1. Introduction
One of the most revolutionary breakthroughs in the world of refractive surgery has been the use of the laser in situ keratomileusis (LASIK) technique. LASIK surgery is widely used in the correction of refractive errors and involves the creation of an anterior lamella or flap, followed by stromal photoablation using an excimer laser [
1]. The creation of this flap is an important step in the surgical procedure and can be performed by a mechanical microkeratome or more recently using a femtosecond laser (FS laser). The FS laser aims to improve the predictability of refractive surgery and avoid its complications [
2,
3]. It is well known that LASIK surgery induces high-order aberrations (HOA) that can produce night vision problems, such as halos, glare and deterioration of contrast function [
4,
5]. The main eye element involved in the generation of such aberrations is the first corneal surface [
6,
7,
8], with the contribution of the second corneal surface being minimal and not significant as many authors reported [
9]. Scientific literature has shown that myopic LASIK refractive surgery treatment produces a change in corneal asphericity, making it more positive [
10], and this change is directly correlated with an increment of the spherical aberration. Furthermore, other high-order aberrations such as coma are increased after LASIK surgery [
8,
11].
An important criterion to assess the success of the surgery is the efficacy index defined as the ratio of mean postoperative uncorrected distance vision (UDVA) to the mean preoperative corrected distance vision (CDVA). LASIK surgery has been demonstrated to be a safe and effective surgery. Thus, when comparing preoperative CDVA and postoperative UDVA, both values are similar and close to 1 [
11,
12,
13,
14] on the decimal scale. These results are to some extent contradicted by the fact that high-order aberrations are significantly increased after surgery. An impairment of visual acuity should be expected resulting in an efficacy index clearly below unity.
This study aims to understand the real effect of the aberrations increment after LASIK surgery on the final patient visual quality, specifically when the visual acuity measurement is considered. For this purpose, a clinical study and different personalized eye model simulations are performed. In clinical study, correlations between pre- and postoperative parameters with visual acuity are analyzed. Similarly, eye simulations (based on topographic and biometric data of real patients) provide an insight of the quality of vision before and after surgery.
4. Discussion
Our clinical results showed that differences between preoperative and postoperative values of anterior corneal radius, asphericity or pachymetry were significant (
p < 0.05), as reported in previous studies [
4,
12,
14,
15,
21,
22,
23]. Despite the change of the posterior corneal radius was also significant, it could not be considered clinically relevant because the mean difference was about 0.02 mm [
10]. The anterior corneal surface was the most relevant surface in the generation of the aberrations after surgery. HOAS RMS, SA and RMS coma were significantly increased after surgery (
p < 0.05) in agreement with published studies [
6,
7,
9,
24]. The contribution to global aberrations from the second corneal surface was not clinically significant as previous reported results [
4,
12,
25]. Study of correlations showed that asphericity, SA, RMS coma and HOAS RMS increased as the pre-surgery spherical equivalent was higher consistent with previously published studies [
23,
26,
27,
28].
Optical aberrations are associated with bad quality of vision, with one of the main causes being a large mesopic pupil diameter (>6 mm) [
29,
30]. Several studies have shown that Femto-Lasik technique is an effective technique [
12,
13,
14,
15] and these results imply that no differences are expected between the preoperative CDVA and the postoperative UDVA after Femto-Lasik surgery. Our study corroborated this statement. However, if a significant increase of aberrations after surgery was obtained, more differences between the preoperative CDVA and the postoperative UDVA would be expected, and a lower efficacy index should be obtained. This absence of differences in vision quality was confirmed with our clinical results as cumulative percentages of eyes with better postoperative UDVA showed (
Figure 2). As this study established, two factors are key to understanding the lack of correlation between vision quality and increased aberrations: the pupil size and a personalized analysis of each case.
Although several studies have been conducted to assess the aberrations induced by different LASIK techniques, there are no consensus results regarding the changes in individual aberration terms [
26]. As indicated by Al-Zeraid et al., the differences between previous reports may be related to the different levels of preoperative aberrations and the pupil analysis diameter used. So far, no literature has been found to question why there is no direct correlation between objective worsening of visual quality and clinical measure of visual acuity after surgery. As commented above, the pupil size commonly used to obtain aberrations is 6 mm [
12,
13,
14,
15]; however, VA is measured under photopic conditions as stablished the ETDRS study protocol [
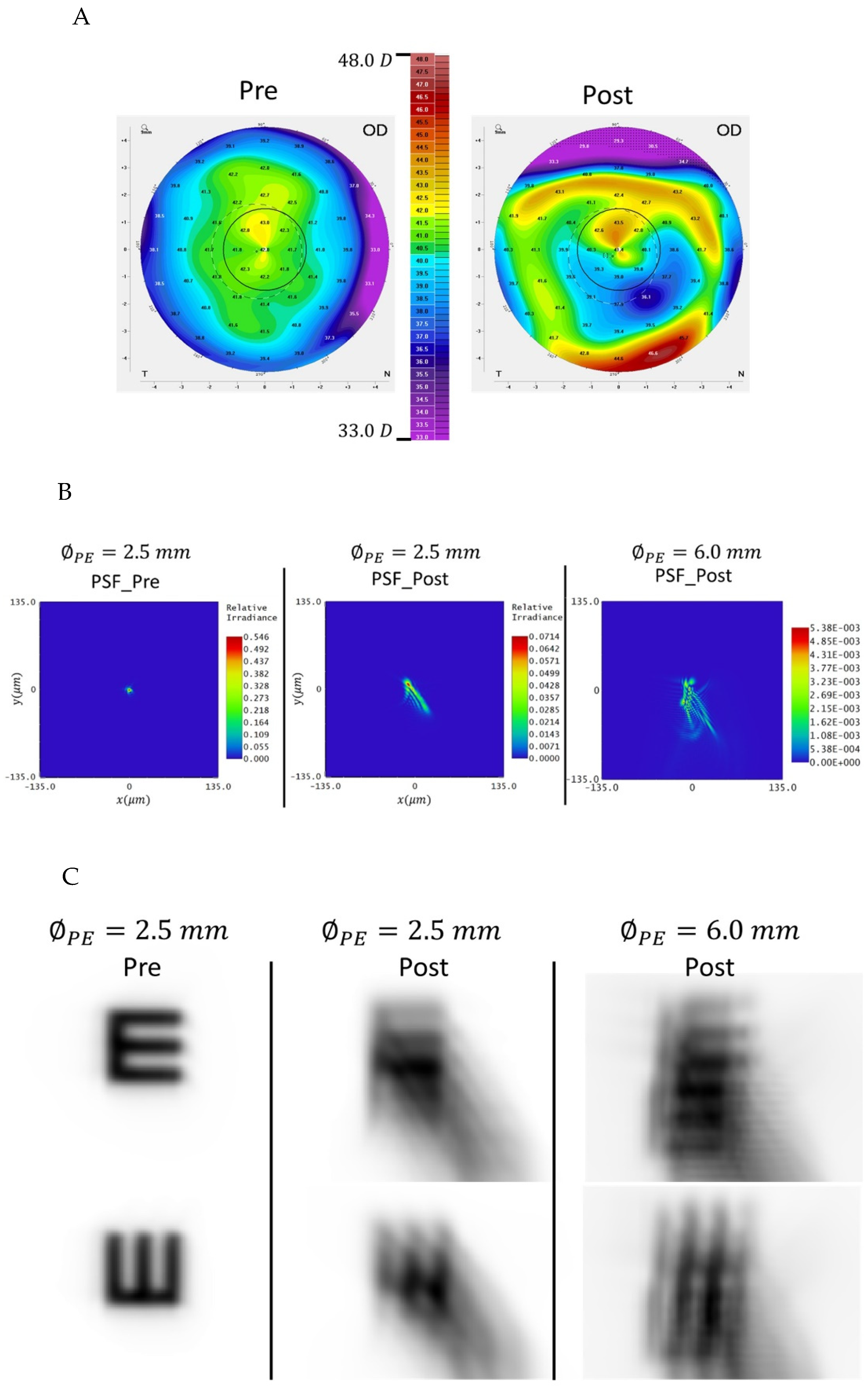
30]. At these illumination levels, normal pupils have lower diameters than 6 mm. Assuming an average photopic pupil size of 2.5 mm and recalculating the value of the aberrations for this diameter, it is possible to explain why the preoperative CDVA and postoperative UDVA are correlated. For this purpose, three eyes, which represent most of the possible relationships between preoperative CDVA and postoperative UCVA, were simulated. Eye 1 had the same preoperative CDVA and postoperative UDVA an equal to 1, in Eye 2 the VA after surgery became better than before surgery (CDVA = 1 and UDVA = 1.25 respectively) and in Eye 3 there was a worsening of VA after surgery (preoperative CDVA = 1 and postoperative UDVA = 0.7).
Our simulations showed that for the pupil size of 6 mm, the three eyes increased HOAS after surgery and vision quality was impaired (
Figure 4,
Figure 5 and
Figure 6) following the general trend of the clinical study. However, clinical measurement of VA did not correlate with this result because postoperative UDVA was not always worse than preoperative CDVA. This correlation between clinical VA measurement and HOAS was found when a 2.5 mm pupil size was considered. The results justified that for Eye 1 the preoperative CDVA and postoperative UDVA were practically identical, for Eye 2 the postoperative UDVA was better and for Eye 3 worse (
Figure 4,
Figure 5 and
Figure 6). As seen in
Table 4,
Table 5 and
Table 6, for the 2.5 mm pupil size, in Eyes 1 and 2, HOAS diminished after surgery, whereas in Eye 3 it increased.
Most of eyes from clinical base data (33) obtained a postoperative VA 1 or close to one and only 4 eyes obtained VA lower than 0.8. In these 4 eyes, the postoperative HOAS was higher than 0.06 µm. We have seen that a postoperative VA equal to or better than preoperative VA is associated with a maintenance or improvement of postoperative HOAS aberrations for a pupil size of 2.5 mm (i.e., Eyes 1 and 2). In addition, in those eyes which HOAS were higher than 0,06 µm and the increase of HOAS after surgery was higher than 0,03 µm (i.e., Eye 3), a lower postoperative VA were expected. However, the amount of this decrease in VA depends on the specific distribution of the aberrations.
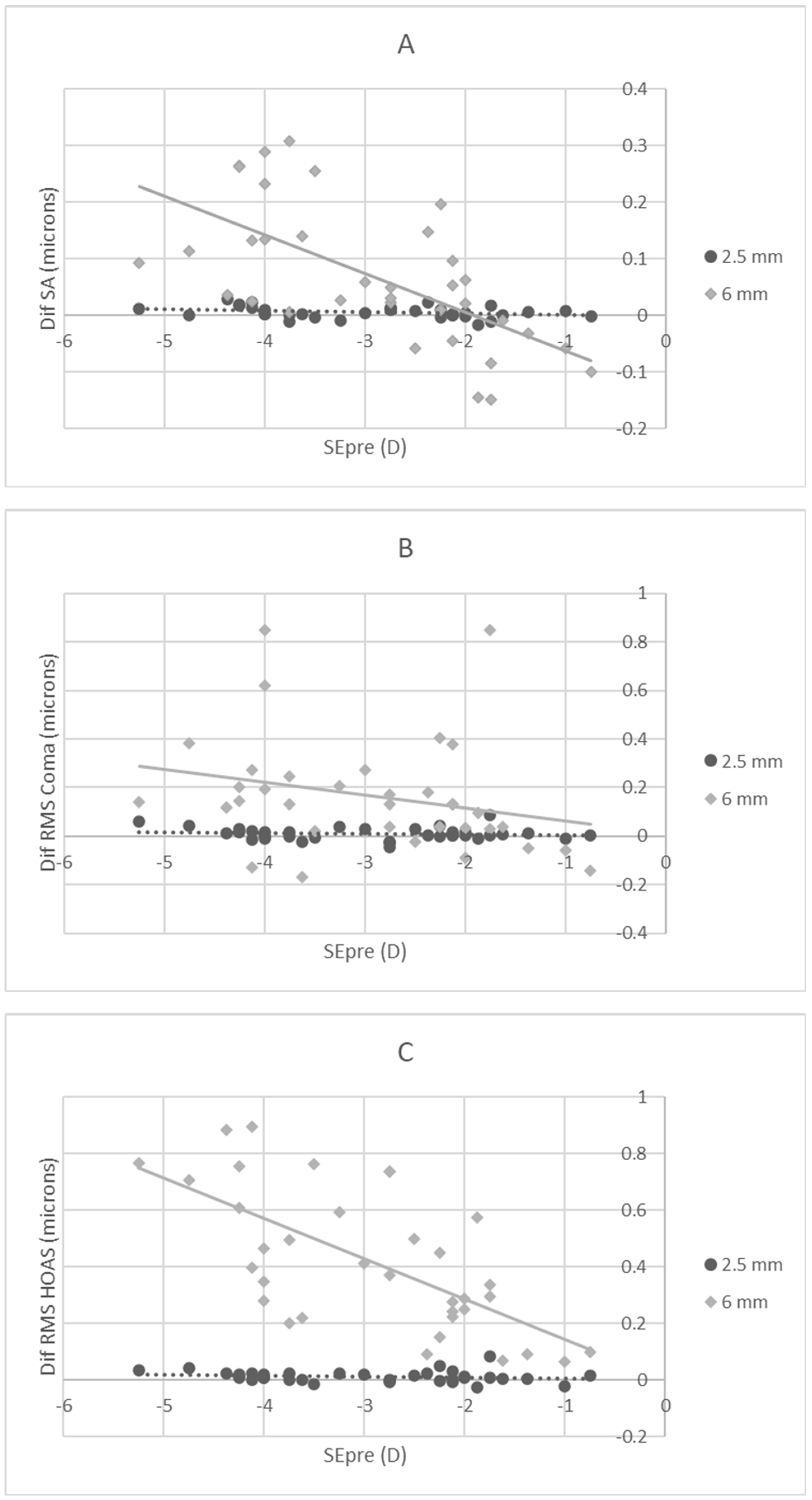
To corroborate these conclusions, correlations were studied for 2.5 mm pupil size.
Table 7 showed that only correlation between SE and SA was significant, but as seen in
Figure 7A, this correlation was not clinically relevant because the values were very low and always close to 0. In addition, differences in coma and RMS HOAS were not significant (see
Table 7 and
Figure 7B,C). This lack of correlations explains why HOAS were not influencing the final patients vision quality and any differences between preoperative CDVA and postoperative UDVA were found. Moreover, this result reinforces the idea that it is necessary a personalized analysis for each patient to find the correlation between the HOAS and the final vision quality (as the three analysed cases have shown).
This study has shown that considering a photopic pupil size (lower than 3 mm) in the analysis of aberrations is key to better understanding the patients final vision quality. In most cases there are not correlation between the change of visual acuity before and after surgery when only the change of HOAS for 6 mm of pupil size is considered. Visual acuity is measured under photopic luminance, and the postoperative VA are determined by the final HOAS and the increment of them after surgery, but for 2.5 mm of pupil size. Our results indicated that HOAS higher than 0.06 µm are likely to produce VA values lower than 1 and, if in addition, the increment of the HOA after surgery is higher than 0.03 µm, a worsening of AV (Eye 3). Although our study has only been simulated on three eyes, the results could be extrapolated to most real cases since the effect of high-order aberrations (basically SA and coma) will produce the same effect on the final quality of vision. Although the simulation could be improved by considering total aberrations of the eye for a better personalized lens model, this assumption does not invalidate our results because we have focused on photopic conditions. We have considered a diameter of 2.5 mm in the entrance pupil plane which would correspond to a smaller beam size in the lens plane. Therefore, our model provides a sufficiently good behavior of the photopic conditions. In addition, the need of total ocular aberrations will lead to clinical drawbacks because the use of aberrometers is not widespread in clinical practice. Specifically, refractive surgery usually only takes into account the corneal measurement. Consequently, our study can be useful to a wider audience since corneal aberrations are easier to obtain.
In conclusion, the personalized analysis of higher order aberrations for photopic pupil sizes will better predict the patient’s final visual acuity post-Lasik surgery.