Living Donor Kidney Transplantation for a Recipient after 41 Years of Hemodialysis
Abstract
:1. Introduction
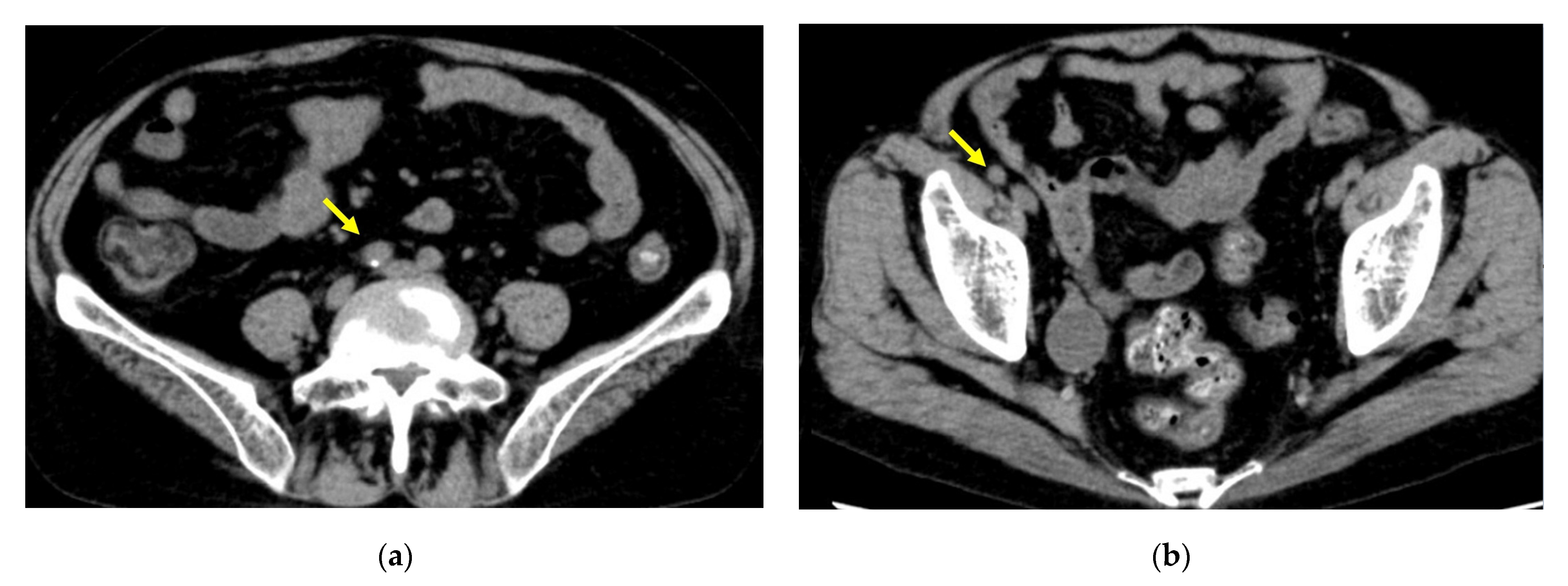
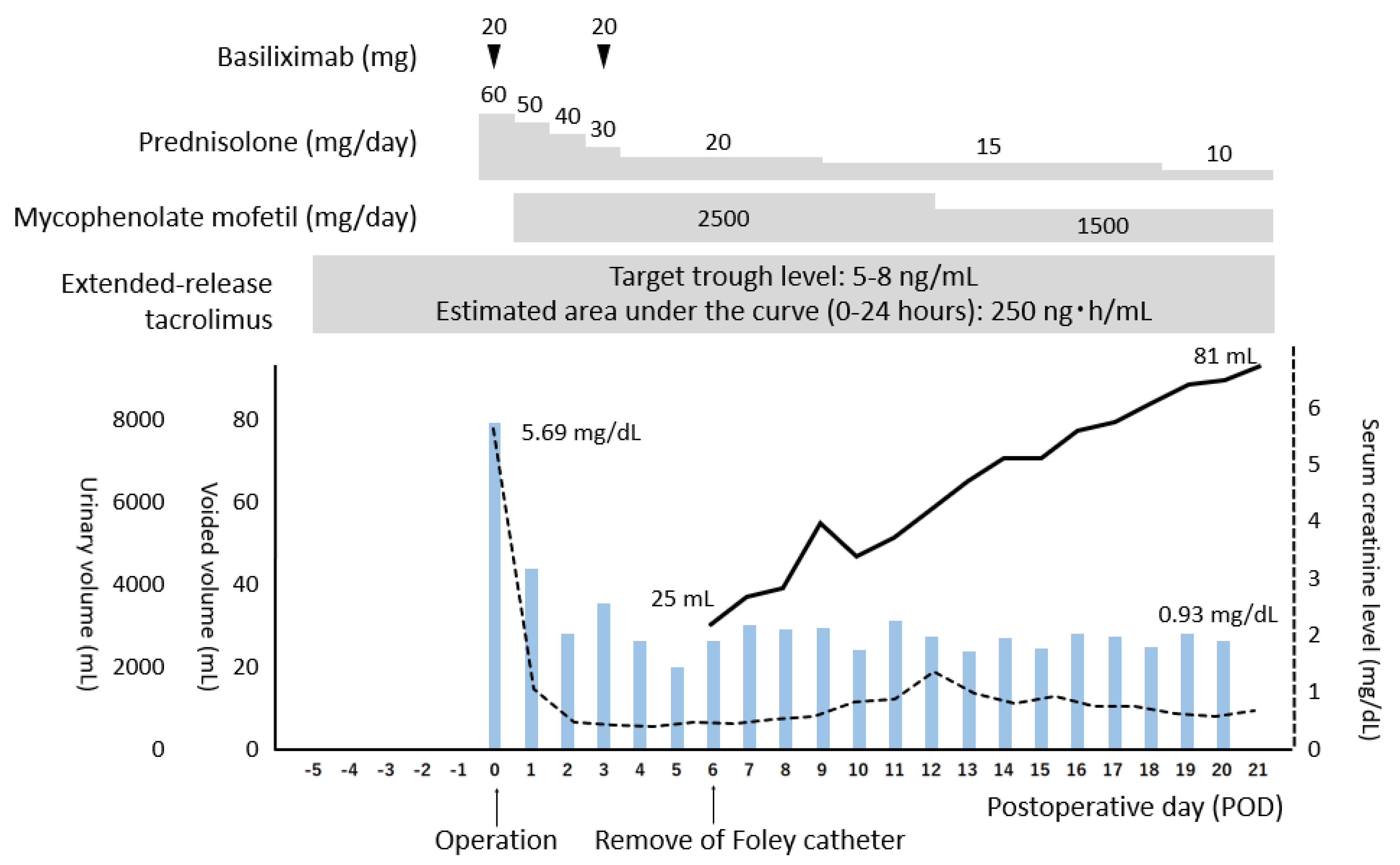
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hart, A.; Smith, J.M.; Skeans, M.A.; Gustafson, S.K.; Wilk, A.R.; Castro, S.; Foutz, J.; Wainright, J.L.; Snyder, J.J.; Kasiske, B.L.; et al. OPTN/SRTR 2018 Annual Data Report: Kidney. Am. J. Transplant. 2020, 20 (Suppl. S1), 20–130. [Google Scholar] [CrossRef]
- Yagisawa, T.; Mieno, M.; Ichimaru, N.; Morita, K.; Nakamura, M.; Hotta, K.; Kenmochi, T.; Yuzawa, K. Trends of kidney transplantation in Japan in 2018: Data from the kidney transplant registry. Renal Replace. Ther. 2019, 5, 3. [Google Scholar] [CrossRef]
- Chun, J.M.; Jung, G.O.; Park, J.B.; Choi, G.S.; Kwon, C.H.; Joh, J.W.; Lee, S.K.; Kim, S.J. Renal transplantation in patients with a small bladder. Transplant. Proc. 2008, 40, 2333–2335. [Google Scholar] [CrossRef]
- Kimura, T.; Ishikawa, N.; Fujiwara, T.; Sakuma, Y.; Nukui, A.; Yashi, M.; Yagisawa, T. Kidney transplantation in patients with long-term (more than 15 years) prior dialysis therapy. Transplant. Proc. 2012, 44, 75–76. [Google Scholar] [CrossRef] [PubMed]
- Martin, X.; Aboutaieb, R.; Soliman, S.; el Essawy, A.; Dawahra, M.; Lefrancois, N. The use of long-term defunctionalized bladder in renal transplantation: Is it safe? Eur. Urol. 1999, 36, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Masaki, N.; Iwadoh, K.; Kondo, A.; Koyama, I.; Nakajima, I.; Fuchinoue, S. Influence of Long-term Dialysis on the Outcome of Kidney Transplantation: A Single-Center Study. Transplant. Proc. 2017, 49, 959–962. [Google Scholar] [CrossRef]
- Serrano, D.P.; Flechner, S.M.; Modlin, C.S.; Wyner, L.M.; Novick, A.C. Transplantation into the long-term defunctionalized bladder. J. Urol. 1996, 156, 885–888. [Google Scholar] [CrossRef]
- Hotta, K.; Miura, M.; Wada, Y.; Fukuzawa, N.; Iwami, D.; Sasaki, H.; Seki, T.; Harada, H. Atrophic bladder in long-term dialysis patients increases the risk for urological complications after kidney transplantation. Int. J. Urol. 2017, 24, 314–319. [Google Scholar] [CrossRef] [Green Version]
- Inoue, T.; Satoh, S.; Saito, M.; Numakura, K.; Tsuruta, H.; Obara, T.; Narita, S.; Horikawa, Y.; Tsuchiya, N.; Habuchi, T. Correlations between pretransplant dialysis duration, bladder capacity, and prevalence of vesicoureteral reflux to the graft. Transplantation 2011, 92, 311–315. [Google Scholar] [CrossRef]
- Wu, Y.J.; Veale, J.L.; Gritsch, H.A. Urological complications of renal transplant in patients with prolonged anuria. Transplantation 2008, 86, 1196–1198. [Google Scholar] [CrossRef]
- Aufhauser, D.D., Jr.; Peng, A.W.; Murken, D.R.; Concors, S.J.; Abt, P.L.; Sawinski, D.; Bloom, R.D.; Reese, P.P.; Levine, M.H. Impact of prolonged dialysis prior to renal transplantation. Clin. Transplant. 2018, 32, e13260. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Park, J.; Kim, Y.H.; Han, D.J.; Song, S.H.; Choo, M.S.; Hong, B. Bladder capacity in kidney transplant patients with end-stage renal disease. Int. Urol. Nephrol. 2015, 47, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Guler, Y.; Erbin, A.; Ozmerdiven, G. Modified Lich-Gregoir Ureteral Reimplantation for the Treatment of Unilateral Primary Vesicoureteral Reflux in Pediatric Patients: A Comparative Analysis with Medium-Term outcomes. Urol. J. 2020, 18, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Politano, V.A.; Leadbetter, W.F. An Operative Technique for the Correction of Vesicoureteral Reflux. J. Urol. 2017, 197, S94–S100. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, H.; Saito, K.; Yamada, T. Ureteroneocystostomy by means of a modified triangular flap method. J. Urol. 1975, 114, 705–708. [Google Scholar] [CrossRef]
- Gregoir, W. The Surgical Treatment of Congenital Vesico-Ureteral Reflux. Acta Chir. Belg. 1964, 63, 431–439. [Google Scholar]
- Secin, F.P.; Rovegno, A.R.; Marrugat, R.E.; Virasoro, R.; Lautersztein, G.A.; Fernandez, H. Comparing Taguchi and Lich-Gregoir ureterovesical reimplantation techniques for kidney transplants. J. Urol. 2002, 168, 926–930. [Google Scholar] [CrossRef]
- Zargar, M.A.; Shahrokh, H.; Mohammadi Fallah, M.R.; Zargar, H. Comparing Taguchi and anterior Lich-Gregoir ureterovesical reimplantation techniques for kidney transplantation. Transplant. Proc. 2005, 37, 3077–3078. [Google Scholar] [CrossRef]
- Lee, R.S.; Bakthavatsalam, R.; Marsh, C.L.; Kuhr, C.S. Ureteral complications in renal transplantation: A comparison of the Lich-Gregoir versus the Taguchi technique. Transplant. Proc. 2007, 39, 1461–1464. [Google Scholar] [CrossRef]
- Moreno-Alarcón, C.; López-Cubillana, P.; López-González, P.; Prieto-González, A.; Ruiz-Morcillo, J.C.; Olarte-Barragán, E.H.; Pinzón-Navarrete, C.P.; Gutiérrez-Gutiérrez, P.F.; Gómez-Gómez, G. Lich-Gregoir technique and routine use of double J catheter as the best combination to avoid urinary complications in kidney transplantation. Transplant. Proc. 2014, 46, 167–169. [Google Scholar] [CrossRef]
- Okamoto, M.; Suzuki, T.; Nobori, S.; Ushigome, H.; Yoshimura, N. A case of successful kidney transplantation after an extremely long-term maintenance haemodialysis of 38 years. NDT Plus 2009, 2, 398–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, K.; Hidaka, Y.; Yamanaga, S.; Kinoshita, K.; Kaba, A.; Toyoda, M.; Yokomizo, H. Living Donor Kidney Transplantation for a Recipient after 41 Years of Hemodialysis. Transplantology 2022, 3, 1-5. https://doi.org/10.3390/transplantology3010001
Tanaka K, Hidaka Y, Yamanaga S, Kinoshita K, Kaba A, Toyoda M, Yokomizo H. Living Donor Kidney Transplantation for a Recipient after 41 Years of Hemodialysis. Transplantology. 2022; 3(1):1-5. https://doi.org/10.3390/transplantology3010001
Chicago/Turabian StyleTanaka, Kosuke, Yuji Hidaka, Shigeyoshi Yamanaga, Kohei Kinoshita, Akari Kaba, Mariko Toyoda, and Hiroshi Yokomizo. 2022. "Living Donor Kidney Transplantation for a Recipient after 41 Years of Hemodialysis" Transplantology 3, no. 1: 1-5. https://doi.org/10.3390/transplantology3010001
APA StyleTanaka, K., Hidaka, Y., Yamanaga, S., Kinoshita, K., Kaba, A., Toyoda, M., & Yokomizo, H. (2022). Living Donor Kidney Transplantation for a Recipient after 41 Years of Hemodialysis. Transplantology, 3(1), 1-5. https://doi.org/10.3390/transplantology3010001





