Effects of One-Shot Hyaluronic Acid Injection in Lifelong Premature Ejaculation: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
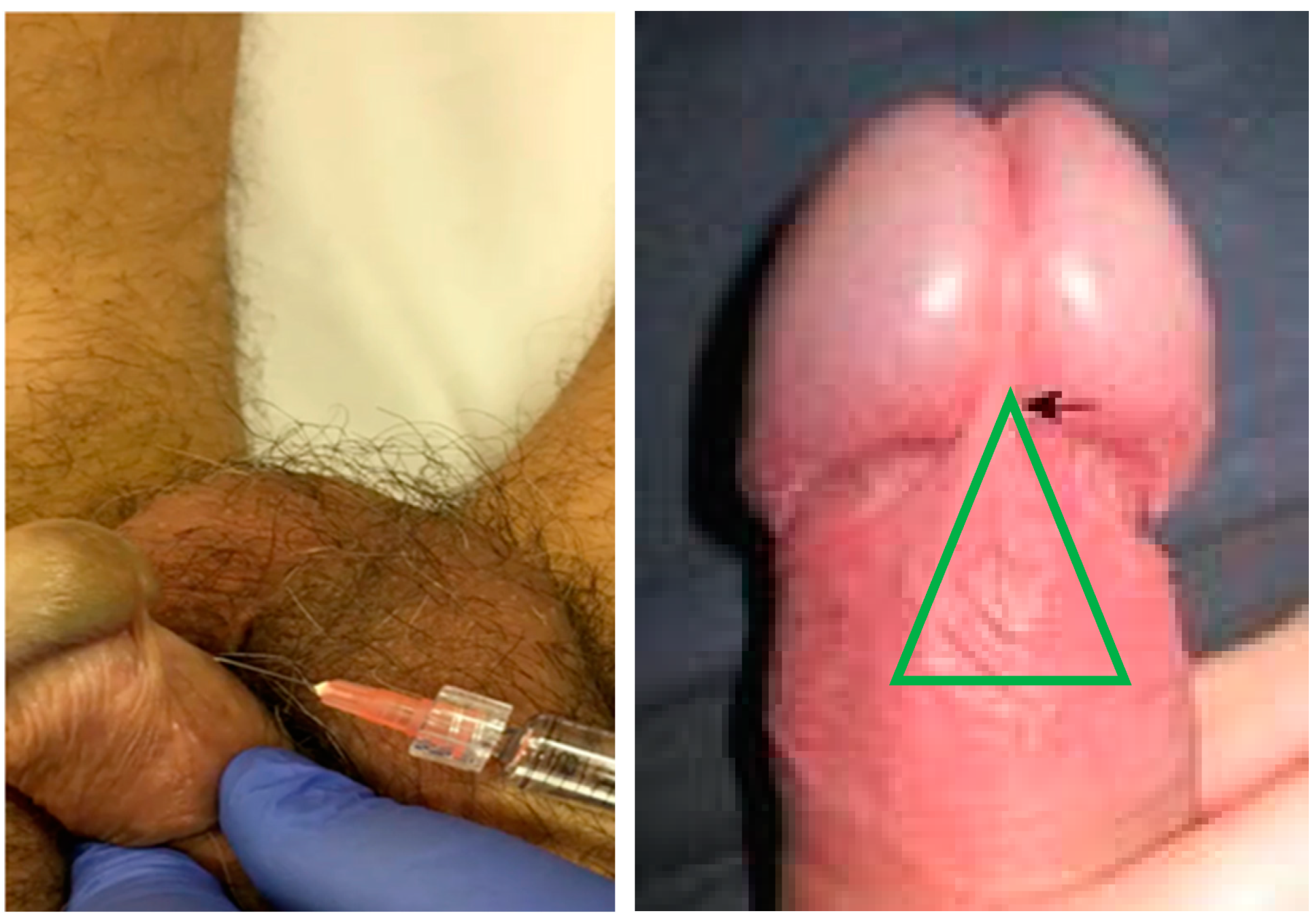
2.2. Hyaluronic Acid Injection
2.3. Statistical Analysis
3. Results
3.1. HA Injection Effect on IELT
3.2. PEDT and IIEF Questionnaires before and after HA Injection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rowland, D.L.; Althof, S.E.; McMahon, C.G. The Unfinished Business of Defining Premature Ejaculation: The Need for Targeted Research. Sex. Med. Rev. 2022, 10, 323–340. [Google Scholar] [CrossRef]
- Althof, S.E.; McMahon, C.G.; Waldinger, M.D.; Serefoglu, E.C.; Shindel, A.W.; Adaikan, P.G.; Becher, E.; Dean, J.; Giuliano, F.; Hellstrom, W.J.; et al. An Update of the International Society of Sexual Medicine’s Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). Sex. Med. 2014, 2, 60–90. [Google Scholar] [CrossRef]
- Soni, K.K.; Jeong, H.S.; Jang, S. Neurons for Ejaculation and Factors Affecting Ejaculation. Biology 2022, 11, 686. [Google Scholar] [CrossRef]
- Martin-Tuite, P.; Shindel, A.W. Management Options for Premature Ejaculation and Delayed Ejaculation in Men. Sex. Med. Rev. 2020, 8, 473–485. [Google Scholar] [CrossRef]
- Hu, Q.B.; Zhang, D.; Ma, L.; Ng, D.M.; Haleem, M.; Ma, Q. Progresses in pharmaceutical and surgical management of premature ejaculation. Chin. Med. J. 2019, 132, 2362–2372. [Google Scholar] [CrossRef]
- Morales, A.; Barada, J.; Wyllie, M.G. A review of the current status of topical treatments for premature ejaculation. BJU Int. 2007, 100, 493–501. [Google Scholar] [CrossRef]
- Liu, Q.; Li, S.; Zhang, Y.; Cheng, Y.; Fan, J.; Jiang, L.; Li, S.; Tang, Y.; Zeng, H.; Wang, J.; et al. Anatomic Basis and Clinical Effect of Selective Dorsal Neurectomy for Patients with Lifelong Premature Ejaculation: A Randomized Controlled Trial. J. Sex. Med. 2019, 16, 522–530. [Google Scholar] [CrossRef]
- Kosseifi, F.; Chebbi, A.; Raad, N.; Ndayra, A.; El Samad, R.; Achkar, K.; Durand, X.; Noujeim, A. Glans penis augmentation using hyaluronic acid for the treatment of premature ejaculation: A narrative review. Transl. Androl. Urol. 2020, 9, 2814–2820. [Google Scholar] [CrossRef] [PubMed]
- Symonds, T.; Perelman, M.A.; Althof, S.; Giuliano, F.; Martin, M.; May, K.; Abraham, L.; Crossland, A.; Morris, M. Development and validation of a premature ejaculation diagnostic tool. Eur. Urol. 2007, 52, 565–573. [Google Scholar] [CrossRef]
- Waldinger, M.D.; Zwinderman, A.H.; Olivier, B.; Schweitzer, D.H. Geometric Mean IELT and Premature Ejaculation: Appropriate Statistics to Avoid Overestimation of Treatment Efficacy. J. Sex. Med. 2008, 5, 492–499. [Google Scholar] [CrossRef]
- Waldinger, M.D.; Olivier, B. Utility of selective serotonin reuptake inhibitors in premature ejaculation. Curr. Opin. Investig. Drugs 2004, 5, 743–747. [Google Scholar]
- Olivier, B.; Chan, J.S.; Pattij, T.; de Jong, T.R.; Oosting, R.S.; Veening, J.G.; Waldinger, M.D. Psychopharmacology of male rat sexual behavior: Modeling human sexual dysfunctions? Int. J. Impot. Res. 2006, 18 (Suppl. S1), S14–S23. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Waldinger, M.D. Premature ejaculation: Different pathophysiologies and etiologies determine its treatment. J. Sex. Marital Ther. 2008, 34, 1–13. [Google Scholar] [CrossRef] [PubMed]
- McMahon, C.G.; Porst, H. Oral Agents for the Treatment of Premature Ejaculation: Review of Efficacy and Safety in the Context of the Recent International Society for Sexual Medicine Criteria for Lifelong Premature Ejaculation. J. Sex. Med. 2011, 8, 2707–2725. [Google Scholar] [CrossRef]
- Russo, A.; Capogrosso, P.; Ventimiglia, E.; La Croce, G.; Boeri, L.; Montorsi, F.; Salonia, A. Efficacy and safety of dapoxetine in treatment of premature ejaculation: An evidence-based review. Int. J. Clin. Pr. 2016, 70, 723–733. [Google Scholar] [CrossRef] [PubMed]
- Jiann, B.P.; Huang, Y.J. Assessing satisfaction in men with premature ejaculation after dapoxetine treatment in real-world practice. Int. J. Clin. Pr. 2015, 69, 1326–1333. [Google Scholar] [CrossRef]
- Mondaini, N.; Fusco, F.; Cai, T.; Benemei, S.; Mirone, V.; Bartoletti, R. Dapoxetine treatment in patients with lifelong premature ejaculation: The reasons of a “Waterloo”. Urology 2013, 82, 620–624. [Google Scholar] [CrossRef]
- Jern, P.; Santtila, P.; Johansson, A.; Sandnabba, N.K. Genetic and environmental effects on the continuity of ejaculatory dysfunction. BJU Int. 2010, 105, 1698–1704. [Google Scholar] [CrossRef]
- Jern, P.; Santtila, P.; Witting, K.; Alanko, K.; Harlaar, N.; Johansson, A.; von der Pahlen, B.; Varjonen, M.; Vikström, N.; Algars, M.; et al. Premature and delayed ejaculation: Genetic and environmental effects in a population-based sample of Finnish twins. J. Sex. Med. 2007, 4, 1739–1749. [Google Scholar] [CrossRef]
- Kim, J.J.; Kwak, T.I.; Jeon, B.G.; Cheon, J.; Moon, D.G. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int. J. Impot. Res. 2004, 16, 547–551. [Google Scholar] [CrossRef][Green Version]
- Quan, Y.; Gao, Z.-R.; Dai, X.; Kuang, L.; Zhang, M.; Li, Q.; Xu, T.; Zhang, X.-W. Complications and management of penile augmentation with hyaluronic acid injection. Asian J. Androl. 2021, 23, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Kwak, T.I.; Jin, M.H.; Kim, J.J.; Moon, D.G. Long-term effects of glans penis augmentation using injectable hyaluronic acid gel for premature ejaculation. Int. J. Impot. Res. 2008, 20, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Littara, A.; Palmieri, B.; Rottigni, V.; Iannitti, T. A clinical study to assess the effectiveness of a hyaluronic acid-based procedure for treatment of premature ejaculation. Int. J. Impot. Res. 2013, 25, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, H.; Abdelnasser, T.; Hosny, H.; Selim, O.; Al-Ahwany, A.; Shamloul, R. Treatment of premature ejaculation by glans penis augmentation using hyaluronic acid gel: A pilot study. Andrologia 2012, 44 (Suppl. S1), 650–653. [Google Scholar] [CrossRef]
- Alahwany, A.; Ragab, M.W.; Zaghloul, A.; Abdallah, H.; Mostafa, T. Hyaluronic acid injection in glans penis for treatment of premature ejaculation: A randomized controlled cross-over study. Int. J. Impot. Res. 2019, 31, 348–355. [Google Scholar] [CrossRef]
- Zucchi, A.; Scroppo, F.I.; Capogrosso, P.; Salonia, A.; Duante, J.; Bini, V.; Liguori, G.; Bartoletti, R. Clinical use of hyaluronic acid in andrology: A review. Andrology 2022, 10, 42–50. [Google Scholar] [CrossRef]

| Median (IQR) | |
|---|---|
| Age (years) | 40 (36.5–45.5) |
| Glucose (mg/dL) | 89 (83.5–96) |
| BMI (Kg/m2) | 25.8 (24.15–26.85) |
| HGB (gr/dL) | 14.8 (14.15–16.3) |
| Total Cholesterol (mg/dL) | 200 (195.5–211.5) |
| HDL Cholesterol (mg/dL) | 57 (48–66) |
| LDL Cholesterol (mg/dL) | 120.8 (104.8–135) |
| Tryglicerid (mg/dL) | 96 (83–146) |
| LH (mUI/mL) | 5.5 (4.75–6.15) |
| FSH (mIU/mL) | 6.4 (5.3–7.75) |
| TT (ng/dL) | 418 (322–534) |
| PRL (ng/mL) | 7.7 (4.89–12.15) |
| PSA (ng/mL) | 2.54 (1.94–3.04) |
| TSH (µIU/mL) | 2.56 (1.14–3.62) |
| Days | Geometric Mean (SD) | Median (IQR) | Folder Increase (95% CI) | p |
|---|---|---|---|---|
| Baseline | 38.65 (1.21) | 40 (33–44) | - | - |
| 30 | 72.24 (1.27) | 79 (62–85.5) | 1.87 (1.84–1.9) | <0.0001 |
| 60 | 63.75 (1.35) | 72 (47–80.5) | 1.65 (1.58–1.72) | <0.0001 |
| 90 | 41.24 (1.17) | 41 (37.5–45.5) | 1.07 (1.05–1.08) | 0.018 |
| Baseline | 30 Days | 60 Days | 90 Days | |
|---|---|---|---|---|
| PEDT | 14 (13–15) | 12 (11–13) * | 12 (11–13) * | 15 (13–15) |
| IIEF | 52 (47–51) | 54 (50.5–57) | 51 (49–53) | 48 (45.5–51) |
| Erectile Function | 29 (26–28) | 27 (26–28) | 27 (25.5–27) | 26 (25–27.5) |
| Orgasmic Function | 7 (5–6.5) | 6 (5–7) | 5 (5–6) | 5 (5–6) |
| Sexual Desire | 7 (6–7) | 6 (6–7) | 6 (5–7) | 6 (5–7) |
| Intercourse Satisfaction | 6 (5–7) | 10 (6–11) * | 7 (6–8) * | 6 (5.5–7) |
| Overall Satisfaction | 3 (3–4) | 5 (5–6) * | 6 (4–7) * | 4 (4–5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perri, A.; Lofaro, D.; Iuliano, S.; Bossio, S.; Rago, V.; Damiano, R.; Di Luigi, L.; La Vignera, S.; Mondaini, N.; Aversa, A. Effects of One-Shot Hyaluronic Acid Injection in Lifelong Premature Ejaculation: A Pilot Study. Endocrines 2022, 3, 538-544. https://doi.org/10.3390/endocrines3030044
Perri A, Lofaro D, Iuliano S, Bossio S, Rago V, Damiano R, Di Luigi L, La Vignera S, Mondaini N, Aversa A. Effects of One-Shot Hyaluronic Acid Injection in Lifelong Premature Ejaculation: A Pilot Study. Endocrines. 2022; 3(3):538-544. https://doi.org/10.3390/endocrines3030044
Chicago/Turabian StylePerri, Anna, Danilo Lofaro, Stefano Iuliano, Sabrina Bossio, Vittoria Rago, Rocco Damiano, Luigi Di Luigi, Sandro La Vignera, Nicola Mondaini, and Antonio Aversa. 2022. "Effects of One-Shot Hyaluronic Acid Injection in Lifelong Premature Ejaculation: A Pilot Study" Endocrines 3, no. 3: 538-544. https://doi.org/10.3390/endocrines3030044
APA StylePerri, A., Lofaro, D., Iuliano, S., Bossio, S., Rago, V., Damiano, R., Di Luigi, L., La Vignera, S., Mondaini, N., & Aversa, A. (2022). Effects of One-Shot Hyaluronic Acid Injection in Lifelong Premature Ejaculation: A Pilot Study. Endocrines, 3(3), 538-544. https://doi.org/10.3390/endocrines3030044










