Persistent Right Umbilical Vein: Clinical Case and Literature Review
Abstract
1. Introduction
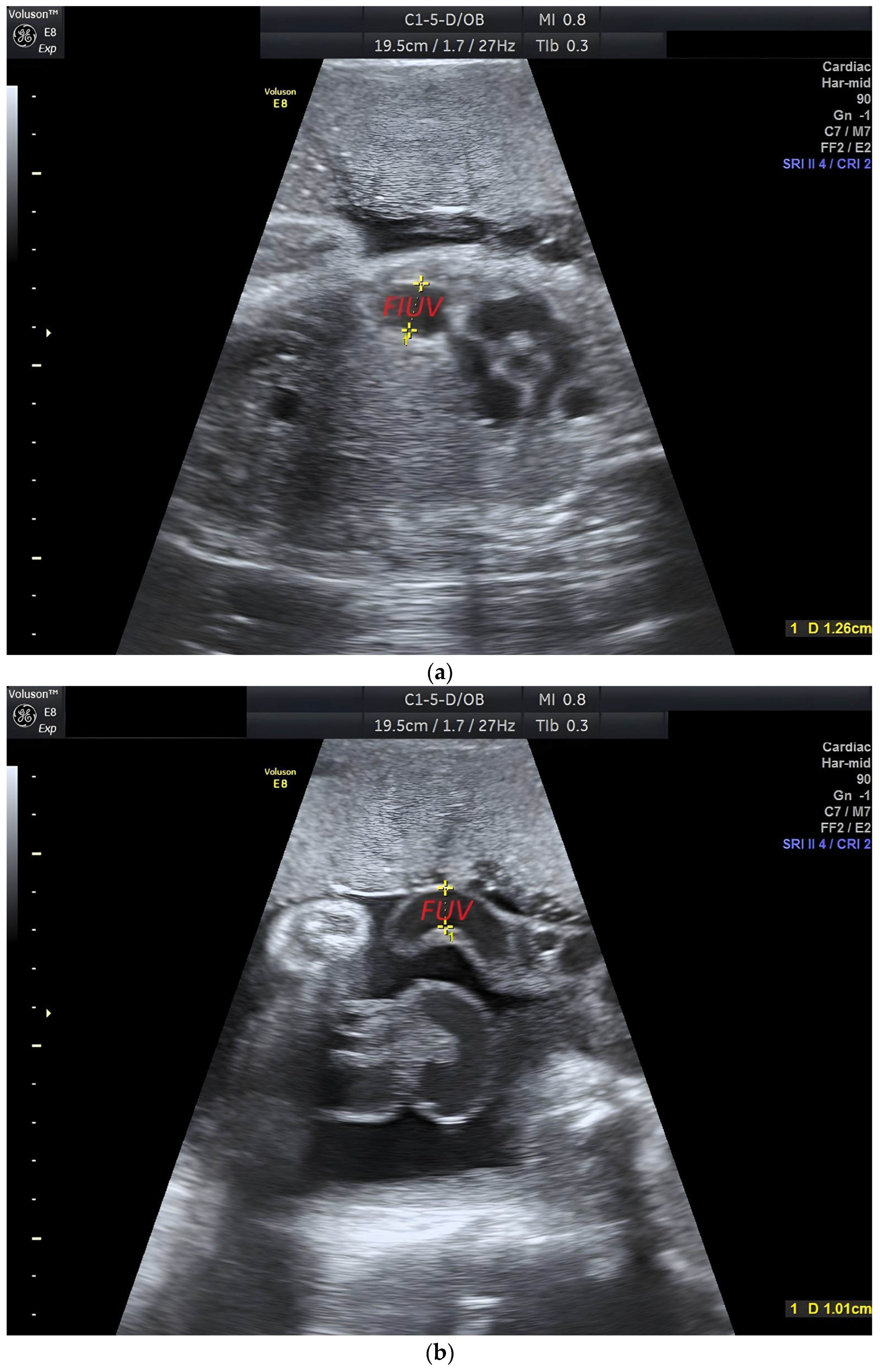
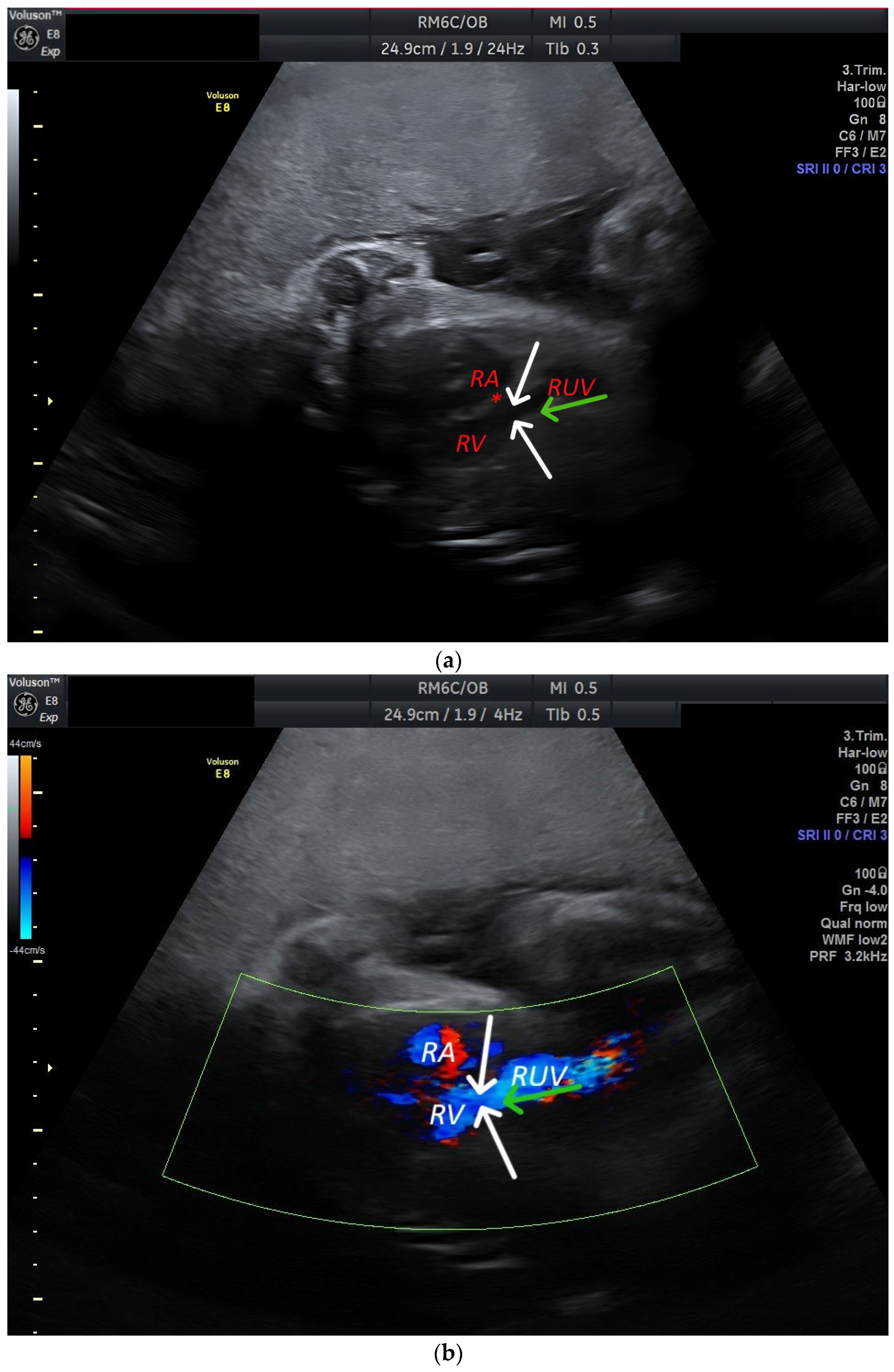
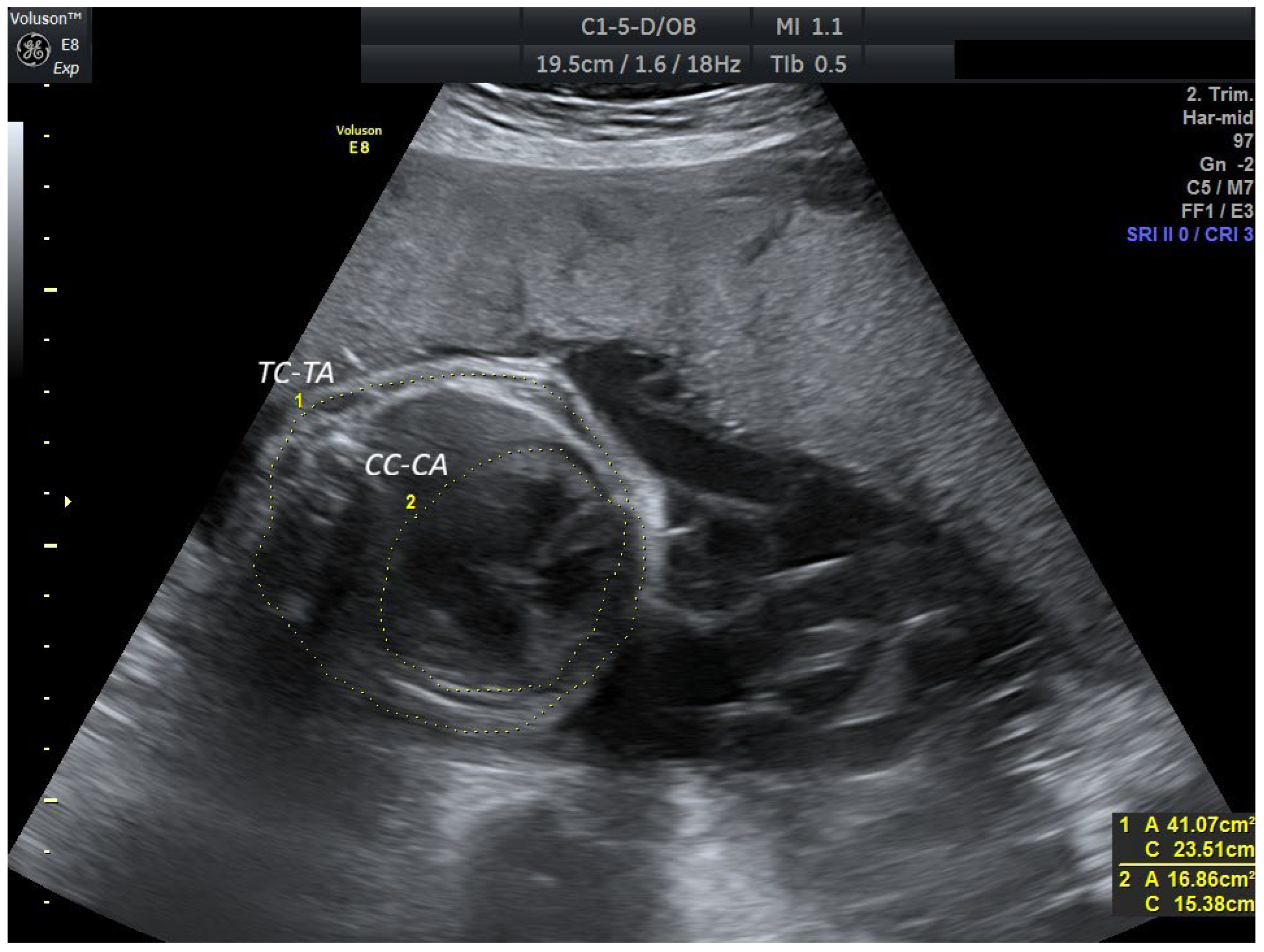
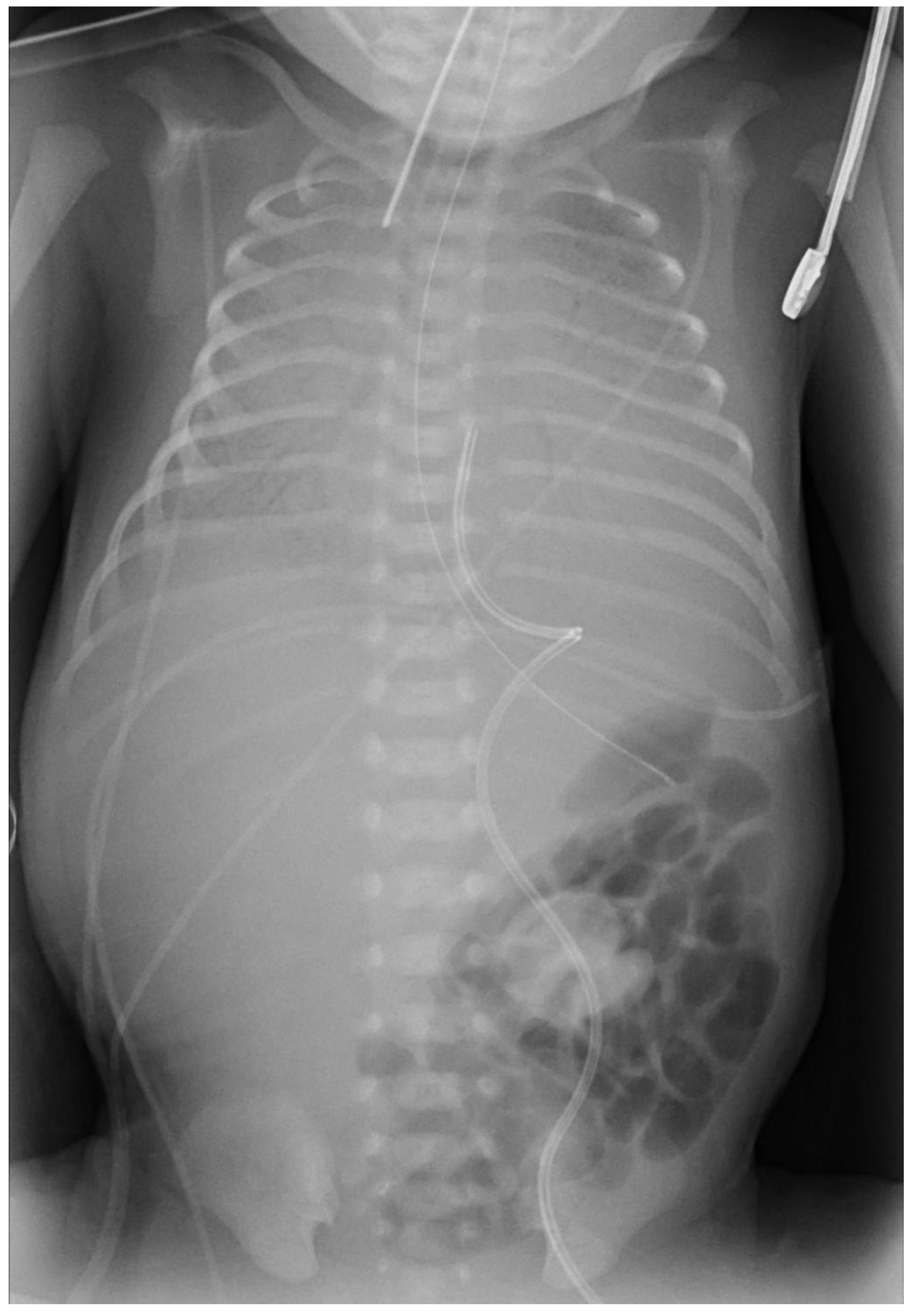
2. Case Report
3. Discussion
3.1. Incidence and Etiology
3.2. Types of PRUV
3.3. Diagnostics
3.4. Clinic and Prognosis
3.5. Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FIUV | Intra-abdominal umbilical vein |
| FUV | Extra-abdominal umbilical vein |
| LUHS | Lithuanian University of Health Sciences |
| MRI | Magnetic resonance imaging |
| MV | Mechanical ventilation |
| NICU | Neonatal Intensive Care Unit |
| PCC | Perinatology Coordination Center |
| PRUV | Persistent right umbilical vein |
| PRUV-E | Persistent right umbilical vein extrahepatic type |
| PRUV-I | Persistent right umbilical vein intrahepatic type |
| RA | Right atrium |
| RV | Right ventricle |
| RUV | Right umbilical vein |
| VUH | Vilnius University Hospital |
References
- Li, J.; Yuan, Q.; Ding, H.; Yang, Z.; Wang, B.; Wang, B. Ultrasonic detection of fetal persistent right umbilical vein and incidence and significance of concomitant anomalies. BMC Pregnancy Childbirth 2020, 20, 610. [Google Scholar] [CrossRef] [PubMed]
- Pinna, G.; De Carolis, M.P.; Lanzone, A.; Del Sordo, G.; Botta, A.; De Carolis, S. Persistence of right umbilical vein: A singular case. Turk. J. Pediatr. 2020, 62, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Sompagdee, N.; Anuwutnavin, S.; Burapasikarin, C.; Ruangvutilert, P.; Thongkloung, P. Nomograms of fetal cardiothoracic ratio from 17 to 37 weeks’ gestation as assessed by three different measurement techniques and their correlation with gestational age. Prenat. Diagn. 2021, 41, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Mathai, B.M.; Singla, S.C.; Nittala, P.P.; Chakravarti, R.J.; Toppo, J.N. Placental Thickness: Its correlation with ultrasonographic gestational age in normal and intrauterine growth-retarded pregnancies in the late second and third trimester. J. Obstet. Gynecol. India 2013, 63, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Spurway, J.; Logan, P.; Pak, S. The development, structure and blood flow within the umbilical cord with particular reference to the venous system. Australas. J. Ultrasound Med. 2015, 15, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, S.V.; Mohammed, S.; Dharan, B.S. Intracardiac relation of extrahepatic persistent right umbilical vein. Indian J. Thorac. Cardiovasc. Surg. 2020, 37, 354–356. [Google Scholar] [CrossRef] [PubMed]
- Wolman, I.; Gull, I.; Fait, G.; Amster, R.; Kupferminc, M.J.; Lessing, J.B.; Jaffa, A.J. Persistent right umbilical vein: Incidence and significance. Ultrasound Obstet. Gynecol. 2002, 19, 562–564. [Google Scholar] [CrossRef] [PubMed]
- Krzyżanowski, A.; Swatowski, D.; Gęca, T.; Kwiatek, M.; Stupak, A.; Woźniak, S.; Kwaśniewska, A. Prenatal diagnosis of persistent right umbilical vein–incidence and clinical impact. A prospective study. Aust. N. Z. J. Obstet. Gynaecol. 2019, 59, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Yagel, S.; Kivilevitch, Z.; Cohen, S.M.; Valsky, D.V.; Messing, B.; Shen, O.; Achiron, R.; Anteby, E.Y. The fetal venous system, part II: Ultrasound evaluation of the fetus with congenital venous system malformation or developing circulatory compromise. Ultrasound Obstet. Gynecol. 2010, 36, 93–111. [Google Scholar] [CrossRef] [PubMed]
- Weichert, J.; Hartge, D.; Germer, U.; Axt-Fliedner, R.; Gembruch, U. Persistent right umbilical vein: A prenatal condition worth mentioning? Ultrasound Obstet. Gynecol. 2011, 37, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhou, Q.; Zhou, C.; Wang, J.; Shi, C.; Long, B.; Zhang, M.; Luo, G. Z-score reference ranges for umbilical vein diameter and blood flow volume in normal fetuses. J. Ultrasound Med. 2022, 41, 907–916. [Google Scholar] [CrossRef]
- Toscano, P.; Saccone, G.; Di Meglio, L.; Di Meglio, L.; Mastantuoni, E.; Riccardi, C.; Sirico, A.; Berghella, V. Intrahepatic persistent fetal right umbilical vein: A retrospective study. J. Matern. Fetal Neonatal Med. 2021, 34, 4025–4028. [Google Scholar] [CrossRef]
- Chan, E.S.; Suchet, I.; Yu, W.; Somerset, D.; Soliman, N.; Kuret, V.; Liu, H.; Keating, S. Absence of ductus venosus: A comparison of two distinctive fetal autopsy cases and embryologic perspectives. Pediatr. Dev. Pathol. 2023, 27, 139–144. [Google Scholar] [CrossRef]
- Martinez, R.; Gamez, F.; Bravo, C.; Sánchez, P.; Orizales, C.; Ortiz, L.; Garcia-Talavera, J.; Gorostidi, M.A. Perinatal outcome after ultrasound prenatal diagnosis of persistent right umbilical vein. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 168, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Morkuniene, R.; Cole, T.J.; Jakimaviciene, E.M.; Bankauskiene, A.; Isakova, J.; Drazdiene, N.; Vitrikas, T.; Vasiliauskiene, L.; Ramasauskaite, D. Regional references vs international standards for assessing weight and length by gestational age in Lithuanian neonates. Front. Pediatr. 2023, 11, 1173685. [Google Scholar] [CrossRef] [PubMed]
| Features | PRUV-I | PRUV-E |
| Frequency | 95% | 5% |
| Drainage | Right portal vein | Directly into systemic veins |
| Associated abnormalities | Rare | More frequent (cardiac, genitourinary, chromosomal, gastrointestinal, nervous, skeletal, respiratory) |
| Hemodynamic impact | Usually minimal | Can significantly alter fetal hemodynamics |
| Connection with the ductus venosus | Usually remains patent | Often absent or altered |
| Prognosis | Generally favorable | Often worse due to associated complications. Close monitoring needed |
| Typical timing of diagnosis | Second trimester | Second trimester |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karakaite, D.; Volochovic, J. Persistent Right Umbilical Vein: Clinical Case and Literature Review. Reprod. Med. 2025, 6, 36. https://doi.org/10.3390/reprodmed6040036
Karakaite D, Volochovic J. Persistent Right Umbilical Vein: Clinical Case and Literature Review. Reproductive Medicine. 2025; 6(4):36. https://doi.org/10.3390/reprodmed6040036
Chicago/Turabian StyleKarakaite, Dagna, and Jelena Volochovic. 2025. "Persistent Right Umbilical Vein: Clinical Case and Literature Review" Reproductive Medicine 6, no. 4: 36. https://doi.org/10.3390/reprodmed6040036
APA StyleKarakaite, D., & Volochovic, J. (2025). Persistent Right Umbilical Vein: Clinical Case and Literature Review. Reproductive Medicine, 6(4), 36. https://doi.org/10.3390/reprodmed6040036





