Abstract
Context. This commentary is based on an innovative approach to the development of predictive analytics. It is centered on the development of predictive models for varying stages of chronic disease through integrating all types of datasets, adds various new features to a theoretically driven data warehousing, creates purpose-specific prediction models, and integrates multi-criteria predictions of chronic disease progression based on a biomedical evolutionary learning platform. After merging across-center databases based on the risk factors identified from modeling the predictors of chronic disease progression, the collaborative investigators could conduct multi-center verification of the predictive model and further develop a clinical decision support system coupled with visualization of a shared decision-making feature for patient care. The Study Problem. The success of health services management research is dependent upon the stability of pattern detection and the usefulness of nosological classification formulated from big-data-to-knowledge research on chronic conditions. However, longitudinal observations with multiple waves of predictors and outcomes are needed to capture the evolution of polychronic conditions. Motivation. The transitional probabilities could be estimated from big-data analysis with further verification. Simulation or predictive models could then generate a useful explanatory pathogenesis of the end-stage-disorder or outcomes. Hence, the clinical decision support system for patient-centered interventions could be systematically designed and executed. Methodology. A customized algorithm for polychronic conditions coupled with constraints-oriented reasoning approaches is suggested. Based on theoretical specifications of causal inquiries, we could mitigate the effects of multiple confounding factors in conducting evaluation research on the determinants of patient care outcomes. This is what we consider as the mechanism for avoiding the black-box expression in the formulation of predictive analytics. The remaining task is to gather new data to verify the practical utility of the proposed and validated predictive equation(s). More specifically, this includes two approaches guiding future research on chronic disease and care management: (1) To develop a biomedical evolutionary learning platform to predict the risk of polychronic conditions at various stages, especially for predicting the micro- and macro-cardiovascular complications experienced by patients with Type 2 diabetes for multidisciplinary care; and (2) to formulate appropriate prescriptive intervention services, such as patient-centered care management interventions for a high-risk group of patients with polychronic conditions. Conclusions. The commentary has identified trends, challenges, and solutions in conducting innovative AI-based healthcare research that can improve understandings of disease-state transitions from diabetes to other chronic polychronic conditions. Hence, better predictive models could be further formulated to expand from inductive (problem solving) to deductive (theory based and hypothesis testing) inquiries in care management research.
1. Introduction
A transdisciplinary framework for chronic disease research has been established by health services researchers [1,2] in the selection of relevant variables for the prediction of disease transition during a life course, as particularly related to Type 2 diabetes [3,4,5], heart failure [6,7], and chronic kidney disease [8]. The Centers for Medicare and Medicaid Services (CMS) has strongly advocated for the use of practical selfcare management strategies to tackle chronic disease management under severe resource constraints [9,10]. It offers a detailed analytical plan with problem-solving steps for delivering high-quality research results.
The concomitant development of the theoretical framework and methodological rigor required for verifying predictive analytics is germane to the formulation of artificial intelligence applications in healthcare. This care management approach may generate pertinent information for implementing and evaluating effective multidisciplinary care for chronic diseases. The present research and review paper offers a novel approach to the design and implementation of Support Vector Machine (SVM), a simple supervised machine learning algorithm used for classification and/or regression. The SVM-based predictive models enhance the prescriptive clinical care for polychronic conditions [11,12]. The transdisciplinary and collaborative nature of confirmatory research may generate useful care management and policy-relevant information to guide the improvement of chronic disease care for a targeted group of high-risk patient population members [13].
The central research inquiry is to address what and how AI healthcare research on the management of chronic diseases can be solidified and guided by the development of theoretically sound and methodologically rigorous approaches to selfcare management research. The purpose of this commentary is twofold: (1) To develop a biomedical evolutionary learning platform for predicting the micro- and macro-cardiovascular complications experienced by patients with chronic conditions for multidisciplinary care; and (2) to formulate appropriate prescriptive intervention services, such as patient-centered care management interventions, for a high-risk group of patients with polychronic conditions.
2. Critical Issues for Chronic Disease and Care Management Research
This paper addresses four critical issues pertaining to the application of artificial intelligence technologies: (1) global trends in chronic care and outcomes evaluation, (2) critical needs for assessing patient-centered care interventions, (3) challenges and solutions for chronic care in promoting coordinated or guided care, and (4) opportunities in transdisciplinary and collaborative care management research.
2.1. Global Trends in Chronic Care and Outcomes Evaluation
As the growth of an aging population is associated with an increase in demand for care, it is natural to pay special attention to the complex needs of frail elders. Four specific care management trends are presented below. First, the path to polychronic conditions reflects the need for covering both physical and mental health domains. The reciprocal relationship between them should be better investigated by health services researchers. Second, chronic care management has emerged as a highly specialized field in clinical medicine. Integrated care coupled with chronic care management requires the development of transdisciplinary orientation and teamwork in the phase of design, implementation, and evaluation of care plans. In the United States, the joint efforts of two governmental agencies such as the Agency for Health Research and Quality (AHRQ) and the CMS have led the ways in formulating chronic care management guidelines. Second, the growth of community-based care as an option or alternative to the institutionalization of the elderly facilitates the growth of post-acute care and long-term care in numerous countries. For instance, Taiwan launched a long-term care (LTC) alternative movement in 2007. To date, Taiwan has ventured into an era of LTC 2.0. with strong financial support for the growth of community-based long term care alternatives. Third, patient engagement is essential for success in performing patient care outcomes assessment and evaluation. The use of logic models in program planning and evaluation has signified how the structure-process-performance-outcomes framework of chronic care management could help optimize global collaboration in chronic care management research. Fourth, assisted technology development has shaped how care is managed and delivered. Furthermore, embracing new applications of information technology and addressing the healthcare labor shortage are two important tasks for global collaboration. It is anticipated that social robotics and other AI-based communication applications may transfer the landscape of chronic care management from a low to a high technology platform.
2.2. Critical Needs for Assessing Patient-Centered Care Interventions
Patient-centered care is characterized by several important principles: (1) problem identification [14] before alleviating the problem, (2) targeting high-risk patients for care management interventions [15], (3) designing and implementing patient-centered care modalities [4,6], and (4) conducting a patient outcome-based evaluation guided by the logic model [9,16]. It is important to note that patient-centered care is characterized by important principles such as respect for a patient’s preference or choice, the provision of coordinated and integrated care, encouragement in shared information and decision-making, presence of personal comfort and emotional support, family involvement and support groups, continuity of care, and equitable care provision.
2.3. Challenges and Solutions for Designing Chronic Care Modalities in Promoting Coordinated or Guided Care
- Challenge One. The Lack of Theoretical Guidance in Selecting Predictor Variables
Longitudinal patient-care datasets could be used to generate predictive models in varying stages of chronic disease. This is an efficient approach for the investigation of the progressive nature of chronic disease. However, a lack of theoretical guidance in selecting predictor variables has seriously affected the predictability of empirical models.
Solutions: The retrospective approach could be replaced by the prospective study approach, using a small set of predictor variables in the evaluation of progressive paths of polychronic conditions. Two-level modeling of the determinants of health and healthcare enables the examination of joint and interaction effects of personal/behavioral factors at the micro-level analysis and ecological/contextual factors at the macro-level analysis. In addition, the exploration of interaction effects of micro- and macro-level variables is essential to the development of predictive models that can detect the influence of contextual and cultural factors on personal and public health. For instance, here are four research questions pertaining to the study for improving selfcare management of chronic conditions: (1) What are the dominant human factors involved in selfcare? (2) What are the contextual or ecological variables that may interact with personal or human factors in the design of selfcare management strategies? (3) How are patient care outcomes specified and measured? (4) What is the value-based appraisal and evaluation of an innovative chronic care modality? The Patient-Centered Outcomes Research Institute (PCORI) [17] has played a vital role in helping people make informed decisions and improving healthcare delivery and outcomes by producing and promoting high-integrity, evidence-based information that comes from research guided by patients, caregivers, and the broader healthcare community.
- Challenge Two. Inadequate Validation of Multidisciplinary Care
The sensitivity and specificity of each predictive model derived from SVM have not been systematically examined to determine the validity of multidisciplinary patient care since stringent and pre-determined criteria, ranging from the proximal, intermediate, and distal outcomes, and measured at the patient- and population-level, have yet to be formulated in evaluation research. Furthermore, the development of “precision care” or personal care modalities should consider both the quality and efficiency of care plans simultaneously [17].
Solutions: The validation criteria of a predictive model should be decided and set in advance so that the predictive power of selfcare management strategies can be determined and enhanced. The prescriptive nature of patient-centered care strategies should consider individual choices or self-efficacy, rather than simply based on the relative cost of care options. The critical research question for validating the effectiveness of multidisciplinary care for polychronic conditions should include the follow inquiry: What is the dose-response relationship of the amount and type of innovative care services for patient care outcomes?
- Challenge Three. The Need for Conducting Prospective or Experimental Studies
Under the pay-for-performance and other incentive policies for promoting selfcare management of polychronic conditions, only prospective studies have potential to generate useful information for designing, implementing, and evaluating chronic care models supplemented by the clinical decision support system. However, limited theoretical specifications for formulating polychronic care management are available to guide the design of interventions. Thus, the usefulness of patient-centered care components for the design of care plans is yet to be ascertained and standardized in empirical research.
Solutions: Clarification is needed to differentiate multidisciplinary care and integrated care in clinical practice. The use of a complex factorial design for outcomes evaluation is an efficient and powerful analytical strategy to generate practical solutions for chronic care problems. It is important to develop or select a theoretically guided framework, such as the logic model, in conducting the implementation of care interventions [16]. When multiple datasets are merged or pooled together for performing statistical analysis, it is important to delineate important confounding factors such as the contextual and provider variations in the establishment of predictive models. The study questions pertaining to the implementation research should address the consistency and integrity of patient adherence to the prescribed intervention. This refers to the identification of treatment integrity when a randomized controlled trial is being conducted.
- Challenge Four. The Rationale for Establishing an Integrated or Guided Care Model
A clear rationale for formalizing an integrated or guided care model at the early stage of chronic disease is imperative and essential to the achievement of optimal health outcomes for a target group of high-risk patients who are likely to experience polychronic conditions later in life.
Solutions: Chronic disease progression or transition is an important concept for studying the chronicity of the disease. It is also important to consider both time-varying and time-constant predictors of the disease evolution or progression when predictive analytics are being formulated. A multivariate modeling approach is preferred since it could simultaneously investigate the main effects and interaction effects of personal, organizational, ecological, and contextual variables in the analysis. Furthermore, the temporal sequence of service utilization and outcome variables should be captured in the design of a multi-wave longitudinal study. Thus, the sequential or causal effects of the intervention on the proximal, intermediate, and distal outcomes could be delineated from the analysis.
2.4. Opportunities for Collaborative and Transdisciplinary Research on Chronic Care Management
Figure 1 portrays a variety of discipline-free analytical methods that could be used in the evaluation of the effectiveness of multilevel predictors of chronic care innovations such as selfcare management strategies. For instance, the prediction of disease transitions over time (e.g., the evolution of diabetes to cardiovascular disorders and chronic kidney disease in varying severity stages) requires having a panel study design capturing the longitudinal data observed from an early to advanced stage of the illness. Thus, the treatments or interventions could be better monitored and followed up by collaborative research teams. Furthermore, the longitudinal study design will require the collection of multi-waves of patient care data for performing parametric and non-parametric statistical modeling of predictors [17]. Moreover, the ultimate solution for developing disease-specific detection, AI-based diagnostics and prevention strategies, relies on the standardization of measurements and metrics used in the design, implementation, and evaluation of healthcare outcomes [18,19,20].
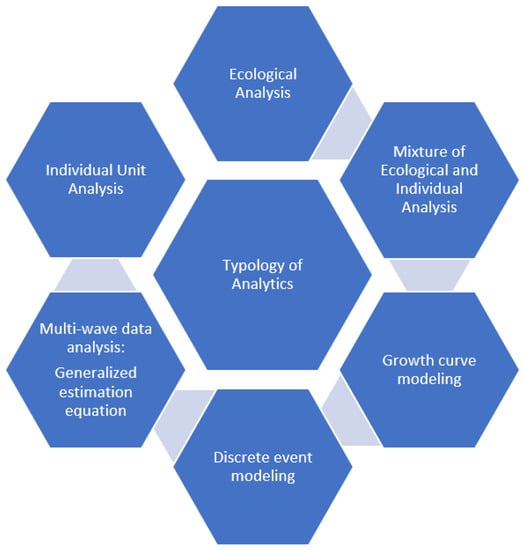
Figure 1.
Disciplinary Free Methods or Modeling Approaches.
The risk identification approach to constructing predictive equations has been extensively used by epidemiologists [19,21]. The development of predictive analytics for enhancing the validity of clinical decision support tools is a logical step for improving the disease management program for diabetes and related complications and critical care events. However, this is not a breakthrough idea, but rather is just a practical step for optimizing diabetes care. The stability of the predictive equations and modeling approaches should be examined, using repeated measures of disease transition or progression. The interplay or the reciprocal relationship between the micro- and macro-vascular changes for diabetes should be determined if the causal links among multiple measures or events are to be established and validated [22,23].
3. Transdisciplinary Science in Search for Theoretically Relevant Predictors of Polychronic Conditions and Outcomes
The Society for Design and Process Science is leading the way to identify theoretically sound frameworks to guide the design and implementation of clinical and administrative decision support systems for promoting selfcare management of chronic conditions [1,21]. By employing advanced data science technologies, theory-based constructs, or domains identified by collaborative scientists in the formulation of the data warehouse, practitioners may facilitate the convergence and integration of personal and social determinants of health into health services and management research. The simultaneity in considering personal and societal (ecological and contextual) factors in explaining the variations in healthcare outcomes enables the detection of interplays among multiple predictors such as personal, behavioral, organizational, ecological, and information technological factors. This reliance on theoretical guidance of care technology and management will foster changes in the design, implementation, and evaluation of healthcare innovations. This theoretically guided approach enables researchers to establish a scientific core for the data system containing useful constructs or domains to be used for formulating predictive analytics. More specifically, as data science is maturing, AI technology, such as ChatGPT in healthcare, will shape the direction of selfcare management strategies and policy developments for promoting the physical and mental health of the population.
Three specific research agendas are suggested for furthering the scientific pursuit of chronic care management. First, the field of predictive analytics should develop a socio-biomedical evolutionary learning platform to predict the risk of polychronic conditions at various stages. The trajectories of chronic disease should be clearly delineated or estimated from transitional probabilities at the population level. The big-data approach to merging the micro- and macro-data generated from public and private health insurance databases, coupled with theoretical specifications of relevant predicators measured at both personal and ecological levels, could effectively validate the disease patterns. Thus, the integrity of care management designed for the high-risk patient population for polychronic conditions could be adequately evaluated. Second, disease management strategies or toolboxes should help maximize both efficiency and effectiveness in achieving the ultimate goals of advancing quality and human dignity [24]. Third, scientific methods for protecting privacy and confidentiality in the release of healthcare data should be employed, particularly in the design of perturbations of personal data containing individual or geographic identifiers.
4. Conclusions
This commentary is unique and original in three ways. First, it identifies the major gaps in care management research and articulates the important role of developing theoretical frameworks coupled with rigorous multivariate modeling approaches for the causal analysis of factors influencing the care process and outcomes of patients with polychronic conditions. Second, we advocate the need to conduct rigorous care management research that will improve the design, process, and patient care outcomes. Third, we also specify the directions for future AI-based healthcare research that will overcome some challenges in designing and performing high-quality and innovative research.
Chronic disease may evolve from a single disease state into polychronic conditions. For example, Type 2 diabetes could evolve with both micro- and macro-vascular complications and further develop into polychronic conditions such as heart failure and chronic kidney disease. Thus, clinical researchers must make boundary spinning efforts to suggest viable and effective interventions for multiple chronic conditions. This is why chronic care management must provide not only specialty care but also comprehensive preventive and maintenance care for treating each target patient as a whole person. In the realm of multidisciplinary and comprehensive care, clinicians should establish clear criteria or quantifiable metrics for assessing and achieving optimal healthcare outcomes. As clinical researchers, it is imperative to design and execute intervention studies that will capture both micro (personal) and macro (provider and ecological) variants or predictive variables. Thus, clinically meaningful results or outcomes could be scientifically gathered via predetermined criteria for clinical evaluation of the effectiveness and efficiency of polychronic care. Commentary on trends, challenges, and solutions in conducting AI healthcare research can improve understandings of disease-state transitions from diabetes to other polychronic conditions. Hence, better predictive models could be further formulated to expand from inductive (problem solving) to deductive (theory centering and hypothesis testing) inquiries in care management research.
As digital health becomes more mature, the big-data-to-knowledge approach may be supplemented by the advance of machine and deep learning methods and guided by a theoretically meaningful framework for developing parsimonious models for maximizing the power of predictive analytics for performing high-quality health services evaluation and care management research [25]. One important development in population health management is the need to identify high-risk and target groups for interventions and then formulating and implementing decision support systems coupled with visualizations of changes in clinical and health outcomes of patients with polychronic conditions [13].
Finally, patient-centered care needs to be accentuated by an emphasis on patient engagement [10,26]. When patients are more aware of the choices available to them, selfcare management could further motivate them to take necessary and sufficient actions for reducing the burden of chronic illness. For optimizing the predictive analytics, it is imperative that an empirical approach, such as using neural network analysis and SVM, should be supplemented by sound theoretical specifications of predictive variables that could identify the causal sequala associated with unstable or declined health outcomes such as the concomitant development of multiple conditions and complications [13], unplanned hospitalization [27,28], and the transition from metabolic syndromes to cardiovascular disorders [29,30,31,32], chronic kidney disease [33,34,35,36], and mortality [37,38,39,40,41].
Author Contributions
T.T.H.W.: design, implementation, and critique of the AI healthcare applications; H.S.W.: review of the literature, editing, and referencing the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wan, T.T. Convergence of Artificial Intelligence Research in Healthcare: Trends and Approaches. J. Integr. Des. Process Sci. 2020, 1–15, Preprint. [Google Scholar] [CrossRef]
- Wan, T.T.H.; Terry, A.; McKee, B.; Kattan, W. KMAP-O framework for care management research of patients with type 2 diabetes. World J. Diabetes 2017, 8, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Wan, T.T.; Wang, B.L. An Integrated Social and Behavioral System Approach to Evaluation of Healthcare Information Technology for Polychronic Conditions. J. Integr. Des. Process Sci. 2021, 25, 148–160. [Google Scholar] [CrossRef]
- Luh, S.; Lin, Y.M.; Wu, P.H. A single framework of precision performance of diabetes disease prognosis for better care with collaboration. J. Integr. Des. Process Sci. 2022. Pre-press. [Google Scholar] [CrossRef]
- Lin, M.-Y.; Liu, J.-S.; Huang, T.-Y.; Wu, P.-H.; Chiu, Y.-W.; Kang, Y.; Hsu, C.-C.; Hwang, S.-J.; Luh, H. Data Analysis of the Risks of Type 2 Diabetes Mellitus Complications before Death Using a Data-Driven Modelling Approach: Methodologies and Challenges in Prolonged Diseases. Information 2021, 12, 326. [Google Scholar] [CrossRef]
- Liu, X.; Liu, L.; Li, Y.; Cao, X. The association between physical symptoms and self-care behaviours in heart failure patients with inadequate self-care behaviours: A cross-sectional study. BMC Cardiovasc. Disord. 2023, 23, 205. [Google Scholar] [CrossRef] [PubMed]
- Wan, T.T.H.; Terry, A.; Cobb, E.; McKee, B.; Tregerman, R.; Barbaro, S.D.S. Strategies to modify the risk of heart failure read-mission: A systematic review and meta analysis. Health Serv. Res.-Manag. Epidemiol. 2017, 4, 2333392817701050. [Google Scholar]
- Hsu, C.-C.; Hwang, S.-J.; Wen, C.-P.; Chang, H.-Y.; Chen, T.; Shiu, R.-S.; Horng, S.-S.; Chang, Y.-K.; Yang, W.-C. High Prevalence and Low Awareness of CKD in Taiwan: A Study on the Relationship Between Serum Creatinine and Awareness From a Nationally Representative Survey. Am. J. Kidney Dis. 2006, 48, 727–738. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services. CMS Vendor Guidelines; Centers for Medicare and Medicaid Services: Baltimore, MD, USA, 2022.
- Nielsen, M.; Buelt, L.; Patel, K.; Nichols, L.M. The Patient-Centered Medical Home’s Impact on Cost and Quality: Annual Review of Evidence, 2014–2015. Patient-Centered Primary Care Collaborative. 2016. Available online: https://www.pcpcc.org/sites/default/files/resources (accessed on 11 July 2023).
- Xie, Z.; Nikolayeva, O.; Luo, J.; Li, D. Building Risk Prediction Models for Type 2 Diabetes Using Machine Learning Techniques. Prev. Chronic Dis. 2019, 16, E130. [Google Scholar] [CrossRef]
- Agliata, A.; Giordano, D.; Bardozzo, F.; Bottiglieri, S.; Facchiano, A.; Tagliaferri, R. Machine Learning as a Support for the Diagnosis of Type 2 Diabetes. Int. J. Mol. Sci. 2023, 24, 6775. [Google Scholar] [CrossRef]
- Wan, T.T.H. Population Health Management for Polychronic Conditions: Evidence Based Research Approaches; Springer: New York, NY, USA, 2018. [Google Scholar]
- Nash, D.; Wohlforth, C. How COVID Crashed the System: A Guide to Fixing American Health Care; Rowan & Littlefield Publishers: New York, NY, USA, 2022. [Google Scholar]
- Wan, T.T.H. Artificial intelligence research in primary care management. Qual. Prim. Care 2018, 26, 114–116. [Google Scholar]
- Goff, Z.; House, A.; Guthrie, E.; Weston, H.; Mansbridge, L. Diabetes care in the acute psychiatric inpatient setting: A logic model for service delivery. Gen. Hosp. Psychiatry 2022, 78, 135–137. [Google Scholar] [CrossRef]
- Wan, T.T.; Matthews, S.; Luh, H.; Zeng, Y.; Wang, Z.; Yang, L. A Proposed Multi-Criteria Optimization Approach to Enhance Clinical Outcomes Evaluation for Diabetes Care: A Commentary. Health Serv. Res. Manag. Epidemiol. 2022, 9, 23333928221089125. [Google Scholar] [CrossRef] [PubMed]
- Cabral, B.P.; Braga, L.A.M.; Syed-Abdul, S.; Mota, F.B. Future of Artificial Intelligence Applications in Cancer Care: A Global Cross-Sectional Survey of Researchers. Curr. Oncol. 2023, 30, 3432–3446. [Google Scholar] [CrossRef]
- Lai, H.; Huang, H.; Keshavjee, K.; Guergachi, A.; Gao, X. Predictive models for diabetes mellitus using machine learning techniques. BMC Endocr. Disord. 2019, 19, 101. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Xie, W.; Li, L.; Wang, L.; You, Q.; Chen, L.; Li, J.; Ke, Y.; Fang, J.; Liu, L.; et al. Development a validation of a pre-diction model for elevated arterial stiffness in Chinese patients with diabetes using machine learning. Front. Physiol. 2021, 12, 714195. [Google Scholar] [CrossRef]
- Rav-Marathe, K.; Wan, T.T.; Marathe, S. The Effect of Health Education on Clinical and Self-Reported Outcomes of Diabetes in a Medical Practice. J. Integr. Des. Process Sci. 2016, 20, 45–63. [Google Scholar] [CrossRef]
- Fowler, M.J. Microvascular and Macrovascular Complications of Diabetes. Clin. Diabetes 2011, 29, 116–122. [Google Scholar] [CrossRef]
- Ismail-Beigi, F.; Craven, T.; Banerji, M.A.; Basile, J.; Calles, J.; Cohen, R.M.; Cuddihy, R.; Cushman, W.C.; Genuth, S.; Grimm, R.H., Jr.; et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: An analysis of the ACCORD randomized trial. Lancet 2010, 376, 419–430. [Google Scholar] [CrossRef]
- Fiedler, B.A.; Wan, T.T.H. Disease management organization approach to chronic illness. Int. J. Public Policy 2010, 6, 260–277. [Google Scholar] [CrossRef]
- Wan, T.T.H. Evidence-Based Health Care Management: Multivariate Modeling Approaches; Kluwer Academic Publishers: Boston, MA, USA, 2002. [Google Scholar]
- Cianfrocco, H. Paving a Path for Better Polychronic Care: How Collaboration, Prioritization, and Engagement Can Improve Outcomes. Harvard Business Review Analytical Services. 2021. Available online: www.optum.com/content/dam/optum3/optum/en/resources/white-papers/hbras_optum-white-paper-1-21-2021.pdf (accessed on 11 July 2023).
- Yang, X.; Ma, R.C.; So, W.-Y.; Kong, A.P.; Ko, G.T.; Ho, C.-S.; Lam, C.W.; Cockram, C.S.; Tong, P.C.; Chan, J.C. Development and validation of a risk score for hospitalization for heart failure in patients with Type 2 Diabetes Mellitus. Cardiovasc. Diabetol. 2008, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Yi, Q.; Wang, Y.; Wang, J.; Yu, H.; Zhang, J.; Hu, M.; Xu, J.; Wu, Z.; Hou, L.; et al. Long-term glycemic variability and risk of adverse health outcomes in patients with diabetes: A systematic review and meta-analysis of cohort studies. Diabetes Res. Clin. Pract. 2022, 192, 110085. [Google Scholar] [CrossRef] [PubMed]
- The ADVANCE Collaborative Group; Patel, A.; MacMahon, S.; Chalmers, J.; Neal, B.; Billot, L.; Woodward, M.; Marre, M.; Cooper, M.; Glasziou, P.; et al. Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Zhu, J.; Sun, N.; Wang, L.; Xie, C.; Tang, Q.; Mao, X.; Fu, X.; Brickell, A.; Hao, Y.; et al. Development and validation of prediction models for hypertension risks in rural Chinese populations. J. Glob. Health 2019, 9, 020601. [Google Scholar] [CrossRef] [PubMed]
- Li, T.-C.; Wang, H.-C.; Li, C.-I.; Liu, C.-S.; Lin, W.-Y.; Lin, C.-H.; Yang, S.-Y.; Lin, C.-C. Establishment and validation of a prediction model for ischemic stroke risks in patients with type 2 diabetes. Diabetes Res. Clin. Prac. 2018, 138, 220–228. [Google Scholar] [CrossRef]
- Garlo, K.G.; White, W.B.; Bakris, G.L.; Zannad, F.; Wilson, C.A.; Kupfer, S.; Vaduganathan, M.; Morrow, D.A.; Cannon, C.P.; Charytan, D.M. Kidney Biomarkers and Decline in eGFR in Patients with Type 2 Diabetes. Clin. J. Am. Soc. Nephrol. 2018, 13, 398–405. [Google Scholar] [CrossRef]
- Lin, C.-C.; Niu, M.J.; Li, C.-I.; Liu, C.-S.; Lin, C.-H.; Yang, S.-Y.; Li, T.-C. Development and validation of a risk prediction model for chronic kidney disease among individuals with type 2 diabetes. Sci. Rep. 2022, 12, 4794. [Google Scholar] [CrossRef]
- Nelson, R.G.; Grams, M.E.; Ballew, S.H.; Sang, Y.; Azizi, F.; Chadban, S.J.; Chaker, L.; Dunning, S.C.; Fox, C.; Hirakawa, Y.; et al. Development of Risk Prediction Equations for Incident Chronic Kidney Disease. JAMA 2019, 322, 2104–2114. [Google Scholar] [CrossRef]
- Jardine, M.J.; Hata, J.; Woodward, M.; Perkovic, V.; Ninomiya, T.; Arima, H.; Zoungas, S.; Cass, A.; Patel, A.; Marre, M.; et al. Prediction of Kidney-Related Outcomes in Patients With Type 2 Diabetes. Am. J. Kidney Dis. 2012, 60, 770–778. [Google Scholar] [CrossRef]
- Li, T.-C.; Li, C.-I.; Liu, C.-S.; Lin, W.-Y.; Lin, C.-H.; Yang, S.-Y.; Chiang, J.-H.; Lin, C.-C. Development and validation of prediction models for the risks of diabetes-related hospitalization and in-hospital mortality in patients with type 2 diabetes. Metab. Clin. Exp. 2018, 85, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, C.; Wang, M.; Yang, S.; Li, T.; Lin, C. Building clinical risk score systems for predicting the all-cause and expanded cardiovascular-specific mortality of patients with type 2 diabetes. Diabetes Obes. Metab. 2021, 23, 467–479. [Google Scholar] [CrossRef]
- De Cosmo, S.; Copetti, M.; Lamacchia, O.; Fontana, A.; Massa, M.; Morini, E.; Pacilli, A.; Fariello, S.; Palena, A.; Rauseo, A.; et al. Development and Validation of a Predicting Model of All-Cause Mortality in Patients With Type 2 Diabetes. Diabetes Care 2013, 36, 2830–2835. [Google Scholar] [CrossRef]
- Robinson, T.E.; Elley, C.R.; Kenealy, T.; Drury, P.L. Development and validation of a predictive risk model for all-cause mor-tality in type 2 diabetes. Diabetes Res. Clin. Pract. 2015, 108, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Prado, D.; Palazón-Bru, A.; Rosa, D.M.F.-D.; Carbonell-Torregrosa, M.; Martínez-Díaz, A.M.; Gil-Guillén, V.F. Predictive models for all-cause and cardiovascular mortality in type 2 diabetic inpatients. A cohort study. Int. J. Clin. Prac. 2015, 69, 474–484. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).