1. Introduction
The congenital absence of maxillary lateral incisors (MLIA), whether unilateral or bilateral, is a relatively frequent dental anomaly, affecting around 2% of the general population [
1]. Management strategies generally involve two principal approaches: space closure through orthodontic means or space opening and preservation to facilitate subsequent prosthetic rehabilitation [
2].
Despite the growing preference for space closure, in cases where prosthetic replacement is the chosen approach, it becomes necessary to provide a temporary substitute to maintain aesthetics and function until the patient reaches full skeletal maturity [
3].
Removable prostheses incorporating denture teeth represent one treatment option. However, patients often poorly accept them due to their potential to impair speech and the fact that they leave the edentulous space visible when removed for meals or hygiene purposes. Maryland bridges typically require irreversible enamel reduction of otherwise healthy adjacent teeth. Moreover, they often fail to support ideal soft tissue contours, which may compromise the overall esthetic outcome when compared to mini-implants [
4].
Temporary anchorage devices (TADs) have been proposed as an alternative procedure for the temporary replacement of missing permanent MLIA in growing patients [
3]. TADs offer several advantages, including preservation of bone, prevention of tooth and root migration, reduced need for grafting, easier orthodontic retention, and improved aesthetics due to lingual TADs placement [
5].
While some authors, such as Ciarlantini R and Melsen B [
3], discourage vertical placement of TADs in favor of bicortical TADs (horizontal) due to their superior preservation of buccolingual alveolar width [
3], other studies present differing perspectives. Several case reports and clinical studies have documented successful outcomes with vertically inserted TADs, suggesting that, under appropriate clinical conditions, this approach can be a viable and effective alternative. Notably, the case report by Cope JB and McFadden D [
5] exemplifies the potential success of vertical insertion, highlighting that the choice of angulation may be influenced by individual anatomical and clinical factors.
This divergence in the literature underscores the need for further investigation into how insertion angulation affects bone response and long-term outcomes. Therefore, this study evaluates the effectiveness of TADs for temporary replacement in permanent MLIA and investigates whether any insertion angulation corresponds to minimizing bone-level change adjacent to the TAD.
2. Materials and Methods
2.1. Study Design
This study integrates a systematic review, following established clinical guidelines, along with a supplementary observational analysis.
2.2. Review Guidelines
This review was conducted in accordance with the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 [
6], and the completed PRISMA checklist is provided in the
Supplementary Materials. The study protocol was registered in the PROSPERO database (CRD420251107694).
2.3. Selection Criteria
Based on research questions, the following eligibility criteria were established: studies involving the use of TADs for the temporary replacement of missing permanent MLIA, and those evaluating outcomes such as changes in alveolar ridge dimensions (height and/or thickness), TAD angulation, bone remodeling, or overall success of the procedure.
Exclusion criteria included duplicate records, systematic reviews, and narrative reviews. In addition, studies that did not address the defined PICO frameworks—such as those not involving TADs for replacement of MLIA—were also excluded.
2.4. Eligibility Criteria
The Population, Intervention, Comparison, Outcomes, and Study design strategy (
Table 1) was used to formulate the guiding questions for this study: “How effective are TADs for the temporary replacement of permanent MLIA?” and “Is there a specific TAD angulation associated with minimal bone changes following placement?”
2.5. Search Strategy
A thorough literature search was performed in the PubMed database (accessed via the National Library of Medicine), Web of Science, and Scopus. Searches were performed between 10 April 2025 and 3 September 2025 across the three databases, with no publication date limits (from database inception to 3 September 2025). An identical advanced search strategy was applied to all databases, targeting titles, abstracts, and keywords with the search query detailed in
Table 2. Furthermore, the reference lists of all included articles were manually examined, resulting in the identification of three additional eligible studies.
2.6. Selection of Articles and Data Collection
The search was conducted both electronically and manually. Zotero® reference management software (version 7.0.15; Roy Rosenzweig Centre for History and New Media, George Mason University, Fairfax, VA, USA) was used to organize references and identify duplicate records, which were subsequently removed.
2.7. Quality Assessment
All the articles included were case reports, reflecting the limited availability of high-level evidence on this topic. The methodological quality of these case reports was assessed using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Case Reports [
7]. The included case reports were classified as having high methodological quality (7–8 criteria met) according to the JBI checklist. Although eight reports did not explicitly mention informed consent, all of them fulfilled the remaining seven criteria.
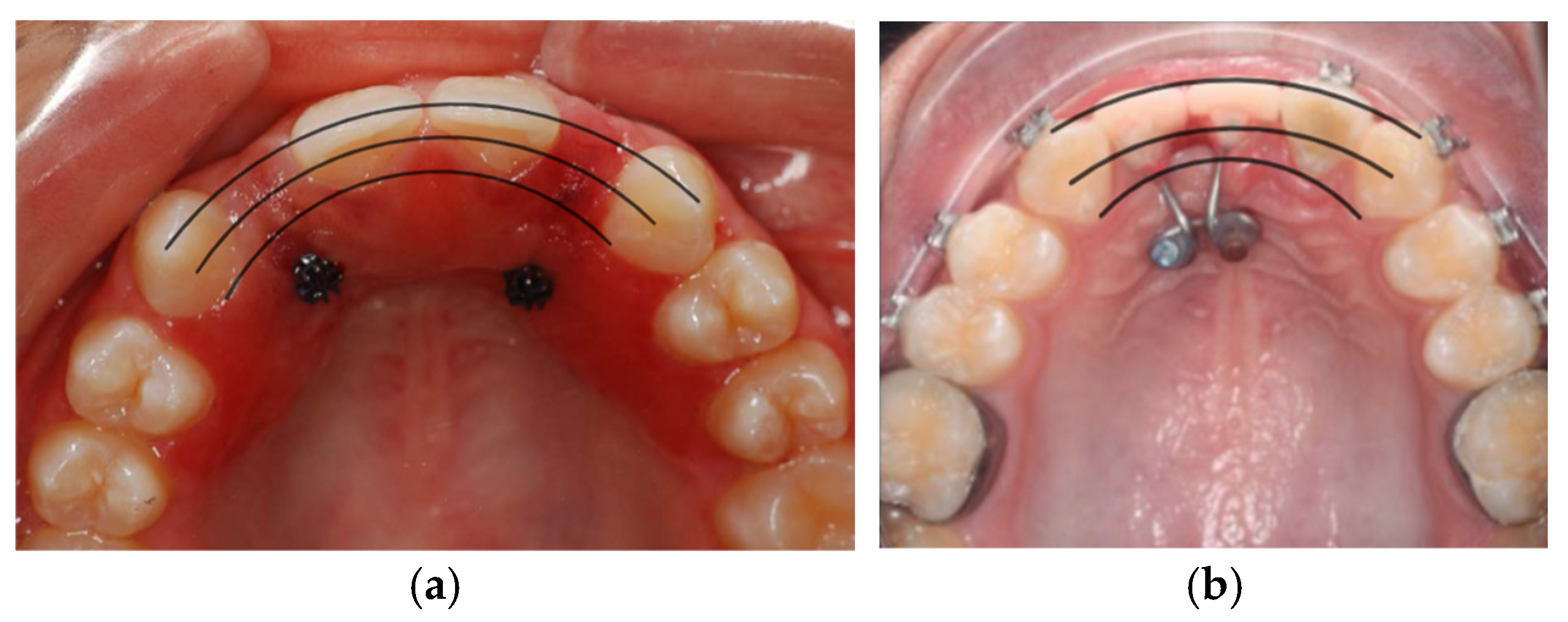
2.8. Angulation Classification of Palatal TADs Using Reference Arcs on Intraoral Images
To standardize the assessment of the insertion angulation of palatal TAD, a protocol based on anatomical reference arcs was developed. This method uses an occlusal intraoral photograph of the maxillary arch, in which three curved reference lines are drawn connecting key anatomical landmarks. The first arc, which is the most coronal (outermost), connects the cusp tips of the right and left canines. The second arc, located slightly more apically, connects the cingula of the anterior teeth. The third and most apical arc connects the marginal gingival contour of the anterior maxillary teeth.
The classification of the TAD sagittal inclination is determined by the location of its insertion point relative to these three arcs (
Table 3).
Although the intraoral photographs analyzed were collected from diverse sources and are not standardized in terms of angle or distance, the application of this protocol allows for a consistent comparative assessment of TAD insertion angulation. By referencing stable anatomical landmarks, namely the canine cusp tips, the cingula of the anterior teeth, and the marginal gingiva, it is possible to trace relative reference arcs that provide a common framework for classification. Despite the lack of photographic standardization, this method enables a systematic evaluation of the sagittal inclination of TADs across multiple cases.
Figure 1 illustrates the intraoral measurements based on the proposed classification. Only two images are shown due to copyright limitations, but this protocol was applied to all intraoral images.
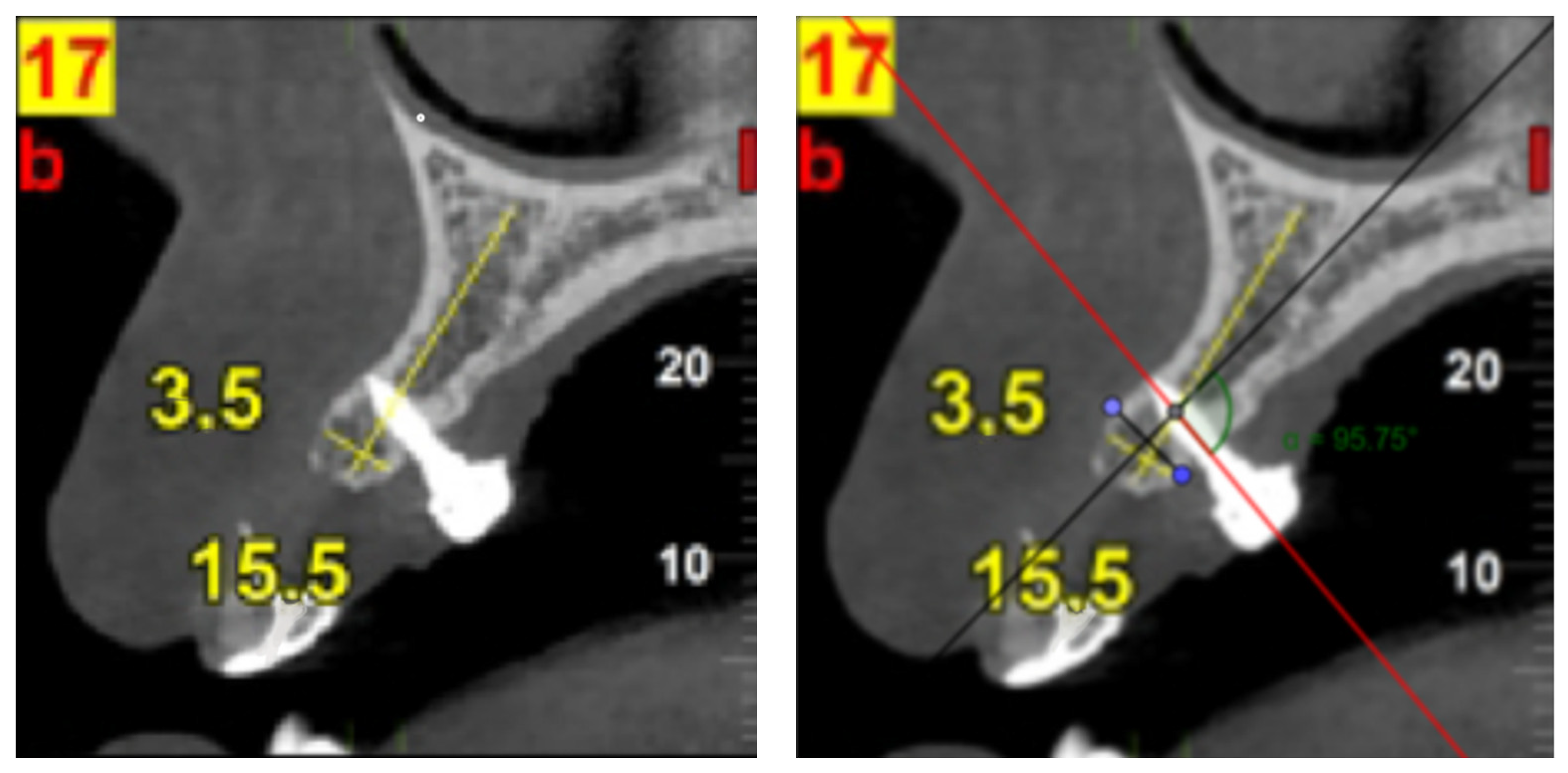
2.9. Supplementary Observational Analysis Based on CBCT Data
To complement the qualitative synthesis of the included case reports, a supplementary observational analysis was conducted on cone-beam computed tomography (CBCT) images extracted from published articles. This methodology enabled a secondary, image-based quantitative assessment beyond the descriptive scope of the original publications, supporting a more nuanced understanding of TAD biomechanics in the context of temporary prosthetic rehabilitation. To evaluate each case, we established the following classification for the measured angulations (
Table 4):
This protocol (
Table 5) was designed to evaluate the relationship between TAD insertion angulation and peri-implant bone response, an aspect not originally quantified by the authors of the primary studies.
Figure 2 illustrates an observational analysis using CBCT data retrieved from the studies included in this review. Due to copyright restrictions, only one CBCT image (Laino L et al. [
8]) is authorized for publication in this article. Nonetheless, the same standardized measurement protocol was applied to the second study with available CBCT imaging (Ciarlantini and Melsen et al. [
3]). Both the original image and the corresponding overlay with measurements are presented to illustrate the applied methodology.
To assess bone response, in case reports where CBCT images taken several years apart were available, measurements were performed directly on the images.
Table 6 presents the protocol used for these measurements.
2.10. Clinical Case Methodology
2.10.1. Case Presentation
The measurements were conducted on a clinical case selected and treated by Professor Teresa Pinho. The case involved a male patient who started orthodontic treatment at the age of 13 due to bilateral MLIA. At 14.5 years of age, the first TADs were placed to support the rehabilitation. The patient provided informed consent. This case aims to report the clinical outcomes of TAD inserted with vertical and diagonal angulations. The patient was selected due to the clinical progression observed: the initial placement of two vertically inserted TADs resulted in mobility, and subsequent failure, 2 months after requiring their replacement, after 2 months waiting for bone to recover. The subsequent insertion of diagonally oriented TADs led to excellent clinical stability and a favorable outcome with 1-year follow-up. In both attempts, the same TADs were used (14 × 2 mm; Kubident®, Seville, Spain).
2.10.2. Protocol Used in This Study
For both CBCT scans (corresponding to the vertical and diagonal insertions), the procedure outlined in
Section 2.9 of the protocol was followed.
3. Results
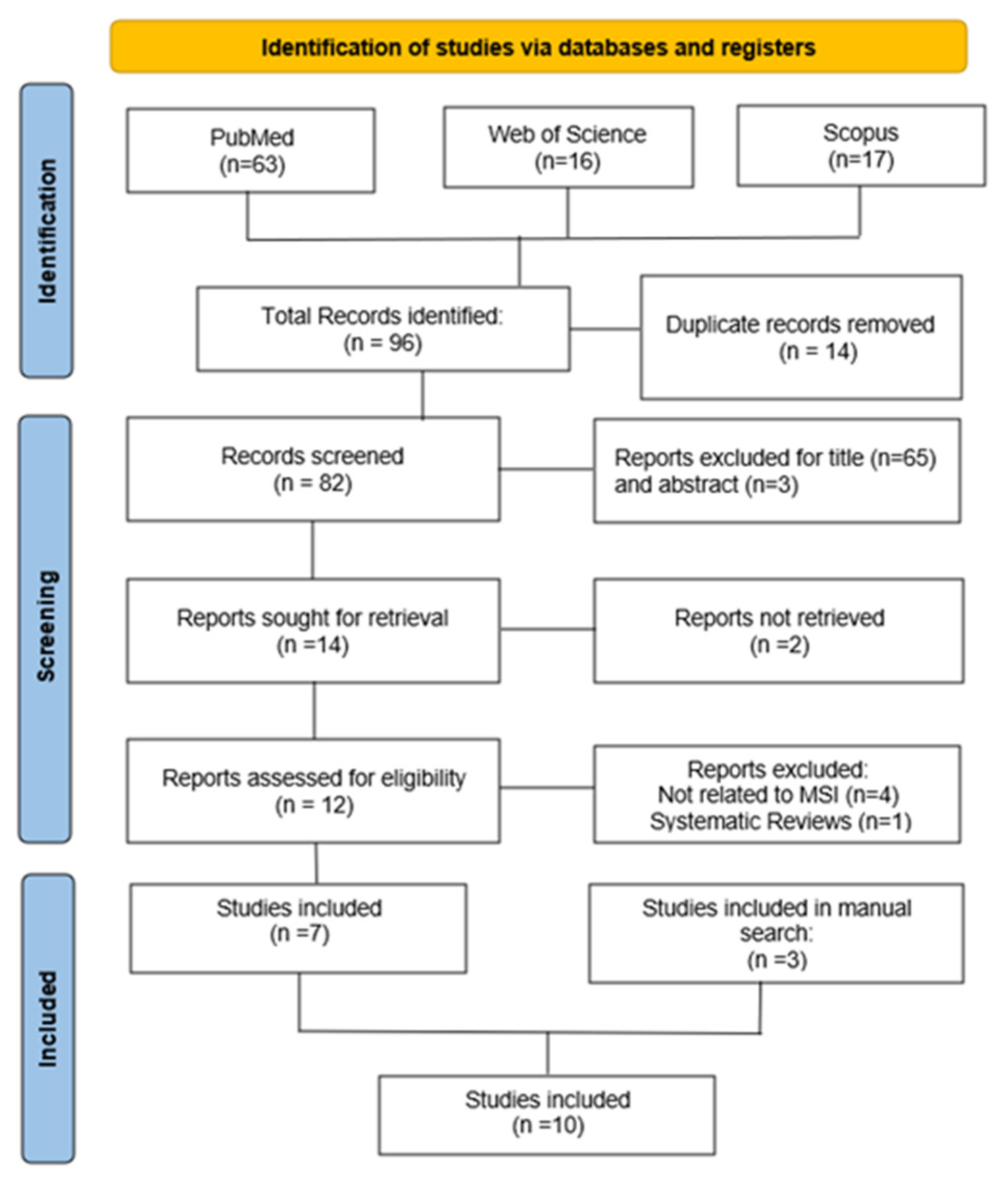
3.1. Selection of Articles
The bibliographic search identified 96 articles, of which 14 were duplicates and were excluded. After evaluating titles and abstracts, 12 articles were selected for full-text analysis. Of these, 5 were excluded based on predefined eligibility criteria, resulting in 7 articles being included in the qualitative synthesis. Including the three articles identified through manual screening, a total of 10 studies were included in the final review. This process is represented in
Figure 3.
Data extracted from the included case reports are presented in
Table 7, respectively. The quality assessment of the included studies was conducted, utilizing the Joanna Briggs Institute critical appraisal checklist for case reports [
7].
3.2. Statistical Analysis of the Data
Due to variability in reporting, not all included studies provided complete data for every variable analyzed. Consequently, percentages for specific categories (angulation, sex, outcome, follow-up period) are based only on the subset of cases where this information was explicitly reported.
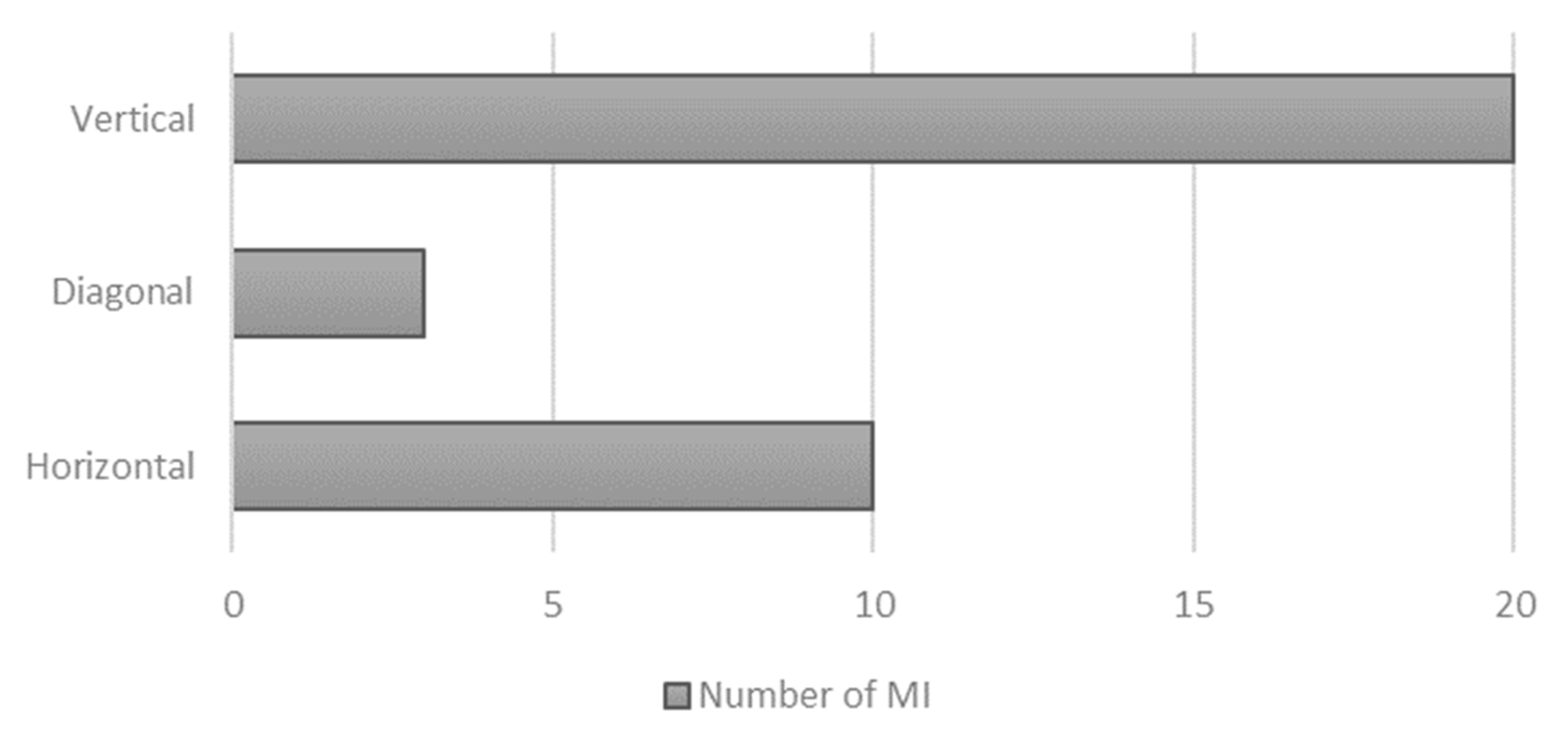
3.2.1. Angulation Distribution of Included TAD
The analysis included 11 cases extracted from published case reports, along with one additional clinical case from our own data. Of these, angulation assessment was made in 10 cases. One study (Rathi NV et al. [
11]) was excluded from this part of the analysis due to the absence of CBCT or intraoral images necessary for angulation classification.
In three of the case reports, insertion angulation was determined by performing measurements on CBCT images, following the protocol outlined in
Table 5. The results of this analysis are presented in
Table 8.
In the remaining seven case reports, measurements were taken from intraoral photographs using the protocol described in
Table 3. The results are presented in
Table 9.
Among the evaluable cases, a total of 33 TADs were analyzed. Of these, 20 TADs (60.6%) were inserted in a vertical orientation [
4,
5,
8,
12] and in the first placement in our clinical case. Three TADs (9.1%) were inserted diagonally, as reported in [
9] and in the second placement of our clinical case. The remaining 10 TADs (30.3%) were placed in a horizontal orientation [
2,
3,
10].
Figure 4 presents the distribution of TADs by angulation category.
3.2.2. Cases That Report Complications
Among the case reports included in this review, there are only three described complications during the rehabilitation process, and only two led to the subsequent replacement of the TADs. In the case report by Graham [
9], an 8 mm TAD exhibited early mobility and was replaced by a 10 mm TAD. Comparison of the periapical radiographs taken before and after replacement revealed a change in insertion angulation, with the second TAD inserted at a less vertical orientation. Although the precise angulation was not measured, this visual difference suggests that modifying the trajectory may have contributed to the improved outcome. In another case, Paquette DE [
10] replaced the TAD not due to mechanical failure, but for esthetic improvement, highlighting the importance of soft tissue management and TAD positioning in anterior zones.
Across all three cases, the replacement TADs remained stable during follow-up and achieved satisfactory functional and esthetic results. These findings underscore the importance of ongoing evaluation and the potential role of insertion angulation and TAD length in clinical success.
3.2.3. Data from Bone Change Evaluation
Bone changes could be quantitatively evaluated in only two of the included cases, as these were the only reports that provided CBCT images. The presence of CBCT allowed for accurate assessment of peri-implant bone conditions, including alveolar ridge height and thickness. In both cases, measurements suggested preservation of the alveolar dimensions following TAD placement, with no significant signs of resorption. In the study by Laino L et al. [
8], the measurements had already been performed and reported by the authors. In the study by Ciarlantini R and Melsen B [
3], the CBCT images provided were used by us to perform new measurements, calibrating our scale according to the reference ruler included in the scans. Although the original images cannot be published due to copyright restrictions,
Table 6 explains the protocol used to make these measurements.
In the study by Laino L et al. [
8], sagittal CBCT sections revealed a slight decrease in vertical bone height from 15.9 mm to 15.5 mm (−0.4 mm; −2.52%), alongside an increase in alveolar ridge thickness from 3.2 mm to 3.5 mm (+0.3 mm; +9.38%). These findings suggest overall vertical bone stability and a modest horizontal gain over the five-year follow-up period.
In the study by Ciarlantini R and Melsen B [
3], the first case showed an increase in vertical bone height from 20.96 mm to 21.39 mm (+0.43 mm; +2.05%) and in alveolar ridge thickness from 4.97 mm to 5.19 mm (+0.22 mm; +4.63%). The second case presented a decrease in both parameters, with vertical bone height decreasing from 22.46 mm to 21.41 mm (−1.05 mm; −4.68%) and ridge thickness from 4.25 mm to 4.14 mm (−0.11 mm; −2.59%).
In contrast, the remaining case reports relied solely on two-dimensional radiographs or clinical observations, which limited the ability to conduct precise quantitative assessments. Although some authors qualitatively described stable gingival contours or favorable tissue support, the lack of volumetric data reduces the strength of the evidence. This reinforces the value of incorporating CBCT in clinical follow-up when bone remodeling or preservation is a relevant outcome.
3.3. Clinical Case
This clinical case refers to a male patient who started orthodontic treatment at the age of 13, presenting with bilateral agenesis. At 14.5 years of age, the first TADs were placed to aid in the rehabilitation. The case is of particular importance to the present study, as it illustrates a complication associated with TAD rehabilitation that was successfully resolved by altering the insertion angulation. Initially, two TADs (14 × 2 mm; Kubident
®, Seville, Spain) were placed with a vertical trajectory (
Figure 5a,b;
Figure 6a), both of which eventually failed 2 months after due to mobility. Following this, 2 months after new TADs were inserted at a diagonal angulation (
Figure 5c,d;
Figure 6b), resulting in a stable and successful rehabilitation outcome (1-year follow-up). This clinical progression supports the hypothesis that TAD angulation may influence long-term stability.
4. Discussion
The present study aimed to explore the relationship between TAD insertion angulation and clinical outcomes in the temporary rehabilitation of maxillary lateral incisor agenesis. Through a systematic review of case reports and the analysis of one clinical case, relevant data were extracted regarding TAD orientation, complications, and bone remodeling outcomes.
4.1. Overview of Clinical Outcomes Across Studies
This review demonstrates that the use of TADs allows for the preservation of both crestal height and buccolingual width of the alveolar bone throughout facial growth, without requiring removal of the retainer [
2] or relying on patient compliance [
8].
All studies included in this review reported high success rates. Although the methods of evaluation varied across reports, ranging from clinical observation to radiographic assessment, the definition of success remained consistent. In all cases, successful outcomes were defined by the absence of mobility, displacement, or TAD loss throughout the observation period. While some studies also highlighted aesthetic integration and soft tissue stability as relevant considerations, these were not adopted as primary criteria for success.
The duration of follow-up varied among the included studies, ranging from a few months to as long as five years (Laino L et al. [
8]), allowing for both short-term and mid-term evaluation of outcomes. Despite this variability, the consistent absence of complications across different time frames reinforces the potential reliability of this approach. However, as shown in the reports by Graham [
9] and Paquette DE [
10], failures did occur, predominantly in vertically inserted TADs, raising questions about the role of insertion trajectory in long-term stability.
It should be noted, however, that insertion angulation is only one of several factors that may contribute to TAD failure. Rathi NV et al. [
13] reported that both the length and diameter of the TADs influence insertion torque, which in turn can significantly enhance the initial stability of the TADs. This association is exemplified in the case report by Graham [
9], where an 8 mm TAD exhibited early failure, while its replacement with a 10 mm TAD resulted in a successful and stable outcome. In our clinical case, however, the TADs used in the first unsuccessful attempt and in the subsequent successful one were of the same dimensions (14 × 2 mm; Kubident
®, Seville, Spain).
4.2. Insertion Angulation and Stability
Anterior teeth angulation and the angulation required for TAD placement in the available bone often do not coincide [
2], making it essential to plan the insertion trajectory carefully. Some authors have reported that vertically inserted TADs may interfere with the vertical development of the alveolar bone during growth, potentially limiting future prosthetic options by reducing alveolar height [
3,
10]. In contrast, horizontally placed TADs may facilitate better bone preservation but have been associated with increased plaque accumulation and greater hygiene challenges, occasionally leading to soft tissue inflammation. Nonetheless, these issues are manageable with proper hygiene instructions and regular follow-up [
10].
Our clinical case supports the hypothesis that modifying the insertion angulation—from vertical to diagonal—may lead to improved outcomes. Together, these findings suggest that insertion angulation is not merely a technical detail but a critical parameter in ensuring the long-term success of TAD-supported rehabilitation.
4.3. Bone Changes and Radiographic Evidence
Only two studies provided CBCT-based quantitative measurements of bone changes (Laino L et al. [
8] and Ciarlantini R and Melsen B [
3]), which showed overall preservation of vertical bone height. In one case, a slight horizontal gain was also recorded, reflecting favorable bone adaptation to mechanical stress.
It is also important to note that the direction of TAD insertion may influence bone remodeling patterns. For instance, one of the cases in the Ciarlantini R and Melsen B [
3] study showed a slight increase in vertical bone height (+0.43 mm), whereas the other exhibited a reduction (–1.05 mm), despite both being followed over similar periods. These variations may reflect individual differences, such as insertion angle, mechanical load, oral hygiene, or growth dynamics.
4.4. Occlusal Considerations and Prosthetic Design in TAD-Supported Restorations
In TAD-supported prosthetic rehabilitation, accurate occlusal planning and crown design are essential for maintaining device stability, promoting bone preservation, and ensuring long-term success. Avoidance of occlusal interferences is widely recognized as one of the most critical factors in preserving TAD stability, along with the physical dimensions of the screw, particularly its diameter and length [
13]. Another relevant consideration is the crown-to-screw length ratio, with a 1:1 proportion reported to favor enhanced mechanical stability [
4]. However, this is not universally applicable, as in the present case, the ratio was greater than 1:1, yet the treatment still resulted in a successful and stable outcome.
The type of prosthetic restoration also plays a significant role in the clinical outcome. Temporary crowns can be either directly screw-retained onto the mini-implant or bonded to an abutment. The screw-retained option facilitates removal and allows for future adjustments, such as color matching or repairs. Conversely, bonded crowns may offer superior initial mechanical stability, potentially reducing the risk of detachment or fracture [
11].
Further investigation is needed to determine the most suitable prosthetic configuration for use with TADs, as the design, retention modality, and associated occlusal forces appear to influence both the mechanical success and biological response of these temporary rehabilitations.
4.5. Limitations of the Available Literature
The current body of literature on the use of TADs for the temporary replacement of missing MLIA remains limited in both quantity and methodological rigor. Most of the studies included were case reports, which, although valuable for clinical insight, lack the statistical power and standardization of higher-level evidence such as randomized controlled trials. In addition, the heterogeneity across studies in terms of patient age, follow-up duration, TAD dimensions, insertion techniques, and outcome measures limits the ability to draw definitive conclusions or perform meta-analytical comparisons.
Another relevant limitation is the lack of standardized radiographic protocols. Only two studies provided CBCT-based measurements, while most relied on periapical radiographs or clinical descriptions, making it difficult to objectively assess bone remodeling. Furthermore, variations in image quality, angulation, and resolution introduce potential measurement bias. The inconsistent reporting of insertion angulation also hampers attempts to correlate angulation with clinical success or bone changes.
In many cases, outcomes were described qualitatively, without quantitative metrics such as precise bone measurements. Additionally, patient-related variables such as oral hygiene, skeletal pattern, and growth stage were rarely controlled or reported in a comparable way. These factors highlight the need for well-designed prospective studies with standardized protocols and longer follow-up periods to validate the preliminary findings observed in the available literature.
5. Conclusions
This systematic review highlights the clinical viability of using TADs for the temporary replacement of MLIA in growing patients. Across the included studies, high success rates were consistently reported, with TAD stability, defined by the absence of mobility or loss, serving as the primary outcome. Although only a limited number of cases included radiographic follow-up with CBCT, the available evidence suggests that this approach allows for the preservation of alveolar bone volume throughout facial growth.
Insertion angulation emerged as a potentially crucial factor influencing clinical success. While both vertical and horizontal orientations were shown to be effective, complications were observed more frequently in vertically inserted TADs, particularly in cases involving shorter TADs. On the other hand, horizontal insertion may present greater hygiene challenges, requiring careful follow-up and patient education.
However, the overall quality of the available literature is limited by the predominance of case reports, lack of standardization, and small sample sizes. More robust clinical trials and prospective studies are needed to confirm these findings and to explore in greater detail the biomechanical implications of TAD design, insertion trajectory, and bone remodeling patterns.
So, the temporary rehabilitation with TADs appears to be a safe and effective option for maintaining space and preserving bone in young patients, if the inserting parameters and follow-up protocols are carefully planned.
Author Contributions
T.P. conceived and designed the work, revised and finalized the manuscript, and performed the clinical case treatment. M.S. designed and conceived the review, acquired, analyzed, and interpreted the data, and drafted the initial version of the review. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by CESPU—Cooperativa de Ensino Superior Politécnico e Universitário under the grant MLIA_REAB-GI2-CESPU-2025.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. The study received ethical approval on 23 September 2021 from the Ethics Committee of University Institute of Health Sciences (Approval Number: CE/IUCS/CESPU-18/21).
Informed Consent Statement
Informed consent was obtained from the subject involved in the study.
Data Availability Statement
Data that support this study’s findings are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Pinho, T.; Tavares, P.; Maciel, P.; Pollmann, C. Developmental absence of maxillary lateral incisors in the Portuguese population. Eur. J. Orthod. 2005, 27, 443–449. [Google Scholar] [CrossRef]
- Kolge, N.E.; Patni, V.J.; Potnis, S. Semi-permanent substitution of maxillary anterior teeth: TADs supported approach. J. Indian Orthod. Soc. 2019, 53, 148–150. [Google Scholar] [CrossRef]
- Ciarlantini, R.; Melsen, B. Semipermanent replacement of missing maxillary lateral incisors by mini-implant retained pontics: A follow-up study. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Gurgel, J.A.; Tavarez, R.R.; Ursi, W.J.; Neves, M.G.; Bramante, F.S.; Pinzan-Vercelino, C.R.M. Mini-implants as provisional anchorage for the replacement of missing anterior teeth: A clinical report. J. Prosthet. Dent. 2014, 112, 706–709. [Google Scholar] [CrossRef] [PubMed]
- Cope, J.B.; McFadden, D. Temporary replacement of missing maxillary lateral incisors with orthodontic miniscrew implants in growing patients: Rationale, clinical technique, and long-term results. J. Orthod. 2014, 41 (Suppl. S1), s62–s74. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: 463 Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The 464 Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Laino, L.; Ciarlantini, R.; Melsen, B. Semi-permanent replacement of missing maxillary lateral incisors with orthodontic mini-implants: A biological approach. Mouth Teeth 2018, 2, 1–3. [Google Scholar] [CrossRef]
- Graham, J.W. Temporary replacement of maxillary lateral incisors with miniscrews and bonded pontics. J. Clin. Orthod. 2007, 41, 321–325. [Google Scholar]
- Paquette, D.E. Miniscrew-supported transitional tooth replacement: An esthetic alternative. J. Clin. Orthod. 2009, 43, 475–482. [Google Scholar]
- Wilmes, B.; Nienkemper, M.; Renger, S.; Drescher, D. Mini-implant-supported temporary pontics. J. Clin. Orthod. 2014, 48, 422–429. [Google Scholar] [PubMed]
- Kalia, A.J. Mini screw orthodontic implant as temporary crown restoration to replace unilateral missing lateral incisor post-orthodontic treatment. J. Oral Implant. 2015, 41, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Rathi, N.V.; Baliga, S.; Thosar, N.R.; Bane, S.P.; Bhansali, P. Management of hypodontia patient using a transitional implant: A case report. Int. J. Clin. Pediatr. Dent. 2023, 16, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Saha, N.; Das, M.; Santra, A.; Zahir, S. Mini-implant supported temporary replacement of teeth in children- a case report. J. Clin. Diagn. Res. 2023, 17, ZD16–ZD18. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).