Prophylactic Corneal Cross-Linking in Myopic Femtosecond Laser-Assisted In Situ Keratomileusis: Long-Term Visual and Refractive Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Ethical Aspects
2.3. Subjects
2.4. Preoperative Examinations
2.5. Surgical Technique
2.5.1. Corneal Cross-Linking
2.5.2. Postoperative Evaluation
2.6. Statistical Analysis
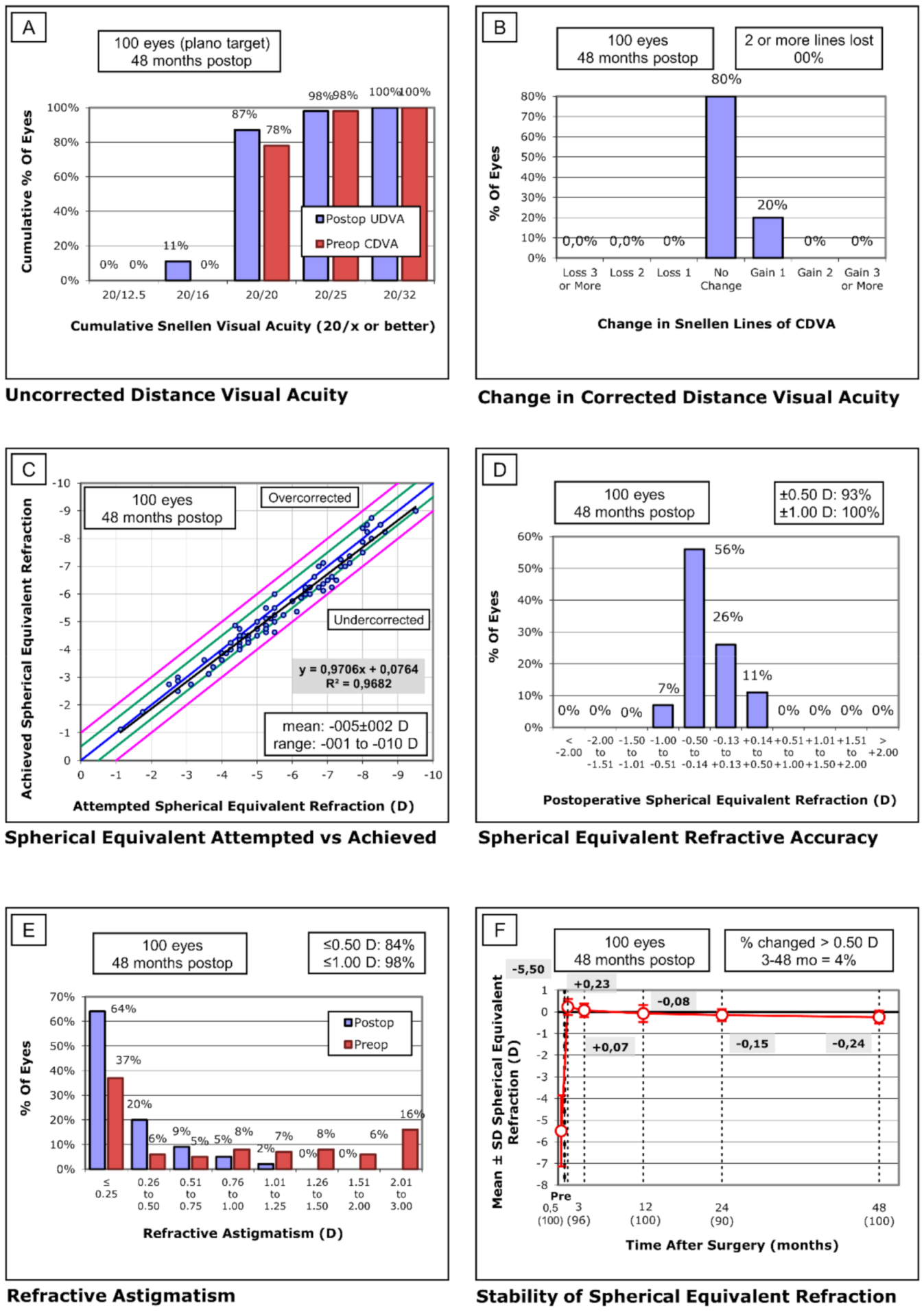
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wen, D.; McAlinden, C.; Flitcroft, I.; Tu, R.; Wang, Q.; Alió, J.; Marshall, J.; Huang, Y.; Song, B.; Hu, L.; et al. Postoperative Efficacy, Predictability, Safety, and Visual Quality of Laser Corneal Refractive Surgery: A Network Meta-analysis. Am. J. Ophthalmol. 2017, 178, 65–78. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.C.Y.; Ng, A.L.K.; Chan, K.K.W.; Cheng, G.P.M.; Wong, I.Y.H.; Jhanji, V. Combined application of prophylactic corneal cross-linking and laser in-situ keratomileusis—A review of literature. Acta Ophthalmol. 2017, 95, 660–664. [Google Scholar] [CrossRef]
- Randleman, J.B.; Trattler, W.B.; Stulting, R.D. Validation of the Ectasia Risk Score System for Preoperative Laser in Situ Keratomileusis Screening. Am. J. Ophthalmol. 2008, 145, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Rodríguez-Vallejo, M.; Piñero, D.P. Tomographic and biomechanical index (TBI) for screening in laser refractive surgery. J. Refract. Surg. 2019, 35, 398. [Google Scholar] [CrossRef] [PubMed]
- Ambrósio, R. Post-LASIK Ectasia: Twenty Years of a Conundrum. Semin. Ophthalmol. 2019, 34, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.W.L.; Lim, L. Review of Laser Vision Correction (LASIK, PRK and SMILE) with Simultaneous Accelerated Corneal Crosslinking–Long-term Results. Curr. Eye Res. 2019, 44, 1171–1180. [Google Scholar] [CrossRef]
- Spörl, E.; Huhle, M.; Kasper, M.; Seiler, T. Erhöhung der festigkeit der hornhaut durch vernetzung. Ophthalmologe 1997, 94, 902–906. [Google Scholar] [CrossRef] [PubMed]
- Celik, H.U.; Alagöz, N.; Yildirim, Y.; Agca, A.; Marshall, J.; Demirok, A.; Yilmaz, O.F. Accelerated corneal crosslinking concurrent with laser in situ keratomileusis. J. Cataract Refract. Surg. 2012, 38, 1424–1431. [Google Scholar] [CrossRef]
- Wollensak, G.; Hammer, C.M.; Spörl, E.; Klenke, J.; Skerl, K.; Zhang, Y.; Sel, S. Biomechanical efficacy of collagen crosslinking in porcine cornea using a femtosecond laser pocket. Cornea 2014, 33, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Kampik, D.; Ralla, B.; Keller, S.; Hirschberg, M.; Friedl, P.; Geerling, G. Influence of corneal collagen crosslinking with riboflavin and ultraviolet-a irradiation on excimer laser surgery. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3929–3934. [Google Scholar] [CrossRef][Green Version]
- Chan, T.C.Y.; Yu, M.C.Y.; Ng, A.L.K.; Cheng, G.P.M.; Zhang, J.; Wang, Y.; Jhanji, V. Short-term variance of refractive outcomes after simultaneous LASIK and high-fluence cross-linking in high myopic correction. J. Refract. Surg. 2016, 32, 664–670. [Google Scholar] [CrossRef]
- Kanellopoulos, A.J.; Asimellis, G. Combined laser in situ keratomileusis and prophylactic high-fluence corneal collagen crosslinking for high myopia: Two-year safety and efficacy. J. Cataract Refract. Surg. 2015, 41, 1426–1433. [Google Scholar] [CrossRef] [PubMed]
- Kanellopoulos, J.; Asimellis, G.; Karabatsas, C. Comparison of prophylactic higher fluence corneal cross-linking to control, in myopic LASIK, one year results. Clin. Ophthalmol. 2014, 2373. [Google Scholar] [CrossRef]
- Seiler, T.G.; Fischinger, I.; Koller, T.; Derhartunian, V.; Seiler, T. Superficial corneal crosslinking during laser in situ keratomileusis. J. Cataract Refract. Surg. 2015, 41, 2165–2170. [Google Scholar] [CrossRef] [PubMed]
- Tomita, M.; Yoshida, Y.; Yamamoto, Y.; Mita, M.; Waring IV, G. In vivo confocal laser microscopy of morphologic changes after simultaneous LASIK and accelerated collagen crosslinking for myopia: One-year results. J. Cataract Refract. Surg. 2014, 40, 981–990. [Google Scholar] [CrossRef]
- Kanellopoulos, A.J. Long-term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusis. Clin. Ophthalmol. 2012, 6, 1125–1130. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tan, J.; Lytle, G.E.; Marshall, J. Consecutive laser in situ keratomileusis and accelerated corneal crosslinking in highly myopic patients: Preliminary results. Eur. J. Ophthalmol. 2014, 25, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Kohnen, T.; Lwowski, C.; Hemkeppler, E.; De’Lorenzo, N.; Petermann, K.; Forster, R.; Herzog, M.; Böhm, M. Comparison of Femto-LASIK with Combined Accelerated Cross-linking to Femto-LASIK in High Myopic Eyes: A Prospective Randomized Trial. Am. J. Ophthalmol. 2020, 211, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Tian, L.; Wang, L.Q.; Huang, Y.F. Efficacy and Safety of LASIK Combined with Accelerated Corneal Collagen Cross-Linking for Myopia: Six-Month Study. BioMed Res. Int. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Bradley Randleman, J.; Santhiago, M.R.; Kymionis, G.D.; Hafezi, F. Corneal cross-linking (CXL): Standardizing terminology and protocol nomenclature. J. Refract. Surg. 2017, 33, 727–729. [Google Scholar] [CrossRef]
- Ng, A.L.K.; Kwok, P.S.K.; Wu, R.T.K.; Jhanji, V.; Woo, V.C.P.; Chan, T.C.Y. Comparison of the Demarcation Line on ASOCT after Simultaneous LASIK and Different Protocols of Accelerated Collagen Crosslinking: A Bilateral Eye Randomized Study. Cornea 2017, 36, 74–77. [Google Scholar] [CrossRef] [PubMed]
- Taneri, S.; Kiessler, S.; Rost, A.; Dick, H.B. Corneal ectasia after LASIK combined with prophylactic corneal cross-linking. J. Refract. Surg. 2017, 33, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Kanellopoulos, A.J.; Asimellis, G.; Salvador-Culla, B.; Chodosh, J.; Ciolino, J.B. High-irradiance CXL combined with myopic LASIK: Flap and residual stroma biomechanical properties studied ex-vivo. Br. J. Ophthalmol. 2015, 99, 870–874. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Variable |
|---|---|
| Treatment target | Prophylaxis |
| Fluence (total) (J/cm2) | 2.7 |
| Soak time (s) | 90 |
| Intensity (mW) | 30 |
| Treatment time (seconds) | 90 |
| Epithelium status | On (Flap folded) |
| Chromophore | Riboflavin (Vibex Rapid Avedro) |
| Chromophore carrier | Balanced Salt Solution |
| Chromophore osmolarity | Iso-Osmolar |
| Chromophore concentration | 0.25% |
| Light source | UVA (KXL System, Avedro) |
| Irradiation mode (interval) | Continuous |
| Protocol modifications | None |
| Protocol abbreviation in manuscript | Prophylactic CXL |
| Author | Year | Corneal CXL | LASIK | Eyes | Follow-up | Efficacy | Safety | Predictability |
|---|---|---|---|---|---|---|---|---|
| Celik et al. [8] | 2012 | Avedro | MK and Schwind | 4 | 12 | 75%/1.06 | 0%/0% | 100%/100% |
| Kanellopoulus [16] | 2012 | Priavision | FS and Wavelight | 43 | 42 | 83.7%/1.09 | 0%/0% | - |
| Tomita et al. [15] | 2014 | Avedro | FS and Schwind | 24 | 12 | 100%/0.99 | 21.7%/0% | 95.7%/95.7% |
| Kanellopoulus et al. [13] | 2014 | Avedro | FS and Wavelight | 73 | 12 | 90.4%/- | 0%/0% | 91.8%/100% |
| Seiler et al. [14] | 2015 | UVX 2000 | FS and Wavelight | 76 | 12 | NR | 0%/0% | ≈85%/≈95% |
| Kanellopoulus et al. [12] | 2015 | Avedro | FS and Wavelight | 65 | 24 | 93.8%/- | 0%/0% | 92.3%/100% |
| Tan et al. [17] | 2015 | Avedro | FS and Schwind | 70 | 3 | 78%/- | 17%/0% | 100%/100% |
| Chang et al. [11] | 2016 | Avedro | FS and Allegretto | 60 | 6 | 86.7%/0.91 | ≈5%/0% | 96%/98% |
| Wu et al. [19] | 2016 | Avedro | FS and Wavelight | 96 | 6 | 87.5%/1.02 | 2%/2% | -/95.83% |
| Kohnen et al. [18] | 2020 | Avedro | FS and Schwind | 26 | 12 | 78%/- | 17%/0% | 87%/91% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso-Aliste, F.; Amián-Cordero, J.; Rachwani-Anil, R.; De-Hita-Cantalejo, C.; Borroni, D.; Rocha-de-Lossada, C.; Sánchez-González, J.-M. Prophylactic Corneal Cross-Linking in Myopic Femtosecond Laser-Assisted In Situ Keratomileusis: Long-Term Visual and Refractive Outcomes. Optics 2021, 2, 55-62. https://doi.org/10.3390/opt2010006
Alonso-Aliste F, Amián-Cordero J, Rachwani-Anil R, De-Hita-Cantalejo C, Borroni D, Rocha-de-Lossada C, Sánchez-González J-M. Prophylactic Corneal Cross-Linking in Myopic Femtosecond Laser-Assisted In Situ Keratomileusis: Long-Term Visual and Refractive Outcomes. Optics. 2021; 2(1):55-62. https://doi.org/10.3390/opt2010006
Chicago/Turabian StyleAlonso-Aliste, Federico, Jonatan Amián-Cordero, Rahul Rachwani-Anil, Concepción De-Hita-Cantalejo, Davide Borroni, Carlos Rocha-de-Lossada, and José-María Sánchez-González. 2021. "Prophylactic Corneal Cross-Linking in Myopic Femtosecond Laser-Assisted In Situ Keratomileusis: Long-Term Visual and Refractive Outcomes" Optics 2, no. 1: 55-62. https://doi.org/10.3390/opt2010006
APA StyleAlonso-Aliste, F., Amián-Cordero, J., Rachwani-Anil, R., De-Hita-Cantalejo, C., Borroni, D., Rocha-de-Lossada, C., & Sánchez-González, J.-M. (2021). Prophylactic Corneal Cross-Linking in Myopic Femtosecond Laser-Assisted In Situ Keratomileusis: Long-Term Visual and Refractive Outcomes. Optics, 2(1), 55-62. https://doi.org/10.3390/opt2010006









