Influence of Different Fiber-Reinforced Biobases on the Marginal Adaptation of Lithium Disilicate Overlay Restorations (A Comparative In Vitro Study)
Abstract
1. Introduction
- A thin film of low-viscosity flowable composite resin is placed atop the bonded dentin [10].
2. Materials and Methods
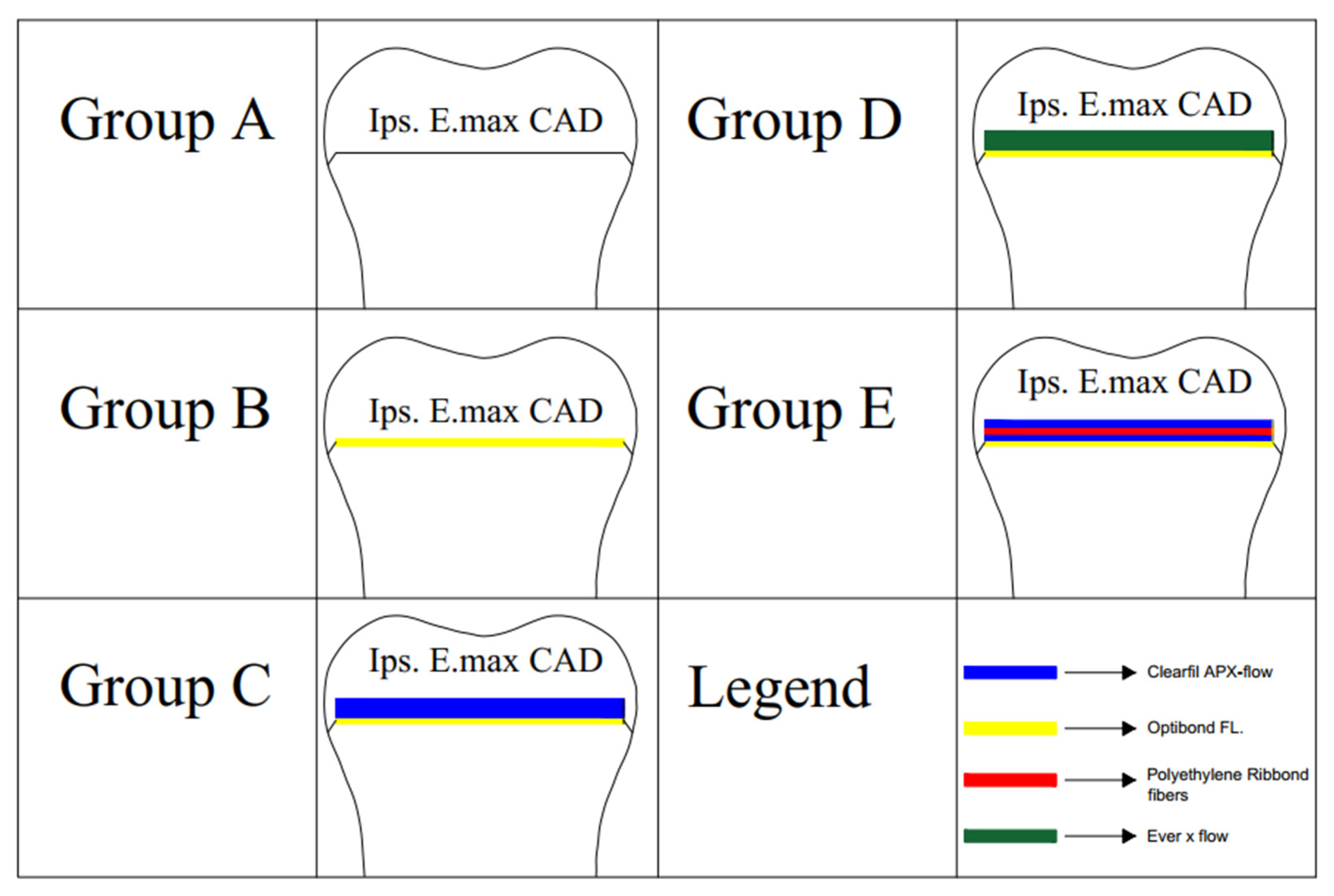
2.1. Tooth Selection and Grouping
2.2. Specimen Preparation and Biobase Application
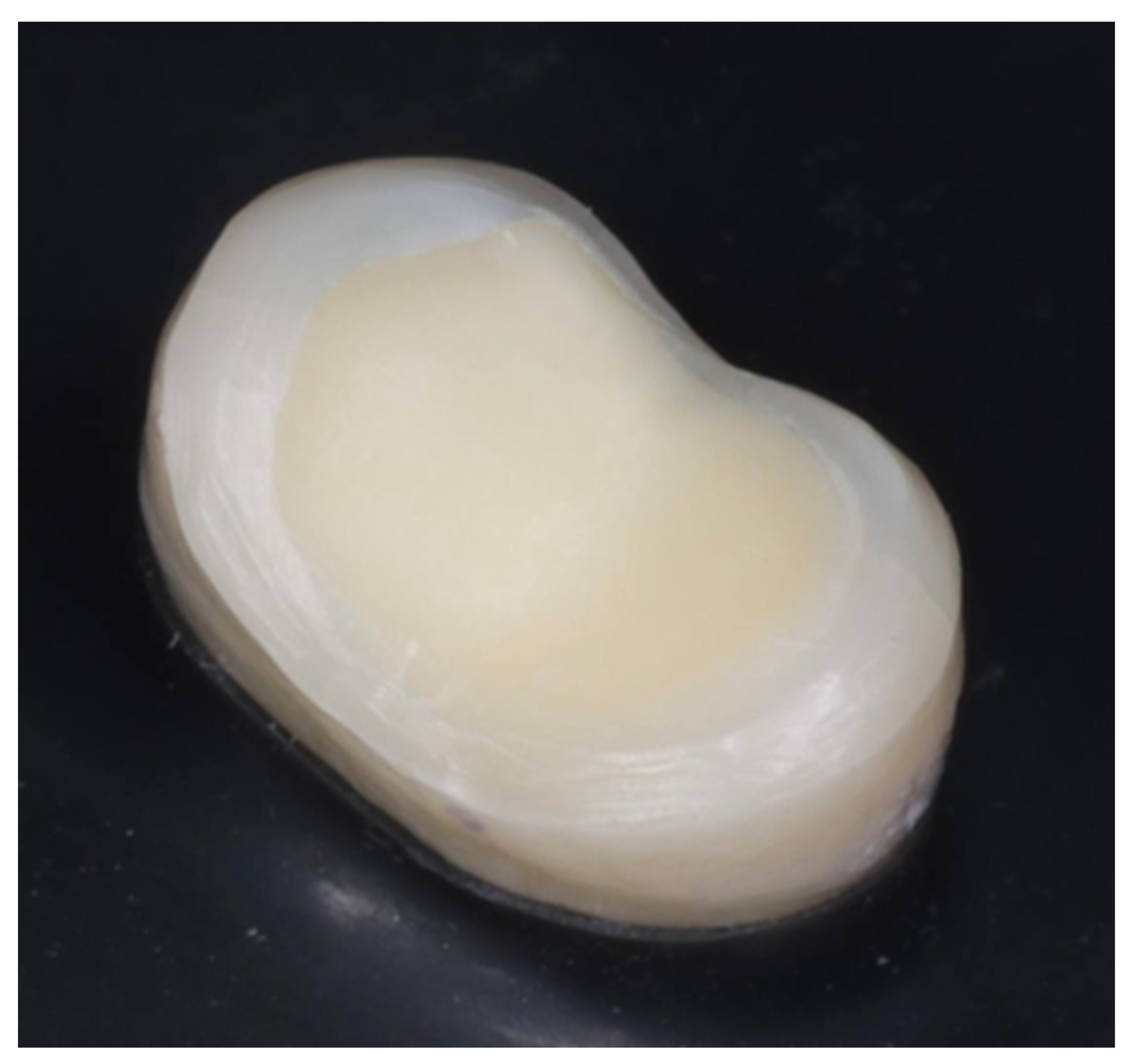
2.3. Digital Workflow and Overlay Fabrication
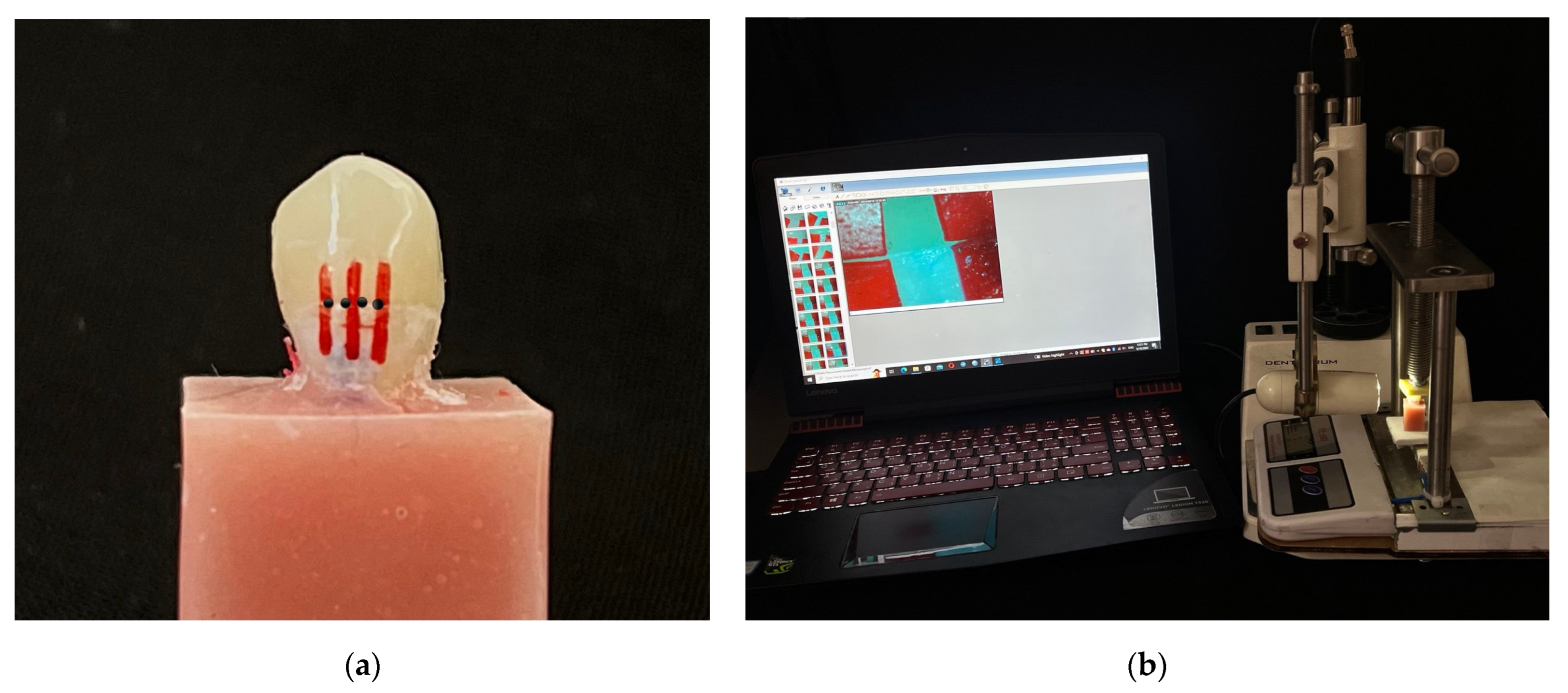
2.4. Marginal Gap Assessment and Cementation
2.5. Statistical Analysis
3. Results
4. Discussion
Clinical Implications of the Current Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus indirect inlay/onlay composite restorations in posterior teeth: A systematic review and meta-analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef]
- Nikaido, T.; Inoue, G.; Takagaki, T.; Takahashi, R.; Sadr, A.; Tagami, J. Resin coating technique for protection of pulp and increasing bonding in indirect restoration. Curr. Oral Health Rep. 2015, 2, 81–86. [Google Scholar] [CrossRef]
- Tseng, C.W.; Yong, C.Y.; Fang, C.Y.; Lee, S.Y.; Wang, Y.C.; Lin, W.C. Comparative analysis of bonding strength between enamel and overlay of varying thicknesses following an aging test. J. Dent. Sci. 2023, 18, 1850–1858. [Google Scholar] [CrossRef]
- Tafuri, G.; D’Addazio, G.; Santilli, M.; Argentieri, G.; Murmura, G.; Caputi, S.; Sinjari, B. Overlay Preparation Accuracy: An In Vitro Study on the Influence of Magnification and Operator Expertise. Prosthesis 2025, 7, 5. [Google Scholar] [CrossRef]
- Hofsteenge, J.W.; Bresser, R.A.; Buijs, G.J.; van der Made, S.A.; Özcan, M.; Cune, M.S.; Gresnigt, M.M. Clinical performance of bonded partial lithium disilicate restorations: The influence of preparation characteristics on survival and success. J. Dent. 2024, 142, 104828. [Google Scholar] [CrossRef]
- Al-Johani, H.; Haider, J.; Satterthwaite, J.; Silikas, N. Lithium silicate-based glass ceramics in dentistry: A narrative review. Prosthesis 2024, 6, 478–505. [Google Scholar] [CrossRef]
- Garoushi, S.; Säilynoja, E.; Vallittu, P.K.; Lassila, L. Fracture-behavior of CAD/CAM ceramic crowns before and after cyclic fatigue aging. Int. J. Prosthodont. 2021, 23, 1–8. [Google Scholar]
- Magne, P. Immediate dentin sealing: A fundamental procedure for indirect bonded restorations. J. Esthet. Restor. Dent. 2005, 17, 144–154. [Google Scholar] [CrossRef]
- de Andrade, O.S.; de Goes, M.F.; Montes, M.A. Marginal adaptation and microtensile bond strength of composite indirect restorations bonded to dentin treated with adhesive and low-viscosity composite. Dent. Mater. 2007, 23, 279–287. [Google Scholar] [CrossRef]
- Magne, P.; Spreafico, R.C. Deep margin elevation: A paradigm shift. Am. J. Esthet. Dent. 2012, 2, 86–96. [Google Scholar]
- Frese, C.; Wolff, D.; Staehle, H.J. Proximal box elevation with resin composite and the dogma of biological width: Clinical R2-technique and critical review. Oper. Dent. 2014, 39, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Kruzic, J.J.; Arsecularatne, J.A.; Tanaka, C.B.; Hoffman, M.J.; Cesar, P.F. Recent advances in understanding the fatigue and wear behavior of dental composites and ceramics. J. Mech. Behav. Biomed. Mater. 2018, 88, 504–533. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.; Braunitzer, G.; Tóth, M.; Szabó, B.P.; Fráter, M. In vitro fracture resistance of adhesively restored molar teeth with different MOD cavity dimensions. J. Prosthodont. 2019, 28, e325–e331. [Google Scholar] [CrossRef]
- Garoushi, S.; Säilynoja, E.; Vallittu, P.K.; Lassila, L. Physical properties and depth of cure of a new short fiber reinforced composite. Dent. Mater. 2013, 29, 835–841. [Google Scholar] [CrossRef]
- Belli, S.; Orucoglu, H.; Yildirim, C.; Eskitascioglu, G. The effect of fiber placement or flowable resin lining on microleakage in Class II adhesive restorations. J. Adhes. Dent. 2007, 9, 175. [Google Scholar]
- Başaran, E.G.; Ayna, E.; Vallittu, P.K.; Lassila, L.V. Load bearing capacity of fiber-reinforced and unreinforced composite resin CAD/CAM-fabricated fixed dental prostheses. J. Prosthet. Dent. 2013, 109, 88–94. [Google Scholar] [CrossRef]
- Monaco, C.; Bortolotto, T.; Arena, A.; Krejci, I. Restoring nonvital premolars with composite resin onlays: Effect of different fiber-reinforced composite layers on marginal adaptation and fracture load. J. Adhes. Dent. 2015, 17, 567–574. [Google Scholar]
- Magne, P.; Milani, T. Short-fiber reinforced MOD restorations of molars with severely undermined cusps. J. Adhes. Dent. 2023, 25, 99–106. [Google Scholar] [CrossRef]
- Otero, C.A.Y.; Bijelic-Donova, J.; Saratti, C.M.; Vallittu, P.K.; di Bella, E.; Krejci, I.; Rocca, G.T. The influence of FRC base and bonded CAD/CAM resin composite endocrowns on fatigue behavior of cracked endodontically-treated molars. J. Mech. Behav. Biomed. Mater. 2021, 121, 104647. [Google Scholar] [CrossRef]
- Fildisi, M.A.; Eliguzeloglu Dalkilic, E. The effect of fiber insertion on fracture strength and fracture modes in endocrown and overlay restorations. Microsc. Res. Tech. 2022, 85, 1799–1807. [Google Scholar] [CrossRef] [PubMed]
- Mansi, Z.M.; Al-Shamma, A.M.; Saleh, A.R. Assessment of marginal adaptation of indirect zirconia crown restorations using self-adhesive resin cements modified with polylysine antibacterial particles. J. Baghdad Coll. Dent. 2024, 36, 50–60. [Google Scholar] [CrossRef]
- Khaledi, A.-A.; Farzin, M.; Akhlaghian, M.; Pardis, S.; Mir, N. Evaluation of the marginal fit of metal copings fabricated by using 3 different CAD-CAM techniques: Milling, stereolithography, and 3D wax printer. J. Prosthet. Dent. 2020, 124, 81–86. [Google Scholar] [CrossRef]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef]
- Falahchai, M.; Rahimabadi, S.; Khabazkar, G.; Babaee Hemmati, Y.; Neshandar Asli, H. Marginal and internal fit and fracture resistance of three-unit provisional restorations fabricated by additive, subtractive, and conventional methods. Clin. Exp. Dent. Res. 2022, 8, 1404–1412. [Google Scholar] [CrossRef]
- Saadallah, S.; Al-Azzawi, A.K.J. The influence of different fabrication and impression techniques on the marginal adaptation of lithium disilicate crowns (A comparative in vitro study). J. Baghdad Coll. Dent. 2017, 29, 20–26. [Google Scholar] [CrossRef]
- Al-Ramadan, A.; Abualsaud, R.; Al-Dulaijan, Y.A.; Al-Thobity, A.M.; Alalawi, H. Accuracy and fit of ceramic filled 3D-printed resin for permanent crown fabrication: An in vitro comparative study. Prosthesis 2024, 6, 1029–1041. [Google Scholar] [CrossRef]
- Yousif, Y.H.; Kadhim, A.J. The effect of immediate dentin sealing on the marginal adaptation of lithium disilicate overlay restorations using different types of luting agents. Brazil. Dent. Sci. 2023, 26, e3925. [Google Scholar] [CrossRef]
- Wolfart, S.; Wegner, S.M.; Al-Halabi, A.; Kern, M. Clinical evaluation of marginal fit of a new experimental all-ceramic system before and after cementation. Int. J. Prosthodont. 2003, 16, 587. [Google Scholar]
- Ibraheem, A.F.; Abdulkareem, A.M. Comparison of the marginal fitness of the ceramic crowns fabricated with different CAD/CAM systems (An in vitro study). J. Baghdad Coll. Dent. 2016, 28, 28–33. [Google Scholar]
- Athab Hasan, S.; Mohammed-Hussain Abdul-Ameer, Z. Effect of three different preparation designs on the marginal adaptation of indirect overlay restoration fabricated from lithium disilicate ceramic material: An in-vitro comparative study. Saudi Dent. J. 2023, 35, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Hmedat, S.J. A Comparison of Vertical Marginal Fit of Three Different Types of All-Ceramic Crown Restorations. Ph.D. Thesis, University of Baghdad, Baghdad, Iraq, 2012. [Google Scholar]
- Gonzalo, E.; Suárez, M.J.; Serrano, B.; Lozano, J.F. Marginal fit of zirconia posterior fixed partial dentures. Int. J. Prosthodont. 2008, 21, 398–399. [Google Scholar] [PubMed]
- Khdeir, R.M.; Ibraheem, A.F. The marginal fitness of CAD/CAM all ceramic crowns constructed by two types of direct digitization techniques (an in vitro study). J. Baghdad Coll. Dent. 2016, 28, 30–33. [Google Scholar] [CrossRef]
- Kim, D.Y.; Song, H.Y. Method of predicting human mobility patterns using deep learning. Neurocomputing 2018, 280, 56–64. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Marginal and internal fit of CAD-CAM inlay/onlay restorations: A systematic review of in vitro studies. J. Prosthet. Dent. 2019, 121, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Alajaji, N.K.; Bardwell, D.; Finkelman, M.; Ali, A. Micro-CT Evaluation of Ceramic Inlays: Comparison of the Marginal and Internal Fit of Five and Three Axis CAM Systems with a Heat Press Technique. J. Esthet. Restor. Dent. 2017, 29, 49–58. [Google Scholar] [CrossRef]
- Ferraris, F.; Sammarco, E.; Romano, G.; Cincera, S.; Giulio, M. Comparison of posterior indirect adhesive restorations (PIAR) with different preparation designs according to the adhesthetics classification. Part 1: Effects on the fracture resistance. Int. J. Esthet. Dent. 2021, 16, 144. [Google Scholar]
- Abduo, J.; Sambrook, R.J. Longevity of ceramic onlays: A systematic review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef]
- Mohammed, Z.H.; Majeed, M.A. Effect of cementation protocol on the marginal adaptation of indirect overlay restorations fabricated from two different all-ceramic CAD/CAM materials. J. Res. Med. Dent. Sci. 2020, 8, 518–525. [Google Scholar]
- Skordou, T.; Kebi, L.; Osnes, C.; Keeling, A. The effect of two different milling instrument sets on CAD proposed cement thickness and fit surface of chairside CAD crowns. J. Osseointegr. 2021, 13, 271–278. [Google Scholar] [CrossRef]
- Hasaneen, F.A.; Mogahed, M.M. Comparative in-vitro study of marginal gap of four CAD/CAM all ceramic systems with thermal aging. Tanta Dent. J. 2021, 18, 12–19. [Google Scholar] [CrossRef]
- Pilecco, R.O.; da Rosa, L.S.; Baldi, A.; Machry, R.V.; Tribst, J.P.M.; Valandro, L.F.; Kleverlaan, C.J.; Scotti, N.; Pereira, G.K.R. How do different intraoral scanners and milling machines affect the fit and fatigue behavior of lithium disilicate and resin composite endocrowns? J. Mech. Behav. Biomed. Mater. 2024, 155, 106557. [Google Scholar] [CrossRef] [PubMed]
- Abdulla, H.A.; Majeed, M.A. Assessment of bioactive resin-modified glass ionomer restorative as a new CAD/CAM material. Part I: Marginal fitness study. Indian J. Forensic Med. Toxicol. 2020, 14, 865–870. [Google Scholar] [CrossRef]
- Mounajjed, R.; Salinas, T.J.; Ingr, T.; Azar, B. Effect of different resin luting cements on the marginal fit of lithium disilicate pressed crowns. J. Prosthet. Dent. 2018, 119, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.R.; Ali, M.; Al Hossan, A.; Majeed-Saidan, A.; Al Qahtani, M. Effect of cementation, cement type and vent holes on fit of zirconia copings. Saudi Dent. J. 2019, 31, 45–51. [Google Scholar] [CrossRef]
- Falahchai, M.; Babaee Hemmati, Y.; Neshandar Asli, H.; Neshandar Asli, M. Marginal adaptation of zirconia-reinforced lithium silicate overlays with different preparation designs. J. Esthet. Restor. Dent. 2020, 32, 823–830. [Google Scholar] [CrossRef]
- Guess, P.C.; Vagkopoulou, T.; Zhang, Y.; Wolkewitz, M.; Strub, J.R. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J. Dent. 2014, 42, 199–209. [Google Scholar] [CrossRef]
- Rocca, G.T.; Saratti, C.M.; Poncet, A.; Feilzer, A.J.; Krejci, I. The influence of FRCs reinforcement on marginal adaptation of CAD/CAM composite resin endocrowns after simulated fatigue loading. Odontology 2016, 104, 220–232. [Google Scholar] [CrossRef]
- Sabet, A. Effect of filling pulp chamber on marginal adaptation and fracture resistance of zirconia reinforced glass ceramic endocrown restorations. Egypt. Dent. J. 2017, 63, 3833–3842. [Google Scholar] [CrossRef]
- Ovul, K.; Arzu, T.-M.; Ahmet, S.; Vj, L.L. Marginal adaptation and microleakage of directly and indirectly made fiber reinforced composite inlays. Open Dent. J. 2011, 5, 33. [Google Scholar] [CrossRef] [PubMed]
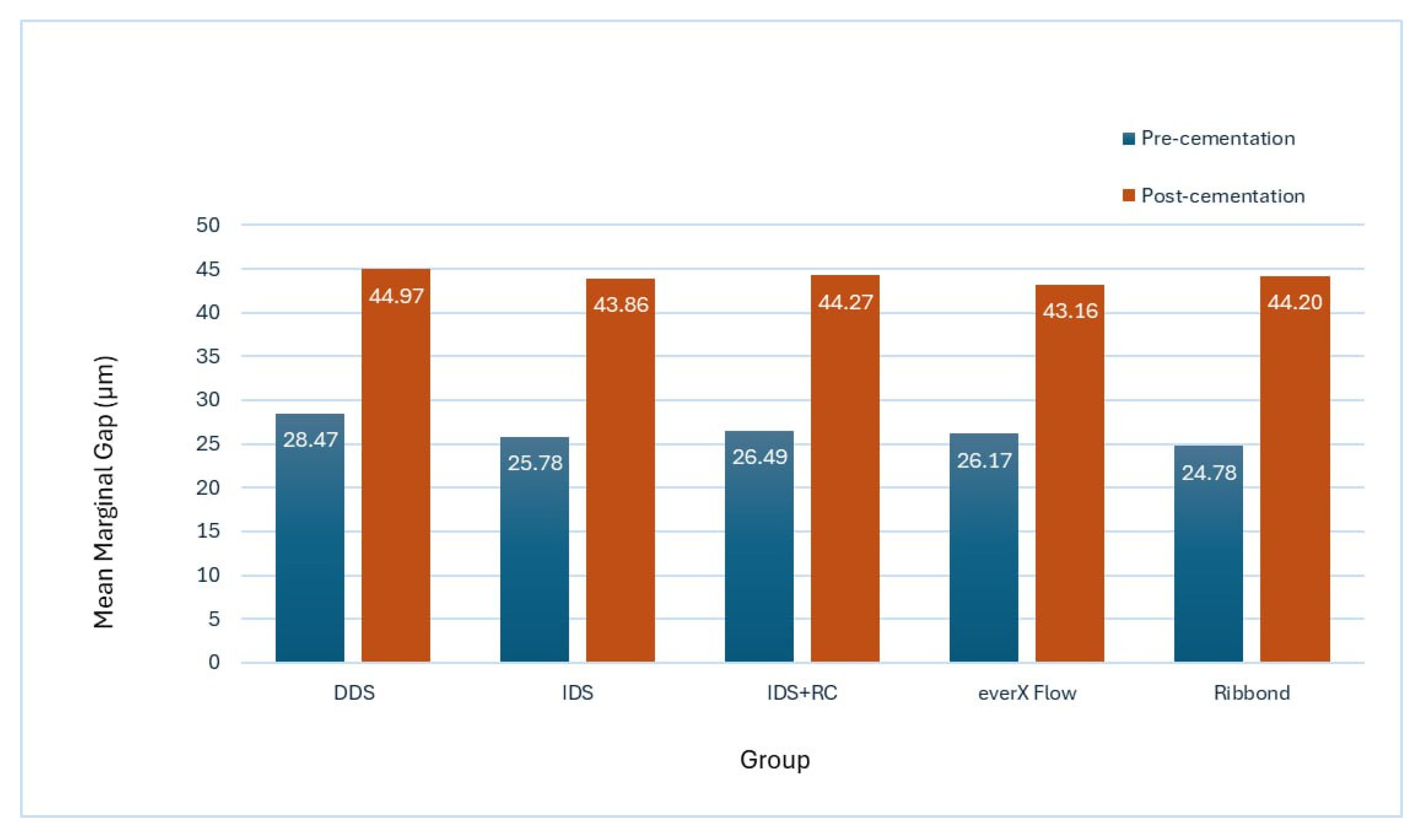
| Pre-Cementation | Post-Cementation | ||||
|---|---|---|---|---|---|
| Group | Mean ± SD | Paired t-Test | Group | Mean ± SD | Paired t-Test |
| A (DDS) | 28.47 ± 4.31 | 0.00 | A (DDS) | 44.97 ± 6.12 | 0.00 |
| B (IDS) | 25.78 ± 4.6 | 0.00 | B (IDS) | 43.86 ± 6.33 | 0.00 |
| C (IDS + RC) | 26.48 ± 4.86 | 0.00 | C (IDS + RC) | 44.27 ± 6.08 | 0.00 |
| D (everX Flow) | 26.17 ± 4.69 | 0.00 | D (everX Flow) | 43.15 ± 6.54 | 0.00 |
| E (Ribbond) | 24.77 ± 4.22 | 0.00 | E (Ribbond) | 44.2 ± 7.51 | 0.00 |
| One-way ANOVA | 0.479 (NS) | One-way ANOVA | 0.981 (NS) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nabat, M.A.; Kadhim, A.J. Influence of Different Fiber-Reinforced Biobases on the Marginal Adaptation of Lithium Disilicate Overlay Restorations (A Comparative In Vitro Study). Prosthesis 2025, 7, 55. https://doi.org/10.3390/prosthesis7030055
Nabat MA, Kadhim AJ. Influence of Different Fiber-Reinforced Biobases on the Marginal Adaptation of Lithium Disilicate Overlay Restorations (A Comparative In Vitro Study). Prosthesis. 2025; 7(3):55. https://doi.org/10.3390/prosthesis7030055
Chicago/Turabian StyleNabat, Maareb Abdulraheem, and Alaa Jawad Kadhim. 2025. "Influence of Different Fiber-Reinforced Biobases on the Marginal Adaptation of Lithium Disilicate Overlay Restorations (A Comparative In Vitro Study)" Prosthesis 7, no. 3: 55. https://doi.org/10.3390/prosthesis7030055
APA StyleNabat, M. A., & Kadhim, A. J. (2025). Influence of Different Fiber-Reinforced Biobases on the Marginal Adaptation of Lithium Disilicate Overlay Restorations (A Comparative In Vitro Study). Prosthesis, 7(3), 55. https://doi.org/10.3390/prosthesis7030055






