Development of a Powered Four-Bar Prosthetic Hip Joint Prototype
Abstract
1. Introduction
2. Materials and Methods
2.1. Design Requirements
- Ideally, the powered hip allows a hip-level amputee to walk with similar kinematics and kinetics as a transfemoral amputee. The Össur Power Knee 2 DC motor provides up to a 96 N-m torque, 300°/s angular velocity, and 503 W power. These motor specifications can achieve transfemoral amputee gait performance [27,56,66].
- Device mass should not exceed 3.2 kg with the motor and battery included. The Össur Power Knee 2 (the prosthetic knee containing the actuator used in the novel powered hip) has a mass of 3.2 kg [17].
- Device length, width, and height must each be less than 17 cm in neutral position. The 75th percentile American male, in the year 2000, had a 17 cm thigh diameter [67].
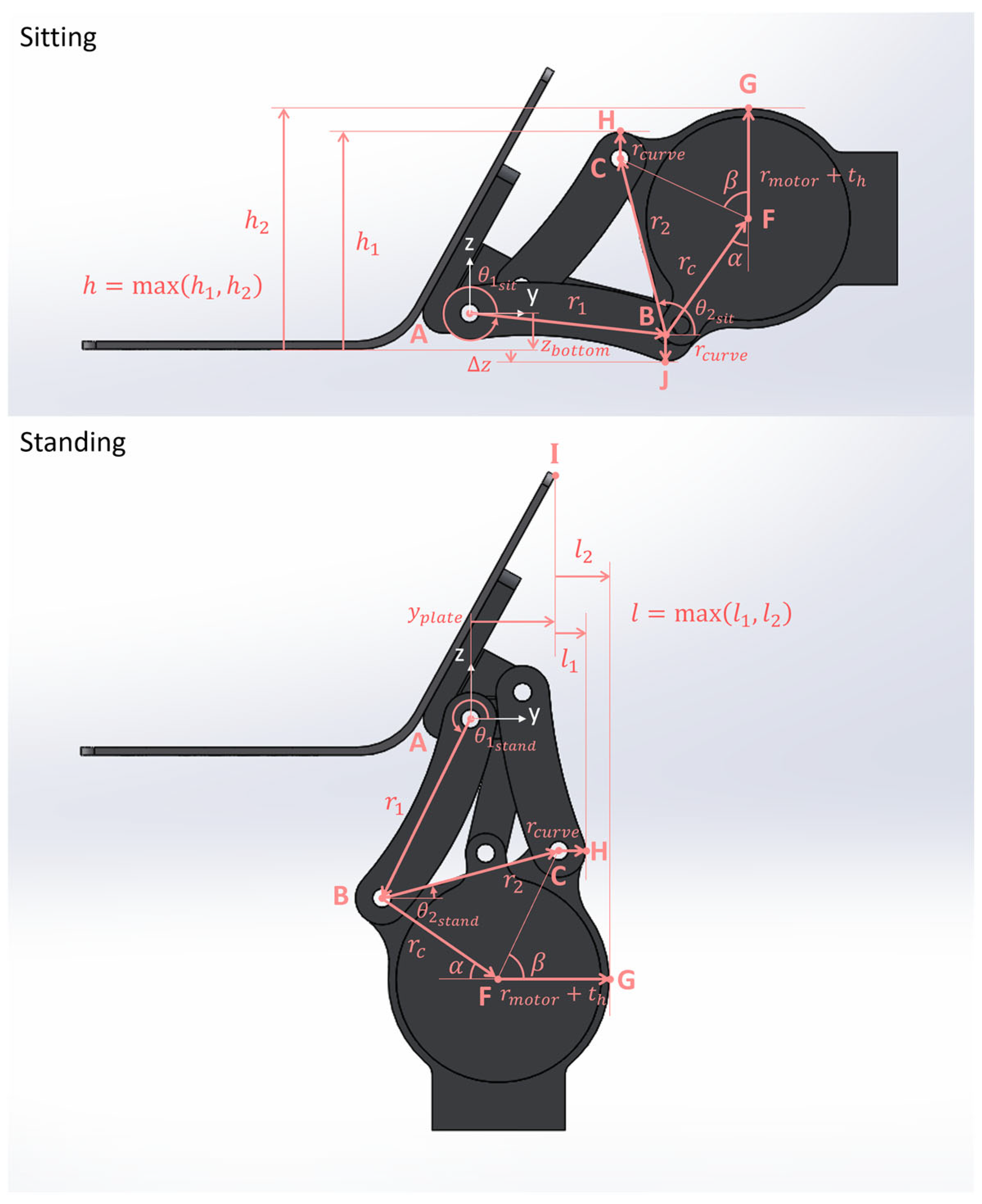
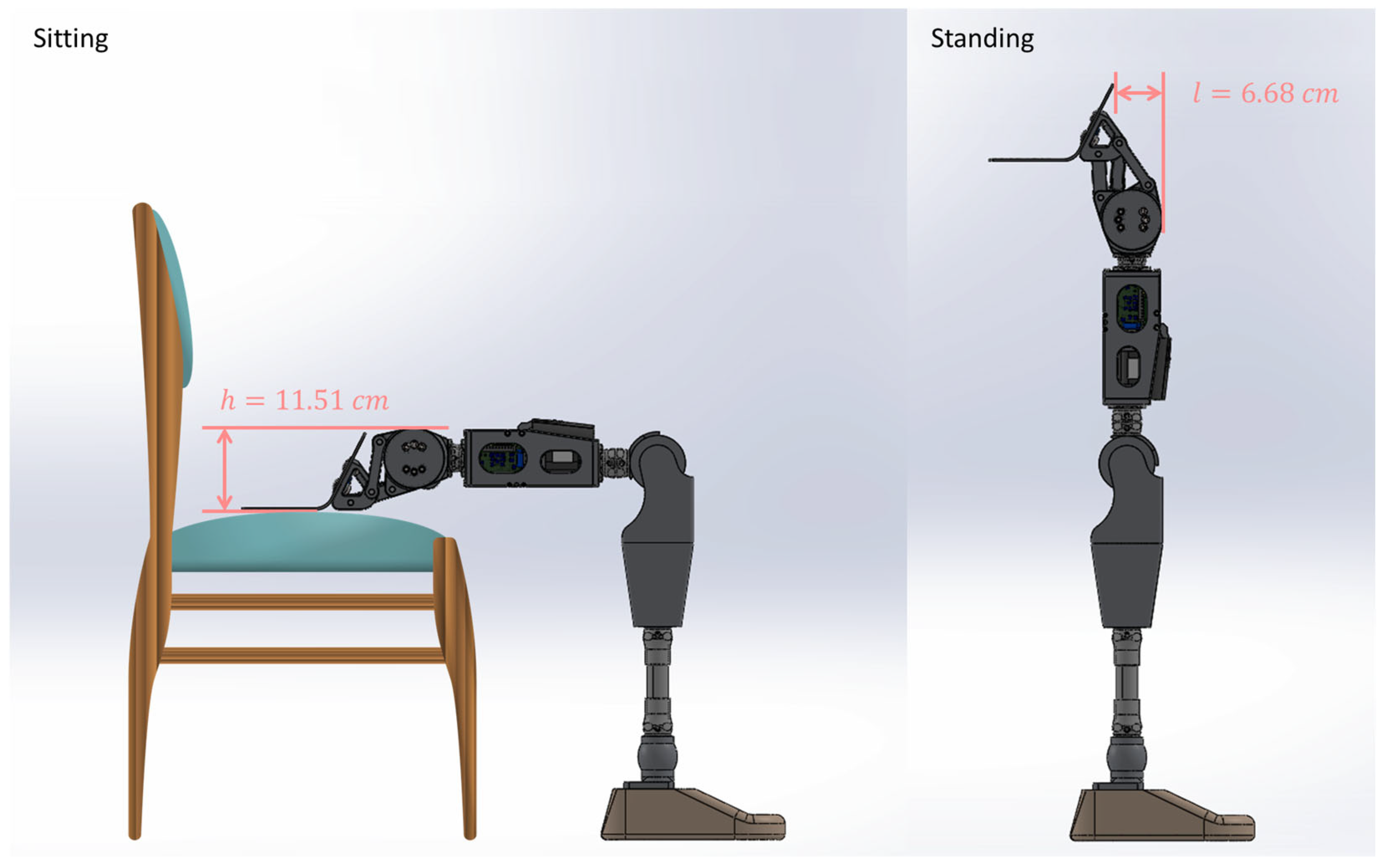
- For optimal cosmesis, the powered hip prosthesis must fit inside the user’s clothing. There must also be no protrusion below the bottom surface of the pelvic socket in the sitting position (comfortable sitting).
- To assist with ground clearance, the powered hip must shorten at mid-swing. Increased ground clearance reduces fall risk.
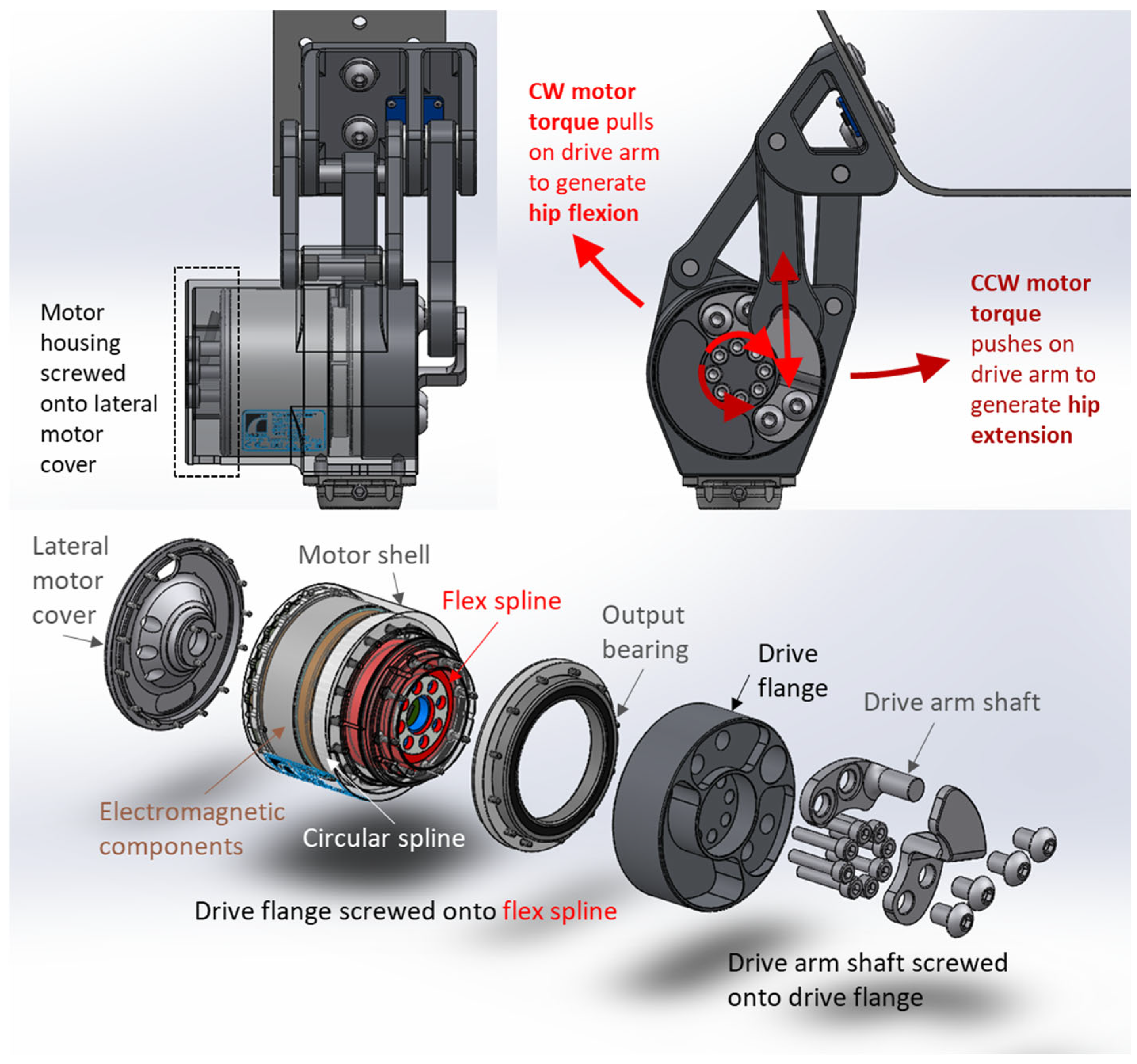
2.2. Prosthetic Hip Joint Design
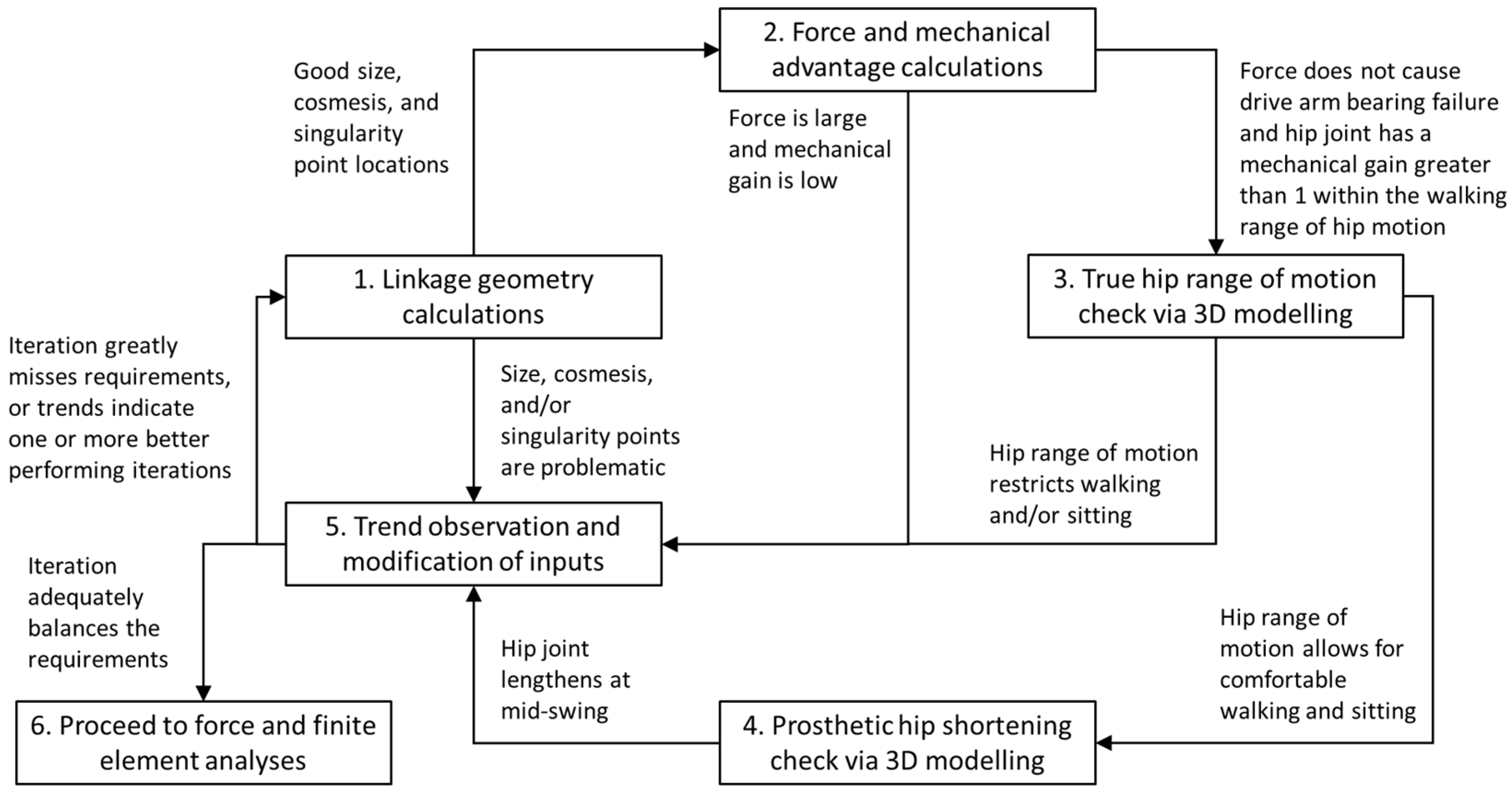
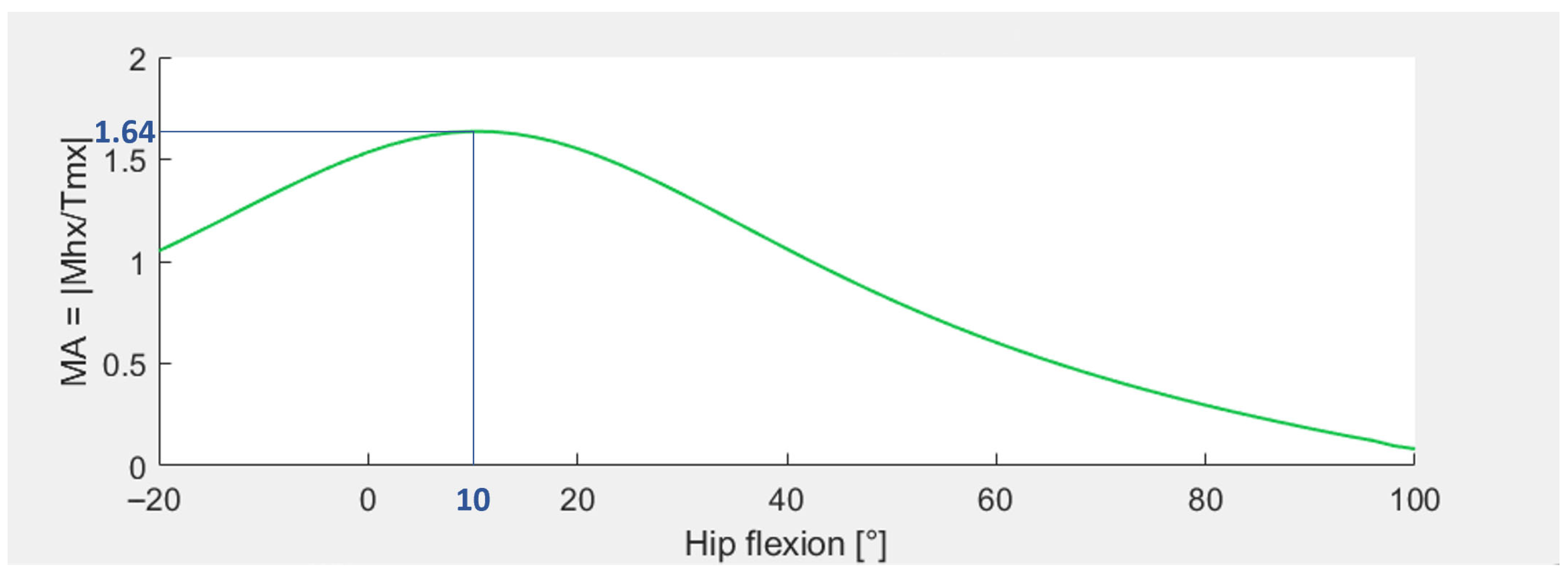
2.3. Four-Bar Linkage Optimization
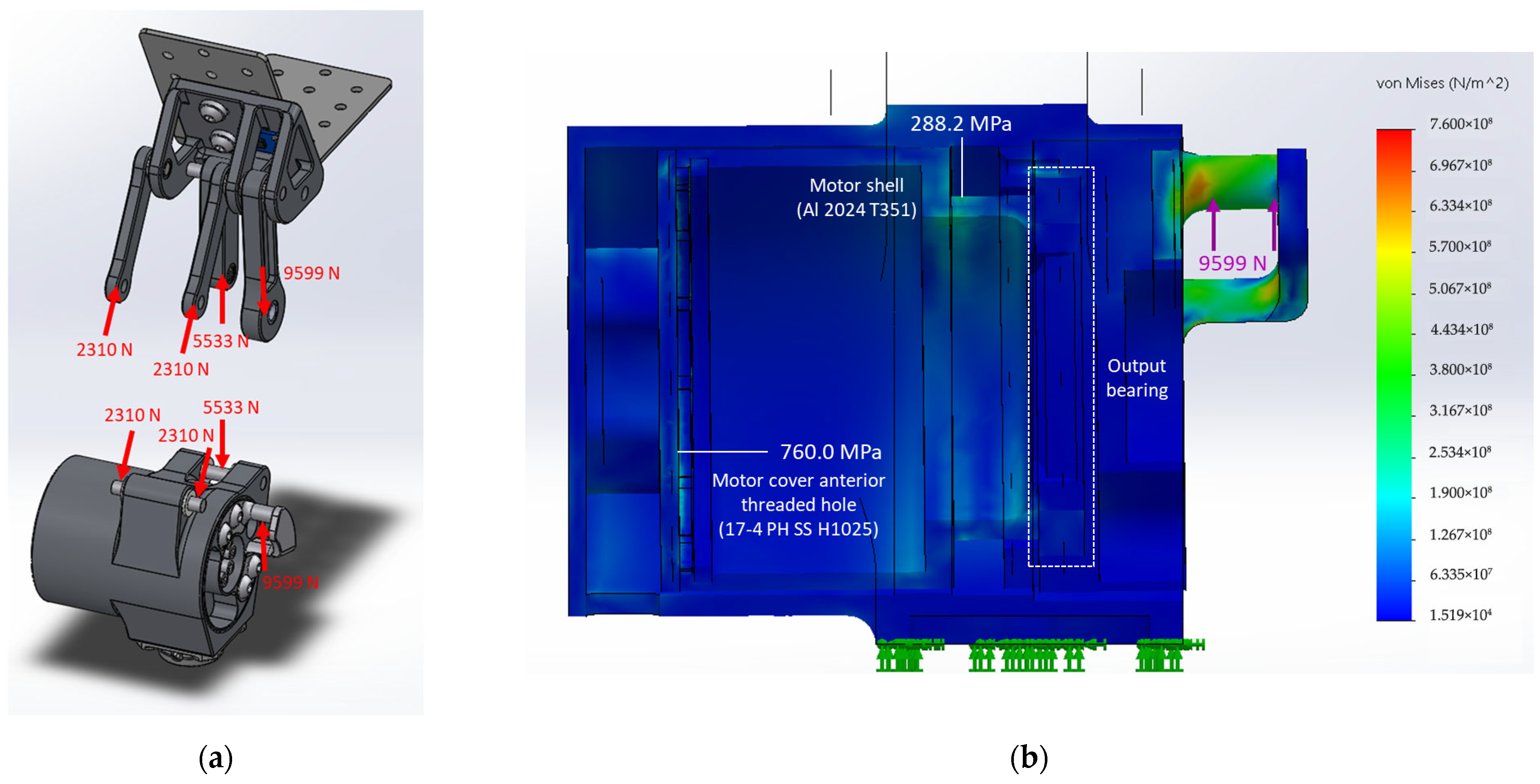
2.4. Force and Finite Element Analyses
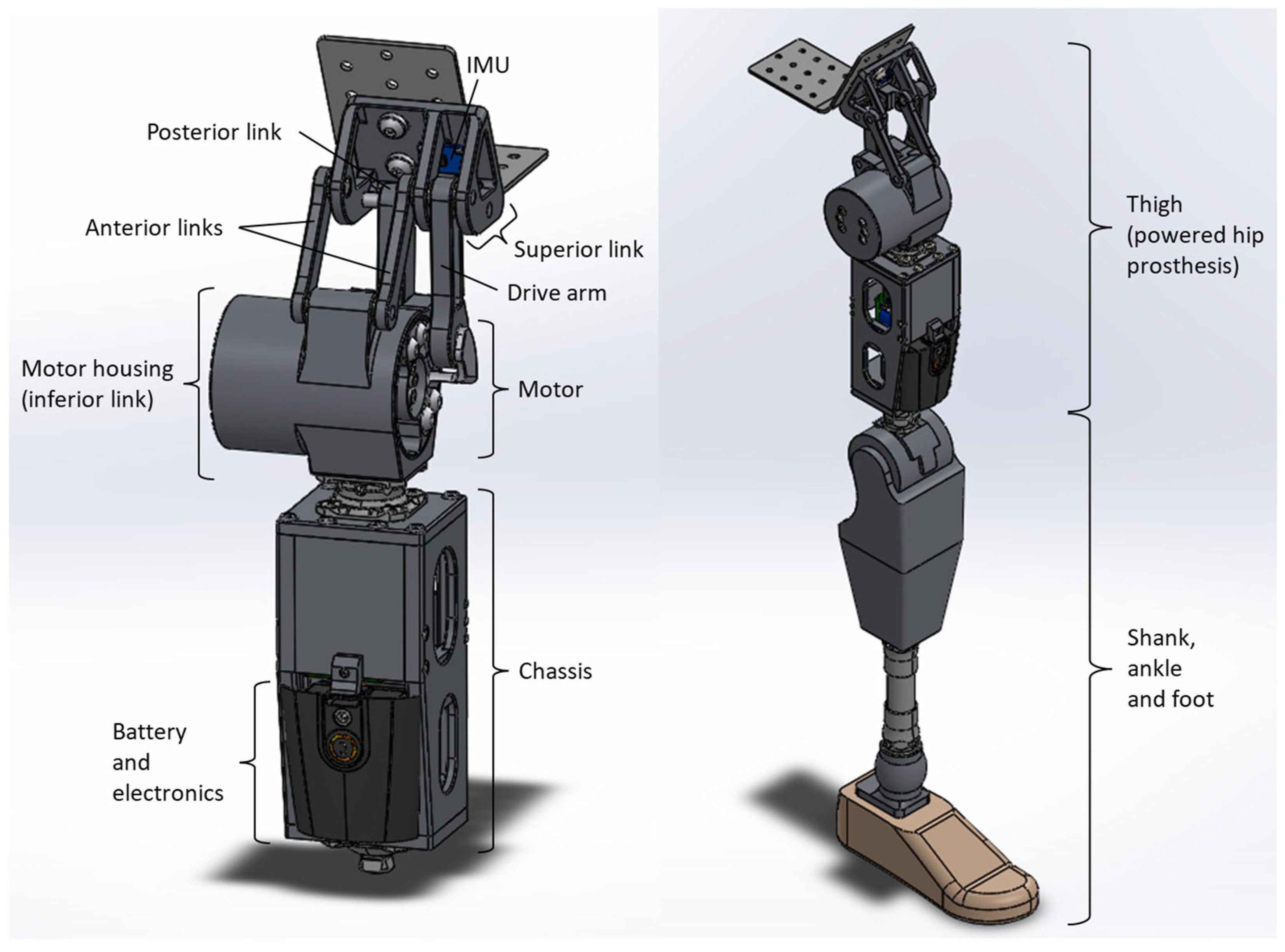
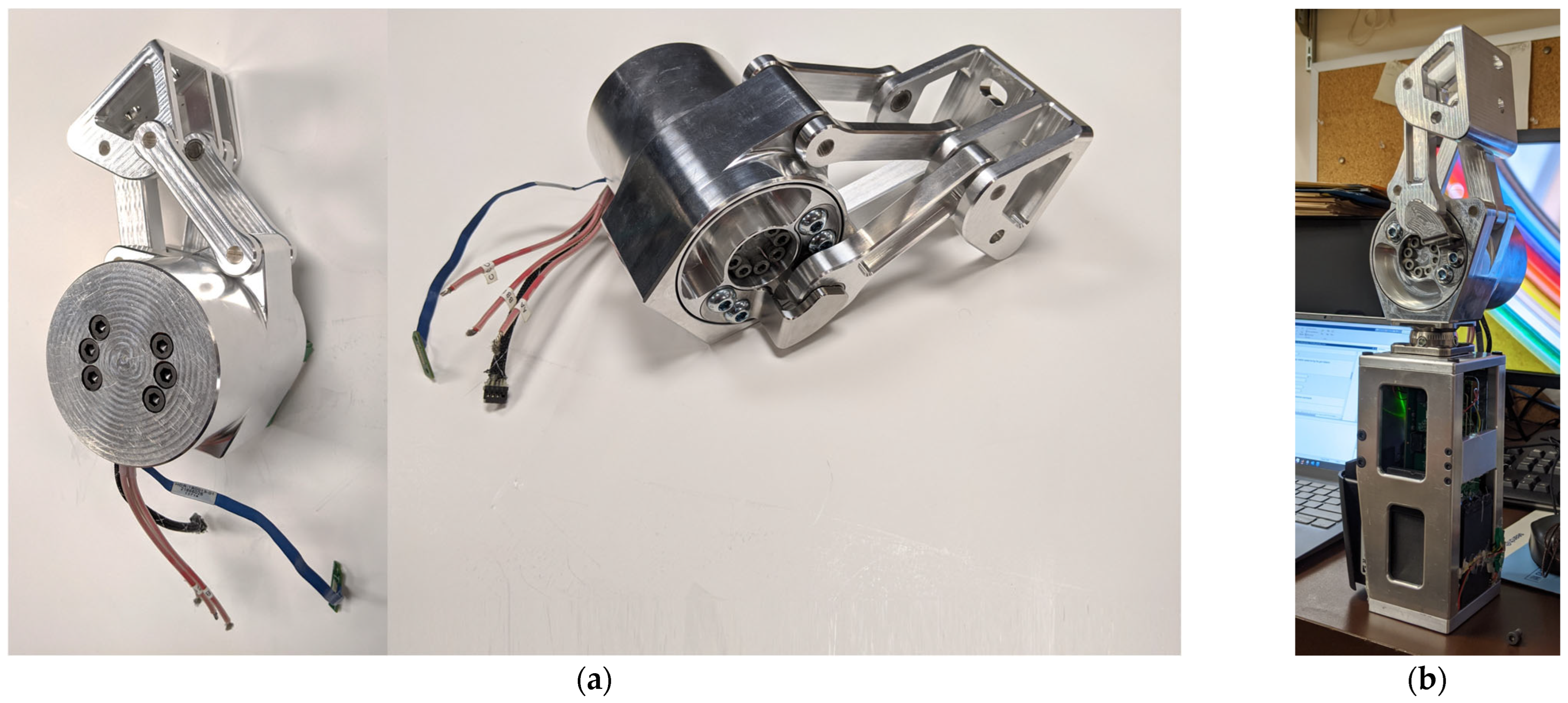
2.5. Prototype
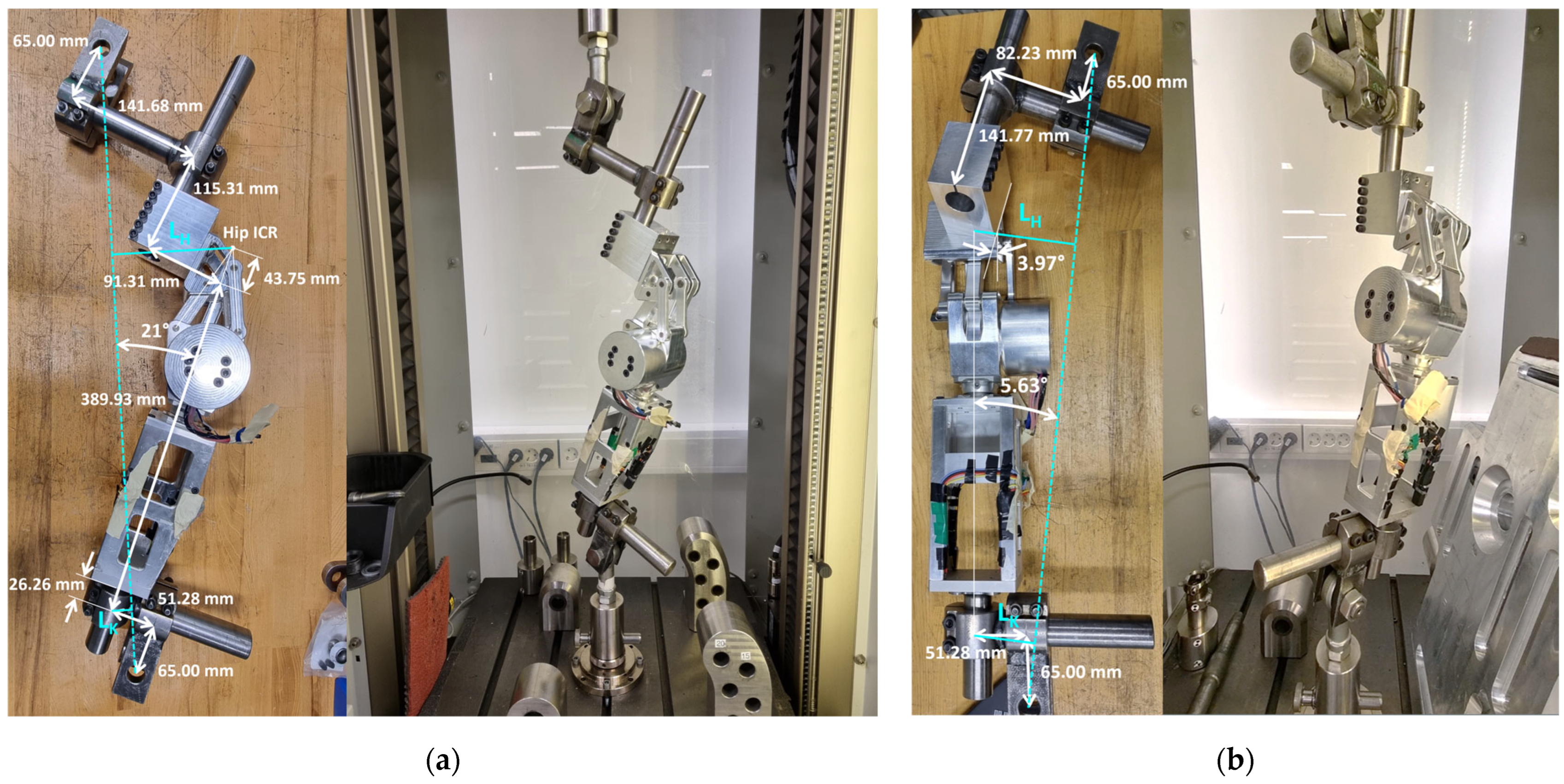
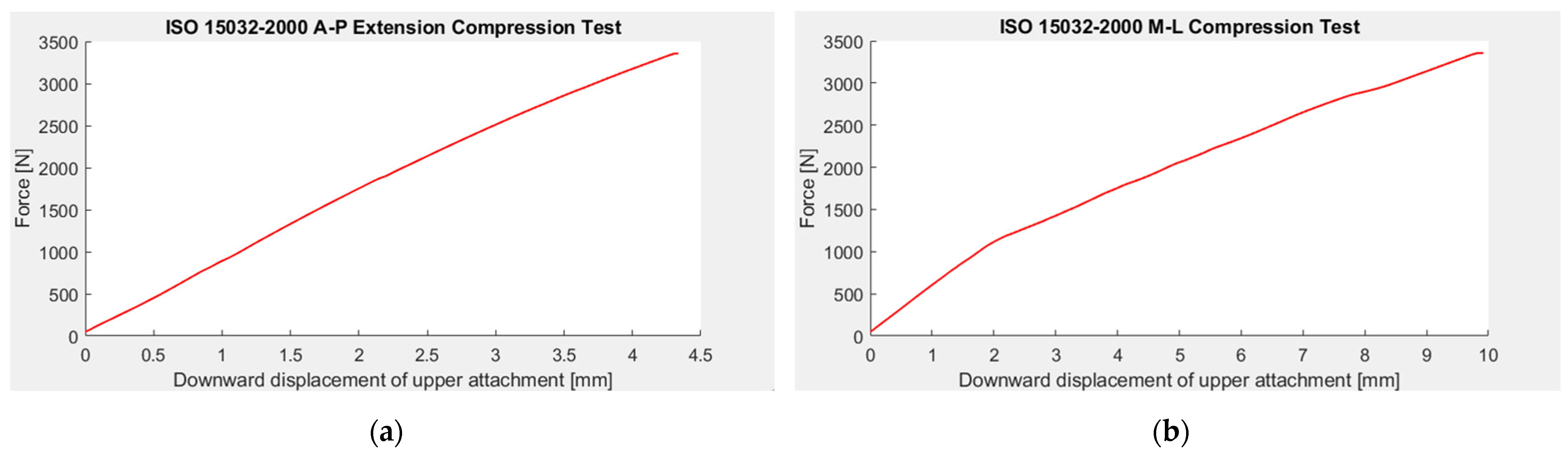
2.6. Structural Tests
- Install the prosthetic thigh in the uniaxial mechanical loading machine with appropriate lever arms,
- Compress the hip to the 50 N stabilizing force,
- Compress the hip joint to the 1024 N settling force and hold the force for 30 s before off-loading to the 50 N stabilizing force,
- Compress the hip joint to the ductile failure ultimate test force of 3360 N and, when this peak force is reached, off-load the hip to the 50 N stabilizing force.
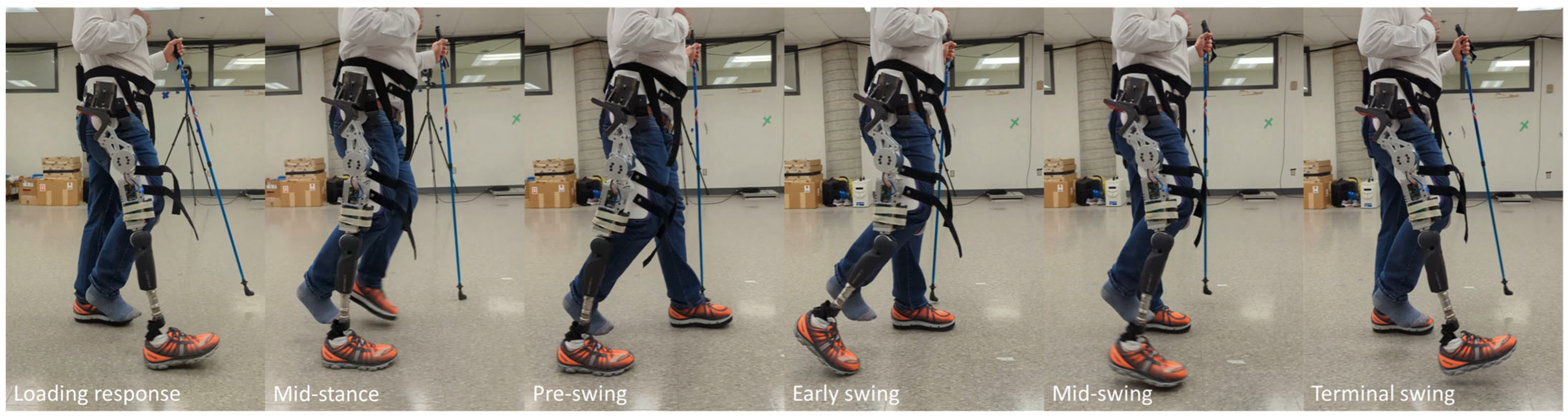
2.7. Walking Tests
2.7.1. Control System
2.7.2. Testing Protocol and Data Collection
3. Results
4. Discussion
- The powered hip was required to provide up to 20° extension and 130° flexion. The prototype met the extension criterion but was 30° short of meeting the flexion criterion. As an early prototype, 100° flexion would permit sitting, but further refinement could increase the flexion range.
- The powered hip met the 100 kg user criterion by passing the mechanical tests and successfully supporting walking for the 98 kg participant.
- The powered hip and chassis combined weight exceeded the 3.2 kg device criterion, with the prototype weighing 4.337 kg. However, participants mentioned that the powered hip did not feel heavy during walking due to the hip flexion-extension assistance the actuator provided. Although a lighter prosthetic mass would be ideal, the extra prototype mass did not greatly affect gait due to the powerful actuator implemented in the four-bar hip.
- The Össur Power Knee 2 DC motor provides a torque of up to 96 N-m, an angular velocity of up to 300°/s, and a power of up to 503 W, easily meeting the actuator criteria.
- The powered hip, from the posterosuperior pin and below but not including the chassis, needed to have a length, width, and height of less than 17 cm in neutral position. The respective powered hip neutral position dimensions are 11.61 cm, 13.48 cm, and 15.51 cm, which meet the size criteria.
- Cosmetic criteria were mostly met. The powered hip is anteriorly mounted, within the acceptable thigh dimensions, and does not protrude from the bottom in the sitting position. The slight anterior bulge of the powered hip can be reduced in future prototypes.
- During mid-swing, the powered hip was required to shorten to enhance toe clearance and reduce tripping risk. The powered hip shortens by 23.8 mm.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Equations for Step 1 of Each Iteration to Optimize Powertrain Linkages
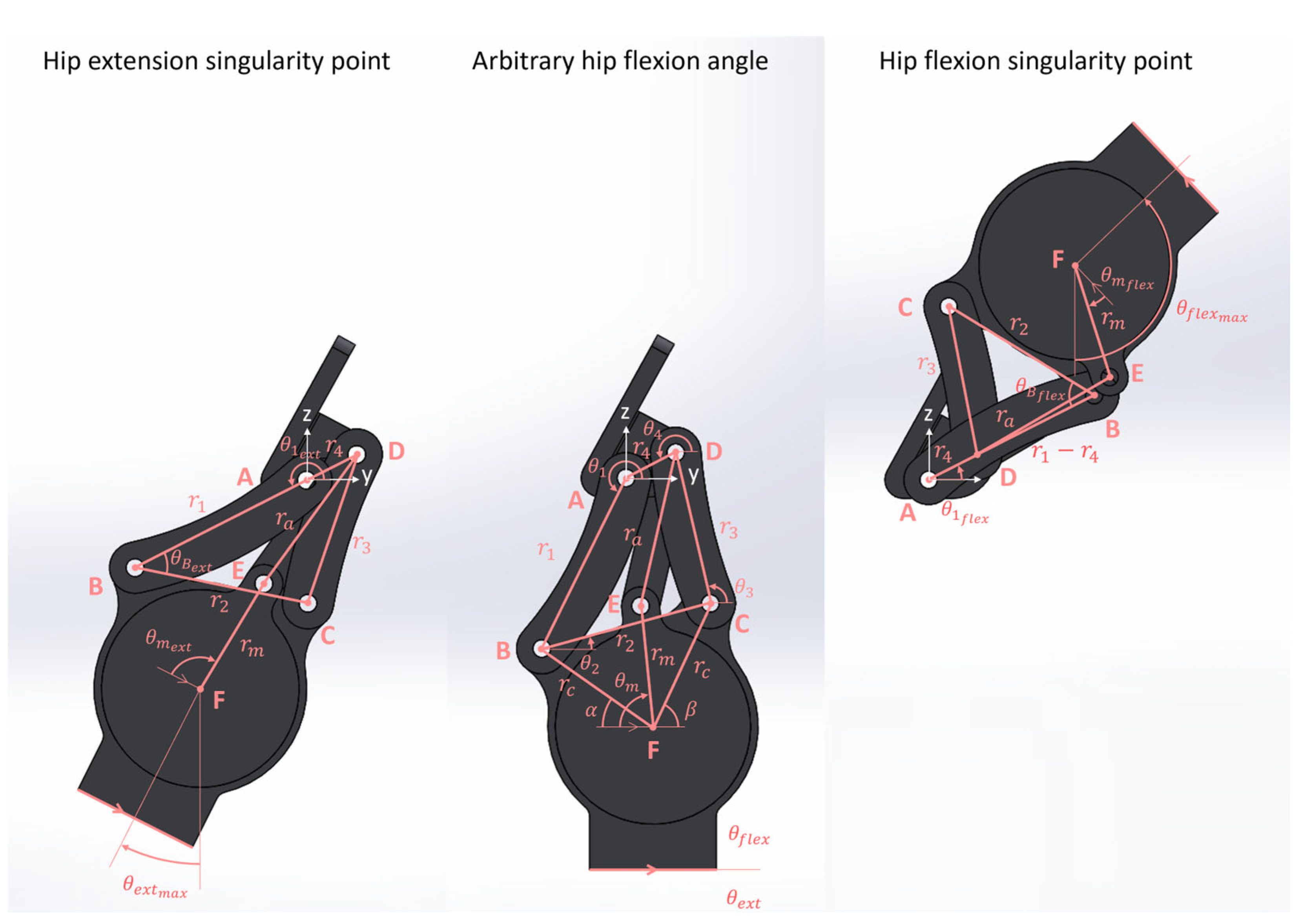
| Inputs (°) 1 | Outputs (cm) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| >21.0 | >131.0 | >152.0 | <9.30 | <9.30 | <9.30 | >2.15 and <3.37 | <2.00 | <17.00 | ≥0.00 |
| Inputs (°) 1 | Outputs (cm) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 36.5 | 109.5 | 89.1 | −39.0 | 6.1224 | 7.0854 | 8.2285 | 3.2739 | 6.0667 | 11.5240 | 1.9915 |
Appendix A.2. Equations for Step 2 of Each Iteration to Optimize Powertrain Linkages
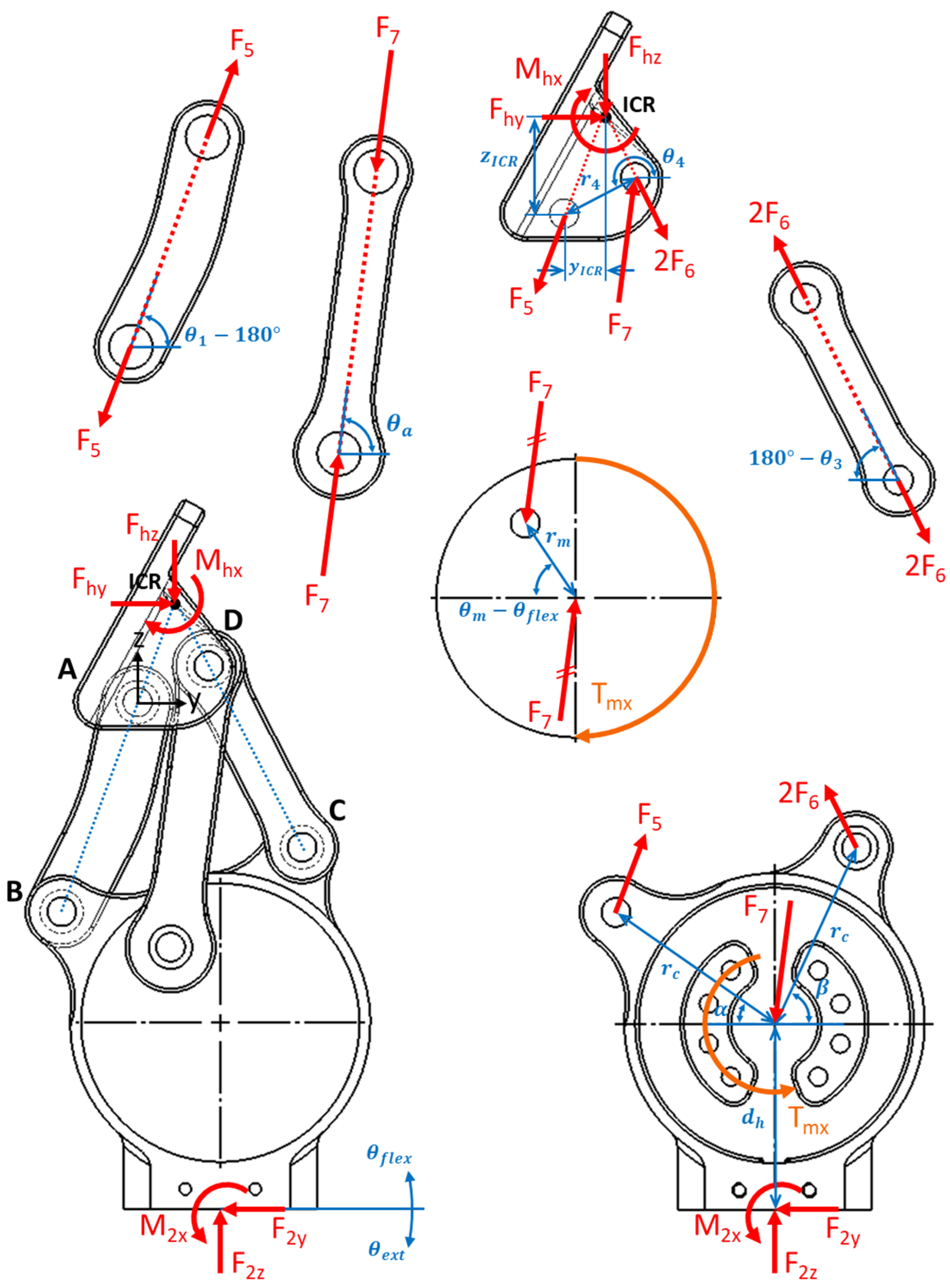
- Starting from full extension, the hip moved through its ROM to full flexion, while maintaining static equilibrium.
- There was no pelvic tilt, pelvic obliquity, or pelvic rotation at any instance within hip ROM.
- Forces acted in the sagittal plane only.
- Motor torque was constant at its maximum 96 N-m (torque direction did not affect force and moment magnitudes (only their signs) so long as free body diagram conventions were respected).
- All motor torque was transmitted through the drive arm with force .
- Body weight was not acting on the joint. Force analysis showed that the single 96 N-m torque at full hip extension was a greater load than the greatest combined body weight and motor torque expected during walking [74].
- Individual component weights and inertial loads were neglected because they were much smaller compared to body weight and motor torque.
References
- Fite, K.B. Overview of the Components Used in Active and Passive Lower-Limb Prosthetic Devices. In Full Stride: Advancing the State of the Art in Lower Extremity Gait Systems; Tepe, V., Peterson, C.M., Eds.; Springer: New York, NY, USA, 2017; pp. 55–74. ISBN 978-1-4939-7247-0. [Google Scholar]
- Helix3D Hip Joint, Right | Hips | Lower Limb Prosthetics | Prosthetics | Ottobock CA Shop. Available online: https://shop.ottobock.ca/en/Prosthetics/Lower-Limb-Prosthetics/Hips/Helix3D-Hip-Joint%2C-right/p/7E10~5R#product-specification-section (accessed on 7 December 2022).
- C-Leg 4. Available online: https://www.ottobock.com/en-us/product/3C88-3~23C98-3 (accessed on 7 December 2022).
- Rheo Knee®. Available online: https://www.ossur.com/en-ca/prosthetics/knees/rheo-knee (accessed on 7 December 2022).
- Power KneeTM. Available online: https://www.ossur.com/en-ca/prosthetics/knees/power-knee (accessed on 7 December 2022).
- INTUY® Knee: Motorized, Lightweight, Intuitive, Safe. Available online: https://www.rbionics.com/products/prosthetic-knee/ (accessed on 2 June 2025).
- Product | BionicM. Available online: https://bionicm.com/product (accessed on 2 June 2025).
- Empower. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Feet---Microprocessor/Empower/p/1A1-2#product-documents-section (accessed on 7 December 2022).
- Ludwigs, E.; Bellmann, M.; Schmalz, T.; Blumentritt, S. Biomechanical Differences Between Two Exoprosthetic Hip Joint Systems during Level Walking. Prosthet. Orthot. Int. 2010, 34, 449–460. [Google Scholar] [CrossRef]
- Kawaguchi, T.; Yamada, T.; Iwashita, K. Biomechanical Gait Analysis for a Hip Disarticulation Prosthesis: Power Source for the Swing Phase of a Hip Disarticulation Prosthetic Limb. J. Phys. Ther. Sci. 2023, 35, 361–365. [Google Scholar] [CrossRef]
- Gholizadeh, H.; Baddour, N.; Botros, M.; Brannen, K.; Golshan, F.; Lemaire, E.D. Hip Disarticulation and Hemipelvectomy Prostheses: A Review of the Literature. Prosthet. Orthot. Int. 2021, 45, 434–439. [Google Scholar] [CrossRef]
- Ueyama, Y.; Kubo, T.; Shibata, M. Robotic Hip-Disarticulation Prosthesis: Evaluation of Prosthetic Gaits in a Non-Amputee Individual. Adv. Robot. 2020, 34, 37–44. [Google Scholar] [CrossRef]
- Bowker, H.; Michael, J. (Eds.) Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles, 2nd ed.; American Academy of Orthopedic Surgeons: Rosemont, IL, USA, 1992. [Google Scholar]
- Chin, T.; Sawamura, S.; Shiba, R.; Oyabu, H.; Nagakura, Y.; Nakagawa, A. Energy Expenditure During Walking in Amputees after Disarticulation of the Hip: A Microprocessor-Controlled Swing-Phase Control Knee Versus a Mechanical-Controlled Stance-Phase Control Knee. J. Bone Jt. Surgery. Br. Vol. 2005, 87, 117–119. [Google Scholar] [CrossRef]
- Chin, T.; Oyabu, H.; Maeda, Y.; Takase, I.; Machida, K. Energy Consumption During Prosthetic Walking and Wheelchair Locomotion by Elderly Hip Disarticulation Amputees. Am. J. Phys. Med. Rehabil. 2009, 88, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Jeans, K.A.; Browne, R.H.; Karol, L.A. Effect of Amputation Level on Energy Expenditure During Overground Walking by Children with an Amputation. J. Bone Jt. Surg. Am. Vol. 2011, 93, 49–56. [Google Scholar] [CrossRef]
- Langlois, D. Powered Hip Joint Unexplored Clinical Opportunities of Powered Prosthetics 2015. In Proceedings of 2015 AOPA National Assembly Clinical Education Program, San Antonio, TX, USA, 7–10 October 2015. [Google Scholar]
- Nowroozi, F.; Salvanelli, M.L.; Gerber, L.H. Energy Expenditure in Hip Disarticulation and Hemipelvectomy Amputees. Arch. Phys. Med. Rehabil. 1983, 64, 300–303. [Google Scholar]
- Houdek, M.T.; Kralovec, M.E.; Andrews, K.L. Hemipelvectomy: High-Level Amputation Surgery and Prosthetic Rehabilitation. Am. J. Phys. Med. Rehabil. 2014, 93, 600–608. [Google Scholar] [CrossRef]
- Modular Hip Joint- Free Motion- | Hips | Lower Limb Prosthetics. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Hips/Modular-Hip-Joint--Free-Motion-/p/7E4 (accessed on 20 February 2023).
- Modular Single Axis Hip Joint. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Hips/Modular-Single-Axis-Hip-Joint/p/7E5~5R (accessed on 20 February 2023).
- Modular Hip Joint Free Mot. Titan | Hips | Lower Limb Prosthetics | Prosthetics | Ottobock CA Shop. Available online: https://shop.ottobock.ca/en/Prosthetics/Lower-Limb-Prosthetics/Hips/Modular-Hip-Joint-Free-Mot-Titan/p/7E7 (accessed on 18 January 2023).
- Modular Hip Joint-Child. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Pediatric-Prosthetics/Pediatric-Hip-Joints/Modular-Hip-Joint-Child/p/7E8#product-documents-section (accessed on 20 February 2023).
- Hydraulic Hip Joint. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Hips/Hydraulic-Hip-Joint/p/7E9 (accessed on 20 February 2023).
- Four Axis Hip Joint 7E6. Available online: https://www.wonderful-po.com/7e6-product/ (accessed on 26 February 2025).
- Blumentritt, S.; Ludwigs, E.; Bellmann, M.; Boiten, H. The New Helix3D Hip Joint. Orthopädie Tech. 2008, 59, 345–349. [Google Scholar]
- Segal, A.D.; Orendurff, M.S.; Klute, G.K.; McDowell, M.L.; Pecoraro, J.A.; Shofer, J.; Czerniecki, J.M. Kinematic and Kinetic Comparisons of Transfemoral Amputee Gait Using C-Leg and Mauch SNS Prosthetic Knees. J. Rehabil. Res. Dev. 2006, 43, 857–870. [Google Scholar] [CrossRef]
- Camargo, J.; Ramanathan, A.; Flanagan, W.; Young, A. A Comprehensive, Open-Source Dataset of Lower Limb Biomechanics in Multiple Conditions of Stairs, Ramps, and Level-Ground Ambulation and Transitions. J. Biomech. 2021, 119, 110320. [Google Scholar] [CrossRef] [PubMed]
- Radcliffe, C.W. Above-Knee Prosthetics. Prosthet. Orthot. Int. 1977, 1, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Radcliffe, C.W. Four-Bar Linkage Prosthetic Knee Mechanisms: Kinematics, Alignment and Prescription Criteria. Prosthet. Orthot. Int. 1994, 18, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Zarrugh, M.Y.; Radcliffe, C.W. Simulation of Swing Phase Dynamics in Above-Knee Prostheses. J. Biomech. 1976, 9, 283–292. [Google Scholar] [CrossRef]
- Radcliffe, C.W. Biomechanics of Knee Stability Control with Four-Bar Prosthetic Knees. In Proceedings of the ISPO Australia Annual Meeting, Melbourne, Australia, 27–29 November 2003. [Google Scholar]
- Chauhan, S.S.; Khare, A.K. Analysis of Four-Bar Linkages Suitable for Above-Knee Prosthesis. Evergreen 2022, 9, 737–744. [Google Scholar] [CrossRef]
- 7E10 Helix3D Instructions for Use 2022. Available online: https://shop.ottobock.ca/en/Prosthetics/Lower-Limb-Prosthetics/Hips/Helix3D-Hip-Joint%2C-right/p/7E10~5R#product-documents-section (accessed on 8 February 2023).
- Marisami, P.; Venkatachalam, R. Towards Optimal Toe-Clearance in Synthesizing Polycentric Prosthetic Knee Mechanism. Comput. Methods Biomech. Biomed. Eng. 2022, 25, 656–667. [Google Scholar] [CrossRef]
- Mohanty, R.K.; Mohanty, R.C.; Sabut, S.K. A Systematic Review on Design Technology and Application of Polycentric Prosthetic Knee in Amputee Rehabilitation. Phys. Eng. Sci. Med. 2020, 43, 781–798. [Google Scholar] [CrossRef]
- Nelson, L.M.; Carbone, N.T. Functional Outcome Measurements of a Veteran With a Hip Disarticulation Using a Helix 3D Hip Joint: A Case Report. JPO J. Prosthet. Orthot. 2011, 23, 21–26. [Google Scholar] [CrossRef]
- Pfeifer, S.; Riener, R.; Vallery, H. An Actuated Transfemoral Prosthesis with Optimized Polycentric Knee Joint. In Proceedings of the 2012 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; pp. 1807–1812. [Google Scholar] [CrossRef]
- Wolf, E.J.; Everding, V.Q.; Linberg, A.L.; Schnall, B.L.; Czerniecki, J.M.; Gambel, J.M. Assessment of Transfemoral Amputees Using C-Leg and Power Knee for Ascending and Descending Inclines and Steps. J. Rehabil. Res. Dev. 2012, 49, 831–842. [Google Scholar] [CrossRef]
- Wolf, E.J.; Everding, V.Q.; Linberg, A.A.; Czerniecki, J.M.; Gambel, C.J.M. Comparison of the Power Knee and C-Leg During Step-up and Sit-to-Stand Tasks. Gait Posture 2013, 38, 397–402. [Google Scholar] [CrossRef]
- Highsmith, M.J.; Kahle, J.T.; Carey, S.L.; Lura, D.J.; Dubey, R.V.; Quillen, W.S. Kinetic Differences Using a Power Knee and C-Leg While Sitting Down and Standing Up: A Case Report. JPO J. Prosthet. Orthot. 2010, 22, 237–243. [Google Scholar] [CrossRef]
- Laferrier, J.; Gailey, R. Advances in Lower-Limb Prosthetic Technology. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 87–110. [Google Scholar] [CrossRef]
- Chiriac, O.A.; Bucur, D. From Conventional Prosthetic Feet to Bionic Feet: A Review. In International Conference of Mechatronics and Cyber—MixMechatronics—2020; Gheorghe, G.I., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 130–138. [Google Scholar]
- Hitt, J.K.; Bellman, R.; Holgate, M.; Sugar, T.G.; Hollander, K.W. The Sparky (Spring Ankle with Regenerative Kinetics) Project: Design and Analysis of a Robotic Transtibial Prosthesis with Regenerative Kinetics. Am. Soc. Mech. Eng. 2008, 5, 1587–1596. [Google Scholar]
- Au, S.K.; Herr, H.; Weber, J.; Martinez-Villalpando, E.C. Powered Ankle-Foot Prosthesis for the Improvement of Amputee Ambulation. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 23–26 August 2007; pp. 3020–3026. [Google Scholar]
- Novelli, G.L.; Andrade, R.M. Towards an Active Ankle-Foot Prosthesis Powered by Dielectric Elastomer Actuators in Antagonistic Pairs. In Proceedings of the 2021 International Symposium on Medical Robotics (ISMR), Atlanta, GA, USA, 17–19 November 2021; pp. 1–6. [Google Scholar]
- Huang, Q.; Li, B.; Jia, F.; Wang, P. A Novel Design of Electro-Hydraulic Driven Active Powered Ankle-Foot Prosthesis. In Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer: Heidelberg, Germany, 2021; Volume 13013, pp. 622–630. [Google Scholar] [CrossRef]
- Poliakov, A.; Ryzhkov, A.; Kolesova, M.; Shtanko, P.; Sopin, P.; Bugayov, P. Novel Design of an Active Transfemoral Prosthesis with Intellectual-Synergetic Control System. In Proceedings of the 2020 International Conference on Electrical, Communication, and Computer Engineering (ICECCE), Istanbul, Turkey, 12–13 June 2020; pp. 1–6. [Google Scholar]
- Jiang, Y.; An, H.; Liu, Y.; Huang, Y.; Ma, H.; Wei, Q. An Active-Passive Lightweight Prosthesis Simulating Normal Human Walking Gait. In Proceedings of the 2022 6th International Conference on Robotics and Automation Sciences (ICRAS), Virtual, 9–11 June 2022; pp. 157–161. [Google Scholar]
- Hafner, B.J.; Askew, R.L. Physical Performance and Self-Report Outcomes Associated with Use of Passive, Adaptive, and Active Prosthetic Knees in Persons with Unilateral, Transfemoral Amputation: Randomized Crossover Trial. J. Rehabil. Res. Dev. 2015, 52, 677–700. [Google Scholar] [CrossRef] [PubMed]
- Fan, M.; Chen, Y.; He, B.; Meng, Q.; Yu, H. Study on Adaptive Adjustment of Variable Joint Stiffness for a Semi-Active Hip Prosthesis. In Intelligent Robotics and Applications; Liu, H., Yin, Z., Liu, L., Jiang, L., Gu, G., Wu, X., Ren, W., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 13–23. [Google Scholar]
- Song, M.; Guo, S.; Wang, X.; Qu, H. Dynamic Analysis and Performance Verification of a Novel Hip Prosthetic Mechanism. Chin. J. Mech. Eng. Engl. Ed. 2020, 33, 17. [Google Scholar] [CrossRef]
- Langlois, D. Power Hip Proof-of-Concept Testing—Technical Brief, Version 1.0; Össur: Reykjavik, Iceland, 2012; pp. 1–6. [Google Scholar]
- Brannen, K.; Baddour, N.; Cho, L.; Langlois, D.; Dumond, P.; Lemaire, E. Development and Evaluation of an Anteriorly Mounted Microprocessor-Controlled Powered Hip Joint Prosthesis. Can. Prosthet. Orthot. J. 2024, 7, 44494. [Google Scholar] [CrossRef] [PubMed]
- Mroz, S.; Baddour, N.; Dumond, P.; Lemaire, E.D. Design and Prototype Validation of a Laterally Mounted Powered Hip Joint Prothesis. J. Rehabil. Assist. Technol. Eng. 2024, 11, 1–16. [Google Scholar] [CrossRef]
- Harandi, V.J.; Ackland, D.C.; Haddara, R.; Lizama, L.E.C.; Graf, M.; Galea, M.P.; Lee, P.V.S. Gait Compensatory Mechanisms in Unilateral Transfemoral Amputees. Med. Eng. Phys. 2020, 77, 95–106. [Google Scholar] [CrossRef]
- Hood, S.; Ishmael, M.K.; Gunnell, A.; Foreman, K.B.; Lenzi, T. A Kinematic and Kinetic Dataset of 18 Above-Knee Amputees Walking at Various Speeds. Sci. Data 2020, 7, 150. [Google Scholar] [CrossRef]
- Mulholland, S.J.; Wyss, U.P. Activities of Daily Living in Non-Western Cultures: Range of Motion Requirements for Hip and Knee Joint Implants. Int. J. Rehabil. Res. 2001, 24, 191–198. [Google Scholar] [CrossRef]
- Kaufman, K.R.; Frittoli, S.; Frigo, C.A. Gait Asymmetry of Transfemoral Amputees Using Mechanical and Microprocessor-Controlled Prosthetic Knees. Clin. Biomech. 2012, 27, 460–465. [Google Scholar] [CrossRef]
- Brandt, A.; Wen, Y.; Liu, M.; Stallings, J.; Huang, H.H. Interactions Between Transfemoral Amputees and a Powered Knee Prosthesis During Load Carriage. Sci. Rep. 2017, 7, 14480. [Google Scholar] [CrossRef]
- Pinheiro, C.; Lopes, J.M.; Moreira, L.; Sanz-Merodio, D.; Figueiredo, J.; Santos, C.P.; Garcia, E. Kinematic and Kinetic Study of Sit-to-Stand and Stand-to-Sit Movements towards a Human-like Skeletal Model. In Proceedings of the 2019 IEEE 6th Portuguese Meeting on Bioengineering (ENBENG), Lisbon, Portugal, 22–23 February 2019; pp. 1–4. [Google Scholar]
- De Pauw, K.; Serrien, B.; Baeyens, J.-P.; Cherelle, P.; De Bock, S.; Ghillebert, J.; Bailey, S.P.; Lefeber, D.; Roelands, B.; Vanderborght, B.; et al. Prosthetic Gait of Unilateral Lower-Limb Amputees with Current and Novel Prostheses: A Pilot Study. Clin. Biomech. 2020, 71, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Kowal, M.; Winiarski, S.; Gieysztor, E.; Kołcz, A.; Walewicz, K.; Borowicz, W.; Rutkowska-Kucharska, A.; Paprocka-Borowicz, M. Symmetry Function in Gait Pattern Analysis in Patients after Unilateral Transfemoral Amputation Using a Mechanical or Microprocessor Prosthetic Knee. J. Neuroeng. Rehabil. 2021, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Fryar, C.D.; Gu, Q.; Ogden, C.L. Anthropometric Reference Data for Children and Adults: United States, 2007–2010. Vital Health Stat. 2012, 252, 1–48. [Google Scholar]
- ISO 15032; Prostheses. Structural Testing of Hip Joints. International Organization for Standardization: Geneva, Switzerland, 2000; ISBN 978-0-580-34965-2.
- Kobayashi, T.; Hisano, G.; Namiki, Y.; Hashizume, S.; Hobara, H. Walking Characteristics of Runners with a Transfemoral or Knee-Disarticulation Prosthesis. Clin. Biomech. 2020, 80, 105132. [Google Scholar] [CrossRef]
- National Aeronautics and Space Administration (NASA). Man-Systems Integration Standards—NASA STD 3000—Anthropometry and Biomechanics; NASA: Washington, DC, USA, 1995; Volume 1.
- The Solution for 3D CAD, Design and Product Development | SOLIDWORKS. Available online: https://www.solidworks.com/ (accessed on 28 April 2025).
- Bader, Y.; Langlois, D.; Baddour, N.; Lemaire, E.D. Development of an Integrated Powered Hip and Microprocessor-Controlled Knee for a Hip–Knee–Ankle–Foot Prosthesis. Bioengineering 2023, 10, 614. [Google Scholar] [CrossRef]
- Fanous, A. Hip Disarticulation Prosthesis Simulator; University of Ottawa: Ottawa, ON, Canada, 2021. [Google Scholar]
- Newport 3—Unique Patented Disk Technology Adjusts Easily for Hip Development. Available online: https://www.orthomerica.com/products/newport/newport-3/ (accessed on 23 October 2023).
- Pro-Flex® ST Waterproof Prosthetic Foot. Available online: https://www.ossur.com/en-ca/prosthetics/feet/pro-flex-st (accessed on 23 October 2023).
- Kinovea. Available online: https://www.kinovea.org/ (accessed on 26 February 2025).
- Botros, M. Design and Evaluation of a Powered Four-Bar Prosthetic Hip Joint; University of Ottawa: Ottawa, ON, Canada, 2024. [Google Scholar]
- MatWeb Aluminum 2024-T4; 2024-T351. Available online: http://www.matweb.com/search/datasheet_print.aspx?matguid=67d8cd7c00a04ba29b618484f7ff7524 (accessed on 8 March 2021).
- 17-4 PH Stainless Steel Bar—17-4 ASTM A564 Supplier | Best Stainless. Available online: https://www.beststainless.com/17-4-ph-stainless-steel.html (accessed on 20 February 2023).
- 7E4, 7E5 Modular Hip Joints—Instructions for Use; Otto Bock: Duderstadt, Germany, 2022; p. 11.
- 7E7 Hip—Instructions for Use 2021. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Hips/Modular-Hip-Joint-Free-Mot-Titan/p/7E7#product-documents-section (accessed on 20 February 2023).
- 7E8 Pediatric Modular Hip Joint—Instructions for Use; Otto Bock: Duderstadt, Germany, 2022; p. 20.
- 7E9 Hip Joint—Instructions for Use 2022. Available online: https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Hips/Hydraulic-Hip-Joint/p/7E9#product-documents-section (accessed on 20 February 2023).
- Vezočnik, M.; Juric, M.B. Average Step Length Estimation Models’ Evaluation Using Inertial Sensors: A Review. IEEE Sens. J. 2019, 19, 396–403. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Aguiar, E.J.; Han, H.; Ducharme, S.W.; Schuna, J.M.; Barreira, T.V.; Moore, C.C.; Busa, M.A.; Lim, J.; Sirard, J.R.; et al. Walking Cadence (Steps/Min) and Intensity in 21–40 Year Olds: CADENCE-Adults. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 8. [Google Scholar] [CrossRef]
- Fryar, C.; Gu, Q.; Afful, J.; Carroll, M.; Ogden, C. Anthropometric Reference Data for Children and Adults: United States, August 2021–August 2023; National Center for Health Statistics (U.S.): Hyattsville, MD, USA, 2025.
- Fakoorian, S.; Roshanineshat, A.; Khalaf, P.; Azimi, V.; Simon, D.; Hardin, E. An Extensive Set of Kinematic and Kinetic Data for Individuals with Intact Limbs and Transfemoral Prosthesis Users. Appl. Bionics Biomech. 2020, 2020, e8864854. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Hargrove, L.J. Deep-Learning to Map a Benchmark Dataset of Non-Amputee Ambulation for Controlling an Open Source Bionic Leg. IEEE Robot. Autom. Lett. 2022, 7, 10597–10604. [Google Scholar] [CrossRef] [PubMed]


| Participant | Height (cm) | Weight (kg) | Age (Years) |
|---|---|---|---|
| 1 | 180 | 95 | 29 |
| 2 | 178 | 95 | 45 |
| 3 | 175 | 98 | 26 |
| Ensemble | 178 ± 3 | 96 ± 2 | 33 ± 10 |
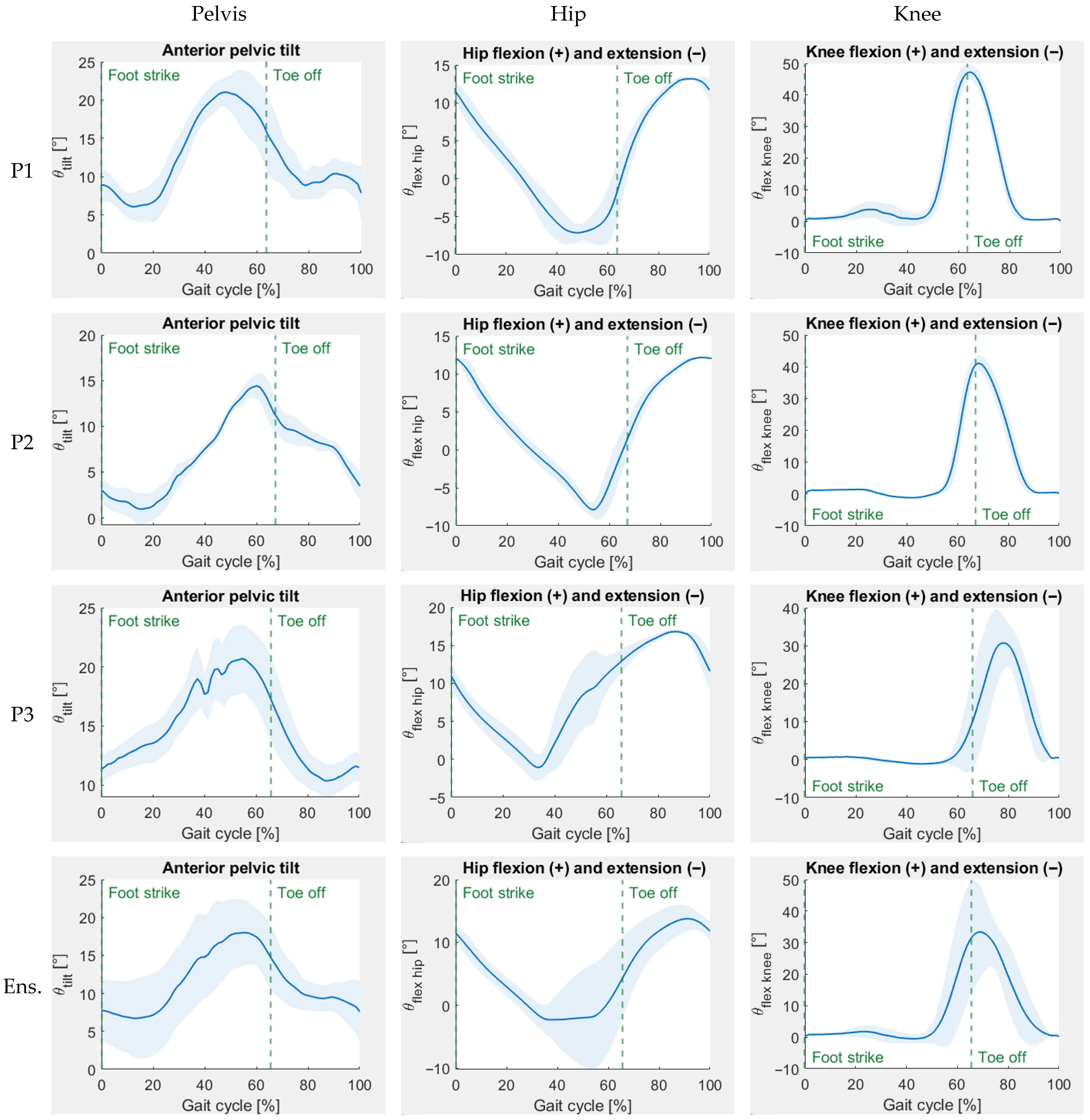
| Participant | Min Ant. Pelvic Tilt (°) | Max Ant. Pelvic Tilt (°) | Pelvic Range of Motion (°) | Max Hip Extension (°) | Max Hip Flexion (°) | Hip Range of Motion (°) | Max Knee Extension (°) | Max Knee Flexion (°) | Knee Range of Motion (°) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 5.19 ± 1.77 | 22.14 ± 2.34 | 16.95 ± 3.32 | 7.98 ± 0.14 | 13.28 ± 0.04 | 21.26 ± 0.17 | 0.61 ± 0.43 | 47.73 ± 2.44 | 48.34 ± 2.53 |
| 2 | 0.43 ± 1.68 | 14.70 ± 1.22 | 14.27 ± 2.29 | 8.76 ± 0.06 | 12.21 ± 0.04 | 20.97 ± 0.09 | 1.23 ± 0.10 | 41.83 ± 2.13 | 43.06 ± 2.19 |
| 3 | 9.90 ± 1.23 | 22.12 ± 2.36 | 12.22 ± 1.63 | 2.71 ± 0.04 | 17.00 ± 0.08 | 19.71 ± 0.07 | 1.31 ± 0.10 | 33.58 ± 6.21 | 34.89 ± 6.26 |
| Ensemble | 5.17 ± 4.22 | 19.65 ± 4.07 | 14.48 ± 3.13 | 6.48 ± 2.74 | 14. 17 ± 2.09 | 20.65 ± 0.69 | 1.05 ± 0.41 | 41.05 ± 7.08 | 42.10 ± 6.88 |
| Participant | Early-Stance Double-Support Time (s) | Prosthetic Side Single-Support Time (s) | Late-Stance Double-Support Time (s) | Sound Side Single-Support Time (s) | Sound Step Length (m) | Prosthetic Step Length (m) | Cadence (steps/min) | Walking Speed (m/s) |
|---|---|---|---|---|---|---|---|---|
| 1 | 0.42 ± 0.06 | 0.23 ± 0.03 | 0.38 ± 0.05 | 0.60 ± 0.06 | 0.43 ± 0.08 | 0.42 ± 0.04 | 77 ± 17 | 0.52 ± 0.05 |
| 2 | 0.46 ± 0.03 | 0.25 ± 0.03 | 0.42 ± 0.04 | 0.56 ± 0.04 | 0.45 ± 0.07 | 0.43 ± 0.04 | 73 ± 12 | 0.52 ± 0.07 |
| 3 | 0.63 ± 0.13 | 0.24 ± 0.04 | 0.56 ± 0.09 | 0.74 ± 0.07 | 0.41 ± 0.06 | 0.28 ± 0.05 | 59 ± 15 | 0.32 ± 0.06 |
| Ensemble | 0.50 ± 0.12 | 0.24 ± 0.03 | 0.46 ± 0.10 | 0.63 ± 0.10 | 0.43 ± 0.07 | 0.38 ± 0.08 | 69 ± 17 | 0.45 ± 0.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Botros, M.; Gholizadeh, H.; Golshan, F.; Langlois, D.; Baddour, N.; Lemaire, E.D. Development of a Powered Four-Bar Prosthetic Hip Joint Prototype. Prosthesis 2025, 7, 105. https://doi.org/10.3390/prosthesis7050105
Botros M, Gholizadeh H, Golshan F, Langlois D, Baddour N, Lemaire ED. Development of a Powered Four-Bar Prosthetic Hip Joint Prototype. Prosthesis. 2025; 7(5):105. https://doi.org/10.3390/prosthesis7050105
Chicago/Turabian StyleBotros, Michael, Hossein Gholizadeh, Farshad Golshan, David Langlois, Natalie Baddour, and Edward D. Lemaire. 2025. "Development of a Powered Four-Bar Prosthetic Hip Joint Prototype" Prosthesis 7, no. 5: 105. https://doi.org/10.3390/prosthesis7050105
APA StyleBotros, M., Gholizadeh, H., Golshan, F., Langlois, D., Baddour, N., & Lemaire, E. D. (2025). Development of a Powered Four-Bar Prosthetic Hip Joint Prototype. Prosthesis, 7(5), 105. https://doi.org/10.3390/prosthesis7050105






