Emergency Treatment of Burns in Adults—Characteristics of Adult Patients and Acute/Pre-Hospital Burn Management
Abstract
1. Introduction
2. Materials and Methods
3. Results
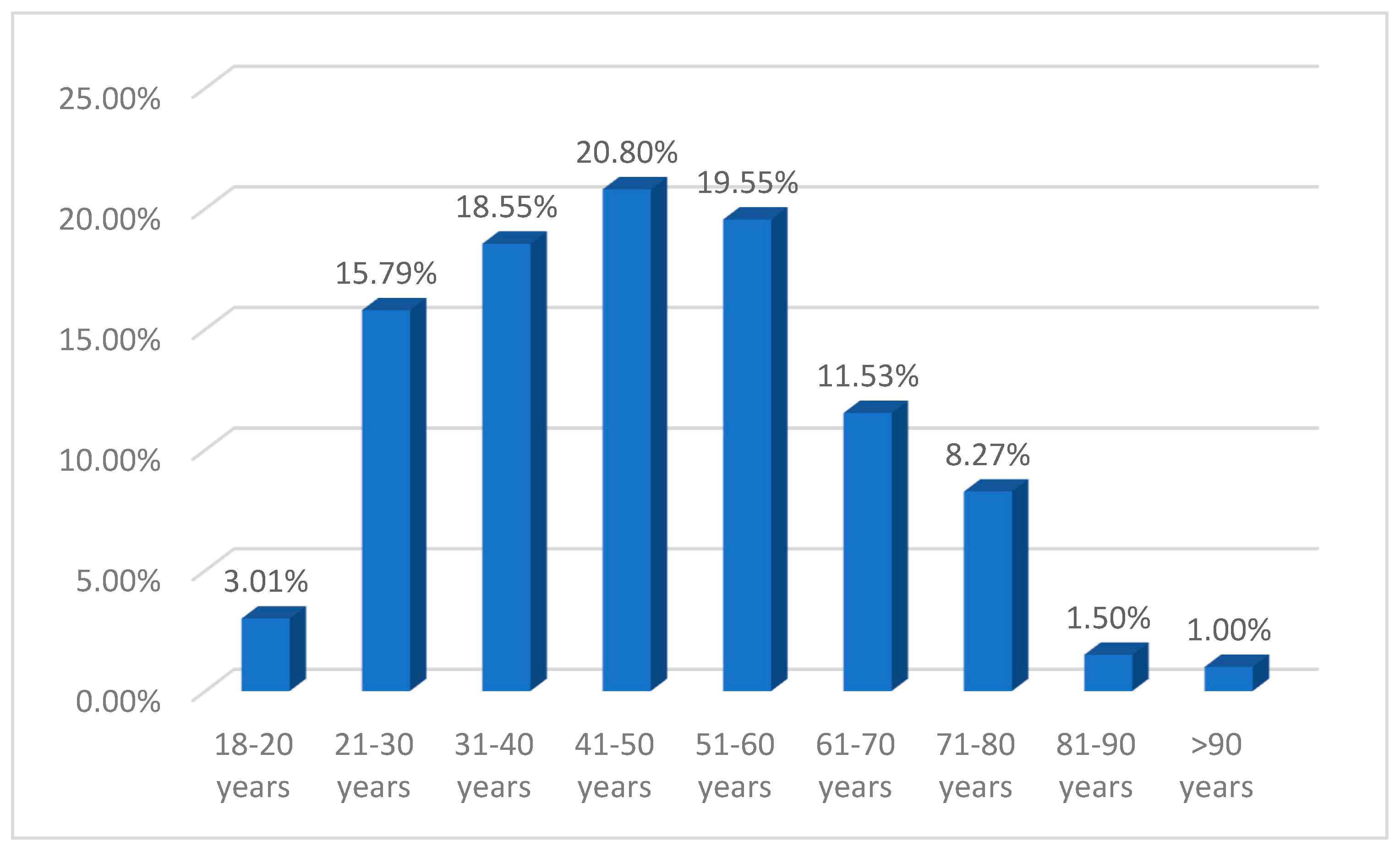
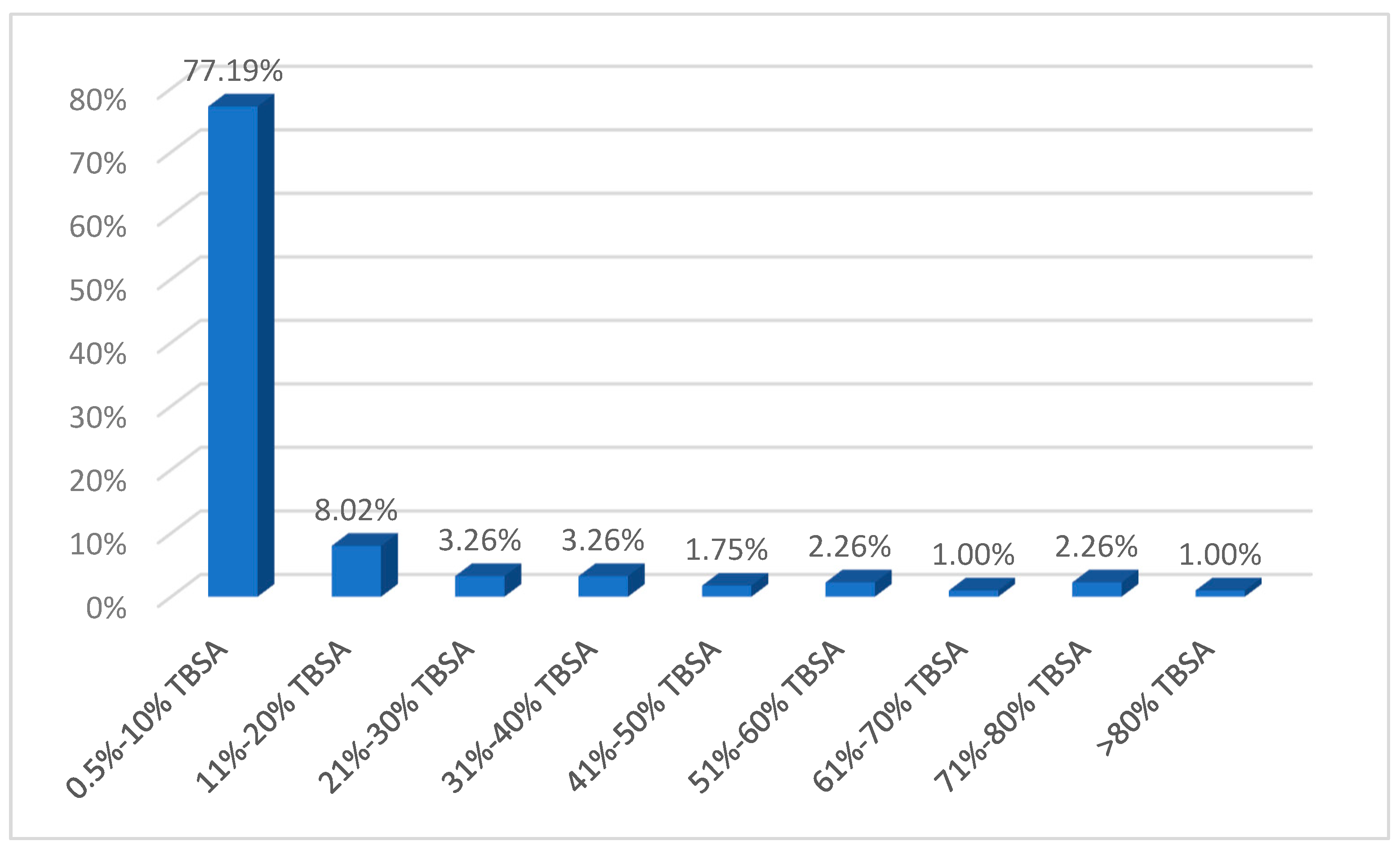
3.1. Demography
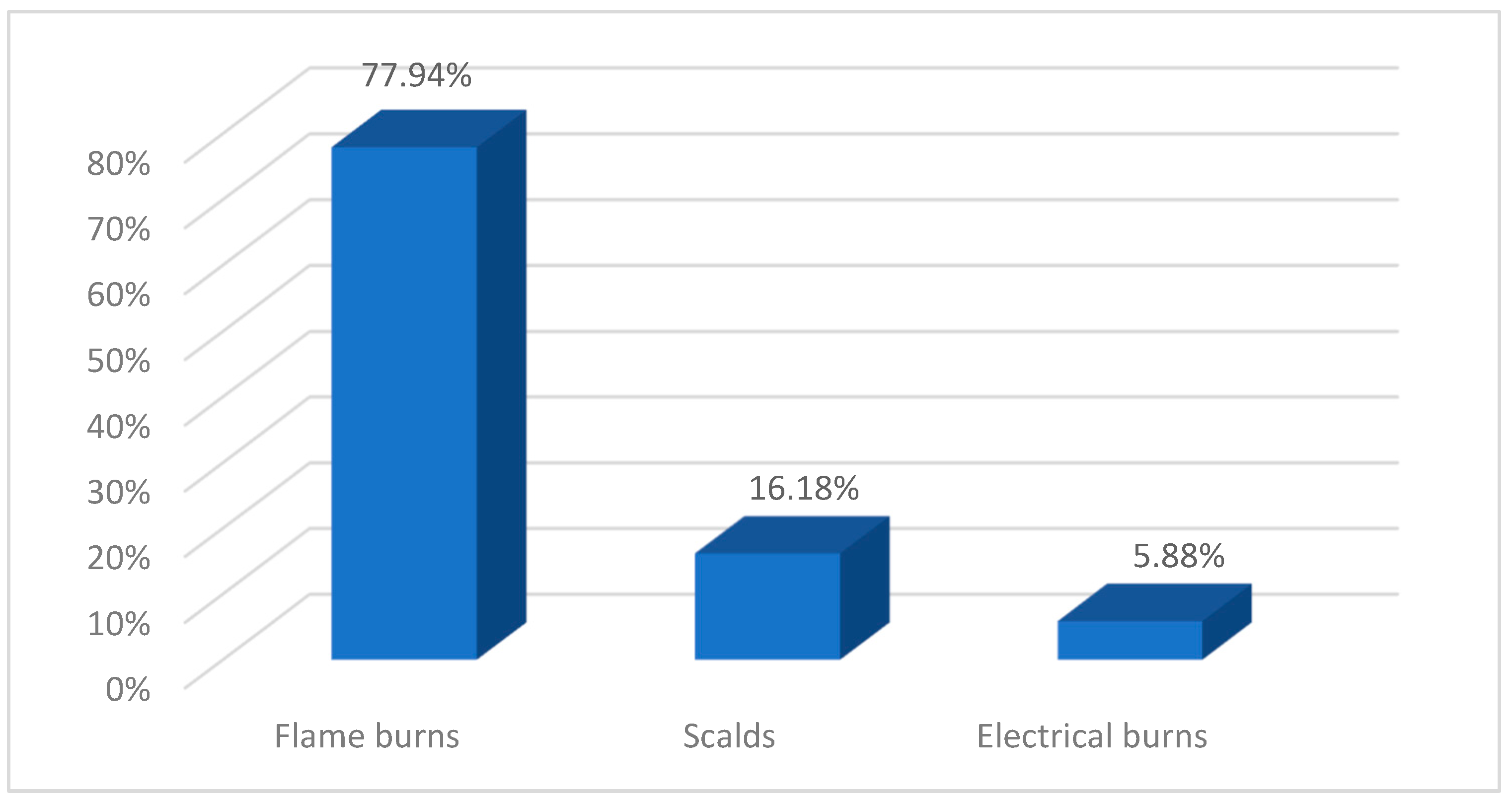
3.2. Etiology
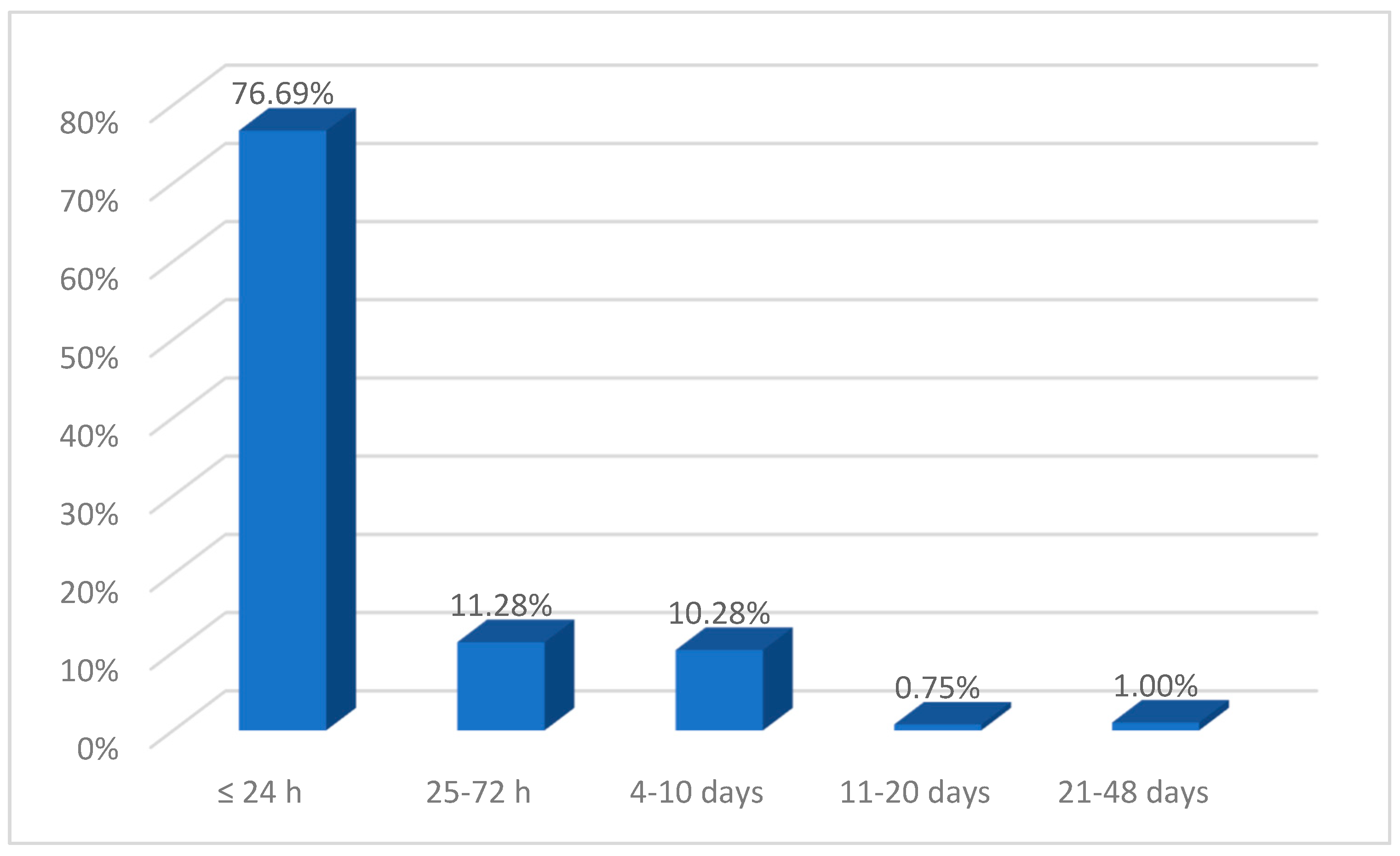
3.3. Time to Presentation
3.4. Pre-Hospital Care
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Legrand, M.; Barraud, D.; Constant, I.; Devauchelle, P.; Donat, N.; Fontaine, M.; Goffinet, L.; Hoffmann, C.; Jeanne, M.; Jonqueres, J. Management of severe thermal burns in the acute phase in adults. Aenesth Crit. Care Pain. Med. 2020, 39, 253–267. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Burns. 13 October 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/burns (accessed on 2 November 2024).
- Stewart, B.T. Epidemiology, Risk Factors, and Prevention of Burn Injuries. 2 November 2022. Available online: https://www.uptodate.com/contents/epidemiology-risk-factors-and-prevention-of-burn-injuries (accessed on 15 August 2024).
- Niculae, A.; Peride, I.; Tiglis, M.; Nechita, A.M.; Petcu, L.C.; Neagu, T.P. Emergency Care for Burn Patients—A Single-Center Report. J. Pers. Med. 2023, 13, 238. [Google Scholar] [CrossRef]
- Stiles, K. Emergency management of burns: Part 1. Emerg Nurse 2018, 26, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Stiles, K. Emergency management of burns: Part 2. Emerg Nurse 2018, 26, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Skokre, E.S.; Mohammed, S.E.M.; Elhapashy, H.M.M.; Elsharkawy, N.B.; Ramadan, O.M.E.; Abdelaziz, E.M. The effectiveness of the psychosocial empowerment program in early adjustment among adult burn survivors. BMC Nurs. 2024, 23, 45. [Google Scholar]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Sogsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. [Google Scholar] [CrossRef]
- Papini, R. Mnagement of burn injuries of various depths. BMJ 2024, 329, 158–160. [Google Scholar] [CrossRef]
- European Burns Association. European Practice Guidelines for Burn Care: Minimum Level of Burn Care Provision in Europe; Version 4; European Burns Association: Barcelona, Spain, 2017. [Google Scholar]
- Royal Adelaide Hospital. First Aid and Emergency Management of Adult Burns. 2023 Practice Guidelines. 2023. Available online: https://www.rah.sa.gov.au/assets/general-downloads/CALHN-RAH-Burns-Unit_First-aid-and-emergency-management-of-adult-burns_2023-Practice-Guidelines-26092023.pdf (accessed on 12 October 2024).
- Wounds International. International Best Practice Guidelines: Effective Skin and Wound Management of Non-Complex Burns; Wounds International (Shofield Healthcare Media Limited Enterprise House): London, UK, 2014. [Google Scholar]
- Ehrl, D.; Heidekrueger, P.I.; Ninkovic, M.; Broer, P.N. Effect of primary admission to burn centers on the outcomes of severely burned patients. Burns 2018, 44, 524–530. [Google Scholar] [CrossRef]
- Allison, K.; Porter, K. Consensus on the prehospital approach to burns patient management. Emerg. Med. J. 2004, 21, 112–114. [Google Scholar] [CrossRef]
- Wood, F.M.; Philips, M.; Jovic, T.; Cassidy, J.T.; Cameron, P.; Edgar, D.W. Water First Aid Is Beneficial In Humans Post-Burn: Evidence from a Bi-National Cohort Study. PLoS ONE 2016, 11, e0147259. [Google Scholar] [CrossRef]
- Harish, V.; Tiwari, N.; Fischer, O.M.; Li, Z.; Maitz, P.K.M. First aid improves clinical outcomes in burn injuries: Evidence from a cohort study of 4918 patients. Burns 2019, 45, 433–439. [Google Scholar] [CrossRef]
- Harish, V.; Li, Z.; Maitz, P.K.M. First aid is associated with improved outcomes in large body surface area burns. Burns 2019, 45, 1743–1748. [Google Scholar] [CrossRef]
- Josuttis, D.; Kruse, M.; Plettig, P.; Lenz, I.K.; Gümbel, D.; Hartmann, S.; Kuepper, S.S.; Gebhardt, V.; Schmittner, M.D. Prehospital treatment of severely burned patients: A retrospective analysis of patients admitted to the Berlin burn centre. Scand. J. Trauma. Resusc. Emerg. Med. 2024, 32, 70. [Google Scholar] [CrossRef]
- Pieptu, V.; Mihai, A.; Groza, C.; Gheorghiță, C.; Cimpoieșu, D.; Azoicăi, D. Burns in the Emergency Department: A One-Year Single Center Analysis on 355 Cases. Chirurgia 2020, 115, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Kouchek, M.; Aghakhani, K.; Dahgmardehei, M.; Memarian, A. Demographic Assessment of Burn Injuries in Iranian Patients. Bull. Emerg. Trauma. 2024, 12, 26–34. [Google Scholar]
- Smolle, C.; Cabiaso-Daniel, J.; Forbes, A.A.; Wurzer, P.; Hundeshagen, G.; Branski, L.K.; Huss, F.; Kamolz, L.P. Recent trends in burn epidemiology worldwide: A systematic review. Burns 2014, 43, 249–257. [Google Scholar] [CrossRef]
- Bordeanu-Diaconescu, E.; Grosu-Bularda, A.; Frunză, A.; Grama, M.; Dumitru, C.; Neagu, C.; Lascăr, I.; Hariga, C. The Impact of Burns Involving Over 50% of Total Body Surface Area—A Six-Year Retrospective Study. Medica (Bucur) 2024, 19, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.; Xiao, S.; Xia, Z. Consensus on the treatment of second-degree burn wounds (2024 edition). Burns Trauma 2024, 30, tkad061. [Google Scholar] [CrossRef] [PubMed]
- Endorf, F.; Gamelli, R. Inhalation injury, pulmonary perturbations, and fluid resuscitation. J. Burn Care Res. 2007, 28, 80–83. [Google Scholar] [CrossRef]
- Walker, P.; Buehner, M.; Wood, L.; Boyer, N.; Driscoll, I.; Lundy, J.; Cancio, L.; Chung, K. Diagnosis and management of inhalation injury: An updated review. Crit. Care 2015, 2015, 351. [Google Scholar] [CrossRef]
- Romanowski, K.S.; Palmieri, T.L.; Sen, S.; Grrenhalgh, D.G. More Than One Third of Intubations in Patients Transferred to Burn Centers are Unnecessary: Proposed Guide;lines for Appropriate Intubation of the Burn Patient. J. Burn. Care Res. 2016, 37, e409–e414. [Google Scholar] [CrossRef] [PubMed]
- Badulak, J.H.; Schurr, M.; Sauaia, A.; Ivaschchenko, A.; Pelz, E. Defining the criteria for intubation of the patient with thermal burns. Burns 2018, 44, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Mittal, B.M.; McQuitty, R.A.; Talon, M.; McQuitty, A.L. Airway Management for Acute and Reconstructive Burns: Our 30-year Experience. Semin. Plast. Surg. 2024, 38, 97–104. [Google Scholar] [CrossRef]
- Rice, P.L.; Orgill, D.P. Emergency Care of Moderate and Severe Thermal Burns in Adults. 20 February 2024. Available online: https://www.uptodate.com/contents/emergency-care-of-moderate-and-severe-thermal-burns-in-adults (accessed on 11 February 2025).
- Acute Respiratory Distress Syndrome Network; Brower, R.G.; Natthay, M.A.; Morris, A.; Schoenfeld, D.; Thompson, B.T.; Wheeler, A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar]
- Chung, K.K.; Wolf, S.E.; Cancio, L.C.; Alvarado, R.; Jones, J.A.; McCorcle, J.; King, B.T.; Barillo, D.J.; Renz, E.M.; Blackbourne, L.H. Resuscitation of severely burned military casualties: Fluid begets more fluid. J. Trauma. 2009, 67, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Allorto, N.L. Primary management of burn injuries: Balancing best practice with pragmatism. S. Afr. Fam. Pract. 2020, 62, 5202. [Google Scholar] [CrossRef]
- Cartotto, R.; Johnson, L.S.; Savetamal, A.; Greenhalgh, D.; Kubasiak, J.C.; Pham, T.N.; Rizzo, J.A.; Sen, S.; Main, E. American Burn Association Clinical Practice Guidelines on Burn Shock Resuscitation. J. Burn. Care Res. 2024, 45, 562–589. [Google Scholar] [CrossRef]
- Schaefer, T.J.; Szymanski, K.D. Burn Evaluation and Management. 8 August 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK430741/ (accessed on 12 June 2024).
- Isakov, A. Urgent air–medical transport: Right patient, place and time. Can. Med. Assoc. J. 2009, 181, 569–570. [Google Scholar] [CrossRef]
- American Burn Association. Guidelines for Burn Patient Referral (Advice on Transfer and Consultation). 2022. Available online: https://ameriburn.org/wp-content/uploads/2024/04/one-page-guidelines-for-burn-patient-referral-1.pdf (accessed on 11 November 2024).
- Sethi, D.; Subramanian, S. When place and time matter: How to conduct safe inter-hospital transfer of patients. Saudi J. Anaesth. 2014, 8, 104–113. [Google Scholar] [CrossRef]


| 2nd A–2nd B Degree | 3rd Degree | |
|---|---|---|
| 0.5–10% TBSA | 66.92% (n = 267) | 4.26% (n = 17) |
| 11–20% TBSA | 4.26% (n = 17) | 3.76% (n = 15) |
| 21–30% TBSA | 1.75% (n = 7) | 1.50% (n = 6) |
| 31–40% TBSA | 2.01% (n = 8) | 1.25% (n = 5) |
| 41–50% TBSA | 0.50% (n = 2) | 1.25% (n = 5) |
| 51–60% TBSA | 1.25% (n = 5) | 1.00% (n = 4) |
| 61–70% TBSA | - | 1.00% (n = 4) |
| 71–80% TBSA | 0.25% (n = 1) | 2.01% (n = 8) |
| >80% TBSA | - | 1.00% (n = 4) |
| Men | Women | Rural | Urban | |
|---|---|---|---|---|
| 1st degree | 5.83% (n = 13) | 6.25% (n = 11) | 3.42% (n = 5) | 7.51% (n = 19) |
| 2nd A-B degree | 73.99% (n = 165) | 81.25% (n = 143) | 70.55% (n = 103) | 81.03% (n = 205) |
| 3rd degree | 20.18% (n = 45) | 12.50% (22) | 26.03% (n = 38) | 11.46% (n = 29) |
| TBSA ≥ 20% | 25.11% (n = 56) | 6.82% (n = 12) | 30.14% (n = 44) | 9.49% (n = 24) |
| Airway burns | 17.04% (n = 38) | 6.25% (n = 11) | 21.23% (n = 31) | 7.11% (n = 18) |
| Associated trauma | 3.14% (n = 7) | 2.27% (n = 4) | 4.79% (n = 7) | 1.58% (n = 4) |
| Variable | R | p | Trust |
|---|---|---|---|
| Age | 0.87 | 0.0025 | 99% |
| TBSA% | −0.61 | 0.0025 | 99% |
| Depth of the burn injury | −0.84 | 0.0025 | 99% |
| Patients with First Aid at the Place of the Accident %(n) * | Patients Without First Aid at the Place of the Accident %(n) * | |
|---|---|---|
| Sex | ||
| Masculine | 63.81% (134) | 47.09% (89) |
| Feminine | 36.19% (76) | 52.91% (100) |
| Residential environment | ||
| Urban | 54.76 (115) | 73.02% (138) |
| Rural | 45.24 (95) | 26.98% (51) |
| Average age | ||
| Total | 48.08 ± 14 years | 49.07 ± 13.88 years |
| Men | 44.63 ± 13.70 years | 47.22 ± 13.57 years |
| Women | 45.87 ± 14.52 years | 50.71 ± 14.06 years |
| Burnt body surface (mean %TBSA) | 18.50 ± 14.06% | 3.68 ± 14.06% |
| Burn degree | ||
| 1st degree | 5.71% (12) | 6.35% (12) |
| 1st–2nd A/2nd B degree | 14.76% (31) | 21.69% (41) |
| 2nd A–2nd B degree | 54.76% (115) | 64.02% (121) |
| 2nd–3rd degree | 24.76% (52) | 7.94% (15) |
| Mean delay from injury to burn center | 17.20 ± 14.06% h | 34.90 ± 14.06% h |
| Inhalation injury | 22.38% (47) | 1.06% (2) |
| Associated injuries | 3.81% (8) | 1.59% (3) |
| Taken from the place of the accident | ||
| Own means | 47.14% (99) | 97.35% (184) |
| Ambulance | 21.90% (46) | 2.65% (5) |
| PA Ambulance | 5.24% (11) | - |
| UTIM Ambulance | 5.71% (12) | - |
| Plane ambulance | 2.38% (5) | - |
| Helicopter ambulance | 17.62% (37) | - |
| Pre-hospital interventions | ||
| Oro-tracheal intubation | 22.86% (48) | 1.06% (2) |
| Peripheral venous line | 40.48% (85) | 2.65% (5) |
| Central venous catheter | 19.05% (40) | 1.59% (3) |
| Urinary catheter | 22.38% (47) | 1.59% (3) |
| Analgesia | 44.29% (93) | 2.12% (4) |
| Parkland formula | 34.76% (73) | 2.12% (4) |
| Patients coming from other medical unit | 23.81% (50) | 2.12% (4) |
| Hospitalization | ||
| Yes | 41.90% (88) | 20.11% (38) |
| In Bucharest Clinical Emergency Hospital | 38.57% (81) | 19.58% |
| In other mnedical units | 3.33% (7) | 0.53% (1) |
| No | 58.10% (122) | 79.89% (151) |
| Did not need hospitalization | 55.71% (117) | 77.78% (147) |
| Refused hospitalization | 2.38% (5) | 2.12% (4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Burns Association. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oprita, B.; Burlacu, G.; Ispas, V.M.; Serban, I.A.; Oprita, R. Emergency Treatment of Burns in Adults—Characteristics of Adult Patients and Acute/Pre-Hospital Burn Management. Eur. Burn J. 2025, 6, 19. https://doi.org/10.3390/ebj6020019
Oprita B, Burlacu G, Ispas VM, Serban IA, Oprita R. Emergency Treatment of Burns in Adults—Characteristics of Adult Patients and Acute/Pre-Hospital Burn Management. European Burn Journal. 2025; 6(2):19. https://doi.org/10.3390/ebj6020019
Chicago/Turabian StyleOprita, Bogdan, Georgeta Burlacu, Vlad Mircea Ispas, Ioana Adriana Serban, and Ruxandra Oprita. 2025. "Emergency Treatment of Burns in Adults—Characteristics of Adult Patients and Acute/Pre-Hospital Burn Management" European Burn Journal 6, no. 2: 19. https://doi.org/10.3390/ebj6020019
APA StyleOprita, B., Burlacu, G., Ispas, V. M., Serban, I. A., & Oprita, R. (2025). Emergency Treatment of Burns in Adults—Characteristics of Adult Patients and Acute/Pre-Hospital Burn Management. European Burn Journal, 6(2), 19. https://doi.org/10.3390/ebj6020019






