Management of Autoimmune Liver Diseases after Liver Transplantation
Abstract
:1. Introduction
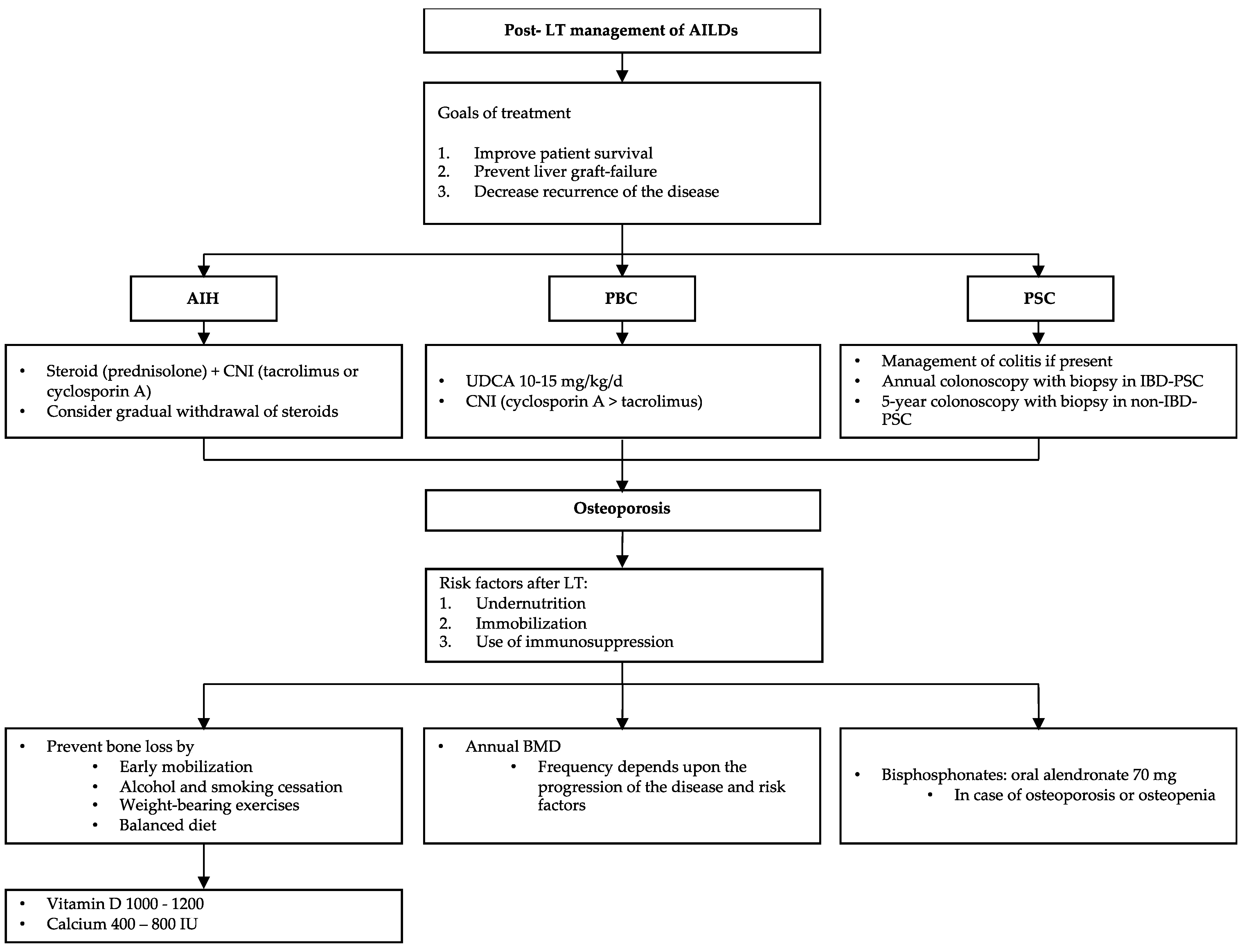
2. Autoimmune Hepatitis
2.1. The Role of Steroids
2.2. Immunosuppression Therapy
3. Primary Biliary Cholangitis
3.1. The Role of Ursodeoxycholic Acid
3.2. Immunosuppression Therapy
4. Primary Sclerosing Cholangitis
4.1. Immunosuppression Therapy
4.2. Role of Colectomy before LT on Post-LT Outcomes
4.3. Colonoscopy Surveillance after Liver Transplantation
5. Bone Maintenance
5.1. Prevention of Osteoporosis
5.2. Early Detection of Osteoporosis
5.3. Treatment of Osteoporosis
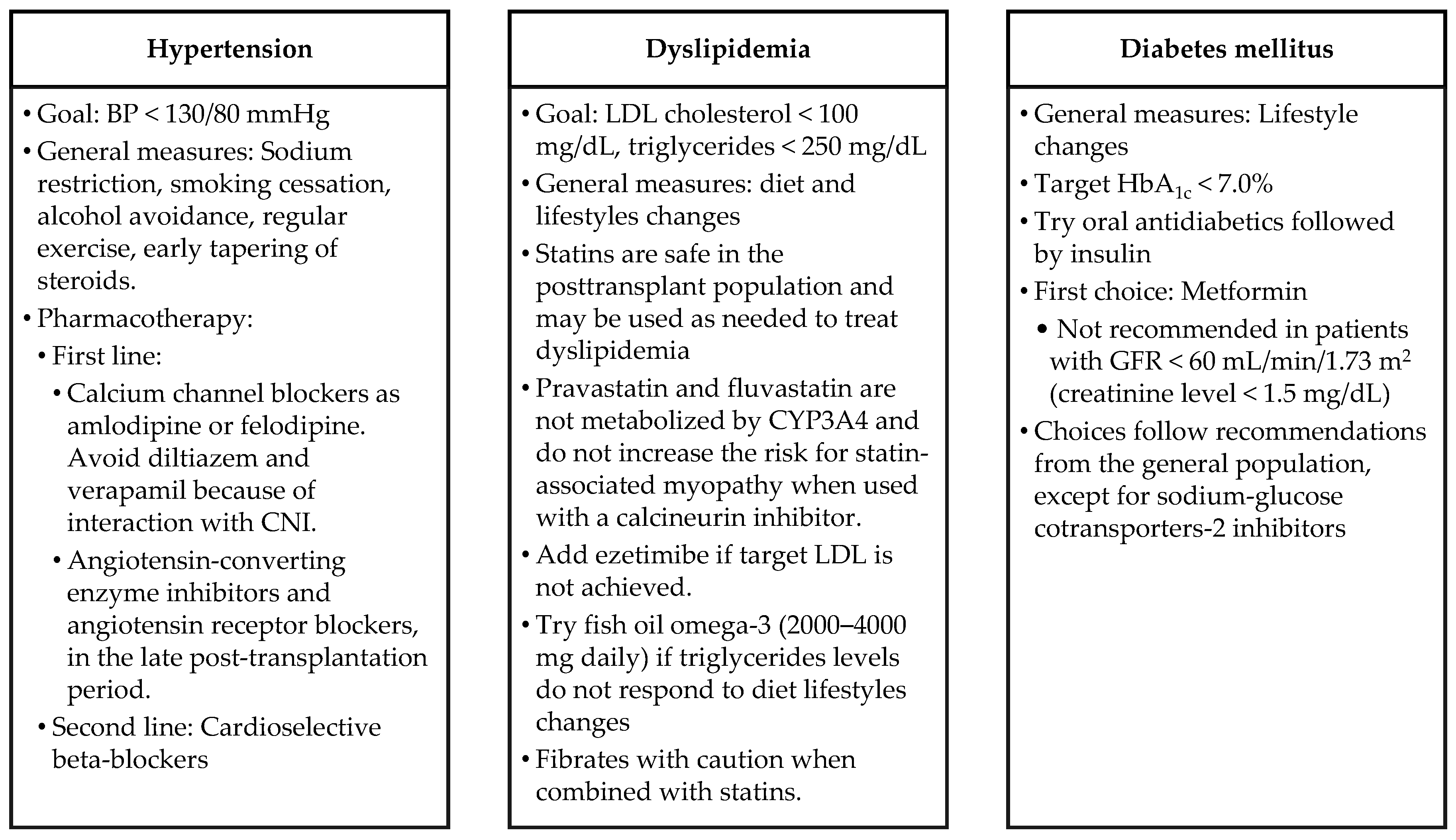
6. Metabolic Syndrome
7. Biopsy in the Diagnosis of Recurrence of AILDs
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Invernizzi, P.; Mackay, I.-R. Autoimmune liver diseases. World J. Gastroenterol. 2008, 14, 3290–3291. [Google Scholar] [CrossRef] [PubMed]
- Montano-Loza, A.J.; Bhanji, R.A.; Wasilenko, S.; Mason, A.L. Systematic review: Recurrent autoimmune liver diseases after liver transplantation. Aliment. Pharmacol. Ther. 2017, 45, 485–500. [Google Scholar] [CrossRef]
- Ilyas, J.A.; O’Mahony, C.A.; Vierling, J.M. Liver transplantation in autoimmune liver diseases. Best Pract. Res. Clin. Gastroenterol. 2011, 25, 765–782. [Google Scholar] [CrossRef] [PubMed]
- Liberal, R.; Zen, Y.; Mieli-Vergani, G.; Vergani, D. Liver transplantation and autoimmune liver diseases. Liver Transpl. 2013, 19, 1065–1077. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Danford, C.J.; Patwardhan, V.R.; Bonder, A. Increased Posttransplant Mortality for Autoimmune Hepatitis Compared with Other Autoimmune Liver Diseases. J. Clin. Gastroenterol. 2020, 54, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Allemant, P.; Ezaz, G.; Trivedi, H.D.; Sanchez-Fernandez, L.; Bonder, A. Long-Term Outcomes after Liver Transplantation in the Hispanic Population. Liver Int. 2020, 40, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.M.; Teo, E.K.; Ng, T.M.; Khor, C.; Fock, K.M. Autoimmune hepatitis in Singapore: A rare syndrome affecting middle-aged women. J. Gastroenterol. Hepatol. 2001, 16, 1384–1389. [Google Scholar] [CrossRef] [PubMed]
- Czaja, A.J. Global Disparities and Their Implications in the Occurrence and Outcome of Autoimmune Hepatitis. Dig. Dis. Sci. 2017, 62, 2277–2292. [Google Scholar] [CrossRef]
- Hurlburt, K.J.; McMahon, B.J.; Deubner, H.; Hsu-Trawinski, B.; Williams, J.L.; Kowdley, K.V. Prevalence of autoimmune liver disease in Alaska Natives. Am. J. Gastroenterol. 2002, 97, 2402–2407. [Google Scholar] [CrossRef]
- Tunio, N.A.; Mansoor, E.; Sheriff, M.Z.; Cooper, G.S.; Sclair, S.N.; Cohen, S.M. Epidemiology of Autoimmune Hepatitis (AIH) in the United States Between 2014 and 2019: A Population-based National Study. J. Clin. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Mack, C.L.; Adams, D.; Assis, D.N.; Kerkar, N.; Manns, M.P.; Mayo, M.J.; Vierling, J.M.; Alsawas, M.; Murad, M.H.; Czaja, A.J. Diagnosis and management of autoimmune hepatitis in adults and children: 2019 practice guidance and guidelines from the American association for the study of liver diseases. Hepatology 2020, 72, 671–722. [Google Scholar] [CrossRef]
- Suri, J.S.; Danford, C.J.; Patwardhan, V.; Bonder, A. Mortality on the UNOS Waitlist for Patients with Autoimmune Liver Disease. J. Clin. Med. Res. 2020, 9, 319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, A. Autoimmune Hepatitis: 2019 Update. Gut Liver 2020, 14, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Stirnimann, G.; Ebadi, M.; Czaja, A.J.; Montano-Loza, A.J. Recurrent and De Novo Autoimmune Hepatitis. Liver Transpl. 2019, 25, 152–166. [Google Scholar] [CrossRef] [Green Version]
- Carbone, M.; Neuberger, J.M. Autoimmune liver disease, autoimmunity and liver transplantation. J. Hepatol. 2014, 60, 210–223. [Google Scholar] [CrossRef] [Green Version]
- Milkiewicz, P.; Hubscher, S.G.; Skiba, G.; Hathaway, M.; Elias, E. Recurrence of autoimmune hepatitis after liver transplantation. Transplantation 1999, 68, 253–256. [Google Scholar] [CrossRef]
- Marudanayagam, R.; Shanmugam, V.; Sandhu, B.; Gunson, B.K.; Mirza, D.F.; Mayer, D.; Buckels, J.; Bramhall, S.R. Liver Retransplantation in Adults: A Single-Centre, 25-Year Experience. HPB 2010, 12, 217–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, H.L.; Bou-Abboud, C.F.; Hassanein, T.; Block, G.D.; Demetris, A.J.; Starzl, T.E.; Van Thiel, D.H. Disease Recurrence and Rejection Following Liver Transplantation for Autoimmune Chronic Active Liver Disease. Transplantation 1992, 53, 136–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prados, E.; Cuervas-Mons, V.; de la Mata, M.; Fraga, E.; Rimola, A.; Prieto, M.; Clemente, G.; Vicente, E.; Casanovas, T.; Fabrega, E. Outcome of Autoimmune Hepatitis after Liver Transplantation. Transplantation 1998, 66, 1645–1650. [Google Scholar] [CrossRef]
- Ratziu, V.; Samuel, D.; Sebagh, M.; Farges, O.; Saliba, F.; Ichai, P.; Farahmand, H.; Gigou, M.; Féray, C.; Reynès, M.; et al. Long-Term Follow-up after Liver Transplantation for Autoimmune Hepatitis: Evidence of Recurrence of Primary Disease. J. Hepatol. 1999, 30, 131–141. [Google Scholar] [CrossRef]
- Reich, D.J.; Fiel, I.; Guarrera, J.V.; Emre, S.; Guy, S.R.; Schwartz, M.E.; Miller, C.M.; Sheiner, P.A. Liver Transplantation for Autoimmune Hepatitis. Hepatology 2000, 32, 693–700. [Google Scholar] [CrossRef]
- Ayata, G.; Gordon, F.D.; Lewis, W.D.; Pomfret, E.; Pomposelli, J.J.; Jenkins, R.L.; Khettry, U. Liver Transplantation for Autoimmune Hepatitis: A Long-Term Pathologic Study. Hepatology 2000, 32, 185–192. [Google Scholar] [CrossRef]
- González-Koch, A.; Czaja, A.J.; Carpenter, H.A.; Roberts, S.K.; Charlton, M.R.; Porayko, M.K.; Rosen, C.B.; Wiesner, R.H. Recurrent autoimmune hepatitis after orthotopic liver transplantation. Liver Transpl. 2001, 7, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Renz, J.F.; Ascher, N.L. Liver transplantation for nonviral, nonmalignant diseases:problem of recurrence. World J. Surg. 2002, 26, 247–256. [Google Scholar] [CrossRef]
- Yusoff, I.F.; House, A.K.; De Boer, W.B.; Ferguson, J.; Garas, G.; Heath, D.; Mitchell, A.; Jeffrey, G. Disease recurrence after liver transplantation in Western Australia. J. Gastroenterol. Hepatol. 2002, 17, 203–207. [Google Scholar] [CrossRef]
- Molmenti, E.P.; Netto, G.J.; Murray, N.G.; Smith, D.M.; Molmenti, H.; Crippin, J.S.; Hoover, T.C.; Jung, G.; Marubashi, S.; Sanchez, E.Q.; et al. Incidence and Recurrence of Autoimmune/alloimmune Hepatitis in Liver Transplant Recipients. Liver Transpl. 2002, 8, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Duclos-Vallée, J.-C.; Sebagh, M.; Rifai, K.; Johanet, C.; Ballot, E.; Guettier, C.; Karam, V.; Hurtova, M.; Feray, C.; Reynes, M.; et al. A 10 Year Follow up Study of Patients Transplanted for Autoimmune Hepatitis: Histological Recurrence Precedes Clinical and Biochemical Recurrence. Gut 2003, 52, 893–897. [Google Scholar] [CrossRef] [Green Version]
- Balan, V.; Ruppert, K.; Demetris, A.J.; Ledneva, T.; Duquesnoy, R.J.; Detre, K.M.; Wei, Y.L.; Rakela, J.; Schafer, D.F.; Roberts, J.P.; et al. Long-Term Outcome of Human Leukocyte Antigen Mismatching in Liver Transplantation: Results of the National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database. Hepatology 2008, 48, 878–888. [Google Scholar] [CrossRef]
- Montano-Loza, A.J.; Mason, A.L.; Ma, M.; Bastiampillai, R.J.; Bain, V.G.; Tandon, P. Risk factors for recurrence of autoimmune hepatitis after liver transplantation. Liver Transpl. 2009, 15, 1254–1261. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, T.L.; Miezynska-Kurtycz, J.; Hodson, J.; Gunson, B.K.; Neuberger, J.; Milkiewicz, P.; Oo, Y.H. Longterm corticosteroid use after liver transplantation for autoimmune hepatitis is safe and associated with a lower incidence of recurrent disease. Liver Transpl. 2016, 22, 34–41. [Google Scholar] [CrossRef] [Green Version]
- Gautam, M.; Cheruvattath, R.; Balan, V. Recurrence of Autoimmune Liver Disease after Liver Transplantation: A Systematic Review. Liver Transpl. 2006, 12, 1813–1824. [Google Scholar] [CrossRef] [PubMed]
- D’Antiga, L. Coronaviruses and immunosuppressed patients: The facts during the third epidemic. Liver Transpl. 2020, 26, 832–834. [Google Scholar] [CrossRef] [PubMed]
- Lladó, L.; Xiol, X.; Figueras, J.; Ramos, E.; Memba, R.; Serrano, T.; Torras, J.; Garcia-Gil, A.; Gonzalez-Pinto, I.; Castellote, J.; et al. Immunosuppression without Steroids in Liver Transplantation Is Safe and Reduces Infection and Metabolic Complications: Results from a Prospective Multicenter Randomized Study. J. Hepatol. 2006, 44, 710–716. [Google Scholar] [CrossRef]
- Vierling, J.M.; Kerkar, N.; Czaja, A.J.; Mack, C.L.; Adams, D.; Assis, D.N.; Manns, M.P.; Mayo, M.J.; Nayfeh, T.; Majzoub, A.M.M.; et al. Immunosuppressive Treatment Regimens in Autoimmune Hepatitis: Systematic Reviews and Meta-Analyses Supporting American Association for the Study of Liver Diseases Guidelines. Hepatology 2020, 72, 753–769. [Google Scholar] [CrossRef] [PubMed]
- Sucher, E.; Sucher, R.; Gradistanac, T.; Brandacher, G.; Schneeberger, S.; Berg, T. Autoimmune Hepatitis-Immunologically Triggered Liver Pathogenesis-Diagnostic and Therapeutic Strategies. J. Immunol. Res. 2019, 2019, 9437043. [Google Scholar] [CrossRef] [PubMed]
- Doycheva, I.; Watt, K.D.; Gulamhusein, A.F. Autoimmune hepatitis: Current and future therapeutic options. Liver Int. 2019, 39, 1002–1013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puustinen, L.; Boyd, S.; Arkkila, P.; Isoniemi, H.; Arola, J.; Färkkilä, M. Histologic surveillance after liver transplantation due to autoimmune hepatitis. Clin. Transplant. 2017, 31. [Google Scholar] [CrossRef]
- de Quadros Onofrio, F.; Neong, E.; Adebayo, D.; Kollmann, D.; Adeyi, O.A.; Fischer, S.; Hirschfield, G.M.; Hansen, B.E.; Bhat, M.; Galvin, Z.; et al. Single-Center North American Experience of Liver Transplantation in Autoimmune Hepatitis: Infrequent Indication but Good Outcomes for Patients. J. Can. Assoc. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Leung, K.K.; Deeb, M.; Hirschfield, G.M. Review article: Pathophysiology and management of primary biliary cholangitis. Aliment. Pharmacol. Ther. 2020, 52, 1150–1164. [Google Scholar]
- Lu, M.; Li, J.; Haller, I.V.; Romanelli, R.J.; VanWormer, J.J.; Rodriguez, C.V.; Raebel, M.A.; Boscarino, J.A.; Schmidt, M.A.; Daida, Y.G.; et al. Factors Associated with Prevalence and Treatment of Primary Biliary Cholangitis in United States Health Systems. Clin. Gastroenterol. Hepatol. 2018, 16, 1333–1341.e6. [Google Scholar] [CrossRef]
- Lleo, A.; Jepsen, P.; Morenghi, E.; Carbone, M.; Moroni, L.; Battezzati, P.M.; Podda, M.; Mackay, I.R.; Eric Gershwin, M.; Invernizzi, P. Evolving Trends in Female to Male Incidence and Male Mortality of Primary Biliary Cholangitis. Sci. Rep. 2016, 6, 25906. [Google Scholar] [CrossRef] [PubMed]
- Onofrio, F.Q.; Hirschfield, G.M.; Gulamhusein, A.F. A Practical Review of Primary Biliary Cholangitis for the Gastroenterologist. Gastroenterol. Hepatol. 2019, 15, 145–154. [Google Scholar]
- Galoosian, A.; Hanlon, C.; Zhang, J.; Holt, E.W.; Yimam, K.K. Clinical Updates in Primary Biliary Cholangitis: Trends, Epidemiology, Diagnostics, and New Therapeutic Approaches. J. Clin. Transl. Hepatol. 2020, 8, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Lindor, K.D.; Bowlus, C.L.; Boyer, J.; Levy, C.; Mayo, M. Primary Biliary Cholangitis: 2018 Practice Guidance from the American Association for the Study of Liver Diseases. Hepatology 2019, 69, 394–419. [Google Scholar]
- Gao, L.; Wang, L.; Woo, E.; He, X.; Yang, G.; Bowlus, C.; Leung, P.S.C.; Gershwin, M.E. Clinical Management of Primary Biliary Cholangitis-Strategies and Evolving Trends. Clin. Rev. Allergy Immunol. 2020, 59, 175–194. [Google Scholar] [CrossRef]
- Aguilar, M.T.; Carey, E.J. Current Status of Liver Transplantation for Primary Biliary Cholangitis. Clin. Liver Dis. 2018, 22, 613–624. [Google Scholar] [CrossRef] [PubMed]
- Martin, P.; Di Martini, A.; Feng, S.; Brown, R., Jr.; Fallon, M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology 2014, 59, 1144–1165. [Google Scholar] [CrossRef]
- Montano-Loza, A.J.; Hansen, B.E.; Corpechot, C.; Roccarina, D.; Thorburn, D.; Trivedi, P.; Hirschfield, G.; McDowell, P.; Poupon, R.; Dumortier, J.; et al. Factors Associated with Recurrence of Primary Biliary Cholangitis After Liver Transplantation and Effects on Graft and Patient Survival. Gastroenterology 2019, 156, 96–107.e1. [Google Scholar] [CrossRef] [Green Version]
- Satapathy, S.K.; Jones, O.D.; Vanatta, J.M.; Kamal, F.; Kedia, S.K.; Jiang, Y.; Nair, S.P.; Eason, J.D. Outcomes of Liver Transplant Recipients with Autoimmune Liver Disease Using Long-Term Dual Immunosuppression Regimen without Corticosteroid. Transpl. Direct 2017, 3, e178. [Google Scholar] [CrossRef]
- Jacob, D.A.; Neumann, U.P.; Bahra, M.; Klupp, J.; Puhl, G.; Neuhaus, R.; Langrehr, J.M. Long-term follow-up after recurrence of primary biliary cirrhosis after liver transplantation in 100 patients. Clin. Transpl. 2006, 20, 211–220. [Google Scholar] [CrossRef]
- Hayashi, M.; Keeffe, E.B.; Krams, S.M.; Martinez, O.M.; Ojogho, O.N.; So, S.K.; Garcia, G.; Imperial, J.C.; Esquivel, C.O. Allograft rejection after liver transplantation for autoimmune liver diseases. Liver Transpl. Surg. 1998, 4, 208–214. [Google Scholar] [CrossRef] [Green Version]
- Levitsky, J.; Goldberg, D.; Smith, A.R.; Mansfield, S.A.; Gillespie, B.W.; Merion, R.M.; Lok, A.S.F.; Levy, G.; Kulik, L.; Abecassis, M.; et al. Acute Rejection Increases Risk of Graft Failure and Death in Recent Liver Transplant Recipients. Clin. Gastroenterol. Hepatol. 2017, 15, 584–593.e2. [Google Scholar] [CrossRef] [Green Version]
- Nevens, F. PBC-transplantation and disease recurrence. Best Pract. Res. Clin. Gastroenterol. 2018, 34–35, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Wong, P.Y.; Portmann, B.; O’Grady, J.G.; Devlin, J.J.; Hegarty, J.E.; Tan, K.C.; Williams, R. Recurrence of primary biliary cirrhosis after liver transplantation following FK506-based immunosuppression. J. Hepatol. 1993, 17, 284–287. [Google Scholar] [CrossRef]
- Dmitrewski, J.; Hubscher, S.G.; Mayer, A.D.; Neuberger, J.M. Recurrence of primary biliary cirrhosis in the liver allograft: The effect of immunosuppression. J. Hepatol. 1996, 24, 253–257. [Google Scholar] [CrossRef]
- Liermann Garcia, R.F.; Evangelista Garcia, C.; McMaster, P.; Neuberger, J. Transplantation for primary biliary cirrhosis: Retrospective analysis of 400 patients in a single center. Hepatology 2001, 33, 22–27. [Google Scholar] [CrossRef]
- Hashimoto, E.; Shimada, M.; Noguchi, S.; Taniai, M.; Tokushige, K.; Hayashi, N.; Takasaki, K.; Fuchinoue, S.; Ludwig, J. Disease recurrence after living liver transplantation for primary biliary cirrhosis: A clinical and histological follow-up study. Liver Transpl. 2001, 7, 588–595. [Google Scholar] [CrossRef]
- Khettry, U.; Anand, N.; Faul, P.N.; Lewis, W.D.; Pomfret, E.A.; Pomposelli, J.; Jenkins, R.L.; Gordon, F.D. Liver transplantation for primary biliary cirrhosis: A long-term pathologic study. Liver Transpl. 2003, 9, 87–96. [Google Scholar] [CrossRef]
- Levitsky, J.; Hart, J.; Cohen, S.M.; Te, H.S. The effect of immunosuppressive regimens on the recurrence of primary biliary cirrhosis after liver transplantation. Liver Transpl. 2003, 9, 733–736. [Google Scholar] [CrossRef]
- Sylvestre, P.B.; Batts, K.P.; Burgart, L.J.; Poterucha, J.J.; Wiesner, R.H. Recurrence of primary biliary cirrhosis after liver transplantation: Histologic estimate of incidence and natural history. Liver Transpl. 2003, 9, 1086–1093. [Google Scholar] [CrossRef]
- Sanchez, E.Q.; Levy, M.F.; Goldstein, R.M.; Fasola, C.G.; Tillery, G.W.; Netto, G.J.; Watkins, D.L.; Weinstein, J.S.; Murray, N.G.; Byers, D.; et al. The Changing Clinical Presentation of Recurrent Primary Biliary Cirrhosis after Liver Transplantation. Transplantation 2003, 76, 1583–1588. [Google Scholar] [CrossRef]
- Neuberger, J.; Gunson, B.; Hubscher, S.; Nightingale, P. Immunosuppression affects the rate of recurrent primary biliary cirrhosis after liver transplantation. Liver Transpl. 2004, 10, 488–491. [Google Scholar] [CrossRef]
- Guy, J.E.; Qian, P.; Lowell, J.A.; Peters, M.G. Recurrent primary biliary cirrhosis: Peritransplant factors and ursodeoxycholic acid treatment post-liver transplant. Liver Transpl. 2005, 11, 1252–1257. [Google Scholar] [CrossRef] [Green Version]
- Morioka, D.; Egawa, H.; Kasahara, M.; Jo, T.; Sakamoto, S.; Ogura, Y.; Haga, H.; Takada, Y.; Shimada, H.; Tanaka, K. Impact of Human Leukocyte Antigen Mismatching on Outcomes of Living Donor Liver Transplantation for Primary Biliary Cirrhosis. Liver Transpl. 2007, 13, 80–90. [Google Scholar] [CrossRef]
- Charatcharoenwitthaya, P.; Pimentel, S.; Talwalkar, J.A.; Enders, F.T.; Lindor, K.D.; Krom, R.A.F.; Wiesner, R.H. Long-term survival and impact of ursodeoxycholic acid treatment for recurrent primary biliary cirrhosis after liver transplantation. Liver Transpl. 2007, 13, 1236–1245. [Google Scholar] [CrossRef]
- Montano-Loza, A.J.; Wasilenko, S.; Bintner, J.; Mason, A.L. Cyclosporine A protects against primary biliary cirrhosis recurrence after liver transplantation. Am. J. Transpl. 2010, 10, 852–858. [Google Scholar] [CrossRef]
- Bosch, A.; Dumortier, J.; Maucort-Boulch, D.; Scoazec, J.-Y.; Wendum, D.; Conti, F.; Morard, I.; Rubbia-Brandt, L.; Terris, B.; Radenne, S.; et al. Preventive Administration of UDCA after Liver Transplantation for Primary Biliary Cirrhosis Is Associated with a Lower Risk of Disease Recurrence. J. Hepatol. 2015, 63, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Egawa, H.; Sakisaka, S.; Teramukai, S.; Sakabayashi, S.; Yamamoto, M.; Umeshita, K.; Uemoto, S. Long-Term Outcomes of Living-Donor Liver Transplantation for Primary Biliary Cirrhosis: A Japanese Multicenter Study. Am. J. Transpl. 2016, 16, 1248–1257. [Google Scholar] [CrossRef] [Green Version]
- Kogiso, T.; Egawa, H.; Teramukai, S.; Taniai, M.; Hashimoto, E.; Tokushige, K.; Sakisaka, S.; Sakabayashi, S.; Yamamoto, M.; Umeshita, K.; et al. Risk Factors for Recurrence of Primary Biliary Cholangitis after Liver Transplantation in Female Patients: A Japanese Multicenter Retrospective Study. Hepatol. Commun. 2017, 1, 394–405. [Google Scholar] [CrossRef] [PubMed]
- Corpechot, C.; Chazouillères, O.; Belnou, P.; Montano-Loza, A.J.; Mason, A.; Ebadi, M.; Eurich, D.; Chopra, S.; Jacob, D.; Schramm, C.; et al. Long-Term Impact of Preventive UDCA Therapy after Transplantation for Primary Biliary Cholangitis. J. Hepatol. 2020, 73, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.R.; Greenan, G.; Arora, S.; Murali, A.; Mayo, M.J. UDCA Decreases Incidence of Primary Biliary Cholangitis and Biliary Complications after Liver Transplant: A Meta-Analysis. Liver Transpl. 2020. [Google Scholar] [CrossRef]
- Li, X.; Peng, J.; Ouyang, R.; Yang, Y.; Yu, C.; Lin, H. Risk factors for recurrent primary biliary cirrhosis after liver transplantation: A systematic review and meta-analysis. Dig. Liver Dis. 2020. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Liver transplantation. J. Hepatol. 2016, 64, 433–485. [Google Scholar] [CrossRef]
- Wiesner, R.H.; Fung, J.J. Present state of immunosuppressive therapy in liver transplant recipients. Liver Transpl. 2011, 17 (Suppl. 3), S1–S9. [Google Scholar] [CrossRef] [PubMed]
- Herzer, K.; Sterneck, M.; Welker, M.-W.; Nadalin, S.; Kirchner, G.; Braun, F.; Malessa, C.; Herber, A.; Pratschke, J.; Weiss, K.H.; et al. Current Challenges in the Post-Transplant Care of Liver Transplant Recipients in Germany. J. Clin. Med. Res. 2020, 9, 3570. [Google Scholar] [CrossRef]
- Chen, C.; Ke, R.; Yang, F.; Cai, Q.; Liu, J.; Huang, X.; Chen, J.; Xu, F.; Jiang, Y. Risk factors for recurrent autoimmune liver diseases after liver transplantation: A meta-analysis. Medicine 2020, 99, e20205. [Google Scholar] [CrossRef]
- Hirschfield, G.M.; Karlsen, T.H.; Lindor, K.D.; Adams, D.H. Primary sclerosing cholangitis. Lancet 2013, 382, 1587–1599. [Google Scholar] [CrossRef]
- Chapman, R.W. Primary sclerosing cholangitis. Medicine 2019, 47, 799–803. [Google Scholar] [CrossRef]
- Karlsen, T.H.; Folseraas, T.; Thorburn, D.; Vesterhus, M. Primary sclerosing cholangitis—A comprehensive review. J. Hepatol. 2017, 67, 1298–1323. [Google Scholar] [CrossRef] [Green Version]
- Lindor, K.D.; Kowdley, K.V.; Harrison, M.E. American College of Gastroenterology. ACG Clinical Guideline: Primary Sclerosing Cholangitis. Am. J. Gastroenterol. 2015, 110, 646–659. [Google Scholar] [CrossRef] [PubMed]
- de Vries, A.B.; Janse, M.; Blokzijl, H.; Weersma, R.K. Distinctive inflammatory bowel disease phenotype in primary sclerosing cholangitis. World J. Gastroenterol. 2015, 21, 1956–1971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmela, C.; Peerani, F.; Castaneda, D.; Torres, J.; Itzkowitz, S.H. Inflammatory Bowel Disease and Primary Sclerosing Cholangitis: A Review of the Phenotype and Associated Specific Features. Gut Liver 2018, 12, 17–29. [Google Scholar] [CrossRef] [Green Version]
- Weismüller, T.J.; Trivedi, P.J.; Bergquist, A.; Imam, M.; Lenzen, H.; Ponsioen, C.Y.; Holm, K.; Gotthardt, D.; Färkkilä, M.A.; Marschall, H.-U.; et al. Patient Age, Sex, and Inflammatory Bowel Disease Phenotype Associate with Course of Primary Sclerosing Cholangitis. Gastroenterology 2017, 152, 1975–1984.e8. [Google Scholar] [CrossRef] [Green Version]
- Irlès-Depé, M.; Roullet, S.; Neau-Cransac, M.; Dumortier, J.; Dharancy, S.; Houssel-Debry, P.; Boillot, O.; Chiche, L.; Laurent, C.; Laharie, D.; et al. Impact of Preexisting Inflammatory Bowel Disease on the Outcome of Liver Transplantation for Primary Sclerosing Cholangitis. Liver Transpl. 2020, 26, 1477–1491. [Google Scholar] [CrossRef]
- Bakhshi, Z.; Hilscher, M.B.; Gores, G.J.; Harmsen, W.S.; Viehman, J.K.; LaRusso, N.F.; Gossard, A.A.; Lazaridis, K.N.; Lindor, K.D.; Eaton, J.E. An Update on Primary Sclerosing Cholangitis Epidemiology, Outcomes and Quantification of Alkaline Phosphatase Variability in a Population-Based Cohort. J. Gastroenterol. 2020, 55, 523–532. [Google Scholar] [CrossRef]
- Tabibian, J.H.; Ali, A.H.; Lindor, K.D. Primary Sclerosing Cholangitis, Part 1: Epidemiology, Etiopathogenesis, Clinical Features, and Treatment. Gastroenterol. Hepatol. 2018, 14, 293–304. [Google Scholar]
- Wunsch, E.; Stadnik, A.; Kruk, B.; Szczepankiewicz, B.; Kotarska, K.; Krawczyk, M.; Górnicka, B.; Wójcicki, M.; Milkiewicz, P. Chronic Fatigue Persists in a Significant Proportion of Female Patients after Transplantation for Primary Sclerosing Cholangitis. Liver Transpl. 2021. [Google Scholar] [CrossRef]
- Gochanour, E.; Jayasekera, C.; Kowdley, K. Primary Sclerosing Cholangitis: Epidemiology, Genetics, Diagnosis, and Current Management. Clin. Liver Dis. 2020, 15, 125–128. [Google Scholar] [CrossRef] [Green Version]
- Vesterhus, M.; Karlsen, T.H. Emerging therapies in primary sclerosing cholangitis: Pathophysiological basis and clinical opportunities. J. Gastroenterol. 2020, 55, 588–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sirpal, S.; Chandok, N. Primary sclerosing cholangitis: Diagnostic and management challenges. Clin. Exp. Gastroenterol. 2017, 10, 265–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayable, A.; Ohabughiro, M.; Cheung, R.; Wong, R.J. Ethnicity-Specific Differences in Liver Transplant Outcomes among Adults with Primary Sclerosing Cholangitis: 2005–2017 United Network for Organ Sharing/Organ Procurement and Transplantation Network. J. Clin. Exp. Hepatol. 2021, 11, 30–36. [Google Scholar] [CrossRef]
- Graziadei, I.W.; Wiesner, R.H.; Marotta, P.J.; Porayko, M.K.; Hay, J.E.; Charlton, M.R.; Poterucha, J.J.; Rosen, C.B.; Gores, G.J.; LaRusso, N.F.; et al. Long-Term Results of Patients Undergoing Liver Transplantation for Primary Sclerosing Cholangitis. Hepatology 1999, 30, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Henson, J.B.; Patel, Y.A.; King, L.Y.; Zheng, J.; Chow, S.-C.; Muir, A.J. Outcomes of liver retransplantation in patients with primary sclerosing cholangitis. Liver Transpl. 2017, 23, 769–780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goss, J.A.; Shackleton, C.R.; Farmer, D.G.; Arnaout, W.S.; Seu, P.; Markowitz, J.S.; Martin, P.; Stribling, R.J.; Goldstein, L.I.; Busuttil, R.W. Orthotopic Liver Transplantation for Primary Sclerosing Cholangitis. A 12-Year Single Center Experience. Ann. Surg. 1997, 225, 472–481, discussion 481–483. [Google Scholar] [CrossRef]
- Jeyarajah, D.R.; Netto, G.J.; Lee, S.P.; Testa, G.; Abbasoglu, O.; Husberg, B.S.; Levy, M.F.; Goldstein, R.M.; Gonwa, T.A.; Tillery, G.W.; et al. Recurrent Primary Sclerosing Cholangitis after Orthotopic Liver Transplantation: Is Chronic Rejection Part of the Disease Process? Transplantation 1998, 66, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- Vera, A.; Moledina, S.; Gunson, B.; Hubscher, S.; Mirza, D.; Olliff, S.; Neuberger, J. Risk factors for recurrence of primary sclerosing cholangitis of liver allograft. Lancet 2002, 360, 1943–1944. [Google Scholar] [CrossRef]
- Khettry, U.; Keaveny, A.; Goldar-Najafi, A.; Lewis, W.D.; Pomfret, E.A.; Pomposelli, J.J.; Jenkins, R.L.; Gordon, F.D. Liver transplantation for primary sclerosing cholangitis: A long-term clinicopathologic study. Hum. Pathol. 2003, 34, 1127–1136. [Google Scholar] [CrossRef]
- Kugelmas, M.; Spiegelman, P.; Osgood, M.J.; Young, D.A.; Trotter, J.F.; Steinberg, T.; Waches, M.E.; Bak, T.; Kam, I.; Everson, G.T. Different immunosuppressive regimens and recurrence of primary sclerosing cholangitis after liver transplantation. Liver Transpl. 2003, 9, 727–732. [Google Scholar] [CrossRef]
- Brandsaeter, B.; Schrumpf, E.; Bentdal, O.; Brabrand, K.; Smith, H.J.; Abildgaard, A.; Clausen, O.P.; Bjoro, K. Recurrent primary sclerosing cholangitis after liver transplantation: A magnetic resonance cholangiography study with analyses of predictive factors. Liver Transpl. 2005, 11, 1361–1369. [Google Scholar] [CrossRef] [PubMed]
- Cholongitas, E.; Shusang, V.; Papatheodoridis, G.V.; Marelli, L.; Manousou, P.; Rolando, N.; Patch, D.; Rolles, K.; Davidson, B.; Burroughs, A.K. Risk Factors for Recurrence of Primary Sclerosing Cholangitis after Liver Transplantation. Liver Transpl. 2008, 14, 138–143. [Google Scholar] [CrossRef]
- Campsen, J.; Zimmerman, M.A.; Trotter, J.F.; Wachs, M.; Bak, T.; Steinberg, T.; Kam, I. Clinically recurrent primary sclerosing cholangitis following liver transplantation: A time course. Liver Transpl. 2008, 14, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.; Lord, J.D.; Yeh, M.M.; Cuevas, C.; Bakthavatsalam, R.; Kowdley, K.V. Risk factors for recurrence of primary sclerosing cholangitis after liver transplantation. Liver Transpl. 2008, 14, 245–251. [Google Scholar] [CrossRef]
- Alabraba, E.; Nightingale, P.; Gunson, B.; Hubscher, S.; Olliff, S.; Mirza, D.; Neuberger, J. A re-evaluation of the risk factors for the recurrence of primary sclerosing cholangitis in liver allografts. Liver Transpl. 2009, 15, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Egawa, H.; Taira, K.; Teramukai, S.; Haga, H.; Ueda, Y.; Yonezawa, A.; Masuda, S.; Tsuji, H.; Ashihara, E.; Takada, U.; et al. Risk factors for recurrence of primary sclerosing cholangitis after living donor liver transplantation: A single center experience. Dig. Dis. Sci. 2009, 54, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Kashyap, R.; Mantry, P.; Sharma, R.; Maloo, M.K.; Safadjou, S.; Qi, Y.; Jain, A.; Maliakkal, B.; Ryan, C.; Orloff, M. Comparative Analysis of Outcomes in Living and Deceased Donor Liver Transplants for Primary Sclerosing Cholangitis. J. Gastrointest. Surg. 2009, 13, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Moncrief, K.J.; Savu, A.; Ma, M.M.; Bain, V.G.; Wong, W.W.; Tandon, P. The natural history of inflammatory bowel disease and primary sclerosing cholangitis after liver transplantation—A single-centre experience. Can. J. Gastroenterol. 2010, 24, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Mason, A.L.; Montano-Loza, A.J. Systematic investigation of elevated cholestatic enzymes during the third posttransplant month. Liver Transpl. 2013, 19 (Suppl. 2), S23–S30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gelley, F.; Zádori, G.; Görög, D.; Kóbori, L.; Fehérvári, I.; Gámán, G.; Gerlei, Z.; Nagy, P.; Sárváry, E.; Nemes, B. Recurrence of Primary Sclerosing Cholangitis after Liver Transplantation - The Hungarian Experience. Interv. Med. Appl. Sci. 2014, 6, 16–18. [Google Scholar] [CrossRef]
- Ravikumar, R.; Tsochatzis, E.; Jose, S.; Allison, M.; Athale, A.; Creamer, F.; Gunson, B.; Iyer, V.; Madanur, M.; Manas, D.; et al. Risk Factors for Recurrent Primary Sclerosing Cholangitis after Liver Transplantation. J. Hepatol. 2015, 63, 1139–1146. [Google Scholar] [CrossRef] [Green Version]
- Hildebrand, T.; Pannicke, N.; Dechene, A.; Gotthardt, D.N.; Kirchner, G.; Reiter, F.P.; Sterneck, M.; Herzer, K.; Lenzen, H.; Rupp, C.; et al. Biliary Strictures and Recurrence after Liver Transplantation for Primary Sclerosing Cholangitis: A Retrospective Multicenter Analysis. Liver Transpl. 2016, 22, 42–52. [Google Scholar] [CrossRef]
- Gordon, F.D.; Goldberg, D.S.; Goodrich, N.P.; Lok, A.S.F.; Verna, E.C.; Selzner, N.; Stravitz, R.T.; Merion, R.M. Recurrent Primary Sclerosing Cholangitis in the Adult-to-Adult Living Donor Liver Transplantation Cohort Study: Comparison of Risk Factors between Living and Deceased Donor Recipients. Liver Transpl. 2016, 22, 1214–1222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueda, Y.; Kaido, T.; Okajima, H.; Hata, K.; Anazawa, T.; Yoshizawa, A.; Yagi, S.; Taura, K.; Masui, T.; Yamashiki, N.; et al. Long-Term Prognosis and Recurrence of Primary Sclerosing Cholangitis After Liver Transplantation: A Single-Center Experience. Transplant Direct 2017, 3, e334. [Google Scholar] [CrossRef] [PubMed]
- Lindström, L.; Jørgensen, K.K.; Boberg, K.M.; Castedal, M.; Rasmussen, A.; Rostved, A.A.; Isoniemi, H.; Bottai, M.; Bergquist, A. Risk Factors and Prognosis for Recurrent Primary Sclerosing Cholangitis after Liver Transplantation: A Nordic Multicentre Study. Scand. J. Gastroenterol. 2018, 53, 297–304. [Google Scholar] [CrossRef]
- Bajer, L.; Slavcev, A.; Macinga, P.; Sticova, E.; Brezina, J.; Roder, M.; Janousek, R.; Trunecka, P.; Spicak, J.; Drastich, P. Risk of Recurrence of Primary Sclerosing Cholangitis after Liver Transplantation Is Associated with de Novo Inflammatory Bowel Disease. World J. Gastroenterol. 2018, 24, 4939–4949. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.F.; Levy, C. Timing, Management, and Outcomes of Liver Transplantation in Primary Sclerosing Cholangitis. Semin. Liver Dis. 2017, 37, 305–313. [Google Scholar]
- Buchholz, B.M.; Lykoudis, P.M.; Ravikumar, R.; Pollok, J.M.; Fusai, G.K. Role of colectomy in preventing recurrent primary sclerosing cholangitis in liver transplant recipients. World J. Gastroenterol. 2018, 24, 3171–3180. [Google Scholar] [CrossRef]
- Trivedi, P.J.; Reece, J.; Laing, R.W.; Slaney, E.; Cooney, R.; Gunson, B.K.; Kamarajah, S.K.; Pinkney, T.; Thompson, F.; Muiesan, P.; et al. The Impact of Ileal Pouch-Anal Anastomosis on Graft Survival Following Liver Transplantation for Primary Sclerosing Cholangitis. Aliment. Pharmacol. Ther. 2018, 48, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Steenstraten, I.C.; Sebib Korkmaz, K.; Trivedi, P.J.; Inderson, A.; van Hoek, B.; Rodriguez Girondo, M.D.M.; Maljaars, P.W.J. Systematic review with meta-analysis: Risk factors for recurrent primary sclerosing cholangitis after liver transplantation. Aliment. Pharmacol. Ther. 2019, 49, 636–643. [Google Scholar] [CrossRef]
- Singh, S.; Edakkanambeth Varayil, J.; Loftus, E.V., Jr.; Talwalkar, J.A. Incidence of colorectal cancer after liver transplantation for primary sclerosing cholangitis: A systematic review and meta-analysis. Liver Transpl. 2013, 19, 1361–1369. [Google Scholar] [CrossRef] [Green Version]
- Lucey, M.R.; Terrault, N.; Ojo, L.; Hay, J.E.; Neuberger, J.; Blumberg, E.; Teperman, L.W. Long-term management of the successful adult liver transplant: 2012 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver Transpl. 2013, 19, 3–26. [Google Scholar] [CrossRef] [Green Version]
- Rao, B.B.; Lashner, B.; Kowdley, K.V. Reviewing the Risk of Colorectal Cancer in Inflammatory Bowel Disease After Liver Transplantation for Primary Sclerosing Cholangitis. Inflamm. Bowel Dis. 2018, 24, 269–276. [Google Scholar] [CrossRef] [Green Version]
- Boonstra, K.; Weersma, R.K.; van Erpecum, K.J.; Rauws, E.A.; Spanier, B.W.M.; Poen, A.C.; van Nieuwkerk, K.M.; Drenth, J.P.; Witteman, B.J.; Tuynman, H.A.; et al. Population-Based Epidemiology, Malignancy Risk, and Outcome of Primary Sclerosing Cholangitis. Hepatology 2013, 58, 2045–2055. [Google Scholar] [CrossRef] [PubMed]
- Rompianesi, G.; Ravikumar, R.; Jose, S.; Allison, M.; Athale, A.; Creamer, F.; Gunson, B.; Manas, D.; Monaco, A.; Mirza, D.; et al. Incidence and Outcome of Colorectal Cancer in Liver Transplant Recipients: A National, Multicentre Analysis on 8115 Patients. Liver Int. 2019, 39, 353–360. [Google Scholar] [CrossRef] [Green Version]
- Rossi, R.E.; Conte, D.; Massironi, S. Primary sclerosing cholangitis associated with inflammatory bowel disease: An update. Eur. J. Gastroenterol. Hepatol. 2016, 28, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Pineton de Chambrun, G.; Itzkowitz, S.; Sachar, D.B.; Colombel, J.-F. Review article: Colorectal neoplasia in patients with primary sclerosing cholangitis and inflammatory bowel disease. Aliment. Pharmacol. Ther. 2011, 34, 497–508. [Google Scholar] [CrossRef]
- Horsley-Silva, J.L.; Rodriguez, E.A.; Franco, D.L.; Lindor, K.D. An update on cancer risk and surveillance in primary sclerosing cholangitis. Liver Int. 2017, 37, 1103–1109. [Google Scholar] [CrossRef] [Green Version]
- Danford, C.J.; Trivedi, H.D.; Bonder, A. Bone Health in Patients with Liver Diseases. J. Clin. Densitom. 2020, 23, 212–222. [Google Scholar] [CrossRef]
- Hay, J.E. Bone disease in cholestatic liver disease. Gastroenterology 1995, 108, 276–283. [Google Scholar] [CrossRef]
- Guichelaar, M.M.J.; Kendall, R.; Malinchoc, M.; Hay, J.E. Bone mineral density before and after OLT: Long-term follow-up and predictive factors. Liver Transpl. 2006, 12, 1390–1402. [Google Scholar] [CrossRef]
- Guichelaar, M.M.J.; Schmoll, J.; Malinchoc, M.; Hay, J.E. Fractures and avascular necrosis before and after orthotopic liver transplantation: Long-term follow-up and predictive factors. Hepatology 2007, 46, 1198–1207. [Google Scholar] [CrossRef] [PubMed]
- Premaor, M.O.; Das, T.K.; Debiram, I.; Parker, R.A.; Ninkovic, M.; Alexander, G.T.; Comston, J.E. Fracture incidence after liver transplantation: Results of a 10-year audit. QJM 2011, 104, 599–606. [Google Scholar] [CrossRef] [Green Version]
- Trivedi, H.D.; Danford, C.J.; Goyes, D.; Bonder, A. Osteoporosis in Primary Biliary Cholangitis: Prevalence, Impact and Management Challenges. Clin. Exp. Gastroenterol. 2020, 13, 17–24. [Google Scholar] [CrossRef] [Green Version]
- Lorentzon, M.; Cummings, S.R. Osteoporosis: The evolution of a diagnosis. J. Intern. Med. 2015, 277, 650–661. [Google Scholar] [CrossRef] [PubMed]
- Compston, J.E. Osteoporosis after liver transplantation. Liver Transpl. 2003, 9, 321–330. [Google Scholar] [CrossRef]
- Monegal, A.; Navasa, M.; Guañabens, N.; Peris, P.; Pons, F.; Martinez de Osaba, M.J.; Ordi, J.; Rimola, A.; Rodés, J.; Muñoz-Gómez, J. Bone Disease after Liver Transplantation: A Long-Term Prospective Study of Bone Mass Changes, Hormonal Status and Histomorphometric Characteristics. Osteoporos. Int. 2001, 12, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Parés, A.; Guañabens, N. Bone health in patients with autoimmune liver diseases. Autoimmune Liver Dis. 2020, 219–232. [Google Scholar] [CrossRef]
- Kovvuru, K.; Kanduri, S.R.; Vaitla, P.; Marathi, R.; Gosi, S.; Garcia Anton, D.F.; Cabeza Rivera, F.H.; Garla, V. Risk Factors and Management of Osteoporosis Post-Transplant. Medicina 2020, 56, 302. [Google Scholar] [CrossRef] [PubMed]
- Chaney, A.; Heckman, M.G.; Diehl, N.N.; Meek, S.; Keaveny, A.P. Effectiveness and outcomes of current practice in treating vitamin d deficiency in patients listed for liver transplantation. Endocr. Pract. 2015, 21, 761–769. [Google Scholar] [CrossRef]
- Doi, J.; Moro, A.; Fujiki, M.; Eghtesad, B.; Quintini, C.; Menon, K.V.N.; Hashimoto, K.; Sasaki, K. Nutrition Support in Liver Transplantation and Postoperative Recovery: The Effects of Vitamin D Level and Vitamin D Supplementation in Liver Transplantation. Nutrients 2020, 12, 3677. [Google Scholar] [CrossRef]
- Ebadi, M.; Bhanji, R.A.; Mazurak, V.C.; Lytvyak, E.; Mason, A.; Czaja, A.J.; Montano-Loza, A.J. Severe vitamin D deficiency is a prognostic biomarker in autoimmune hepatitis. Aliment. Pharmacol. Ther. 2019, 49, 173–182. [Google Scholar] [CrossRef]
- Guañabens, N.; Parés, A.; Mariñoso, L.; Brancós, M.A.; Piera, C.; Serrano, S.; Rivera, F.; Rodés, J. Factors influencing the development of metabolic bone disease in primary biliary cirrhosis. Am. J. Gastroenterol. 1990, 85, 1356–1362. [Google Scholar]
- Bengoa, J.M.; Sitrin, M.D.; Meredith, S.; Kelly, S.E.; Shah, N.; Baker, A.L.; Rosenberg, I.H. Intestinal calcium absorption and vitamin D status in chronic cholestatic liver disease. Hepatology 1984, 4, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Danford, C.J.; Trivedi, H.D.; Papamichael, K.; Tapper, E.B.; Bonder, A. Osteoporosis in primary biliary cholangitis. World J. Gastroenterol. 2018, 24, 3513–3520. [Google Scholar] [CrossRef]
- Agmon-Levin, N.; Kopilov, R.; Selmi, C.; Nussinovitch, U.; Sánchez-Castañón, M.; López-Hoyos, M.; Amital, H.; Kivity, S.; Gershwin, E.M.; Shoenfeld, Y. Vitamin D in Primary Biliary Cirrhosis, a Plausible Marker of Advanced Disease. Immunol. Res. 2015, 61, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Guo, G.-Y.; Shi, Y.-Q.; Wang, L.; Ren, X.; Han, Z.-Y.; Guo, C.-C.; Cui, L.-N.; Wang, J.-B.; Zhu, J.; Wang, N.; et al. Serum Vitamin D Level Is Associated with Disease Severity and Response to Ursodeoxycholic Acid in Primary Biliary Cirrhosis. Aliment. Pharmacol. Ther. 2015, 42, 221–230. [Google Scholar] [CrossRef]
- Wang, Z.; Peng, C.; Wang, P.; Sui, J.; Wang, Y.; Sun, G.; Liu, M. Serum vitamin D level is related to disease progression in primary biliary cholangitis. Scand. J. Gastroenterol. 2020, 55, 1333–1340. [Google Scholar] [CrossRef]
- Arnold, J.C.; Hauser, D.; Ziegler, R.; Kommerell, B.; Otto, G.; Theilmann, L.; Wüster, C. Bone disease after liver transplantation. Transpl. Proc. 1992, 24, 2709–2710. [Google Scholar]
- Vlăduţ, C.; Ciocîrlan, M.; Bilous, D.; Șandru, V.; Stan-Ilie, M.; Panic, N.; Becheanu, G.; Jinga, M.; Costache, R.S.; Costache, D.O.; et al. An Overview on Primary Sclerosing Cholangitis. J. Clin. Med. Res. 2020, 9, 754. [Google Scholar] [CrossRef] [Green Version]
- Lan, G.-B.; Xie, X.-B.; Peng, L.-K.; Liu, L.; Song, L.; Dai, H.-L. Current Status of Research on Osteoporosis after Solid Organ Transplantation: Pathogenesis and Management. BioMed Res. Int. 2015, 2015, 413169. [Google Scholar] [CrossRef] [Green Version]
- Crippin, J.S. Bone disease after liver transplantation. Liver Transpl. 2001, 7, S27–S35. [Google Scholar] [CrossRef] [PubMed]
- Crawford, B.A.L.; Kam, C.; Pavlovic, J.; Byth, K.; Handelsman, D.J.; Angus, P.W.; McCaughan, G.W. Zoledronic acid prevents bone loss after liver transplantation: A randomized, double-blind, placebo-controlled trial. Ann. Intern. Med. 2006, 144, 239–248. [Google Scholar] [CrossRef]
- Atamaz, F.; Hepguler, S.; Akyildiz, M.; Karasu, Z.; Kilic, M. Effects of alendronate on bone mineral density and bone metabolic markers in patients with liver transplantation. Osteoporos. Int. 2006, 17, 942–949. [Google Scholar] [CrossRef]
- Shane, E.; Cohen, A.; Stein, E.M.; McMahon, D.J.; Zhang, C.; Young, P.; Pandit, K.; Staron, R.B.; Verna, E.C.; Brown, R.; et al. Zoledronic AcidVersusAlendronate for the Prevention of Bone Loss after Heart or Liver Transplantation. J. Clin. Endocrinol. Metab. 2012, 97, 4481–4490. [Google Scholar] [CrossRef] [Green Version]
- Bhat, M.; Usmani, S.E.; Azhie, A.; Woo, M. Metabolic Consequences of Solid Organ Transplantation. Endocr. Rev. 2020. [Google Scholar] [CrossRef]
- De Luca, L.; Kalafateli, M.; Bianchi, S.; Alasaker, N.; Buzzetti, E.; Rodríguez-Perálvarez, M.; Thorburn, D.; O’Beirne, J.; Patch, D.; Leandro, G.; et al. Cardiovascular Morbidity and Mortality Is Increased Post-Liver Transplantation Even in Recipients with No Pre-Existing Risk Factors. Liver Int. 2019, 39, 1557–1565. [Google Scholar] [CrossRef]
- Watt, K.D.S.; Pedersen, R.A.; Kremers, W.K.; Heimbach, J.K.; Charlton, M.R. Evolution of causes and risk factors for mortality post-liver transplant: Results of the NIDDK long-term follow-up study. Am. J. Transpl. 2010, 10, 1420–1427. [Google Scholar] [CrossRef]
- Khurmi, N.S.; Chang, Y.-H.; Eric Steidley, D.; Singer, A.L.; Hewitt, W.R.; Reddy, K.S.; Moss, A.A.; Mathur, A.K. Hospitalizations for Cardiovascular Disease After Liver Transplantation in the United States. Liver Transpl. 2018, 24, 1398–1410. [Google Scholar] [CrossRef] [Green Version]
- Albeldawi, M.; Aggarwal, A.; Madhwal, S.; Cywinski, J.; Lopez, R.; Eghtesad, B.; Zein, N.N. Cumulative risk of cardiovascular events after orthotopic liver transplantation. Liver Transpl. 2012, 18, 370–375. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Kallwitz, E.R.; Loy, V.; Mettu, P.; Von Roenn, N.; Berkes, J.; Cotler, S.J. Physical activity and metabolic syndrome in liver transplant recipients. Liver Transpl. 2013, 19, 1125–1131. [Google Scholar] [CrossRef]
- Mann, S.; Beedie, C.; Jimenez, A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: Review, synthesis and recommendations. Sports Med. 2014, 44, 211–221. [Google Scholar] [CrossRef] [Green Version]
- Piercy Katrina, L.; Troiano Richard, P. Physical Activity Guidelines for Americans From the US Department of Health and Human Services. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e005263. [Google Scholar]
- Dunn, M.A.; Rogal, S.S.; Duarte-Rojo, A.; Lai, J.C. Physical Function, Physical Activity, and Quality of Life After Liver Transplantation. Liver Transpl. 2020, 26, 702–708. [Google Scholar] [CrossRef]
- Kim, N.G.; Sharma, A.; Saab, S. Cardiovascular and metabolic disease in the liver transplant recipient. Best Pract. Res. Clin. Gastroenterol. 2020, 46–47, 101683. [Google Scholar] [CrossRef] [PubMed]
- Reuben, A. Long-term management of the liver transplant patient: Diabetes, hyperlipidemia, and obesity. Liver Transpl. 2001, 7, S13–S21. [Google Scholar] [CrossRef]
- Sharma, P.; Arora, A. Approach to prevention of non-alcoholic fatty liver disease after liver transplantation. Transl. Gastroenterol. Hepatol. 2020, 5, 51. [Google Scholar] [CrossRef]
- Jiménez-Pérez, M.; González-Grande, R.; Omonte Guzmán, E.; Amo Trillo, V.; Rodrigo López, J.M. Metabolic complications in liver transplant recipients. World J. Gastroenterol. 2016, 22, 6416–6423. [Google Scholar] [CrossRef] [PubMed]
- Akarsu, M.; Bakir, Y.; Karademir, S.; Unek, T.; Bacakoglu, A.; Astarcioglu, I. Prevalence and risk factors for obesity after liver transplantation: A single-center experience. Hepat. Mon. 2013, 13, e7569. [Google Scholar]
- Segev, D.L.; Sozio, S.M.; Shin, E.J.; Nazarian, S.M.; Nathan, H.; Thuluvath, P.J.; Montgomery, R.A.; Cameron, A.M.; Maley, W.R. Steroid Avoidance in Liver Transplantation: Meta-Analysis and Meta-Regression of Randomized Trials. Liver Transpl. 2008, 14, 512–525. [Google Scholar] [CrossRef]
- Hüsing, A.; Kabar, I.; Schmidt, H.H. Lipids in liver transplant recipients. World J. Gastroenterol. 2016, 22, 3315–3324. [Google Scholar] [CrossRef]
- Charlton, M.; Levitsky, J.; Aqel, B.; OʼGrady, J.; Hemibach, J.; Rinella, M.; Fung, J.; Ghabril, M.; Thomason, R.; Burra, P.; et al. International Liver Transplantation Society Consensus Statement on Immunosuppression in Liver Transplant Recipients. Transplantation 2018, 102, 727–743. [Google Scholar] [CrossRef]
- Charlton, M.; Rinella, M.; Patel, D.; McCague, K.; Heimbach, J.; Watt, K. Everolimus Is Associated with Less Weight Gain Than Tacrolimus 2 Years After Liver Transplantation: Results of a Randomized Multicenter Study. Transplantation 2017, 101, 2873–2882. [Google Scholar] [CrossRef]
| Reference | Sample Size | Frequency | Risk Factors for Recurrence |
|---|---|---|---|
| Wright et al. [18] | 43 | 11 (25.6%) | HLA-DR3-positive recipient |
| Prados et al. [19] | 27 | 9 (33%) 8% at 1 year 68% at 5 years | HLA-DR3-positive recipient |
| Ratziu et al. [20] | 25 | 3 (20%) | NR |
| Milkiewicz et al. [16] | 47 | 13 (28%) | Discontinuation of steroids HLA-DR3-positive recipient (n.s.) |
| Reich et al. [21] | 32 | 6 (25%) at 15 ± 2 months | Re-transplantation for rAIH Transplantation for chronic AIH (patients transplanted for fulminant AIH seem to be protected from recurrence) (n.s.) |
| Ayata et al. [22] | 14 | 5 (42%) | HLA-DR3-positive recipient High-grade inflammation of the native liver Tacrolimus-based immunosuppressive regimens |
| González-Koch et al. [23] | 41 | 7 (17%) at 4.6 ± 1 years | HLA-DR3 or HLA-DR4 incidence in recipient |
| Renz et al. [24] | 37 | 12 (32%) at 25 ± 22 months | NR |
| Yusoff et al. [25] | 12 | 2 (17%) | NR |
| Molmenti et al. [26] | 45 | 11 (20%) | NR |
| Duclos-Vallée et al. [27] | 17 | 7 (41%) at 2.5 ± 1.7 years | HLA-DR3-positive recipient |
| Balan et al. [28] | NR | NR | HLA-DR locus mismatching |
| Montano-Loza et al. [29] | 46 | 11 (24%) 18% at 5 years 32% at 10 years | Concomitant autoimmune disease Abnormal pre-LT AST, ALT, IgG Moderate to severe hepatic inflammation in the liver explants |
| Krishnamoorthy et al. [30] | 73 | 5 (7%) 6% at 5 years 11% at 10 years | NR |
| Reference | Sample Size | Frequency | Risk Factors for Recurrence |
|---|---|---|---|
| Wong et al. [54] | 2 | 2 (100%) | Tacrolimus-based immunosuppression |
| Dmitrewski et al. [55] | 27 | 8 (30%) | Tacrolimus-based immunosuppression |
| Liermann Garcia et al. [56] | 400 | 68 (17%) at 36 months | Younger age at transplant Tacrolimus-based immunosuppression |
| Hashimoto et al. [57] | 6 | 2 (33%) | Tacrolimus-based immunosuppression |
| Khettry et al. [58] | 43 | 8 (18.6%) | Not significant results |
| Levitsky et al. [59] | 46 | 7 (15%) at 78 months | Not significant results |
| Sylvestre et al. [60] | 100 | 17 (17%) at 4.7 years | NR |
| Sanchez et al. [61] | 156 | 17 (10.9%) at 72.1 months | Used of tacrolimus rather than cyclosporine |
| Neuberger et al. [62] | 485 | 114 (23%) | Recipient’s age Use of tacrolimus |
| Guy et al. [63] | 48 | 17 (35%) | Not significant results |
| Jacob et al. [50] | 100 | 14 (14%) | Tacrolimus-based immunosuppression |
| Morioka et al. [64] | 50 | 9 (18%) | Average trough level of Tacrolimus within 1-year LDLT HLA-DR locus mismatching |
| Charatcharoenwitthaya et al. [65] | 164 | 52 (32%) at 3.5 years | Older recipient age at transplant Male gender Tacrolimus-based immunosuppression |
| Montano-Loza et al. [66] | 108 | 28 (26%) 13% at 5 years 29% at 10 years | Tacrolimus-based immunosuppression Use of mycophenolate mofetil |
| Bosch et al. [67] | 90 | 48 (53%) 27% at 5 years 47% at 10 years | No significant factors |
| Egawa et al. [68] | 444 | 65 (14%) 9.6% at 5 years 20.6% at 10 years | Younger age at transplant (<48 years) IgM > 554 mg/dL Gender mismatch Use of Cyclosporin A as initial immunosuppression |
| Kogiso et al. [69] | 330 | 58 (14.0%) at 4.6 (0.8–14.5) years | Younger recipient age Higher serum IgM Donor sex mismatch Human leukocyte antigen B60 and DR8 Initial treatment with cyclosporine A |
| Montano-Loza et al. [48] | 785 | 173(22%) at 5 years 283(36%) at 10 years | Biochemical cholestasis within the first 6 months Tacrolimus use |
| Corpechot et al. [70] | 780 | 233 (30%) 18% at 5 years 31% at 10 years | Exposure to tacrolimus |
| Reference | Sample Size | Frequency | Risk Factors for Recurrence |
|---|---|---|---|
| Goss et al. [94] | 127 | 11 (8.6%) | NR |
| Jeyarajah et al. [95] | 100 | 18 (18%) at 21 months | Younger recipient age CMV infection IBD presence |
| Graziadei et al. [92] | 150 | 30 (20%) at 55 months | NR |
| Vera et al. [96] | 152 | 56 (37%) at 36 months | Male gender |
| Khettry et al. [97] | 51 | 6 (14%) | Donor-recipient gender mismatch |
| Kugelmas et al. [98] | 71 | 15 (21.1%) | Use of orthoclone (OKT3) |
| Brandsaeter et al. [99] | 61 | 19 (39%) | Steroid-resistant rejection |
| Balan et al. [29] | NR | NR | HLA-A locus mismatching |
| Cholongitas et al. [100] | 69 | 7 (13.5%) at 6 months | Ulcerative colitis requiring maintenance steroids |
| Campsen et al. [101] | 130 | 22 (16.9%) at 60 months | Presence of cholangiocarcinoma before transplantation |
| Alexander et al. [102] | 69 | 7 (10%) at 68 months | Presence of HLA-DRB1*08 ACR Steroid-resistant ACR |
| Alabraba et al. [103] | 230 | 54 (23.5%) at 4.6 years | Presence of intact colon after transplant |
| Egawa et al. [104] | 30 | 11 (37%) | CMV diseases Related donor |
| Kashyap et al. [105] | 58 | 11 (19%) at 41.5 months | NR |
| Moncrief et al. [106] | 59 | 15 (25%) at 40.2 months 21% at 5 years 37% at 10 years | Acute cellular rejection Cytomegalovirus mismatch |
| Mason et al. [107] | 92 | NR | Cholestasis at 3 months |
| Gelley et al. [108] | 6 (12%) | Active IBD in the colon | |
| Ravikumar et al. [109] | 679 | 81 (14.3%) at 9 years | Younger age Presence of UC after LT |
| Hildebrand et al. [110] | 335 | 62 (20.3%) at 4.6 years | IBD Older donor age Higher INR at the time of LT |
| Gordon et al. [111] | 306 | 34 (11%) 8.7% at 5 years 22.4% at 10 years | Biliary complication Higher donor age Pre-transplant cholangiocarcinoma |
| Ueda et al. [112] | 45 | 16 (40%) at 30 months 39.3% at 5 years 45.8% at 10 years | Active IBD after LT |
| Lindström et al. [113] | 440 | 85 (19%) | Treatment with tacrolimus |
| Bajer et al. [114] | 47 | 21 (44.7%) at 63 months | De novo colitis after LT History of ACR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barba Bernal, R.; Medina-Morales, E.; Goyes, D.; Patwardhan, V.; Bonder, A. Management of Autoimmune Liver Diseases after Liver Transplantation. Transplantology 2021, 2, 162-182. https://doi.org/10.3390/transplantology2020016
Barba Bernal R, Medina-Morales E, Goyes D, Patwardhan V, Bonder A. Management of Autoimmune Liver Diseases after Liver Transplantation. Transplantology. 2021; 2(2):162-182. https://doi.org/10.3390/transplantology2020016
Chicago/Turabian StyleBarba Bernal, Romelia, Esli Medina-Morales, Daniela Goyes, Vilas Patwardhan, and Alan Bonder. 2021. "Management of Autoimmune Liver Diseases after Liver Transplantation" Transplantology 2, no. 2: 162-182. https://doi.org/10.3390/transplantology2020016
APA StyleBarba Bernal, R., Medina-Morales, E., Goyes, D., Patwardhan, V., & Bonder, A. (2021). Management of Autoimmune Liver Diseases after Liver Transplantation. Transplantology, 2(2), 162-182. https://doi.org/10.3390/transplantology2020016






