Abstract
Chronic obstructive pulmonary disease (COPD) is a global public health burden that stands out as a leading cause of mortality around the world, especially in less developed countries. COPD treatment should be centered on the individual necessities of each patient, integrating pharmacological therapy, immunization, nutritional support, pulmonary rehabilitation and control of comorbidities. Combining a long-acting antimuscarinic (LAMA) with a long-acting beta2-agonist (LABA) bronchodilator has proven to be more effective than monotherapy with LABA or LAMA, in terms of the functional improvement of forced expiratory volume (FEV1), symptoms and life quality and may be helpful in patients with progressive dyspnea. The eosinophil blood count is a simple biomarker that could guide personalized treatment strategies by identifying patients with greater clinical benefits of inhaled corticosteroid (ICS) treatment. However, one critical concern is the increased risk of pneumonia in individuals treated with ICS.
Chronic obstructive pulmonary disease (COPD) is a complex disorder characterized by pulmonary and systemic dysfunctions that affected approximately 384 million people worldwide in 2020 [1]. According to the World Health Organization data, COPD represents a public health challenge that is intimately related to smoking, occupational exposure and exposure to biomass combustion [2]. COPD is associated with a substantial socioeconomic burden and stands out as a leading cause of mortality around the world, especially in less developed countries [3]. However, notable progress has been achieved to reduce smoking prevalence worldwide. Additionally, with a better understanding of the pathophysiology and the molecular basis of the disease, treatment can be more effective and tailored to a patient’s phenotype. In this context, peripheral blood eosinophils have shown to be a low-cost and accessible tool to guide COPD pharmacological treatment [4]. Evidence suggests that the eosinophil blood count can be a trustworthy marker to identify phenotypes that are more or less likely to benefit from treatment with inhaled corticosteroids (ICSs) [5].
COPD treatment should be centered on the individual necessities of each patient, integrating pharmacological therapy, immunization, nutritional support, pulmonary rehabilitation and control of comorbidities. These interventions aim to minimize the impact of symptoms on life quality and prevent exacerbations, accelerated functional decline and mortality.
Combining bronchodilators with different action mechanisms could be an effective way to reduce symptoms and increase the potential of bronchodilation, with less risk of adverse effects than increasing the bronchodilator dose in isolation [3]. The use of long-acting antimuscarinic (LAMA) together with long-acting beta2-agonist (LABA) bronchodilators has proven to be more effective than monotherapy with LABA or LAMA, in terms of the functional improvement of forced expiratory volume (FEV1), symptoms and life quality, as well as maintaining the effectiveness of the bronchodilator over a longer period of time [6]. These finding have been replicated in different populations and ethnic groups [7,8].
It is known that progressive dyspnea is the principal factor for incapacity and reduced life quality in patients with COPD [9]. During exercise, airflow obstruction and reduced pulmonary elastic retraction favor an incremental increase in residual volume, with the concomitant flattening of the inspiratory capacity (IC) [10]. As illustrated in Figure 1, bronchodilation therapy is the first-line treatment option for the control of dyspnea, with potential benefits employing the LABA/LAMA combination in patients that are in a more serious condition or in individuals undergoing monotherapy with persistent symptoms [11]. Recent studies have shown the superiority of the LABA/LAMA combination for significant improvement in pulmonary function (IC and FEV1) when compared to a placebo and monotherapy with both drugs administered individually, as well as reducing hyperinsufflation [12,13].
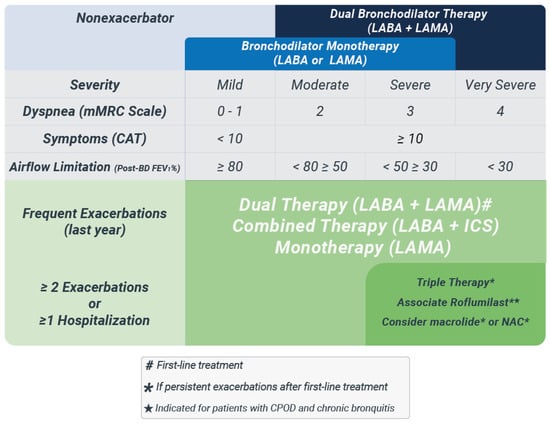
Figure 1.
Bronchodilator therapy with potential benefits for COPD patients—blue zone: patients without frequent exacerbations; green zone: frequent exacerbation phenotype. LABA: long-acting β2-agonist; LAMA: long-acting antimuscarinic; mMRC: modified Medical Research Council dyspnea scale; CAT: COPD assessment test; FEV1%: forced expiratory volume predicted; BD: bronchodilator; ICS: inhaled corticosteroids; NAC: N-acetylcysteine. Adapted from Fernandes FLA et al., 2017 [11].
There is an intense ongoing debate concerning the ideal eosinophil limits to serve as the basis for the indication of inhaled corticosteroids (ICSs) in stable COPD. The eosinophil blood (EOS) count is a simple and reasonably reproducible tool that should only be used therapeutically after taking into consideration individual exacerbating risk factors (severity, hospitalizations and previous exacerbations). Elevated eosinophil concentrations have been positively associated with a higher exacerbation risk in COPD patients [14]. However, one critical concern is the increased risk of pneumonia, oral candidiasis and hoarseness in COPD patients treated with ICSs [15]. Subgroups with an increased risk of pneumonia include patients with a previous pneumonia history, aged above 55, BMI < 25, current smokers and individuals with advanced disease and greater airflow limitations [16].
According to the Global Obstructive Lung Disease Initiative (GOLD), ongoing treatment with corticosteroids offers few clinical benefits in individuals with an EOS count of less than 100 cells/microliter. Patients with EOS > 300 represent the subgroup with the highest probable benefit, while the clinical response of the 100–300 EOS interval continues to be variable and uncertain [3]. The adequate classification of eosinophilic/noneosinophilic phenotypes allows for personalized treatment strategies by identifying patients with greater potential clinical benefits and avoiding unnecessary adverse effects [17].
A recent European Respiratory Society (ERS) guideline published in 2020 put forward objective criteria for the conscientious use of ICSs in the treatment of COPD. In patients without a frequent history of exacerbation, usually defined as one or two exacerbations per year, there is a conditional recommendation to consider the suspension of ICSs in favor of ongoing therapy with one or two bronchodilators [18]. The panel also opposed the suspension of ICS in patients with EOS > 300 cells/microliter, with or without a previous history of frequent exacerbations. For patients with EOS < 300, there was no formal recommendation concerning the suspension of ICS for a lack of conclusive evidence [18]. If there is to be an interruption, it should be abrupt, without the need for gradual weaning. The principle recommendations are summarized in Figure 2.
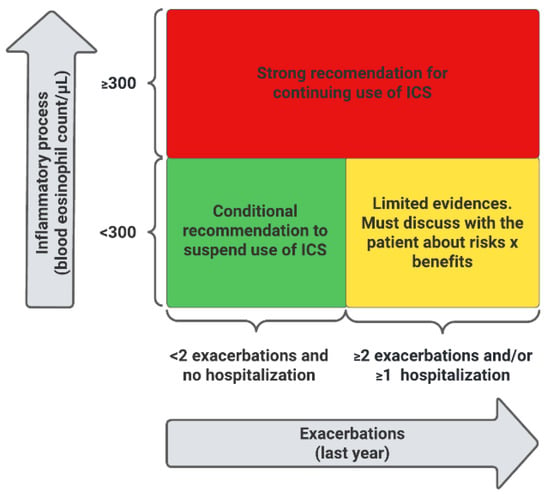
Figure 2.
ICS treatment in COPD patients. Red zone: ICS use is recommended; yellow zone: controversial use of ICS; green zone: consider withdrawing ICS. ICS: inhaled corticosteroids. Adapted from Chalmers JD et al., 2020 [18].
In summary, symptoms management, and the prevention of functional decline and exacerbations are fundamental objectives in the effective treatment of COPD. Bronchodilator therapy together with LABA/LAMA shows superiority in the control of dyspnea, improved life quality and a reduction in hyperinsufflation in comparison to monotherapy with an isolated bronchodilator. Patients with EOS > 300 represent the subgroup with the greatest potential clinical benefits. Therefore, inhaled corticosteroids should be considered in COPD patients with eosinophilic phenotypes and/or with a high clinical risk of exacerbations.
Author Contributions
Conceptualization: R.G.F., J.d.B.J.; Supervision: J.d.B.J.; Visualization: R.G.F., L.F.A.; Writing–original draft: R.G.F., L.F.A., J.d.B.J.; Writing–review & editing: R.G.F., L.F.A., J.d.B.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
RGF participated in educational meetings funded by AstraZeneca, Boehringer Ingelheim, Chiesi and GlaxoSmithKline.
References
- Queiroz, C.F.; Lemos, A.C.M.; Bastos, M.D.L.S.; Neves, M.C.L.C.; Camelier, A.A.; Carvalho, N.; De Carvalho, E.M. Inflammatory and immunological profiles in patients with COPD: Relationship with FEV 1 reversibility. J. Bras. Pneumol. 2016, 42, 241–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pauwels, R.A.; Buist, A.S.; Ma, P.; Jenkins, C.R.; Hurd, S.S.; GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: National Heart, Lung, and Blood Institute and World Health Or-ganization Global Initiative for Chronic Obstructive Lung Disease (GOLD): Executive summary. Respir. Care 2001, 46, 798–825. [Google Scholar] [PubMed]
- Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2021. Available online: https://goldcopd.org/ (accessed on 10 May 2021).
- Cheng, S.-L. Blood eosinophils and inhaled corticosteroids in patients with COPD: Systematic review and meta-analysis. Int. J. Chron. Obstr. Pulm. Dis. 2018, 13, 2775–2784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eltoboli, O.; Mistry, V.; Barker, B.; Brightling, C. Relationship between blood and bronchial submucosal eosinophilia and reticular basement membrane thickening in chronic obstructive pulmonary disease. Respirology 2015, 20, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Guía de Práctica Clínica Latinoamericana de EPOC—ALAT Basada en evidencia, Asociación Latinoamericana de Tórax 2019. Available online: https://alatorax.org/ (accessed on 10 May 2021).
- Rodrigo, G.J.; Price, D.; Anzueto, A.; Singh, D.; Altman, P.; Bader, G.; Patalano, F.; Fogel, R.; Kostikas, K. LABA/LAMA combinations versus LAMA monotherapy or LABA/ICS in COPD: A systematic review and meta-analysis. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 907–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrecheguren, M.; Monteagudo, M.; Miravitlles, M. Population-based study of LAMA monotherapy effectiveness compared with LABA/LAMA as ini- tial treatment for COPD in primary care. Prim. Care Respir. Med. 2018, 28, 36. [Google Scholar] [CrossRef] [PubMed]
- Nici, L.; Donner, C.; Wouters, E.; Zuwallack, R.; Ambrosino, N.; Bourbeau, J.; Carone, M.; Celli, B.; Engelen, M.; Fahy, B.; et al. American Thoracic Society/European Respiratory Society Statement on Pulmonary Rehabilitation. Am. J. Respir. Crit. Care Med. 2006, 173, 1390–1413. [Google Scholar] [CrossRef] [PubMed]
- Diaz, O.; Villafranca, C.; Ghezzo, H.; Borzone, G.; Leiva, A.; Milic-Emil, J.; Lisboa, C. Role of inspiratory capacity on exercise tolerance in COPD patients with and without tidal expiratory flow limitation at rest. Eur. Respir. J. 2000, 16, 269–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandes, F.L.; Cukier, A.; Camelier, A.A.; Fritscher, C.C.; Costa, C.H.; Pereira, E.D.; Godoy, I.; Cançado, J.E.; Romaldini, J.G.; Chatkin, J.M.; et al. Recommendations for the pharmaco-logical treatment of COPD: Questions and answers. J. Bras. Pneumol. 2017, 43, 290–301. [Google Scholar] [CrossRef]
- O’Donnell, D.E.; Casaburi, R.; Frith, P.; Kirsten, A.; De Sousa, D.; Hamilton, A.; Xue, W.; Maltais, F. Effects of combined tiotropium/olodaterol on inspiratory capacity and exercise endurance in COPD. Eur. Respir. J. 2017, 49, 1601348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buhl, R.; Maltais, F.; Abrahams, R.; Bjermer, L.; Derom, E.; Ferguson, G.; Fležar, M.; Hébert, J.; McGarvey, L.; Pizzichini, E.; et al. Tiotropium and olodaterol fixed-dose combinationversusmono-components in COPD (GOLD 2–4). Eur. Respir. J. 2015, 45, 969–979. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, M.C.; Yeung, Y.C.; Yu, E.L.M.; Yu, W.C. Blood Eosinophil and Risk of Exacerbation in Chronic Obstructive Pulmonary Disease Patients: A Retrospective Cohort Analysis. Int. J. Chronic Obstr. Pulm. Dis. 2020, 15, 2869–2877. [Google Scholar] [CrossRef] [PubMed]
- Yang, I.A.; Clarke, M.S.; Sim, E.H.A.; Fong, K.M. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database System. Rev. 2012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crim, C.; Dransfield, M.T.; Bourbeau, J.; Jones, P.W.; Hanania, N.A.; Mahler, D.A.; Vestbo, J.; Wachtel, A.; Martinez, F.J.; Barnhart, F.; et al. Pneumonia Risk with Inhaled Fluticasone Furoate and Vilanterol Compared with Vilanterol Alone in Patients with COPD. Ann. Am. Thorac. Soc. 2015, 12, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Zeiger, R.S.; Tran, T.N.; Butler, R.K.; Schatz, M.; Li, Q.; Khatry, D.B.; Martin, U.; Kawatkar, A.A.; Chen, W. Relationship of Blood Eosinophil Count to Exacerbations in Chronic Obstructive Pulmonary Disease. J. Allergy Clin. Immunol. Pract. 2018, 6, 944–954.e5. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, J.D.; Laska, I.F.; Franssen, F.M.E.; Janssens, W.; Pavord, I.; Rigau, D.; McDonnell, M.J.; Roche, N.; Sin, D.D.; Stolz, D.; et al. Withdrawal of inhaled corticosteroids in COPD: A European Respiratory Society guideline. Eur. Respir. J. 2020, 55, 2000351. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).