Conversion of Femoral-Tibial Bypass Surgery into Deep Vein Arterialization in a Patient with Severe Peripheral Artery Disease: Post-Operative Computed Tomography and Angiography Findings
Abstract
1. Introduction
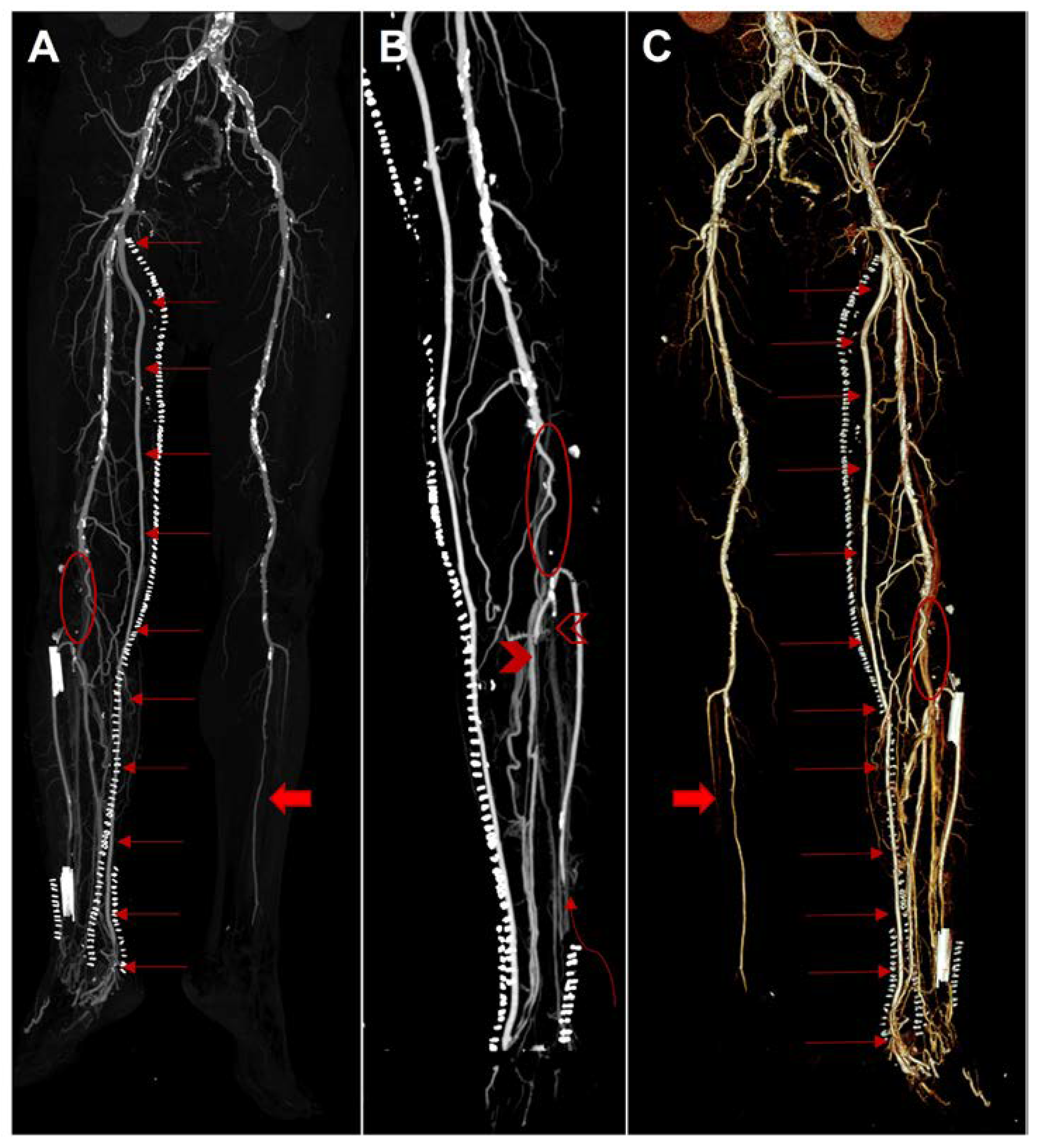
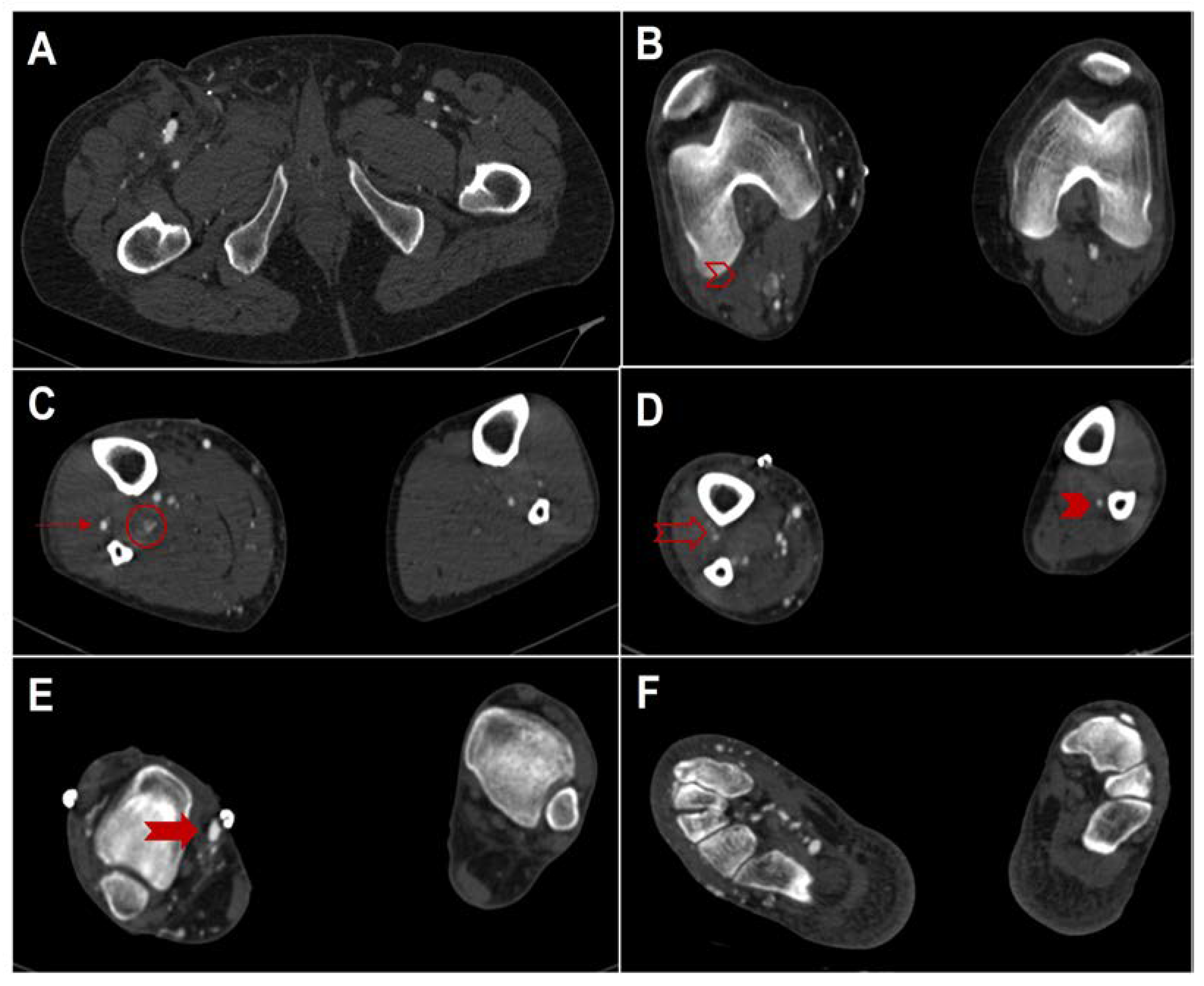
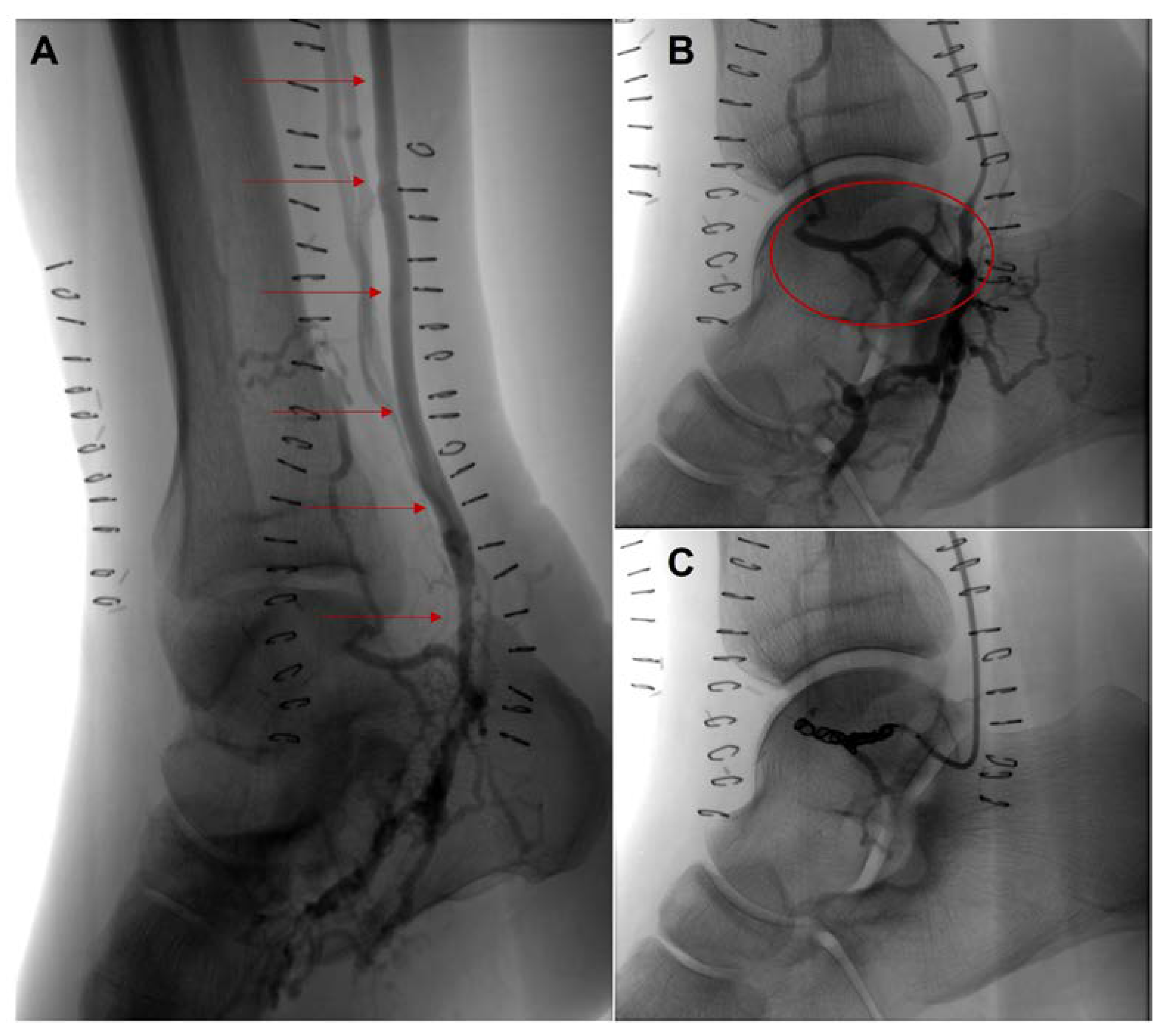
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sibley, R.C.; Reis, S.P.; MacFarlane, J.J.; Reddick, M.A.; Kalva, S.P.; Sutphin, P.D. Noninvasive Physiologic Vascular Studies: A Guide to Diagnosing Peripheral Arterial Disease. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2017, 37, 346–357. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.-B.; Bartelink, M.-L.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.-P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in Collaboration with the European Society for Vascular Surgery (ESVS): Document Covering Atherosclerotic Disease of Extracranial Carotid and Vertebral, Mesenteric, Renal, Upper and Lower Extremity ArteriesEndorsed by: The European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur. Heart J. 2018, 39, 763–816. [Google Scholar] [CrossRef] [PubMed]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.R.; TASC II Working Group; Bell, K.; Caporusso, J.; Durand-Zaleski, I.; et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2007, 33 (Suppl. S1), S1–S75. [Google Scholar] [CrossRef] [PubMed]
- Abu Dabrh, A.M.; Steffen, M.W.; Undavalli, C.; Asi, N.; Wang, Z.; Elamin, M.B.; Conte, M.S.; Murad, M.H. The Natural History of Untreated Severe or Critical Limb Ischemia. J. Vasc. Surg. 2015, 62, 1642–1651.e3. [Google Scholar] [CrossRef] [PubMed]
- Adam, D.J.; Beard, J.D.; Cleveland, T.; Bell, J.; Bradbury, A.W.; Forbes, J.F.; Fowkes, F.G.R.; Gillepsie, I.; Ruckley, C.V.; Raab, G.; et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL): Multicentre, Randomised Controlled Trial. Lancet Lond. Engl. 2005, 366, 1925–1934. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.-B.; Suresh, K.R.; Murad, M.H.; et al. Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. J. Vasc. Surg. 2019, 69, 3S–125S.e40. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.T.; Gologorsky, R.; Kibrik, P.; Chandra, V.; Prent, A.; Lee, J.; Dua, A. Open, Percutaneous, and Hybrid Deep Venous Arterialization Technique for No-Option Foot Salvage. J. Vasc. Surg. 2020, 71, 2152–2160. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, R.B.; Baker, J.D.; Ernst, C.; Johnston, K.W.; Porter, J.M.; Ahn, S.; Jones, D.N. Recommended Standards for Reports Dealing with Lower Extremity Ischemia: Revised Version. J. Vasc. Surg. 1997, 26, 517–538. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Belli, A.M.; Jacob, S. Distal Venous Arterialisation for Salvage of Critically Ischaemic Inoperable Limbs. Lancet Lond. Engl. 1999, 354, 1962–1965. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, S.; Powell, R.J. Management of the No-Option Foot: Deep Vein Arterialization. Semin. Vasc. Surg. 2022, 35, 210–218. [Google Scholar] [CrossRef]
- Montelione, N.; Catanese, V.; Gabellini, T.; Codispoti, F.A.; Nenna, A.; Spinelli, F.; Stilo, F. Duplex and Angiographic-Assisted Evaluation of Outcomes of Endovascular Embolization after Surgical Deep Vein Arterialization for the Treatment No-Option Critical Limb Ischemia Patients. Diagnostics 2022, 12, 2986. [Google Scholar] [CrossRef]
- Allen, J.; Murray, A. Comparison of Three Arterial Pulse Waveform Classification Techniques. J. Med. Eng. Technol. 1996, 20, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.; Cranny, G.; Burch, J.; Aguiar-Ibáñez, R.; Craig, D.; Wright, K.; Berry, E.; Gough, M.; Kleijnen, J.; Westwood, M. A Systematic Review of Duplex Ultrasound, Magnetic Resonance Angiography and Computed Tomography Angiography for the Diagnosis and Assessment of Symptomatic, Lower Limb Peripheral Arterial Disease. Health Technol. Assess. Winch. Engl. 2007, 11, 1–184. [Google Scholar] [CrossRef] [PubMed]
- Vlachopoulos, C.; Georgakopoulos, C.; Koutagiar, I.; Tousoulis, D. Diagnostic Modalities in Peripheral Artery Disease. Curr. Opin. Pharmacol. 2018, 39, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Met, R.; Bipat, S.; Legemate, D.A.; Reekers, J.A.; Koelemay, M.J.W. Diagnostic Performance of Computed Tomography Angiography in Peripheral Arterial Disease: A Systematic Review and Meta-Analysis. JAMA 2009, 301, 415–424. [Google Scholar] [CrossRef]
- ESUR Guidelines 10. Available online: https://www.esur.org/wp-content/uploads/2022/03/esur-guidelines-10_0-final-version.pdf (accessed on 1 October 2022).
- Parillo, M.; Vaccarino, F.; Beomonte Zobel, B.; Quattrocchi, C.C. A Rare Case of Contained Chronic Rupture of Abdominal Aortic Aneurysm Associated With Vertebral Erosion: Pre- and Post-Operative Findings on Computed Tomography and a Narrative Review. Vasc. Endovasc. Surg. 2022, 56, 15385744221108040. [Google Scholar] [CrossRef] [PubMed]
- Menke, J.; Larsen, J. Meta-Analysis: Accuracy of Contrast-Enhanced Magnetic Resonance Angiography for Assessing Steno-Occlusions in Peripheral Arterial Disease. Ann. Intern. Med. 2010, 153, 325–334. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parillo, M.; De Stefano, D.; Catanese, V.; Mallio, C.A.; Spinelli, F.; Stilo, F.; Quattrocchi, C.C. Conversion of Femoral-Tibial Bypass Surgery into Deep Vein Arterialization in a Patient with Severe Peripheral Artery Disease: Post-Operative Computed Tomography and Angiography Findings. Hearts 2023, 4, 12-19. https://doi.org/10.3390/hearts4010002
Parillo M, De Stefano D, Catanese V, Mallio CA, Spinelli F, Stilo F, Quattrocchi CC. Conversion of Femoral-Tibial Bypass Surgery into Deep Vein Arterialization in a Patient with Severe Peripheral Artery Disease: Post-Operative Computed Tomography and Angiography Findings. Hearts. 2023; 4(1):12-19. https://doi.org/10.3390/hearts4010002
Chicago/Turabian StyleParillo, Marco, Domenico De Stefano, Vincenzo Catanese, Carlo Augusto Mallio, Francesco Spinelli, Francesco Stilo, and Carlo Cosimo Quattrocchi. 2023. "Conversion of Femoral-Tibial Bypass Surgery into Deep Vein Arterialization in a Patient with Severe Peripheral Artery Disease: Post-Operative Computed Tomography and Angiography Findings" Hearts 4, no. 1: 12-19. https://doi.org/10.3390/hearts4010002
APA StyleParillo, M., De Stefano, D., Catanese, V., Mallio, C. A., Spinelli, F., Stilo, F., & Quattrocchi, C. C. (2023). Conversion of Femoral-Tibial Bypass Surgery into Deep Vein Arterialization in a Patient with Severe Peripheral Artery Disease: Post-Operative Computed Tomography and Angiography Findings. Hearts, 4(1), 12-19. https://doi.org/10.3390/hearts4010002








