, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Li-Geng, T.; Kilham, J.; McLeod, K.M. Cultural Influences on Dietary Self-Management of Type 2 Diabetes in East Asian Americans: A Mixed-Methods Systematic Review. Health Equity 2020, 4, 31–42. [Google Scholar] [CrossRef]
- McKenzie, A.L.; Athinarayanan, S.J.; McCue, J.J.; Adams, R.N.; Keyes, M.; McCarter, J.P.; Volek, J.S.; Phinney, S.D.; Hallberg, S.J. Type 2 Diabetes Prevention Focused on Normalization of Glycemia: A Two-Year Pilot Study. Nutrients 2021, 13, 749. [Google Scholar] [CrossRef]
- Ren, M.; Zhang, H.; Qi, J.; Hu, A.; Jiang, Q.; Hou, Y.; Feng, Q.; Ojo, O.; Wang, X. An Almond-Based Low Carbohydrate Diet Improves Depression and Glycometabolism in Patients with Type 2 Diabetes through Modulating Gut Microbiota and GLP-1: A Randomized Controlled Trial. Nutrients 2020, 12, 3036. [Google Scholar] [CrossRef]
- Iatcu, C.O.; Steen, A.; Covasa, M. Gut Microbiota and Complications of Type-2 Diabetes. Nutrients 2021, 14, 166. [Google Scholar] [CrossRef]
- Salazar, J.; Angarita, L.; Morillo, V.; Navarro, C.; Martinez, M.S.; Chacin, M.; Torres, W.; Rajotia, A.; Rojas, M.; Cano, C.; et al. Microbiota and Diabetes Mellitus: Role of Lipid Mediators. Nutrients 2020, 12, 3039. [Google Scholar] [CrossRef]
- Bailey, C.J. Metformin: Historical overview. Diabetologia 2017, 60, 1566–1576. [Google Scholar] [CrossRef] [PubMed]
- Petroni, M.L.; Brodosi, L.; Marchignoli, F.; Sasdelli, A.S.; Caraceni, P.; Marchesini, G.; Ravaioli, F. Nutrition in Patients with Type 2 Diabetes: Present Knowledge and Remaining Challenges. Nutrients 2021, 13, 2748. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.S.; Ordovas, J.M. Precision nutrition for gut microbiome and diabetes research: Application of nutritional n-of-1 clinical trials. J. Diabetes 2021, 13, 1059–1061. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Fu, Y.; Tian, Y.; Gou, W.; Miao, Z.; Yang, M.; Ordovas, J.M.; Zheng, J.S. Individual Postprandial Glycemic Responses to Diet in n-of-1 Trials: Westlake N-of-1 Trials for Macronutrient Intake (WE-MACNUTR). J. Nutr. 2021, 151, 3158–3167. [Google Scholar] [CrossRef]
- Tian, Y.; Ma, Y.; Fu, Y.; Zheng, J.S. Application of n-of-1 Clinical Trials in Personalized Nutrition Research: A Trial Protocol for Westlake N-of-1 Trials for Macronutrient Intake (WE-MACNUTR). Curr. Dev. Nutr. 2020, 4, nzaa143. [Google Scholar] [CrossRef]




| Consensus Recommendation [14] | Resources Assumed | Application in Rural Areas |
|---|---|---|
| Effectiveness of diabetes nutrition therapy | ||
| Presence of dietitians with experience in diabetes. Clinics with multidisciplinary teams, including specialties (personnel). Local, affordable fitness studios (aerobic and resistance weights). | Absence of multidisciplinary clinics and other healthcare professionals, especially dietitians, shortage of nurses in rural areas [24]. There is a need for all types of healthcare professionals in rural areas [25]. The rural physician is at the frontline and must address MNT. |
| DSMES services must meet national standards, and must be accredited by the ADA or ADCES. They require a sponsor organization, dedicated multidisciplinary team, staff training, access to exercise facilities, meeting rooms, technology for data reporting, etc., see https://www.cdc.gov/diabetes/dsmes-toolkit/index.html. Access date 12 December 2023. | Developing a local DSMES program requires significant resources and capital investment and is probably out of scope for a rural family medicine physician in private practice. |
| Presence of dietitians with experience in diabetes. | The rural physician must address MNT. |
| Intensive lifestyle intervention programs typically require specialized foods, access to exercise facilities, and regular follow-ups with a multidisciplinary team. DPP require significant resources, at least three dedicated staff (lifestyle coach, data preparer, program coordinator), a CDC-approved curriculum (all aspects, including mental health), a multidisciplinary team to provide education, and capital investment. See https://www.cdc.gov/diabetes/prevention/index.html. Access date 12 December 2023. | Developing a local DPP requires significant resources and capital investment and is probably out of scope for a rural family medicine physician in private practice. The rural physician must address MNT. |
| Presence of dietitians with experience in diabetes. Universal insurance coverage for MNT. | Is a rural physician able to bill Medicare for MNT or does it have to be a dietitian? Can any form of nutritional therapy be billed for by a rural physician? Opportunity for Medicare and other insurers, to also reimburse rural physicians for providing nutritional therapy. In rural areas, there is limited access to health insurance, compared to urban areas [26]. |
| Local DPP. Presence of dietitians with experience in diabetes. | Is a rural physician able to bill Medicare for MNT or does it have to be a dietitian? Can any form of nutritional therapy be billed for by a rural physician? An opportunity for Medicare to also reimburse rural physicians for providing nutritional therapy. In rural areas there is limited access to health insurance, compared to urban areas [26]. |
| Macronutrients | ||
| Resources to assess macronutrient distribution (software, personnel, and time). Resources to follow-up on macronutrient distribution (software, personnel, and time). Easy access to a wide variety of foods. | For a review of dietary assessment toolkits, see [27]. There are relatively inexpensive, digital options for rural physicians if they want to perform dietary assessment, e.g., using Food Processor (ESHA, Salem, OR, USA), MyFood 24 (Nexus, Leeds, UK), or Power Diary (Salt Lake City, UT, USA). However, time is required to interpret the results and formulate a plan. |
| Resources to assess dietary intake, especially carbohydrate, how much carbohydrate at each meal, etc. (software, personnel, and time). Resources to follow-up on dietary intake (software, personnel, and time). Easy access to a wide variety of foods. Local, affordable fitness studios (aerobic and resistance weights). | For a review of dietary assessment toolkits, see [27]. There are, relatively inexpensive, digital options for rural physicians if they want to perform dietary assessment, e.g., Food Processor (ESHA, Salem, OR, USA), MyFood 24 (Nexus, Leeds, UK), Power Diary (Salt Lake City, UT, USA)—we are not endorsing these products. However, time is required to interpret the results. The rural physician can provide patient education on carbohydrate counting—may have to develop the content so it is appropriate for their patients. |
| Easy access to a wide variety of foods. Patient can afford to eat better. | The rural physician will have to be aware of where locals purchase foods and seek out foods with more fiber. Supplements may be the best option—must consider affordability. The rural physician can provide patient education on increasing fiber—may have to develop the content so it is appropriate for their patients. |
| Eating patterns | ||
| Easy access to a wide variety of foods, especially plant foods, which are central to all beneficial dietary patterns. Patient can afford to eat better. | Food insecurity may need to be considered. The rural physician can provide patient education on improving dietary patterns—may have to develop the content so it is based on what is available locally. |
| Easy access to a wide variety of foods, especially plant foods, which are central to all beneficial dietary patterns. Easy access to whole foods. Patient can afford to eat better. | Food insecurity may need to be considered. The rural physician can provide patient education on improving dietary patterns—may have to develop the content so it is based on what is available locally. |
| Easy access to a wide variety of foods, especially good-quality carbohydrate foods. Patient can afford to eat better. | This recommendation more than likely means reducing refined carbohydrate intake. The rural physician can provide patient education on reducing carbohydrate intake—may have to develop the content so it is based on what is available locally. |
| Easy access to a wide variety of foods, appropriate for a low- or very- low-carbohydrate diet. Patient can afford this specialized diet. | Food insecurity may need to be considered. The rural physician can provide patient education on reducing carbohydrate intake—may have to develop the content so it is based on what is available locally. |
| Energy balance and weight management | ||
| Resources to assess dietary intake, especially carbohydrate intake, how much carbohydrate consumed at each meal, etc. (software, personnel, and time). Resources to follow-up on dietary intake (software, personnel, and time). Local, convenient, DSMES program and DPP. | Developing a local DSMES program, or DPP, requires significant resources and capital investment and is probably out of scope for a rural family medicine physician in private practice. |
| Resources to assess dietary intake, i.e., portion sizes (software, personnel, and time). Resources to follow-up on dietary intake (software, personnel, and time). | Food insecurity may need to be considered. The rural physician can provide patient education on portion size and reducing carbohydrate—may have to develop the content so it is based on what is available locally. |
| Presence of diabetes weight loss programs, including DSMES, DPP and intensive lifestyle intervention. Resources to assess and follow-up for dietary intake (software, personnel, and time). Local, affordable exercise facilities (aerobic and resistance weights). | Achieving consistent and sustained weight loss in patients with diabetes requires time and effort. In addition, patients need support to maintain motivation. Rural physician would need to develop a weight loss program appropriate for the area and patients. This may be out of scope for the rural physician. |
| Resources to assess dietary intake and create eating plans with caloric deficits (software, personnel, and time). Clinics with multidisciplinary teams, including specialties (personnel). Local, affordable exercise facilities (aerobic and resistance weights). Health insurance that covers weight loss medications and/or metabolic surgery. | Rural physician would need to develop a weight loss program, with access to medications and/or metabolic surgery, appropriate for the area and patients. This may be out of scope for the rural physician. |
| Resources to assess dietary intake and create eating plans with caloric deficits (software, personnel, and time). Local, affordable exercise facilities (aerobic and resistance weights). Health insurance that covers weight loss medications. | The rural physician would need to develop a weight loss program, with access to medications, appropriate for the area and patients. This may be out of scope for the rural physician. |
| Resources to assess dietary intake and create eating plans with caloric deficits (software, personnel, and time). Clinics with multidisciplinary teams, including specialties (personnel). Local, affordable exercise facilities (aerobic and resistance weights). Easy access to a wide variety of foods. | The rural physician would need to develop a healthy eating plan to help prevent diabetes appropriate for the area and patients. This may be out of scope for the rural physician. |
| Presence of local DSMES program. Easy access to a mental health specialist/multidisciplinary clinical team. Presence of dietitians with experience in diabetes and eating disorders. Health insurance that covers eating disorder therapies. | The rural physician, if comfortable, could begin to address eating disorders; however, specialty care is needed. |
| Sweeteners | ||
| No comment. | No issue for the rural physician to educate on this topic. |
| No comment. | No issue for the rural physician to educate on this topic. |
| Alcohol consumption | ||
| No comment. | No issue for the rural physician to educate on this topic. |
| No comment. | No issue for the rural physician to educate on this topic. |
| Micronutrients, herbal supplements, and risk of medication-associated deficiency | ||
| No comment. | No issue for the rural physician to educate on this topic. However, considering the poorer diets in rural areas, a daily multinutrient supplement may help prevent insufficiencies. |
| No comment. | No issue for the rural physician to educate on this topic. However, considering the poorer diets in rural areas, a daily multinutrient supplement may help prevent insufficiencies. |
| No comment. | No issue for the rural physician to educate on this topic. |
| MNT and antihyperglycemic medications (including insulin) | ||
| Presence of dietitians with experience in diabetes. | The rural physician has to address MNT. |
| No comment. | No issue for the rural physician to educate on this topic. |
| Resources to assess dietary intake, i.e., carbohydrate intakes at meals and snack time (software, personnel, and time). | The rural physician would need to develop an individualized eating plan to help keep carbohydrate intake consistent throughout the day, that is appropriate for the area. This may be out of scope for the rural physician. |
| Health insurance that covers CGM or SMBG. | No issue for the rural physician to educate on this topic. |
| Role of nutrition therapy in the prevention and management of diabetes complications (CVD, diabetic kidney disease, and gastroparesis) | ||
| No comment. | No issue for the rural physician to educate on this topic. |
| No comment. | No issue for the rural physician to educate on this topic. |
| No comment. | No issue for the rural physician to educate on this topic. |
| Easy access to a wide variety of foods. | No issue for the rural physician to educate on this topic, possibly offer supplements as an alternative. |
| Resources to assess dietary intake, i.e., protein intake (software, personnel, and time). Presence of dietitians with experience in diabetes and DKD. | This can be a challenge for rural physicians, as other guidelines and data exist. The National Kidney Foundations nutritional guidelines suggest 0.6–0.8 g/kg/d, but with higher caloric intake, and more medical supervision to mitigate any potential risk for malnutrition [28]. Two-year data from Virta Health (poster) show that sustained nutritional ketosis may help preserve kidney function [29]. A meta-analysis supports that lower-carbohydrate diets maintain eGFR better (albeit by a small number) than standard diets do [30]. |
| Easy access to the appropriate foods. | Appropriate foods, including medical foods, may not be readily available. |
| Resources to assess dietary intake, i.e., carbohydrate intakes (software, personnel, and time). Coupling with CGM or SMBG to make the patient more aware of what foods contribute to hyperglycemia. Health insurance that covers CGM devices or SMBG. | The rural physician can educate on carbohydrate counting and carbohydrate quality. The rural physician would need to develop a program appropriate for the area and patients. |
| Health insurance that covers CGM and/or insulin pump therapy. | The rural physician can educate on carbohydrate counting and carbohydrate quality. The rural physician would need to develop a food list appropriate for the area and patients. |
| Personalized nutrition | ||
| Resources to assess and follow-up for dietary intake, (software, personnel, and time). Easy access to specialist/multidisciplinary clinical team. Presence of dietitians with experience in diabetes. | The field of personalized nutrition is still in its infancy [31]; however, the rural population requires some form of personalized nutrition, distinct from those in urban areas. Currently, this does not seem applicable to rural physicians. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kelly, O.J.; Deya Edelen, E.; Sharma, A.; Kashyap, K.; Patel, R.; Saiprakash, S.; Shah, A.; Konduri, S. Decoding Diabetes Nutritional Guidelines for Physicians in Underserved American Populations. Endocrines 2024, 5, 1-23. https://doi.org/10.3390/endocrines5010001
Kelly OJ, Deya Edelen E, Sharma A, Kashyap K, Patel R, Saiprakash S, Shah A, Konduri S. Decoding Diabetes Nutritional Guidelines for Physicians in Underserved American Populations. Endocrines. 2024; 5(1):1-23. https://doi.org/10.3390/endocrines5010001
Chicago/Turabian StyleKelly, Owen J., Elizabeth Deya Edelen, Anika Sharma, Karishma Kashyap, Radhika Patel, Samyukthaa Saiprakash, Ali Shah, and Sriya Konduri. 2024. "Decoding Diabetes Nutritional Guidelines for Physicians in Underserved American Populations" Endocrines 5, no. 1: 1-23. https://doi.org/10.3390/endocrines5010001
APA StyleKelly, O. J., Deya Edelen, E., Sharma, A., Kashyap, K., Patel, R., Saiprakash, S., Shah, A., & Konduri, S. (2024). Decoding Diabetes Nutritional Guidelines for Physicians in Underserved American Populations. Endocrines, 5(1), 1-23. https://doi.org/10.3390/endocrines5010001