Characterisation of Fluid Administration in Burn Shock—A Retrospective Cohort Analysis
Abstract
1. Introduction
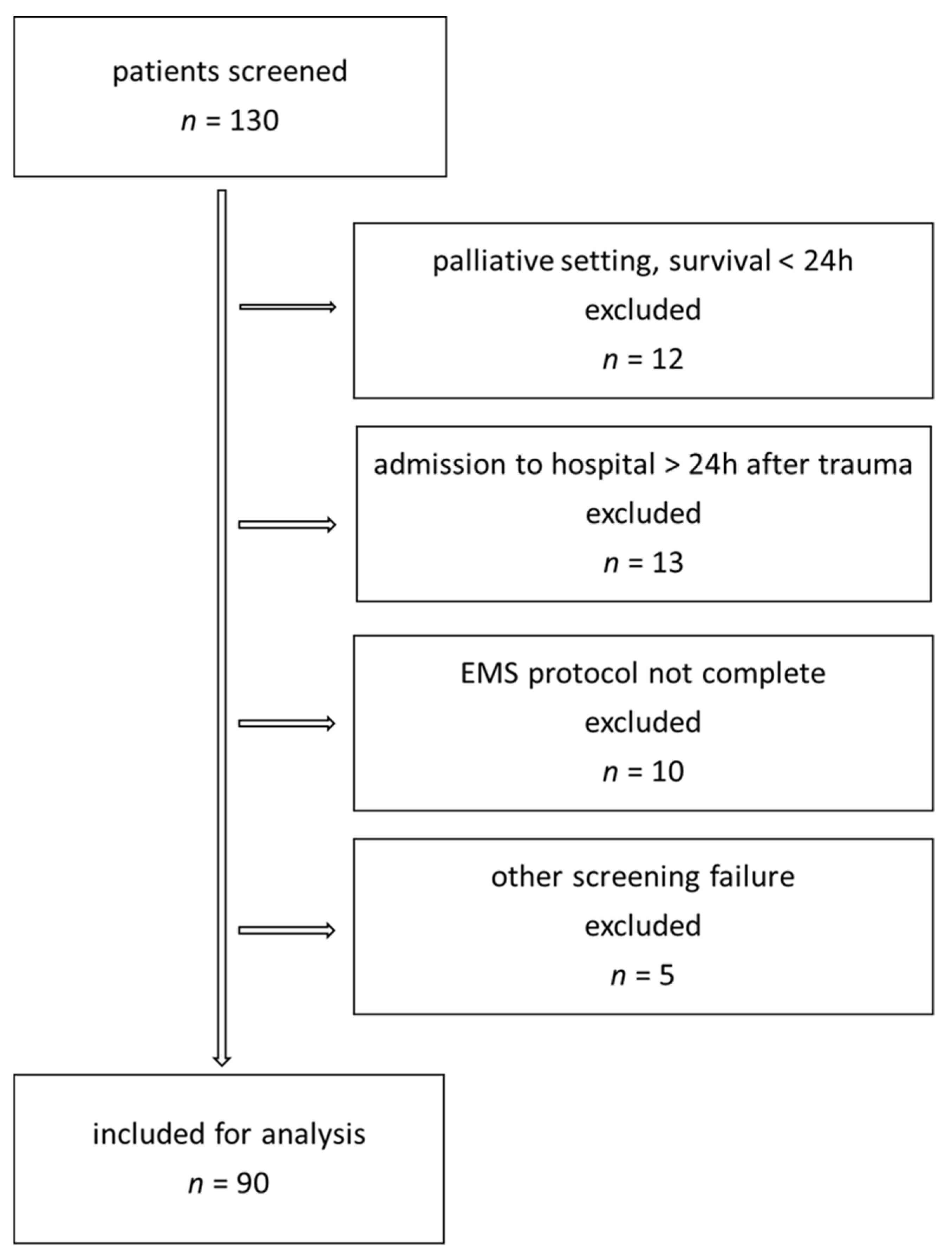
2. Methods
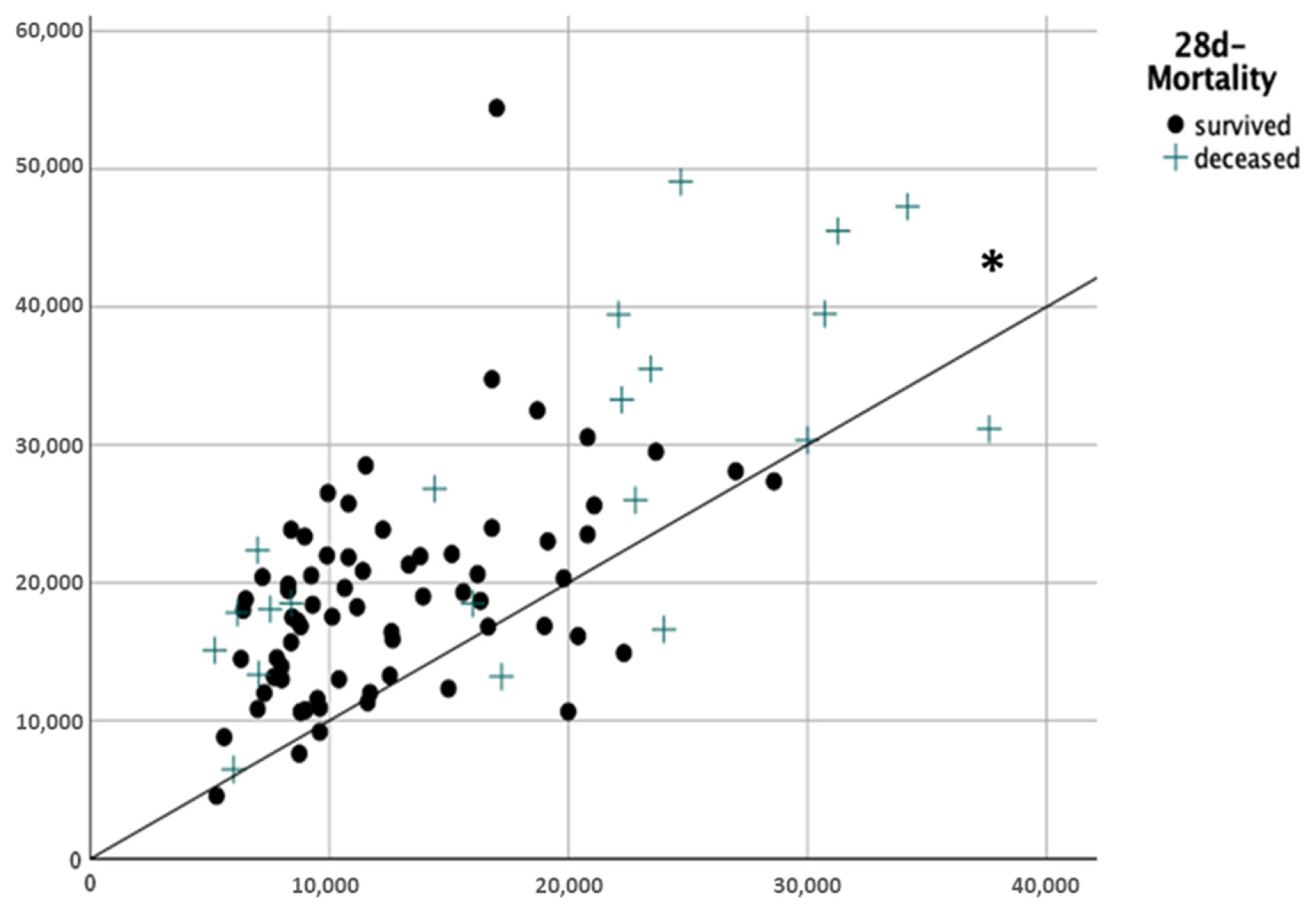
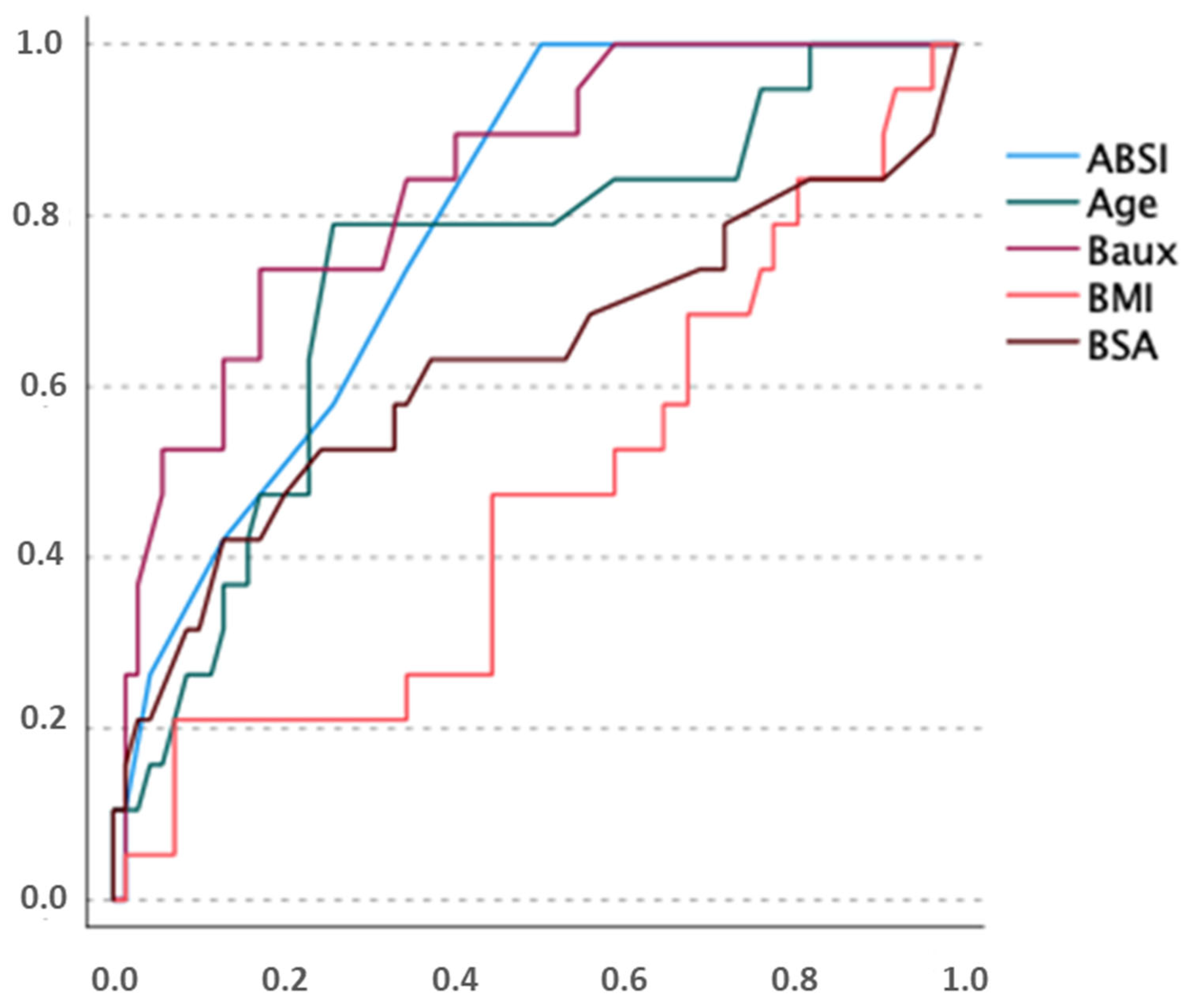
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 3rd-degree burn | full-thickness burn including epidermis and dermis |
| 4th-degree burn | including all skin layers as well as muscles, tendons and bones |
| ABSI score | abbreviated burn severity index, prognostic score, predicts burn-caused mortality |
| ACLF | acute-on-chronic liver failure |
| Baux index | prognostic score, predicts burn-caused mortality |
| BE | base excess |
| BMI | body mass index |
| bpm | beats per minute |
| BSA | body surface area |
| FiO2 | fraction of inspired oxygen |
| Gpt/L | giga-particles per litre |
| HR | heart rate |
| HUO | hourly urinary output |
| IAP | intra-abdominal pressure |
| INR | international normalised ratio |
| MAP | mean arterial pressure |
| mmHg | millimetres of mercury |
| PaO2 | partial pressure of oxygen in arterial blood |
| PEEP | positive end-expiratory pressure |
| pH | potential of hydrogen |
| Pmax | maximum inspiratory airway pressure |
| POC | point of care testing |
| Revised Baux score | prognostic score, predicts burn-caused mortality |
| TTE | transthoracic echocardiography |
References
- Daniels, M.; Fuchs, P.C.; Lefering, R.; Grigutsch, D.; Seyhan, H.; Limper, U.; Registry, T.G.B.; Schiefer, J.L. Is the Parkland formula still the best method for determining the fluid resuscitation volume in adults for the first 24 hours after injury?—A retrospective analysis of burn patients in Germany. Burns 2021, 47, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Paratz, J.D.; Stockton, K.; Paratz, E.D.; Blot, S.; Muller, M.; Lipman, J.; Boots, R.J. Burn resuscitation--hourly urine output versus alternative endpoints: A systematic review. Shock 2014, 42, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.; García-de-Lorenzo, A.; Herrero, E.; Lopez, T.; Galvan, B.; Asensio, M.J.; Cachafeiro, L.; Casado, C. A protocol for resuscitation of severe burn patients guided by transpulmonary thermodilution and lactate levels: A 3-year prospective cohort study. Crit. Care 2013, 17, R176. [Google Scholar] [CrossRef]
- Pantalone, D.; Bergamini, C.; Martellucci, J.; Alemanno, G.; Bruscino, A.; Maltinti, G.; Sheiterle, M.; Viligiardi, R.; Panconesi, R.; Guagni, T.; et al. The Role of DAMPS in Burns and Hemorrhagic Shock Immune Response: Pathophysiology and Clinical Issues. Review. Int. J. Mol. Sci. 2021, 22, 7020. [Google Scholar] [CrossRef]
- Dobson, G.P.; Morris, J.L.; Letson, H.L. Pathophysiology of severe burn injuries: New therapeutic opportunities from a systems perspective. J. Burn Care Res. 2024, 45, 1041–1050. [Google Scholar] [CrossRef]
- Rae, L.; Fidler, P.; Gibran, N. The Physiologic Basis of Burn Shock and the Need for Aggressive Fluid Resuscitation. Crit. Care Clin. 2016, 32, 491–505. [Google Scholar] [CrossRef]
- Baxter, C.R.; Shires, T. Physiological response to crystalloid resuscitation of severe burns. Ann. N. Y. Acad. Sci. 1968, 150, 874–894. [Google Scholar] [CrossRef]
- Holm, C.; Mayr, M.; Tegeler, J.; Hörbrand, F.; Henckel von Donnersmarck, G.; Mühlbauer, W.; Pfeiffer, U.J. A clinical randomized study on the effects of invasive monitoring on burn shock resuscitation. Burns 2004, 30, 798–807. [Google Scholar] [CrossRef]
- Navar, P.D.; Saffle, J.R.; Warden, G.D. Effect of inhalation injury on fluid resuscitation requirements after thermal injury. Am. J. Surg. 1985, 150, 716–720. [Google Scholar] [CrossRef]
- Dai, N.T.; Chen, T.M.; Cheng, T.Y.; Chen, S.L.; Chen, S.G.; Chou, G.H.; Chou, T.D.; Wang, H.J. The comparison of early fluid therapy in extensive flame burns between inhalation and noninhalation injuries. Burns 1998, 24, 671–675. [Google Scholar] [CrossRef]
- Culnan, D.M.; Farner, K.; Bitz, G.H.; Capek, K.D.; Tu, Y.; Jimenez, C.; Lineaweaver, W.C. Volume Resuscitation in Patients with High-Voltage Electrical Injuries. Ann. Plast. Surg. 2018, 80, S113–S118. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Yuan, K. Another important factor affecting fluid requirement after severe burn: A retrospective study of 166 burn patients in Shanghai. Burns 2011, 37, 1145–1149. [Google Scholar] [CrossRef] [PubMed]
- Markell, K.W.; Renz, E.M.; White, C.E.; Albrecht, M.E.; Blackbourne, L.H.; Park, M.S.; Barillo, D.A.; Chung, K.K.; Kozar, R.A.; Minei, J.P.; et al. Abdominal complications after severe burns. J. Am. Coll. Surg. 2009, 208, 940–947, discussion 947–949. [Google Scholar] [CrossRef]
- Klein, M.B.; Hayden, D.; Elson, C.; Nathens, A.B.; Gamelli, R.L.; Gibran, N.S.; Herndon, D.N.; Arnoldo, B.; Silver, G.; Schoenfeld, D.; et al. The association between fluid administration and outcome following major burn: A multicenter study. Ann. Surg. 2007, 245, 622–628. [Google Scholar] [CrossRef]
- Mason, S.A.; Nathens, A.B.; Jeschke, M.G. “Hold the Pendulum: Rates of Acute Kidney Injury Are Increased in Patients Who Receive Resuscitation Volumes Less Than Predicted by the Parkland Equation”. Ann. Surg. 2017, 266, e108. [Google Scholar] [CrossRef]
- Arlati, S.; Storti, E.; Pradella, V.; Bucci, L.; Vitolo, A.; Pulici, M. Decreased fluid volume to reduce organ damage: A new approach to burn shock resuscitation? A preliminary study. Resuscitation 2007, 72, 371–378. [Google Scholar] [CrossRef]
- Saffle, J.I. The phenomenon of “fluid creep” in acute burn resuscitation. J. Burn Care Res. 2007, 28, 382–395. [Google Scholar] [CrossRef]
- Dittrich, M.H.M.; Hosni, N.D.; de Carvalho, W.B. Association between fluid creep and infection in burned children: A cohort study. Burns 2020, 46, 1036–1042. [Google Scholar] [CrossRef]
- Engrav, L.H.; Colescott, P.L.; Kemalyan, N.; Heimbach, D.M.; Gibran, N.S.; Solem, L.D.; Dimick, A.R.; Gamelli, R.L.; Lentz, C.W. A biopsy of the use of the Baxter formula to resuscitate burns or do we do it like Charlie did it? J. Burn Care Rehabil. 2000, 21, 91–95. [Google Scholar] [CrossRef]
- Cartotto, R.; Zhou, A. Fluid creep: The pendulum hasn’t swung back yet! J. Burn Care Res. 2010, 31, 551–558. [Google Scholar] [CrossRef]
- Burmeister, D.M.; Smith, S.L.; Muthumalaiappan, K.; Hill, D.M.; Moffatt, L.T.; Carlson, D.L.; Kubasiak, J.C.; Chung, K.K.; Wade, C.E.; Cancio, L.C.; et al. An Assessment of Research Priorities to Dampen the Pendulum Swing of Burn Resuscitation. J. Burn Care Res. 2021, 42, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Osler, T.; Glance, L.G.; Hosmer, D.W. Simplified estimates of the probability of death after burn injuries: Extending and updating the baux score. J. Trauma Acute Care Surg. 2010, 68, 690–697. [Google Scholar] [CrossRef] [PubMed]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Lambden, S.; Laterre, P.F.; Levy, M.M.; Francois, B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit. Care 2019, 23, 374. [Google Scholar] [CrossRef]
- Shankar-Hari, M.; Phillips, G.S.; Levy, M.L.; Seymour, C.W.; Liu, V.X.; Deutschman, C.S.; Angus, D.C.; Rubenfeld, G.D.; Singer, M. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 775–787. [Google Scholar] [CrossRef]
- O’Grady, J.G.; Alexander, G.J.; Hayllar, K.M.; Williams, R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 1989, 97, 439–445. [Google Scholar] [CrossRef]
- Sarin, S.K.; Kedarisetty, C.K.; Abbas, Z.; Amarapurkar, D.; Bihari, C.; Chan, A.C.; Chawla, Y.K.; Dokmeci, A.K.; Garg, H.; Ghazinyan, H.; et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hepatol. Int. 2014, 8, 453–471. [Google Scholar] [CrossRef]
- Ball, R.L.; Keyloun, J.W.; Brummel-Ziedins, K.; Orfeo, T.; Palmieri, T.L.; Johnson, L.S.; Moffatt, L.T.; Pusateri, A.E.; Shupp, J.W. Burn-Induced Coagulopathies: A Comprehensive Review. Shock 2020, 54, 154–167. [Google Scholar] [CrossRef]
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Malbrain, M.L.; Cheatham, M.L.; Kirkpatrick, A.; Sugrue, M.; Parr, M.; De Waele, J.; Balogh, Z.; Leppäniemi, A.; Olvera, C.; Ivatury, R.; et al. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006, 32, 1722–1732. [Google Scholar] [CrossRef]
- Cartotto, R.; Burmeister, D.M.; Kubasiak, J.C. Burn Shock and Resuscitation: Review and State of the Science. J. Burn Care Res. 2022, 43, 567–585. [Google Scholar] [CrossRef] [PubMed]
- Cartotto, R.; Callum, J. A review of the use of human albumin in burn patients. J. Burn Care Res. 2012, 33, 702–717. [Google Scholar] [CrossRef] [PubMed]
- Yowler, C.J.; Fratianne, R.B. Current status of burn resuscitation. Clin. Plast. Surg. 2000, 27, 1–10. [Google Scholar] [CrossRef]
- Navickis, R.J.; Greenhalgh, D.G.; Wilkes, M.M. Albumin in Burn Shock Resuscitation: A Meta-Analysis of Controlled Clinical Studies. J. Burn Care Res. 2016, 37, e268–e278. [Google Scholar] [CrossRef]
- Saffle, J.R. Fluid Creep and Over-resuscitation. Crit. Care Clin. 2016, 32, 587–598. [Google Scholar] [CrossRef]
- Cancio, L.C.; Chávez, S.; Alvarado-Ortega, M.; Barillo, D.J.; Walker, S.C.; McManus, A.T.; Goodwin, C.W. Predicting increased fluid requirements during the resuscitation of thermally injured patients. J. Trauma Acute Care Surg. 2004, 56, 404–413, discussion 404–413. [Google Scholar] [CrossRef]
- Ivy, M.E.; Atweh, N.A.; Palmer, J.; Possenti, P.P.; Pineau, M.; D’Aiuto, M. Intra-abdominal hypertension and abdominal compartment syndrome in burn patients. J. Trauma Acute Care Surg. 2000, 49, 387–391. [Google Scholar] [CrossRef]
- Chung, K.K.; Wolf, S.E.; Cancio, L.C.; Alvarado, R.; Jones, J.A.; McCorcle, J.; King, B.T.; Barillo, D.J.; Renz, E.M.; Blackbourne, L.H. Resuscitation of severely burned military casualties: Fluid begets more fluid. J. Trauma Acute Care Surg. 2009, 67, 231–237, discussion 237. [Google Scholar] [CrossRef]
- Inoue, T.; Okabayashi, K.; Ohtani, M.; Yamanoue, T.; Wada, S.; Iida, K. Effect of smoke inhalation injury on fluid requirement in burn resuscitation. Hiroshima J. Med. Sci. 2002, 51, 1–5. [Google Scholar]
- Xiao, S.; Pan, Z.; Li, H.; Zhang, Y.; Li, T.; Zhang, H.; Ning, J. The impact of inhalation injury on fluid resuscitation in major burn patients: A 10-year multicenter retrospective study. Eur. J. Med. Res. 2024, 29, 283. [Google Scholar] [CrossRef]
- Prat, N.J.; Herzig, M.C.; Kreyer, S.; Montgomery, R.K.; Parida, B.K.; Linden, K.; Scaravilli, V.; Belenkiy, S.M.; Cancio, L.C.; Batchinsky, A.I.; et al. Platelet and coagulation function before and after burn and smoke inhalation injury in sheep. J. Trauma Acute Care Surg. 2017, 83, S59–S65. [Google Scholar] [CrossRef] [PubMed]
- Cartotto, R.C.; Innes, M.; Musgrave, M.A.; Gomez, M.; Cooper, A.B. How well does the Parkland formula estimate actual fluid resuscitation volumes? J. Burn Care Rehabil. 2002, 23, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Ning, F.; Jiang, H.; Qiu, J.; Wang, L. Different Depths May Not Determine the Fluid Resuscitation Volume in Early-stage Management of Severe Burns: A Model-comparison Retrospective Analysis of Fluid Volume Determining Factors. J. Burn Care Res. 2022, 43, 412–418. [Google Scholar] [CrossRef]
- Cotton, B.A.; Guy, J.S.; Morris, J.A., Jr.; Abumrad, N.N. The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock 2006, 26, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Nitzschke, S.L.; Aden, J.K.; Serio-Melvin, M.L.; Shingleton, S.K.; Chung, K.K.; Waters, J.A.; King, B.T.; Burns, C.J.; Lundy, J.B.; Salinas, J.; et al. Wound healing trajectories in burn patients and their impact on mortality. J. Burn Care Res. 2014, 35, 474–479. [Google Scholar] [CrossRef]
- Harrington, D.T. Complicated Burn Resuscitation. Crit. Care Clin. 2016, 32, 577–586. [Google Scholar] [CrossRef]
- Abla, H.; Tran, V.; Pang, A.; Stroever, S.; Shaw, C.; Dissanaike, S.; Griswold, J. Assessing resuscitation in burn patients with varying degrees of liver disease. Burns 2024, 50, 991–996. [Google Scholar] [CrossRef]
| Organ Dysfunction/Failure | Score |
|---|---|
| kidney | Acute kidney injury score (AKI) (serum creatinine/urinary output) [23] |
| shock | Norepinephrine > 0.1 πg/kg/min for MAP > 65 mmHg [24,25] |
| liver | King’s College Criteria (INR/serum bilirubin/age/etiology) [26] |
| ACLF score [27] | |
| coagulopathy | INR > 1.5 and thrombocytes < 150 Gpt/L [24,28] |
| lung | Berlin criteria for acute respiratory distress syndrome (PaO2/FiO2, x-ray) [29] |
| abdominal | |
| compartment | IAP > 20 mmHg for 24 h and organ dysfunction [30] |
| Number (%) or Median (IQR 25–75) (n = 90) | ||
|---|---|---|
| Sex (%) | female | 30 (33.3) |
| male | 60 (66.7) | |
| Age (years) | 52 (37–63) | |
| TBSA (%KOF) | 36 (25–51) | |
| Inhalation injury | 46 (51.1) | |
| Full-thickness burn | 76 (84.4) | |
| Electrocution | 2 (2.2) | |
| BMI | 27 (23–31) | |
| Baux | 104 (86–120) | |
| ABSI | 9 (8–11) | |
| Number (%) or Median (IQR 25–75) | ||||||
|---|---|---|---|---|---|---|
| All | <4 mL/kgKG/% | 4–6 mL/kgKG/% | >6 mL/kgKG/% | p | ||
| (n = 90) | (n = 13) | (n = 31) | (n = 46) | |||
| Sex (%) | female | 30 (33.3) | 4 (30.8) | 10 (32.3) | 16 (34.8) | 0.952 |
| male | 60 (66.7) | 9 (69.2) | 21 (67.7) | 30 (65.2) | ||
| Age (years) | 52 (37–63) | 56 (45–73) | 48 (36–62) | 54 (39–62) | 0.384 | |
| TBSA (%KOF) | 36 (25–51) | 50 (29–60) | 50 (34–65) | 30 (25–38) | <0.001 | |
| Inhalation injury | 46 (51.1) | 5 (38.5) | 16 (51.6) | 25 (58.1) | 0.453 | |
| High-voltage burns | 2 (2.2) | 1 (7.7) | 0 (0) | 1 (2.2) | 0.287 | |
| Full-thickness burns | 76 (84.4) | 9 (69.3) | 26 (83.9) | 42 (91.3) | 0.128 | |
| ABSI | 9 (8–11) | 10 (9–11) | 11 (7–12) | 9 (8–10) | 0.015 | |
| BMI | 27 (23–31) | 31 (28–33) | 29 (26–31) | 24 (22–28) | <0.001 | |
| Baux | 104 (86–120) | 106 (94–127) | 106 (90–127) | 95 (78–116) | 0.059 | |
| Ivy index (mL/kg) | ||||||
| <250 | 50 (55) | 12 (92) | 17 (55) | 21 (46) | 0.011 | |
| >250 | 40 (44) | 1 (7.7) | 14 (45) | 25 (54) | ||
| all ICU survivors | <4 mL/kgKG/% | 4–6 mL/kgKG/% | >6 mL/kgKG/% | p | ||
| (n = 59) | (n = 8) | (n = 20) | (n = 31) | |||
| No. of surgeries | 7.0 (5.0–11.0) | 3.5 (2.0–6.5) | 9.0 (6.5–14.5) | 7.0 (5.0–9.0) | 0.008 | |
| Number (%) | |||||
|---|---|---|---|---|---|
| All | <4 mL/kgKG/% | 4–6 mL/kgKG/% | >6 mL/kgKG/% | p | |
| (n = 90) | (n = 13) | (n = 31) | (n = 46) | ||
| art. hypertension | 21 (23.3) | 2 (15.4) | 9 (29.0) | 10 (21.7) | 0.581 |
| coronary art. disease | 6 (6.7) | 1 (7.7) | 2 (6.5) | 3 (6.5) | 0.987 |
| heart failure | 6 (6.7) | 3 (23.1) | 1 (3.2) | 2 (4.3) | 0.037 |
| diabetes mell. | 10 (11.1) | 2 (15.4) | 4 (12.9) | 4 (8.7) | 0.736 |
| pulm. disease | 3 (3.3) | 0 (0) | 0 (0) | 3 (6.5) | 0.227 |
| alcohol abuse | 13 (14.4) | 0 (0) | 3 (9.7) | 10 (21.7) | 0.093 |
| drugs other | 3 (3.3) | 0 (0) | 2 (6.5) | 1 (2.2) | 0.455 |
| liver disease | 7 (7.8) | 0 (0) | 1 (3.2) | 6 (13.0) | 0.152 |
| psych. disease | 21 (23.3) | 3 (23.1) | 7 (22.6) | 11 (23.9) | 0.991 |
| Number (%) or Median (IQR 25–75) | |||||
|---|---|---|---|---|---|
| All | <4 mL/kgBW/% | 4–6 mL/kgBW/% | >6 mL/kgBW/% | p | |
| (n = 90) | (n = 13) | (n = 31) | (n = 46) | ||
| Mortality 72 h | 4 (4.4) | 1 (7.7) | 2 (6.5) | 1 (2.2) | 0.556 |
| Mortality 28 d | 21 (23.3) | 3 (23.1) | 8 (25.8) | 10 (21.7) | 0.918 |
| Mortality ICU | 31 (34.4) | 5 (38.5) | 11 (35.5) | 15 (32.6) | 0.916 |
| ARDS | 43 (47.8) | 5 (38.5) | 16 (51.6) | 22 (47.8) | 0.721 |
| ALF | 6 (6.7) | 0 (0) | 1 (3.2) | 5 (11.4) | 0.222 |
| Coagulopathy | 47 (52.2) | 6 (46.2) | 15 (48.4) | 26 (56.5) | 0.699 |
| AKIN | 47 (52.2) | 7 (53.8) | 15 (48.4) | 25 (54.3) | 0.869 |
| Shock | 77 (85.6) | 8 (61.5) | 21 (90.3) | 41 (89.1) | 0.029 |
| ACS | 14 (15.6) | 0 (0) | 6 (19.4) | 8 (17.4) | 0.240 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Burns Association. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kruse, M.; Lenz, I.K.; Josuttis, D.; Plettig, P.; Hahnenkamp, K.; Gümbel, D.; Güthoff, C.; Hartmann, B.; Aman, M.; Schmittner, M.D.; et al. Characterisation of Fluid Administration in Burn Shock—A Retrospective Cohort Analysis. Eur. Burn J. 2025, 6, 35. https://doi.org/10.3390/ebj6020035
Kruse M, Lenz IK, Josuttis D, Plettig P, Hahnenkamp K, Gümbel D, Güthoff C, Hartmann B, Aman M, Schmittner MD, et al. Characterisation of Fluid Administration in Burn Shock—A Retrospective Cohort Analysis. European Burn Journal. 2025; 6(2):35. https://doi.org/10.3390/ebj6020035
Chicago/Turabian StyleKruse, Marianne, Ida Katinka Lenz, David Josuttis, Philip Plettig, Klaus Hahnenkamp, Denis Gümbel, Claas Güthoff, Bernd Hartmann, Martin Aman, Marc Dominik Schmittner, and et al. 2025. "Characterisation of Fluid Administration in Burn Shock—A Retrospective Cohort Analysis" European Burn Journal 6, no. 2: 35. https://doi.org/10.3390/ebj6020035
APA StyleKruse, M., Lenz, I. K., Josuttis, D., Plettig, P., Hahnenkamp, K., Gümbel, D., Güthoff, C., Hartmann, B., Aman, M., Schmittner, M. D., & Gebhardt, V. (2025). Characterisation of Fluid Administration in Burn Shock—A Retrospective Cohort Analysis. European Burn Journal, 6(2), 35. https://doi.org/10.3390/ebj6020035






