Skeletal Characteristics of Children and Adolescents with Turner Syndrome
Abstract
1. Introduction
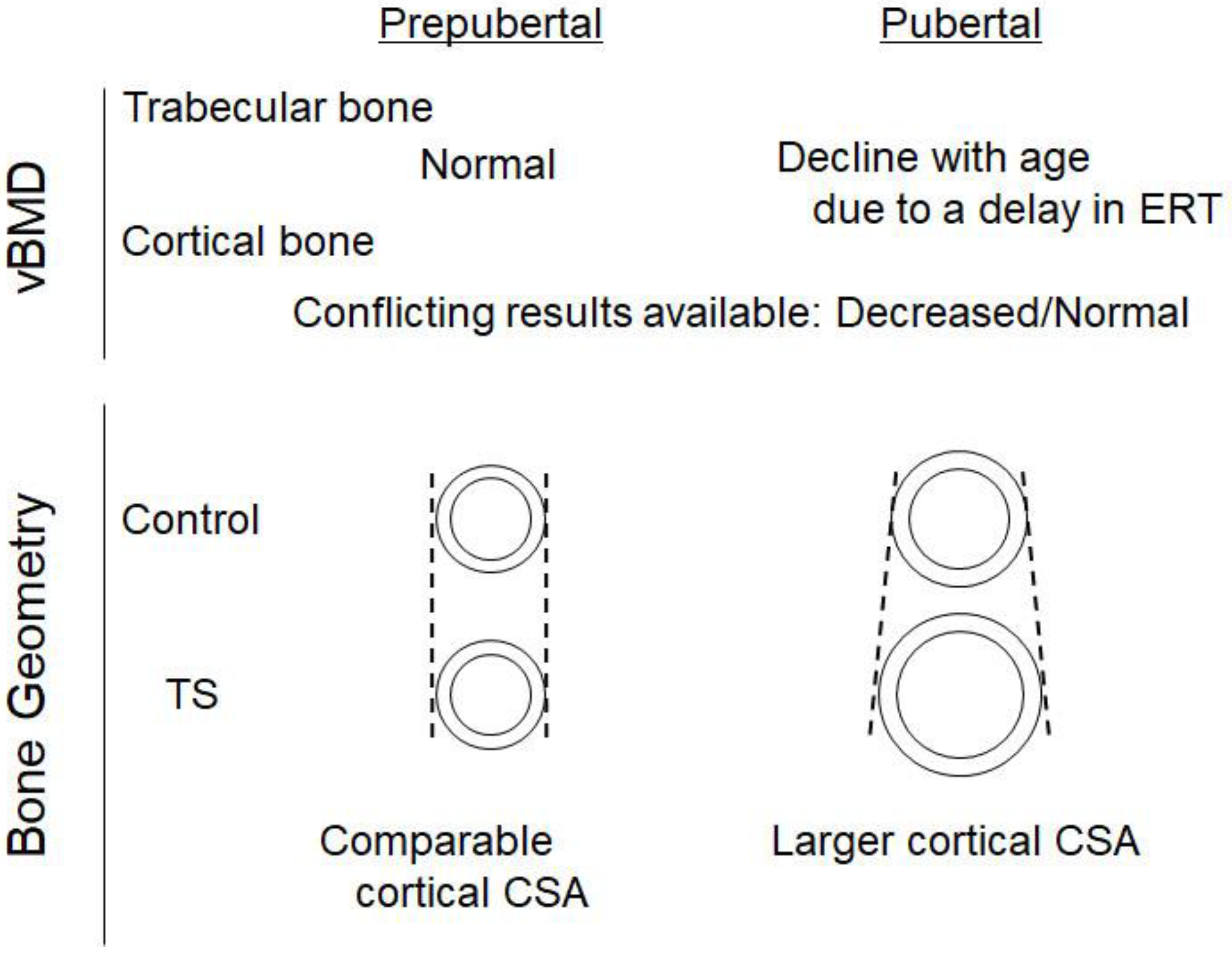
2. BMD in Prepubertal Children with TS
3. BMD in Peripubertal and Pubertal Girls with TS
3.1. Effects of Estrogen Insufficiency on the BMD of the Trabecular Bone
3.2. Effects of Estrogen Insufficiency on the BMD of Cortical Bone
4. Bone Geometry and Strength in TS during Pre-Pubertal and Pubertal Periods
5. Fracture Risks in Children and Adolescents with TS
6. Effects of Growth Hormone Treatment on Bone Mass and Geometry in Children with TS
7. Effects of ERT during Adolescence on BMD in Young Adults with TS
8. Future Directions and Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gravholt, C.H.; Andersen, N.H.; Conway, G.S.; Dekkers, O.M.; Geffner, M.E.; Klein, K.O.; Lin, A.E.; Mauras, N.; Quigley, C.A.; Rubin, K.; et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: Proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur. J. Endocrinol. 2017, 177, G1–G70. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Viuff, M.H.; Brun, S.; Stochholm, K.; Andersen, N.H. Turner syndrome: Mechanisms and management. Nat. Rev. Endocrinol. 2019, 15, 601–614. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Vestergaard, P.; Hermann, A.P.; Mosekilde, L.; Brixen, K.; Christiansen, J.S. Increased fracture rates in Turner’s syndrome: A nationwide questionnaire survey. Clin. Endocrinol. 2003, 59, 89–96. [Google Scholar] [CrossRef]
- Freriks, K.; Timmermans, J.; Beerendonk, C.C.; Verhaak, C.M.; Netea-Maier, R.T.; Otten, B.J.; Braat, D.D.; Smeets, D.F.; Kunst, D.H.; Hermus, A.R.; et al. Standardized multidisciplinary evaluation yields significant previously undiagnosed morbidity in adult women with Turner syndrome. J. Clin. Endocrinol. Metab. 2011, 96, E1517–E1526. [Google Scholar] [CrossRef]
- Han, T.S.; Cadge, B.; Conway, G.S. Hearing impairment and low bone mineral density increase the risk of bone fractures in women with Turner’s syndrome. Clin. Endocrinol. 2006, 65, 643–647. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Juul, S.; Naeraa, R.W.; Hansen, J. Morbidity in Turner syndrome. J. Clin. Epidemiol. 1998, 51, 147–158. [Google Scholar] [CrossRef]
- Cintron, D.; Rodriguez-Gutierrez, R.; Serrano, V.; Latortue-Albino, P.; Erwin, P.J.; Murad, M.H. Effect of estrogen replacement therapy on bone and cardiovascular outcomes in women with turner syndrome: A systematic review and meta-analysis. Endocrine 2017, 55, 366–375. [Google Scholar] [CrossRef]
- Landin-Wilhelmsen, K.; Bryman, I.; Windh, M.; Wilhelmsen, L. Osteoporosis and fractures in Turner syndrome-importance of growth promoting and oestrogen therapy. Clin. Endocrinol. 1999, 51, 497–502. [Google Scholar] [CrossRef]
- Klein, K.O.; Rosenfield, R.L.; Santen, R.J.; Gawlik, A.M.; Backeljauw, P.F.; Gravholt, C.H.; Sas, T.C.J.; Mauras, N. Estrogen Replacement in Turner Syndrome: Literature Review and Practical Considerations. J. Clin. Endocrinol. Metab. 2018, 103, 1790–1803. [Google Scholar] [CrossRef]
- Cameron-Pimblett, A.; Davies, M.C.; Burt, E.; Talaulikar, V.S.; La Rosa, C.; King, T.F.J.; Conway, G.S. Effects of Estrogen Therapies on Outcomes in Turner Syndrome: Assessment of Induction of Puberty and Adult Estrogen Use. J. Clin. Endocrinol. Metab. 2019, 104, 2820–2826. [Google Scholar] [CrossRef] [PubMed]
- Nishigaki, S.; Itonaga, T.; Hasegawa, Y.; Kawai, M. Starting age of oestrogen-progestin therapy is negatively associated with bone mineral density in young adults with Turner syndrome independent of age and body mass index. Clin. Endocrinol. 2021, 95, 84–91. [Google Scholar] [CrossRef]
- Itonaga, T.; Koga, E.; Nishigaki, S.; Kawai, M.; Sakakibara, H.; Hasegawa, Y. A retrospective multicenter study of bone mineral density in adolescents and adults with Turner syndrome in Japan. Endocr. J. 2020, 67, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Kodama, M.; Komura, H.; Kodama, T.; Nishio, Y.; Kimura, T. Estrogen therapy initiated at an early age increases bone mineral density in Turner syndrome patients. Endocr. J. 2012, 59, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.H.; Wong, P.; Strauss, B.J.; Ebeling, P.R.; Milat, F.; Vincent, A. A Cross-Sectional and Longitudinal Analysis of Trabecular Bone Score in Adults With Turner Syndrome. J. Clin. Endocrinol. Metab. 2018, 103, 3792–3800. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.H.; Wong, P.; Strauss, B.J.; Jones, G.; Ebeling, P.R.; Milat, F.; Vincent, A. Delay in estrogen commencement is associated with lower bone mineral density in Turner syndrome. Climacteric 2017, 20, 436–441. [Google Scholar] [CrossRef]
- Augoulea, A.; Zachou, G.; Lambrinoudaki, I. Turner syndrome and osteoporosis. Maturitas 2019, 130, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Soucek, O.; Zapletalova, J.; Zemkova, D.; Snajderova, M.; Novotna, D.; Hirschfeldova, K.; Plasilova, I.; Kolouskova, S.; Rocek, M.; Hlavka, Z.; et al. Prepubertal girls with Turner syndrome and children with isolated SHOX deficiency have similar bone geometry at the radius. J. Clin. Endocrinol. Metab. 2013, 98, E1241–E1247. [Google Scholar] [CrossRef]
- Rajpathak, S.N.; Vellarikkal, S.K.; Patowary, A.; Scaria, V.; Sivasubbu, S.; Deobagkar, D.D. Human 45,X fibroblast transcriptome reveals distinct differentially expressed genes including long noncoding RNAs potentially associated with the pathophysiology of Turner syndrome. PLoS ONE 2014, 9, e100076. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.L.; Long, L.M.; Feuillan, P.; Cassorla, F.; Cutler, G.B., Jr. Normal bone density of the wrist and spine and increased wrist fractures in girls with Turner’s syndrome. J. Clin. Endocrinol. Metab. 1991, 73, 355–359. [Google Scholar] [CrossRef]
- Hogler, W.; Briody, J.; Moore, B.; Garnett, S.; Lu, P.W.; Cowell, C.T. Importance of estrogen on bone health in Turner syndrome: A cross-sectional and longitudinal study using dual-energy X-ray absorptiometry. J. Clin. Endocrinol. Metab. 2004, 89, 193–199. [Google Scholar] [CrossRef][Green Version]
- Soucek, O.; Lebl, J.; Snajderova, M.; Kolouskova, S.; Rocek, M.; Hlavka, Z.; Cinek, O.; Rittweger, J.; Sumnik, Z. Bone geometry and volumetric bone mineral density in girls with Turner syndrome of different pubertal stages. Clin. Endocrinol. 2011, 74, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Nanao, K.; Tsuchiya, Y.; Kotoh, S.; Hasegawa, Y. Low vertebral cancellous bone density in peripubertal girls with Turner’s syndrome and boys with hypogonadism. J. Pediatr. Endocrinol. Metab. 2002, 15, 1537–1542. [Google Scholar] [CrossRef]
- Bakalov, V.K.; Axelrod, L.; Baron, J.; Hanton, L.; Nelson, L.M.; Reynolds, J.C.; Hill, S.; Troendle, J.; Bondy, C.A. Selective reduction in cortical bone mineral density in turner syndrome independent of ovarian hormone deficiency. J. Clin. Endocrinol. Metab. 2003, 88, 5717–5722. [Google Scholar] [CrossRef] [PubMed]
- Soucek, O.; Schonau, E.; Lebl, J.; Willnecker, J.; Hlavka, Z.; Sumnik, Z. A 6-Year Follow-Up of Fracture Incidence and Volumetric Bone Mineral Density Development in Girls With Turner Syndrome. J. Clin. Endocrinol. Metab. 2018, 103, 1188–1197. [Google Scholar] [CrossRef]
- Rauch, F.; Tutlewski, B.; Schonau, E. The bone behind a low areal bone mineral density: Peripheral quantitative computed tomographic analysis in a woman with osteogenesis imperfecta. J. Musculoskelet. Neuronal Interact. 2002, 2, 306–308. [Google Scholar]
- Pitukcheewanont, P.; Numbenjapon, N.; Safani, D.; Rossmiller, S.; Gilsanz, V.; Costin, G. Bone size and density measurements in prepubertal children with Turner syndrome prior to growth hormone therapy. Osteoporos. Int. 2011, 22, 1709–1715. [Google Scholar] [CrossRef] [PubMed]
- Shaw, N.J.; Rehan, V.K.; Husain, S.; Marshall, T.; Smith, C.S. Bone mineral density in Turner’s syndrome—A longitudinal study. Clin. Endocrinol. 1997, 47, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Holroyd, C.R.; Davies, J.H.; Taylor, P.; Jameson, K.; Rivett, C.; Cooper, C.; Dennison, E.M. Reduced cortical bone density with normal trabecular bone density in girls with Turner syndrome. Osteoporos. Int. 2010, 21, 2093–2099. [Google Scholar] [CrossRef] [PubMed]
- Carrascosa, A.; Gussinye, M.; Terradas, P.; Yeste, D.; Audi, L.; Vicens-Calvet, E. Spontaneous, but not induced, puberty permits adequate bone mass acquisition in adolescent Turner syndrome patients. J. Bone Miner. Res. 2000, 15, 2005–2010. [Google Scholar] [CrossRef]
- Seeman, E. Clinical review 137: Sexual dimorphism in skeletal size, density, and strength. J. Clin. Endocrinol. Metab. 2001, 86, 4576–4584. [Google Scholar] [CrossRef]
- Zhang, X.Z.; Kalu, D.N.; Erbas, B.; Hopper, J.L.; Seeman, E. The effects of gonadectomy on bone size, mass, and volumetric density in growing rats are gender-, site-, and growth hormone-specific. J. Bone Miner. Res. 1999, 14, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Yeh, J.K.; Chen, M.M.; Aloia, J.F. Ovariectomy-induced high turnover in cortical bone is dependent on pituitary hormone in rats. Bone 1996, 18, 443–450. [Google Scholar] [CrossRef]
- Turner, R.T.; Hannon, K.S.; Demers, L.M.; Buchanan, J.; Bell, N.H. Differential effects of gonadal function on bone histomorphometry in male and female rats. J. Bone Miner. Res. 1989, 4, 557–563. [Google Scholar] [CrossRef]
- Turner, C.H.; Burr, D.B. Basic biomechanical measurements of bone: A tutorial. Bone 1993, 14, 595–608. [Google Scholar] [CrossRef]
- Dantas, N.C.B.; Braz, A.F.; Malaquias, A.; Lemos-Marini, S.; Arnhold, I.J.P.; Silveira, E.R.; Antonini, S.R.; Guerra-Junior, G.; Mendonca, B.; Jorge, A.; et al. Adult Height in 299 Patients with Turner Syndrome with or without Growth Hormone Therapy: Results and Literature Review. Horm. Res. Paediatr. 2021, 94, 63–70. [Google Scholar] [CrossRef]
- Ahn, J.M.; Suh, J.H.; Kwon, A.R.; Chae, H.W.; Kim, H.S. Final Adult Height after Growth Hormone Treatment in Patients with Turner Syndrome. Horm. Res. Paediatr. 2019, 91, 373–379. [Google Scholar] [CrossRef]
- Lanes, R.; Lindberg, A.; Carlsson, M.; Chrysis, D.; Aydin, F.; Camacho-Hubner, C.; King, D.; Davenport, M. Near Adult Height in Girls with Turner Syndrome Treated with Growth Hormone Following Either Induced or Spontaneous Puberty. J. Pediatr. 2019, 212, 172–179.e1. [Google Scholar] [CrossRef] [PubMed]
- Cleemann Wang, A.; Hagen, C.P.; Nedaeifard, L.; Juul, A.; Jensen, R.B. Growth and Adult Height in Girls With Turner Syndrome Following IGF-1 Titrated Growth Hormone Treatment. J. Clin. Endocrinol. Metab. 2020, 105, 2566–2574. [Google Scholar] [CrossRef]
- Fujita, K.; Yokoya, S.; Fujieda, K.; Shimatsu, A.; Tachibana, K.; Tanaka, H.; Tanizawa, T.; Teramoto, A.; Nishi, Y.; Hasegawa, Y.; et al. Adult heights of 258 girls with turner syndrome on low dose of growth hormone therapy in Japan. Clin. Pediatr. Endocrinol. 2010, 19, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Yan, K.; Yuping, X.; Zhang, Q.; Wang, L.; Gong, F.; Zhu, H.; Xia, W.; Pan, H. Bone microarchitecture and volumetric bone density impairment in young male adults with childhood-onset growth hormone deficiency. Eur. J. Endocrinol. 2019, 180, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Tritos, N.A.; Johannsson, G.; Korbonits, M.; Miller, K.K.; Feldt-Rasmussen, U.; Yuen, K.C.; King, D.; Mattsson, A.F.; Jonsson, P.J.; Koltowska-Haggstrom, M.; et al. Effects of long-term growth hormone replacement in adults with growth hormone deficiency following cure of acromegaly: A KIMS analysis. J. Clin. Endocrinol. Metab. 2014, 99, 2018–2029. [Google Scholar] [CrossRef] [PubMed]
- Barake, M.; Klibanski, A.; Tritos, N.A. Effects of recombinant human growth hormone therapy on bone mineral density in adults with growth hormone deficiency: A meta-analysis. J. Clin. Endocrinol. Metab. 2014, 99, 852–860. [Google Scholar] [CrossRef] [PubMed]
- Willemsen, R.H.; Arends, N.J.; Bakker-van Waarde, W.M.; Jansen, M.; van Mil, E.G.; Mulder, J.; Odink, R.J.; Reeser, M.; Rongen-Westerlaken, C.; Stokvis-Brantsma, W.H.; et al. Long-term effects of growth hormone (GH) treatment on body composition and bone mineral density in short children born small-for-gestational-age: Six-year follow-up of a randomized controlled GH trial. Clin. Endocrinol. 2007, 67, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Sas, T.C.; de Muinck Keizer-Schrama, S.M.; Stijnen, T.; van Teunenbroek, A.; van Leeuwen, W.J.; Asarfi, A.; van Rijn, R.R.; Drop, S.L.; Dutch Advisory Group on Growth Hormone. Bone mineral density assessed by phalangeal radiographic absorptiometry before and during long-term growth hormone treatment in girls with Turner’s syndrome participating in a randomized dose-response study. Pediatr. Res. 2001, 50, 417–422. [Google Scholar] [CrossRef][Green Version]
- Ari, M.; Bakalov, V.K.; Hill, S.; Bondy, C.A. The effects of growth hormone treatment on bone mineral density and body composition in girls with turner syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 4302–4305. [Google Scholar] [CrossRef]
- Aycan, Z.; Cetinkaya, E.; Darendeliler, F.; Vidinlisan, S.; Bas, F.; Bideci, A.; Demirel, F.; Darcan, S.; Buyukgebiz, A.; Yildiz, M.; et al. The effect of growth hormone treatment on bone mineral density in prepubertal girls with Turner syndrome: A multicentre prospective clinical trial. Clin. Endocrinol. 2008, 68, 769–772. [Google Scholar] [CrossRef]
- Bakalov, V.K.; Van, P.L.; Baron, J.; Reynolds, J.C.; Bondy, C.A. Growth hormone therapy and bone mineral density in Turner syndrome. J. Clin. Endocrinol. Metab. 2004, 89, 4886–4889. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bertelloni, S.; Cinquanta, L.; Baroncelli, G.I.; Simi, P.; Rossi, S.; Saggese, G. Volumetric bone mineral density in young women with Turner’s syndrome treated with estrogens or estrogens plus growth hormone. Horm. Res. 2000, 53, 72–76. [Google Scholar] [CrossRef]
- Nour, M.A.; Burt, L.A.; Perry, R.J.; Stephure, D.K.; Hanley, D.A.; Boyd, S.K. Impact of Growth Hormone on Adult Bone Quality in Turner Syndrome: A HR-pQCT Study. Calcif. Tissue Int. 2016, 98, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Barake, M.; Arabi, A.; Nakhoul, N.; El-Hajj Fuleihan, G.; El Ghandour, S.; Klibanski, A.; Tritos, N.A. Effects of growth hormone therapy on bone density and fracture risk in age-related osteoporosis in the absence of growth hormone deficiency: A systematic review and meta-analysis. Endocrine 2018, 59, 39–49. [Google Scholar] [CrossRef]
- Benetti-Pinto, C.L.; Bedone, A.; Magna, L.A.; Marques-Neto, J.F. Factors associated with the reduction of bone density in patients with gonadal dysgenesis. Fertil. Steril. 2002, 77, 571–575. [Google Scholar] [CrossRef]
- Silva, B.C.; Broy, S.B.; Boutroy, S.; Schousboe, J.T.; Shepherd, J.A.; Leslie, W.D. Fracture Risk Prediction by Non-BMD DXA Measures: The 2015 ISCD Official Positions Part 2: Trabecular Bone Score. J. Clin. Densitom. 2015, 18, 309–330. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Tsuburai, T.; Tokinaga, A.; Nakajima, I.; Kitayama, R.; Imai, Y.; Nagata, T.; Yoshida, H.; Hirahara, F.; Sakakibara, H. Efficacy of estrogen replacement therapy (ERT) on uterine growth and acquisition of bone mass in patients with Turner syndrome. Endocr. J. 2015, 62, 965–970. [Google Scholar] [CrossRef]
- Hernandez, C.J.; Beaupre, G.S.; Carter, D.R. A theoretical analysis of the relative influences of peak BMD, age-related bone loss and menopause on the development of osteoporosis. Osteoporos. Int. 2003, 14, 843–847. [Google Scholar] [CrossRef]
- Rizzoli, R.; Bianchi, M.L.; Garabedian, M.; McKay, H.A.; Moreno, L.A. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone 2010, 46, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Weaver, C.M.; Gordon, C.M.; Janz, K.F.; Kalkwarf, H.J.; Lappe, J.M.; Lewis, R.; O’Karma, M.; Wallace, T.C.; Zemel, B.S. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: A systematic review and implementation recommendations. Osteoporos. Int. 2016, 27, 1281–1386. [Google Scholar] [CrossRef]
- Berger, C.; Goltzman, D.; Langsetmo, L.; Joseph, L.; Jackson, S.; Kreiger, N.; Tenenhouse, A.; Davison, K.S.; Josse, R.G.; Prior, J.C.; et al. Peak bone mass from longitudinal data: Implications for the prevalence, pathophysiology, and diagnosis of osteoporosis. J. Bone Miner. Res. 2010, 25, 1948–1957. [Google Scholar] [CrossRef]
- Klein, K.O.; Baron, J.; Colli, M.J.; McDonnell, D.P.; Cutler, G.B., Jr. Estrogen levels in childhood determined by an ultrasensitive recombinant cell bioassay. J. Clin. Investig. 1994, 94, 2475–2480. [Google Scholar] [CrossRef] [PubMed]
- Paris, F.; Servant, N.; Terouanne, B.; Balaguer, P.; Nicolas, J.C.; Sultan, C. A new recombinant cell bioassay for ultrasensitive determination of serum estrogenic bioactivity in children. J. Clin. Endocrinol. Metab. 2002, 87, 791–797. [Google Scholar] [CrossRef]
- Frederiksen, H.; Johannsen, T.H.; Andersen, S.E.; Albrethsen, J.; Landersoe, S.K.; Petersen, J.H.; Andersen, A.N.; Vestergaard, E.T.; Schorring, M.E.; Linneberg, A.; et al. Sex-specific Estrogen Levels and Reference Intervals from Infancy to Late Adulthood Determined by LC-MS/MS. J. Clin. Endocrinol. Metab. 2020, 105, 754–768. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Ariyasu, D.; Izawa, M.; Igaki-Miyamoto, J.; Fukuma, M.; Hatano, M.; Yagi, H.; Goto, M. Gradually increasing ethinyl estradiol for Turner syndrome may produce good final height but not ideal BMD. Endocr. J. 2017, 64, 221–227. [Google Scholar] [CrossRef]
- Reid, I.R. A broader strategy for osteoporosis interventions. Nat. Rev. Endocrinol. 2020, 16, 333–339. [Google Scholar] [CrossRef]
- Estell, E.G.; Rosen, C.J. Emerging insights into the comparative effectiveness of anabolic therapies for osteoporosis. Nat. Rev. Endocrinol. 2021, 17, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Kawai, M.; Modder, U.I.; Khosla, S.; Rosen, C.J. Emerging therapeutic opportunities for skeletal restoration. Nat. Rev. Drug Discov. 2011, 10, 141–156. [Google Scholar] [CrossRef] [PubMed]
- Chiarito, M.; Piacente, L.; Chaoul, N.; Pontrelli, P.; D’Amato, G.; Grandone, A.; Russo, G.; Street, M.E.; Wasniewska, M.G.; Brunetti, G.; et al. Role of Wnt-signaling inhibitors DKK-1 and sclerostin in bone fragility associated with Turner syndrome. J. Endocrinol. Investig. 2022, 45, 1255–1263. [Google Scholar] [CrossRef]
- Valdes, A.; Bajaj, T. Estrogen Therapy. In Treasure Island; StatPearls: Tampa, FL, USA, 2022. [Google Scholar]
| Author | Year | Age (Years) # | Bone Mineral Density | Bone Geometry | ||||
|---|---|---|---|---|---|---|---|---|
| Number | Methods | Trabecular Bone ## | Cortical Bone ## | |||||
| Prepubertal | ||||||||
| Ross et al. [19] | 1991 | 4–13 | 78 | DPA DXA | Lower LS aBMD by DPA, but the difference disappeared after adjustments for bone age or height age | Lower aBMD of the wrist after adjustments for chronological age, bone age, or BMI by SPA | na | |
| Nanao et al. [22] | 2002 | 4–6.9 | 5 | QCT | Similar LS vBMD to age-matched controls | na | na | |
| 7–9.9 | 8 | |||||||
| 10–12.9 | 15 | Lower LS vBMD than age-matched controls | ||||||
| Högler et al. [20] | 2004 | 10.46 ± 3.25 | 51 | DXA | LS vBMD Z score higher than −1.5 in 44 out of 51 | FN vBMD Z-score higher than −1.5 in 38 out of 51 | na | |
| <10 * | 21 | LS vBMD Z score higher than −1.5 in all subjects | FN vBMD Z-score higher than −1.5 in 16 out of 21 | |||||
| Soucek et al. [21] | 2011 | 10.3 ± 2.2 | 22 | pQCT | Similar vBMD of the radius to age-matched controls | Lower vBMD of the radius than age-matched controls | Higher radial CSA than age-matched controls after adjustments for height. Lower cortical thickness than age- matched controls | |
| <10 * | 8 | Normal vBMD of the radius in all subjects | Lower vBMD of the radius than the lower limit of the age-matched reference in 3 out of 10 | CSA above the lower limit in all subjects. Cortical thickness: the lower half of the normal range in 6, lower than the lower limit in 1 | ||||
| Pitukcheewanont et al. [26] | 2011 | 11.9 ± 3.3 | 22 | DXA pQCT | Similar LS vBMD to age-matched controls after adjustments for weight, height, skeletal age, and pubertal stage | Similar femoral vBMD with age-matched controls after adjustments for weight, height, skeletal age, and pubertal stage | Similar cortical bone CSA to age-matched controls after adjustments for weight, height, skeletal age, and pubertal stage | |
| Prepubertal/Pubertal | ||||||||
| Shaw et al. [27] | 1997 | 4–17 | 18 | DXA | Lower LS aBMD than the age-matched controls, but the difference disappeared after adjustments for body weight and pubertal status | na | na | |
| Holroyd et al. [28] | 2010 | 12.7 ± 3.8 7–19 | 22 | DXA pQCT | Similar LS BMAD and radial vBMD Z-scores as the age- and Tanner-stage-matched controls | Lower FN BMAD and radial vBMD Z-scores than the age- and Tanner-stage-matched controls | A similar radial cortical thickness Z-score as the age- and Tanner-stage-matched controls | |
| Soucek et al. [24] | 2018 | 10.0 ± 2.2 13.5 ± 1.5 16.1 ± 0.4 | 15 14 3 | pQCT | Normal height-specific z-score of the radius vBMD during the prepubertal period. Age-dependent decrease in the radial vBMD Z-score thereafter | Normal vBMD during prepubertal ages, followed by a decrease during peripubertal ages. Thereafter, an increase was observed during pubertal initiation/induction | Comparable height-specific CSA during prepubertal period. The height-specific CSA Z-score showed an age- dependent increase | |
| Pubertal | ||||||||
| Högler et al. [20] | 2004 | 13.89 ± 2.23 | 16 | DXA | Age-dependent decrease during the pre- and peripubertal, and pubertal periods | The FN vBMD Z-score is constant during the pre- and peripubertal, and pubertal periods | na | |
| 18.98 ± 2.40 | 16 | |||||||
| Soucek et al. [21] | 2011 | 14.3 ± 1.7 17.4 ± 1.2 | 25 20 | pQCT | Lower radial vBMD Z-score than the reference value | Lower radial vBMD Z-score than the reference value | Similar height-adjusted CSA as the reference value | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawai, M.; Hasegawa, Y. Skeletal Characteristics of Children and Adolescents with Turner Syndrome. Endocrines 2022, 3, 476-487. https://doi.org/10.3390/endocrines3030038
Kawai M, Hasegawa Y. Skeletal Characteristics of Children and Adolescents with Turner Syndrome. Endocrines. 2022; 3(3):476-487. https://doi.org/10.3390/endocrines3030038
Chicago/Turabian StyleKawai, Masanobu, and Yukihiro Hasegawa. 2022. "Skeletal Characteristics of Children and Adolescents with Turner Syndrome" Endocrines 3, no. 3: 476-487. https://doi.org/10.3390/endocrines3030038
APA StyleKawai, M., & Hasegawa, Y. (2022). Skeletal Characteristics of Children and Adolescents with Turner Syndrome. Endocrines, 3(3), 476-487. https://doi.org/10.3390/endocrines3030038







