Liver and Kidney Transplantation in Elderly Patients
Abstract
1. Introduction
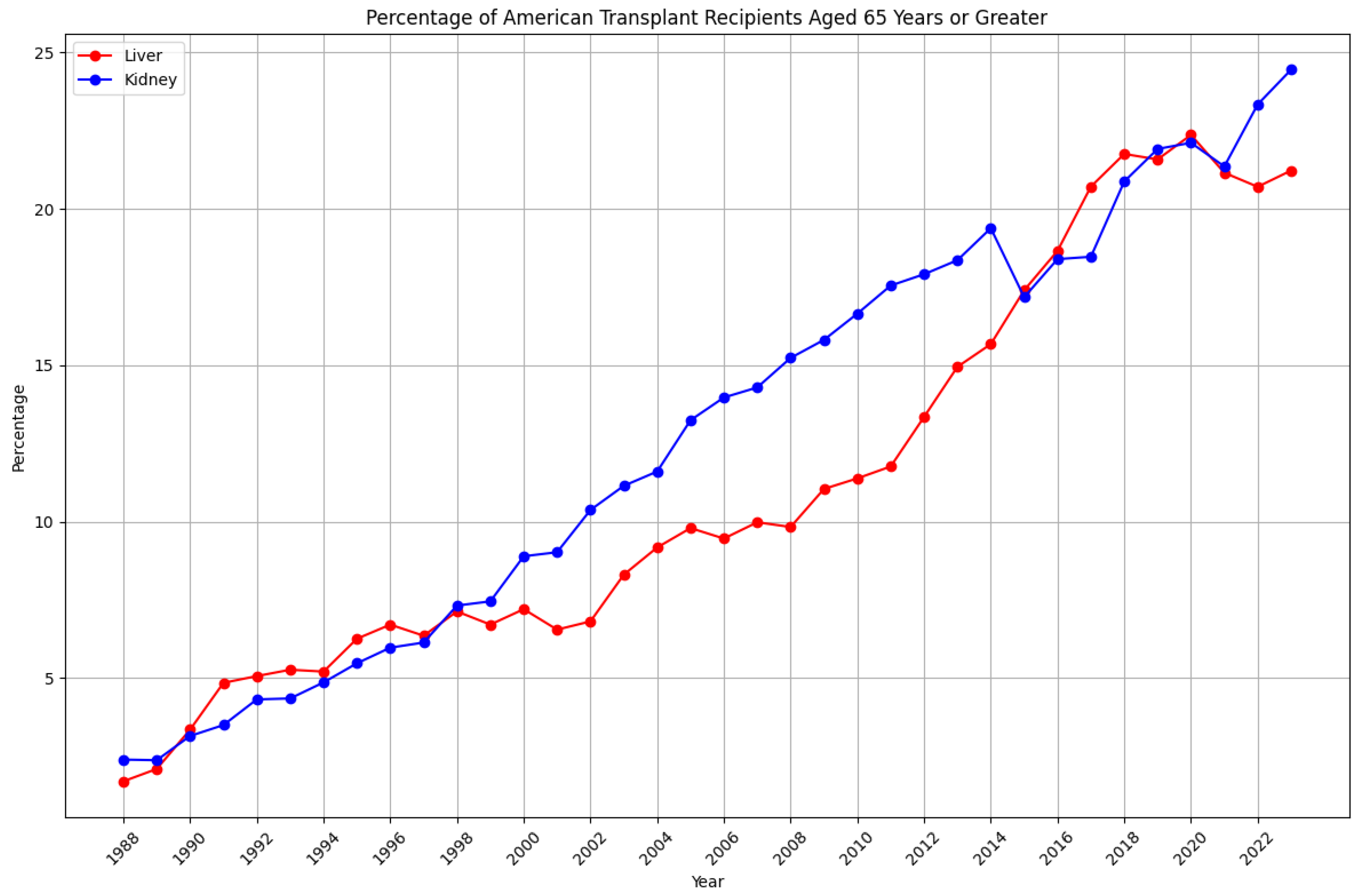
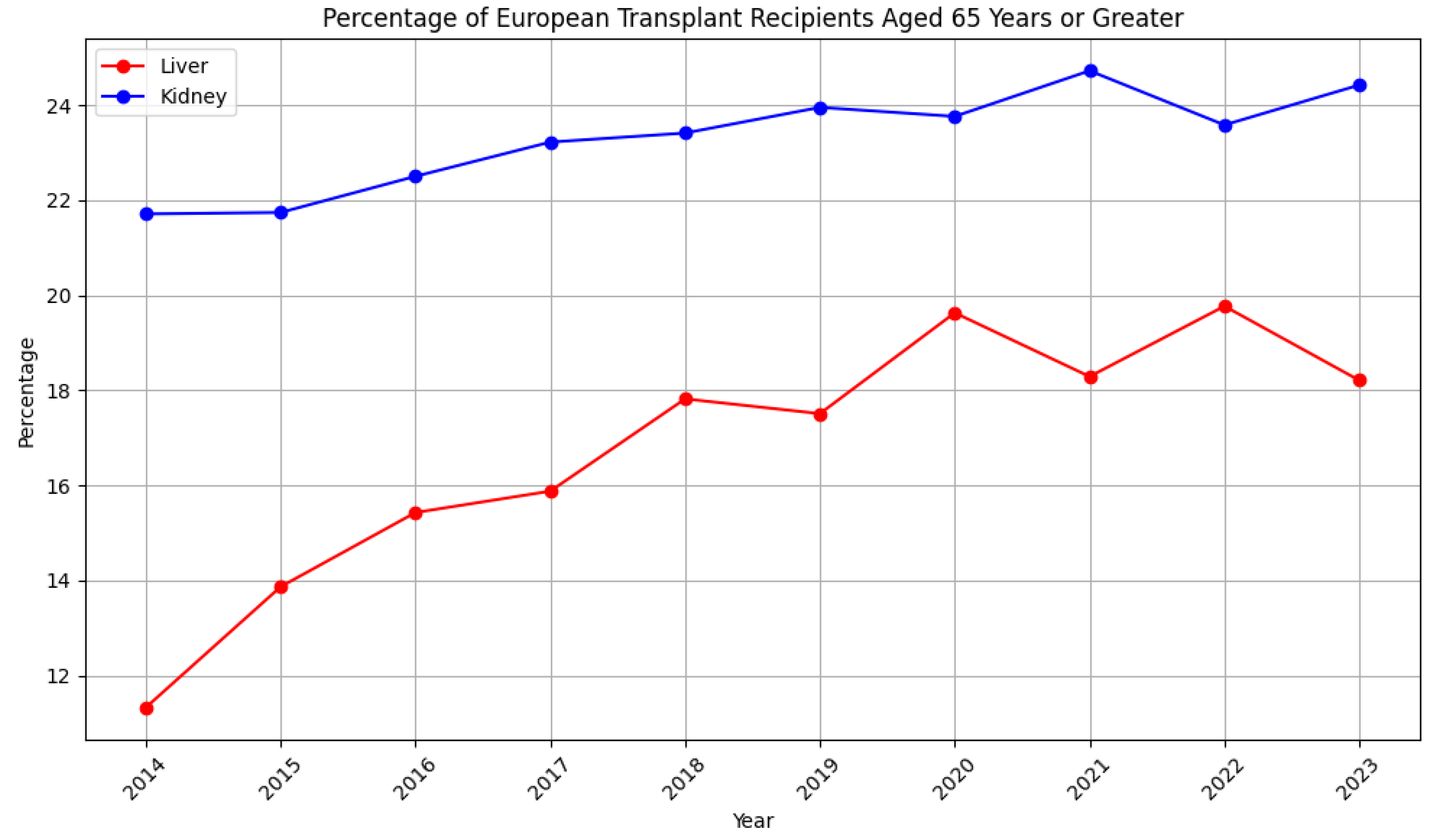
2. Transplants in the Elderly: A Growing Trend
3. Age Matters: The Implications of Aging in Transplant Recipients
4. Evaluating an Elderly Transplant Candidate: Preoperative Considerations
5. Post-Operative Outcomes and Considerations
6. An Ongoing Debate: Upper Age Limits for Transplantation
7. The Ethical Implications of Transplantation in the Elderly
8. Preparing for Life after Transplantation
9. Future Directions
10. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- 2020 Census. 2020. Available online: https://www.census.gov (accessed on 15 November 2023).
- Vespa, J.; Armstrong, D.M.; Medina, L.; Bureau, U.S.C. Demographic Turning Points for the United States: Population Projections for 2020 to 2060; US Department of Commerce, Economics and Statistics Administration: Washington, DC, USA, 2018.
- Danovitch, G.; Savransky, E. Challenges in the counseling and management of older kidney transplant candidates. Am. J. Kidney Dis. 2006, 47 (Suppl. S2), S86–S97. [Google Scholar] [CrossRef] [PubMed]
- Michon, L.; Hamburger, J.; Oeconomos, N.; Delinotte, P.; Richet, G.; Vaysse, J.; Antoine, B. An attempted kidney transplantation in man: Medical and biological aspects. Presse Med. 1953, 61, 1419–1423. [Google Scholar]
- Starzl, T.E.; Brettschneider, L.; Groth, C.G. Liver transplantation. Bull. Soc. Int. Chir. 1967, 26, 474–488. [Google Scholar] [PubMed]
- Falade-Nwulia, O.; Suarez-Cuervo, C.; Nelson, D.R.; Fried, M.W.; Segal, J.B.; Sulkowski, M.S. Oral Direct-Acting Agent Therapy for Hepatitis C Virus Infection: A Systematic Review. Ann. Intern. Med. 2017, 166, 637–648. [Google Scholar] [CrossRef] [PubMed]
- Perricone, G.; Duvoux, C.; Berenguer, M.; Cortesi, P.A.; Vinaixa, C.; Facchetti, R.; Mazzarelli, C.; Rockenschaub, S.R.; Martini, S.; Morelli, C.; et al. Delisting HCV-infected liver transplant candidates who improved after viral eradication: Outcome 2 years after delisting. Liver Int. 2018, 38, 2170–2177. [Google Scholar] [CrossRef] [PubMed]
- US Renal Disease Systems. 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2020.
- McCullough, K.P.; Morgenstern, H.; Saran, R.; Herman, W.H.; Robinson, B.M. Projecting ESRD Incidence and Prevalence in the United States through 2030. J. Am. Soc. Nephrol. 2019, 30, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.D. Matplotlib: A 2D Graphics Environment. Comput. Sci. Eng. 2007, 9, 90–95. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Garonzik-Wang, J.M.; Govindan, P.; Grinnan, J.W.; Liu, M.; Ali, H.M.; Chakraborty, A.; Jain, V.; Ros, R.L.; James, N.T.; Kucirka, L.M.; et al. Frailty and delayed graft function in kidney transplant recipients. Arch. Surg. 2012, 147, 190–193. [Google Scholar] [CrossRef]
- Schaenman, J.; Castellon, L.; Liang, E.C.; Nanayakkara, D.; Abdalla, B.; Sarkisian, C.; Goldwater, D. The Frailty Risk Score predicts length of stay and need for rehospitalization after kidney transplantation in a retrospective cohort: A pilot study. Pilot Feasibility Stud. 2019, 5, 144. [Google Scholar] [CrossRef]
- McAdams-DeMarco, M.A.; Law, A.; Salter, M.L.; Chow, E.; Grams, M.; Walston, J.; Segev, D.L. Frailty and early hospital readmission after kidney transplantation. Am. J. Transplant. 2013, 13, 2091–2095. [Google Scholar] [CrossRef] [PubMed]
- McAdams-DeMarco, M.A.; Law, A.; King, E.; Orandi, B.; Salter, M.; Gupta, N.; Chow, E.; Alachkar, N.; Desai, N.; Varadhan, R.; et al. Frailty and mortality in kidney transplant recipients. Am. J. Transplant. 2015, 15, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, M.; Poltavskiy, E.; Dodge, J.L.; Lai, J.C. Frailty is independently associated with increased hospitalisation days in patients on the liver transplant waitlist. World J. Gastroenterol. 2017, 23, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Durand, F.; Levitsky, J.; Cauchy, F.; Gilgenkrantz, H.; Soubrane, O.; Francoz, C. Age and liver transplantation. J. Hepatol. 2019, 70, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Fozouni, L.; Lai, J.C. Frailty as an Immune-Mediated Condition That Leads to an Increased Risk of Acute Cellular Rejection in Liver Transplant Recipients. Clin. Liver Dis. 2020, 15, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Buta, B.; Zheng, S.; Langdon, J.; Adeosun, B.; Bandeen-Roche, K.; Walston, J.; Xue, Q.L. Agreement between standard and self-reported assessments of physical frailty syndrome and its components in a registry of community-dwelling older adults. BMC Geriatr. 2022, 22, 705. [Google Scholar] [CrossRef] [PubMed]
- Gelson, W.; Hoare, M.; Vowler, S.; Shankar, A.; Gibbs, P.; Akbar, A.N.; Alexander, G.J. Features of immune senescence in liver transplant recipients with established grafts. Liver Transpl. 2010, 16, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Cawthon, R.M.; Smith, K.R.; O’Brien, E.; Sivatchenko, A.; Kerber, R.A. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet 2003, 361, 393–395. [Google Scholar] [CrossRef]
- Nanmoku, K.; Matsuda, Y.; Yamamoto, T.; Tsujita, M.; Hiramitsu, T.; Goto, N.; Katayama, A.; Watarai, Y.; Kobayashi, T.; Uchida, K. Clinical characteristics and outcomes of renal transplantation in elderly recipients. Transplant. Proc. 2012, 44, 281–283. [Google Scholar] [CrossRef]
- Ponticelli, C.; Podesta, M.A.; Graziani, G. Renal transplantation in elderly patients. How to select the candidates to the waiting list? Transplant. Rev. 2014, 28, 188–192. [Google Scholar] [CrossRef]
- Mousa, O.Y.; Nguyen, J.H.; Ma, Y.; Rawal, B.; Musto, K.R.; Dougherty, M.K.; Shalev, J.A.; Harnois, D.M. Evolving Role of Liver Transplantation in Elderly Recipients. Liver Transpl. 2019, 25, 1363–1374. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.P.; Tsai, Y.F.; Lin, J.R.; Liu, F.C.; Yu, H.P. Recipient Age and Mortality Risk after Liver Transplantation: A Population-Based Cohort Study. PLoS ONE 2016, 11, e0152324. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.J.; Pappas, L.; Thiesset, H.F.; Vargas, G.; Sorensen, J.B.; Kim, R.D.; Hutson, W.R.; Boucher, K.; Box, T. Liver transplantation in septuagenarians receiving model for end-stage liver disease exception points for hepatocellular carcinoma: The national experience. Liver Transplant. 2012, 18, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Su, F.; Yu, L.; Berry, K.; Liou, I.W.; Landis, C.S.; Rayhill, S.C.; Reyes, J.D.; Ioannou, G.N. Aging of Liver Transplant Registrants and Recipients: Trends and Impact on Waitlist Outcomes, Post-Transplantation Outcomes, and Transplant-Related Survival Benefit. Gastroenterology 2016, 150, 441–453. [Google Scholar] [CrossRef]
- Cross, T.J.S.; Antoniades, C.G.; Muiesan, P.; Al-Chalabi, T.; Aluvihare, V.; Agarwal, K.; Portmann, B.C.; Rela, M.; Heaton, N.D.; O’Grady, J.G.; et al. Liver transplantation in patients over 60 and 65 years: An evaluation of long-term outcomes and survival. Liver Transplant. 2007, 13, 1382–1388. [Google Scholar] [CrossRef]
- Rao, P.S.; Merion, R.M.; Ashby, V.B.; Port, F.K.; Wolfe, R.A.; Kayler, L.K. Renal transplantation in elderly patients older than 70 years of age: Results from the Scientific Registry of Transplant Recipients. Transplantation 2007, 83, 1069–1074. [Google Scholar] [CrossRef]
- Wolfe, R.A.; Ashby, V.B.; Milford, E.L.; Ojo, A.O.; Ettenger, R.E.; Agodoa, L.Y.; Held, P.J.; Port, F.K. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 1999, 341, 1725–1730. [Google Scholar] [CrossRef]
- Heldal, K.; Hartmann, A.; Grootendorst, D.C.; de Jager, D.J.; Leivestad, T.; Foss, A.; Midtvedt, K. Benefit of kidney transplantation beyond 70 years of age. Nephrol. Dial. Transplant. 2010, 25, 1680–1687. [Google Scholar] [CrossRef]
- Sener, A.; Schweitzer, E.J.; Munivenkatappa, R.; Cooper, M.; Bartlett, S.T.; Philosophe, B.; Barth, R.N. Deceased-donor renal transplantation in the geriatric population demonstrates equal graft survival compared with younger recipients. Transplantation 2009, 87, 1549–1554. [Google Scholar] [CrossRef] [PubMed]
- Lønning, K.; Midtvedt, K.; Leivestad, T.; Reisæter, A.V.; Line, P.D.; Hartmann, A.; Heldal, K. Are Octogenarians With End-Stage Renal Disease Candidates for Renal Transplantation? Transplantation 2016, 100, 2705–2709. [Google Scholar] [CrossRef]
- Cottone, C.; Pena Polanco, N.A.; Bhamidimarri, K.R. Transplant of Elderly Patients: Is There an Upper Age Cutoff? Clin. Liver Dis. 2021, 25, 209–227. [Google Scholar] [CrossRef] [PubMed]
- van Loon, I.N.; Goto, N.A.; Boereboom, F.T.J.; Bots, M.L.; Hoogeveen, E.K.; Gamadia, L.; van Bommel, E.F.H.; van de Ven, P.J.G.; Douma, C.E.; Vincent, H.H.; et al. Geriatric Assessment and the Relation with Mortality and Hospitalizations in Older Patients Starting Dialysis. Nephron 2019, 143, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Hudomiet, P.; Hurd, M.D.; Rohwedder, S. Dementia Prevalence in the United States in 2000 and 2012: Estimates Based on a Nationally Representative Study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2018, 73 (Suppl. S1), S10–S19. [Google Scholar] [CrossRef] [PubMed]
- Borson, S.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The mini-cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef] [PubMed]
- Kotin, P.; Hall, E.M. “Cardiac” or congestive cirrhosis of liver. Am. J. Pathol. 1951, 27, 561–571. [Google Scholar] [PubMed]
- Smetana, G.W.; Lawrence, V.A.; Cornell, J.E. Preoperative pulmonary risk stratification for noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann. Intern. Med. 2006, 144, 581–595. [Google Scholar] [CrossRef]
- McAdams-DeMarco, M.A.; Ying, H.; Van Pilsum Rasmussen, S.; Schrack, J.; Haugen, C.E.; Chu, N.M.; González Fernández, M.; Desai, N.; Walston, J.D.; Segev, D.L. Prehabilitation prior to kidney transplantation: Results from a pilot study. Clin. Transplant. 2019, 33, e13450. [Google Scholar] [CrossRef]
- Volk, M.L.; Sonnenday, C. Patient-centered liver transplantation. Clin. Liver Dis. 2016, 8, 24–27. [Google Scholar] [CrossRef]
- Desai, S.; Hong, J.C.; Saab, S. Cardiovascular risk factors following orthotopic liver transplantation: Predisposing factors, incidence and management. Liver Int. 2010, 30, 948–957. [Google Scholar] [CrossRef]
- Anastácio, L.R.; Ferreira, L.G.; Ribeiro Hde, S.; Liboredo, J.C.; Lima, A.S.; Correia, M.I. Metabolic syndrome after liver transplantation: Prevalence and predictive factors. Nutrition 2011, 27, 931–937. [Google Scholar] [CrossRef]
- Laryea, M.; Watt, K.D.; Molinari, M.; Walsh, M.J.; McAlister, V.C.; Marotta, P.J.; Nashan, B.; Peltekian, K.M. Metabolic syndrome in liver transplant recipients: Prevalence and association with major vascular events. Liver Transplant. 2007, 13, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, M.; Titeca Beauport, D.; Lobbedez, T.; Choukroun, G.; Hurault de Ligny, B.; Hazzan, M.; Guerrot, D.; Bertrand, D. Risk Factors for Early Graft Failure and Death After Kidney Transplantation in Recipients Older Than 70 Years. Kidney Int. Rep. 2019, 4, 656–666. [Google Scholar] [CrossRef] [PubMed]
- Lai, X.; Chen, G.; Qiu, J.; Wang, C.; Chen, L. Recipient-related risk factors for graft failure and death in elderly kidney transplant recipients. PLoS ONE 2014, 9, e112938. [Google Scholar] [CrossRef] [PubMed]
- Lehner, L.J.; Staeck, O.; Halleck, F.; Liefeldt, L.; Bamoulid, J.; Budde, K. Need for optimized immunosuppression in elderly kidney transplant recipients. Transplant. Rev. 2015, 29, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Peters-Sengers, H.; Berger, S.P.; Heemskerk, M.B.A.; al Arashi, D.; Homan van der Heide, J.J.; Hemke, A.C.; ten Berge, I.J.M.; Idu, M.M.; Betjes, M.G.H.; van Zuilen, A.D.; et al. Stretching the Limits of Renal Transplantation in Elderly Recipients of Grafts from Elderly Deceased Donors. J. Am. Soc. Nephrol. 2017, 28, 621–631. [Google Scholar] [CrossRef]
- Li, H.Y.; Wei, Y.G.; Yan, L.N.; Li, B. Outcomes Between Elderly and Young Hepatocellular Carcinoma Living Donor Liver Transplantation Recipients: A Single-Center Experience. Medicine 2016, 95, e2499. [Google Scholar] [CrossRef] [PubMed]
- Aduen, J.F.; Sujay, B.; Dickson, R.C.; Heckman, M.G.; Hewitt, W.R.; Stapelfeldt, W.H.; Steers, J.L.; Harnois, D.M.; Kramer, D.J. Outcomes after liver transplant in patients aged 70 years or older compared with those younger than 60 years. Mayo Clin. Proc. 2009, 84, 973–978. [Google Scholar] [CrossRef] [PubMed]
- VanWagner, L.B.; Lapin, B.; Levitsky, J.; Wilkins, J.T.; Abecassis, M.M.; Skaro, A.I.; Lloyd-Jones, D.M. High early cardiovascular mortality after liver transplantation. Liver Transplant. 2014, 20, 1306–1316. [Google Scholar] [CrossRef]
- VanWagner, L.B.; Serper, M.; Kang, R.; Levitsky, J.; Hohmann, S.; Abecassis, M.; Skaro, A.; Lloyd-Jones, D.M. Factors Associated With Major Adverse Cardiovascular Events After Liver Transplantation Among a National Sample. Am. J. Transplant. 2016, 16, 2684–2694. [Google Scholar] [CrossRef]
- Watt, K.D.; Pedersen, R.A.; Kremers, W.K.; Heimbach, J.K.; Charlton, M.R. Evolution of causes and risk factors for mortality post-liver transplant: Results of the NIDDK long-term follow-up study. Am. J. Transplant. 2010, 10, 1420–1427. [Google Scholar] [CrossRef]
- Mohan, B.P.; Iriana, S.; Khan, S.R.; Yarra, P.; Ponnada, S.; Gallegos-Orozco, J.F. Outcomes of liver transplantation in patients 70 years or older: A systematic review and meta-analysis. Ann. Hepatol. 2022, 27, 100741. [Google Scholar] [CrossRef]
- Vitale, A.; Morales, R.R.; Zanus, G.; Farinati, F.; Burra, P.; Angeli, P.; Frigo, A.C.; Del Poggio, P.; Rapaccini, G.; Di Nolfo, M.A.; et al. Barcelona Clinic Liver Cancer staging and transplant survival benefit for patients with hepatocellular carcinoma: A multicentre, cohort study. Lancet Oncol. 2011, 12, 654–662. [Google Scholar] [CrossRef]
- Vitale, A.; Volk, M.L.; De Feo, T.M.; Burra, P.; Frigo, A.C.; Ramirez Morales, R.; De Carlis, L.; Belli, L.; Colledan, M.; Fagiuoli, S.; et al. A method for establishing allocation equity among patients with and without hepatocellular carcinoma on a common liver transplant waiting list. J. Hepatol. 2014, 60, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Schaubel, D.E.; Guidinger, M.K.; Biggins, S.W.; Kalbfleisch, J.D.; Pomfret, E.A.; Sharma, P.; Merion, R.M. Survival benefit-based deceased-donor liver allocation. Am. J. Transplant. 2009, 9 Pt 2, 970–981. [Google Scholar] [CrossRef]
- Sutherland, A.I.; JN, I.J.; Forsythe, J.L.; Dor, F.J. Kidney and liver transplantation in the elderly. Br. J. Surg. 2016, 103, e62–e72. [Google Scholar] [CrossRef] [PubMed]
- Netuveli, G.; Blane, D. Quality of life in older ages. Br. Med. Bull. 2008, 85, 113–126. [Google Scholar] [CrossRef]
- Wang, Y.; Hemmelder, M.H.; Bos, W.J.W.; Snoep, J.D.; de Vries, A.P.J.; Dekker, F.W.; Meuleman, Y. Mapping health-related quality of life after kidney transplantation by group comparisons: A systematic review. Nephrol. Dial. Transplant. 2021, 36, 2327–2339. [Google Scholar] [CrossRef]
- Humar, A.; Denny, R.; Matas, A.J.; Najarian, J.S. Graft and quality of life outcomes in older recipients of a kidney transplant. Exp. Clin. Transplant. 2003, 1, 69–72. [Google Scholar] [PubMed]
- Tsarpali, V.; Midtvedt, K.; Lønning, K.; Bernklev, T.; Lippe, N.V.; Reisæter, A.V.; Brunborg, C.; Heldal, K. Health-Related Quality of Life in Older Kidney Transplant Recipients: A National Cohort Study of Short- and Longer-Term Outcomes. Kidney Med. 2021, 3, 974–983. [Google Scholar] [CrossRef]
- Yang, L.S.; Shan, L.L.; Saxena, A.; Morris, D.L. Liver transplantation: A systematic review of long-term quality of life. Liver Int. 2014, 34, 1298–1313. [Google Scholar] [CrossRef]
- Park, W.Y.; Kim, J.H.; Ko, E.J.; Min, J.-W.; Ban, T.H.; Yoon, H.-E.; Kim, Y.S.; Jin, K.; Yang, C.W.; Han, S.; et al. Impact of Kidney Donor Profile Index Scores on Post-Transplant Clinical Outcomes Between Elderly and Young Recipients, A Multicenter Cohort Study. Sci. Rep. 2020, 10, 7009. [Google Scholar] [CrossRef]
- Yang, F.C.; Chen, H.M.; Huang, C.M.; Hsieh, P.L.; Wang, S.S.; Chen, C.M. The Difficulties and Needs of Organ Transplant Recipients during Postoperative Care at Home: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5798. [Google Scholar] [CrossRef]
- Brustia, R.; Monsel, A.; Skurzak, S.; Schiffer, E.; Carrier, F.M.; Patrono, D.; Kaba, A.; Detry, O.; Malbouisson, L.; Andraus, W.; et al. Guidelines for Perioperative Care for Liver Transplantation: Enhanced Recovery After Surgery (ERAS) Recommendations. Transplantation 2022, 106, 552–561. [Google Scholar] [CrossRef]
- Feizpour, C.A.; Patel, M.S.; Syed, M.A.; Carrasco, A.; Shah, J.; Hanish, S.; Sosa, L.; Fogus, S.; Bennett, S.; Shi, C.; et al. Enhanced recovery in liver transplantation: A value-based approach to complex surgical care. Surgery 2021, 170, 1830–1837. [Google Scholar] [CrossRef] [PubMed]
- Hillingsø, J.G.; Rostved, A.A.; Dengsø, K.E.; Sørensen, C.L.; Frederiksen, H.J.; Krohn, P.S.; Petersen, C.R.; Larsen, P.N.; Fukumori, D.; Burgdorff, S.K.; et al. Enhanced recovery after surgery is feasible and safe in liver transplantation: A cohort study. HPB 2022, 24, 2022–2028. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Zhu, M.; Li, Z.; Zhu, J.; Xiao, F.; Liu, F.; Wang, Y.; Liu, C. Enhanced recovery after surgery protocols in patients undergoing liver transplantation: A retrospective comparative cohort study. Int. J. Surg. 2020, 78, 108–112. [Google Scholar] [CrossRef]
- Lipshutz, G.S.; Hiatt, J.; Ghobrial, R.M.; Farmer, D.G.; Martinez, M.M.; Yersiz, H.; Gornbein, J.; Busuttil, R.W. Outcome of liver transplantation in septuagenarians: A single-center experience. Arch. Surg. 2007, 142, 775–781. [Google Scholar] [CrossRef]
- Ozkul, F.; Erbis, H.; Yilmaz, V.T.; Kocak, H.; Osmanoglu, I.A.; Dinckan, A. Effect of age on the outcome of renal transplantation: A single-center experience. Pak. J. Med. Sci. 2016, 32, 827–830. [Google Scholar] [CrossRef] [PubMed]
- Gheith, O.; Halim, M.A.; Al-Otaibi, T.; El-Sayed, A.; Nair, P.; Mahmoud, T.; Fathy, A.; Hameed, M.A.; Samy, A.; El Serwy, N.; et al. Elderly Kidney Transplant Recipients: Single-Center Experience in the Middle East. Exp. Clin. Transplant. 2019, 17, 135–141. [Google Scholar] [CrossRef]
- Mikolasevic, I.; Racki, S.; Spanjol, J.; Zupan, Z.; Jakopcic, I.; Devcic, B.; Orlic, L. Outcomes following renal transplantation in older renal transplant recipients: A single-center experience and “Croatian senior program”. Int. Urol. Nephrol. 2015, 47, 1415–1422. [Google Scholar] [CrossRef]
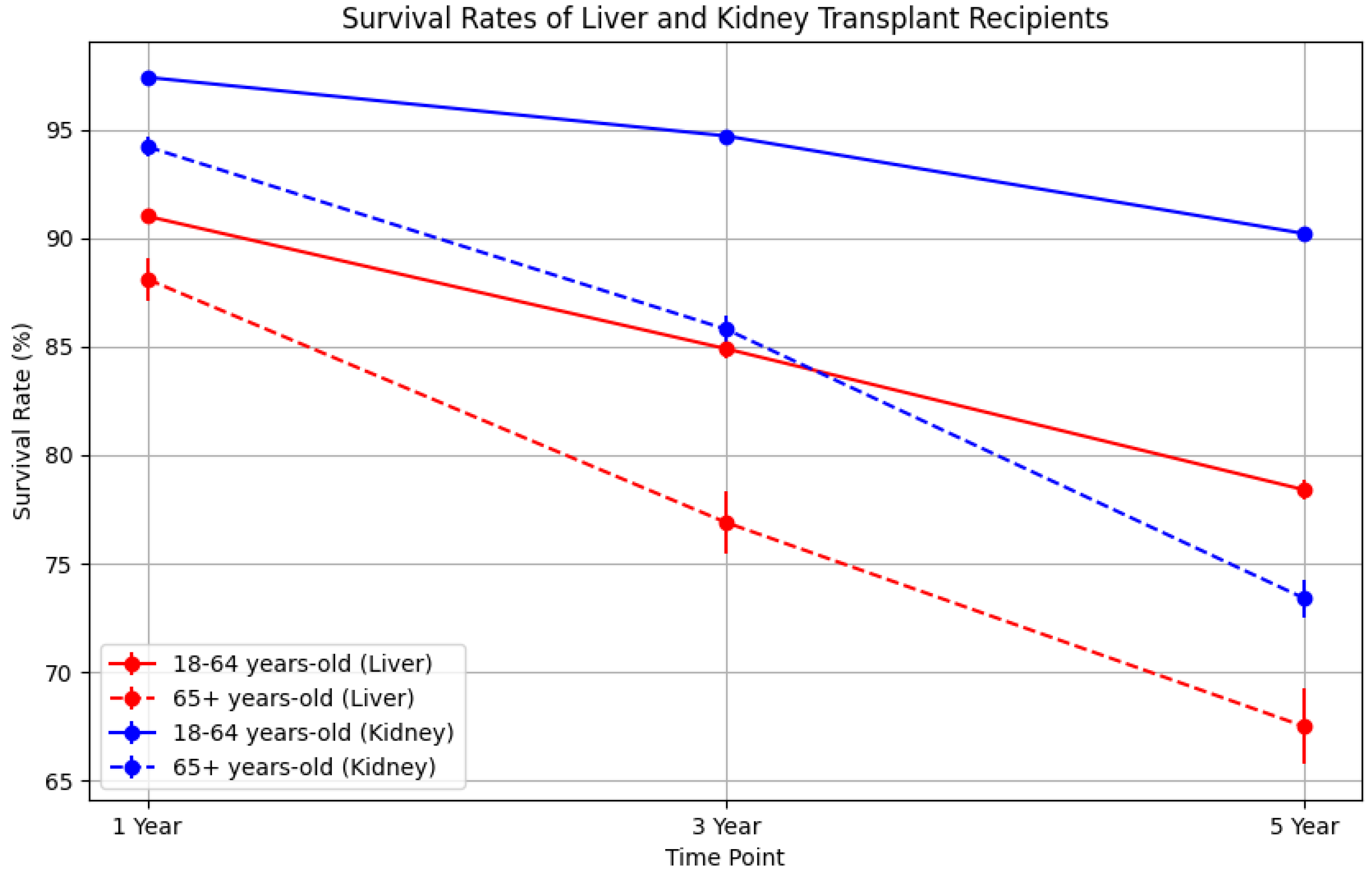
| Age Group | Organ | Time Point | Number of Recipients Alive | Patient Survival Rate (%) | 95% Confidence Interval |
|---|---|---|---|---|---|
| 18–64 | Liver | 1 Year | 17,755 | 91.0 | (90.6, 91.3) |
| 65+ | Liver | 1 Year | 3505 | 88.1 | (87.0, 89.0) |
| 18–64 | Liver | 3 Years | 15,818 | 84.9 | (84.5, 85.4) |
| 65+ | Liver | 3 Years | 2407 | 76.9 | (75.4, 78.3) |
| 18–64 | Liver | 5 Years | 4991 | 78.4 | (78.0, 78.9) |
| 65+ | Liver | 5 Years | 1779 | 67.5 | (65.7, 69.2) |
| 18–64 | Kidney | 1 Year | 51,013 | 97.4 | (97.3, 97.5) |
| 65+ | Kidney | 1 Year | 11,603 | 94.2 | (93.7, 94.6) |
| 18–64 | Kidney | 3 Years | 39,097 | 94.7 | (94.5, 94.9) |
| 65+ | Kidney | 3 Years | 9867 | 85.8 | (85.1, 86.4) |
| 18–64 | Kidney | 5 Years | 32,962 | 90.2 | (90.1, 90.4) |
| 65+ | Kidney | 5 Years | 7675 | 73.4 | (72.6, 74.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzzi, J.; Strand, E.; Ozturk, B.; Agarkov, D.; Deshpande, R. Liver and Kidney Transplantation in Elderly Patients. Transplantology 2024, 5, 98-109. https://doi.org/10.3390/transplantology5020010
Guzzi J, Strand E, Ozturk B, Agarkov D, Deshpande R. Liver and Kidney Transplantation in Elderly Patients. Transplantology. 2024; 5(2):98-109. https://doi.org/10.3390/transplantology5020010
Chicago/Turabian StyleGuzzi, John, Eric Strand, Burhan Ozturk, Daniel Agarkov, and Ranjit Deshpande. 2024. "Liver and Kidney Transplantation in Elderly Patients" Transplantology 5, no. 2: 98-109. https://doi.org/10.3390/transplantology5020010
APA StyleGuzzi, J., Strand, E., Ozturk, B., Agarkov, D., & Deshpande, R. (2024). Liver and Kidney Transplantation in Elderly Patients. Transplantology, 5(2), 98-109. https://doi.org/10.3390/transplantology5020010






