AI in Prosthodontics: A Narrative Review Bridging Established Knowledge and Innovation Gaps Across Regions and Emerging Frontiers
Abstract
1. Introduction
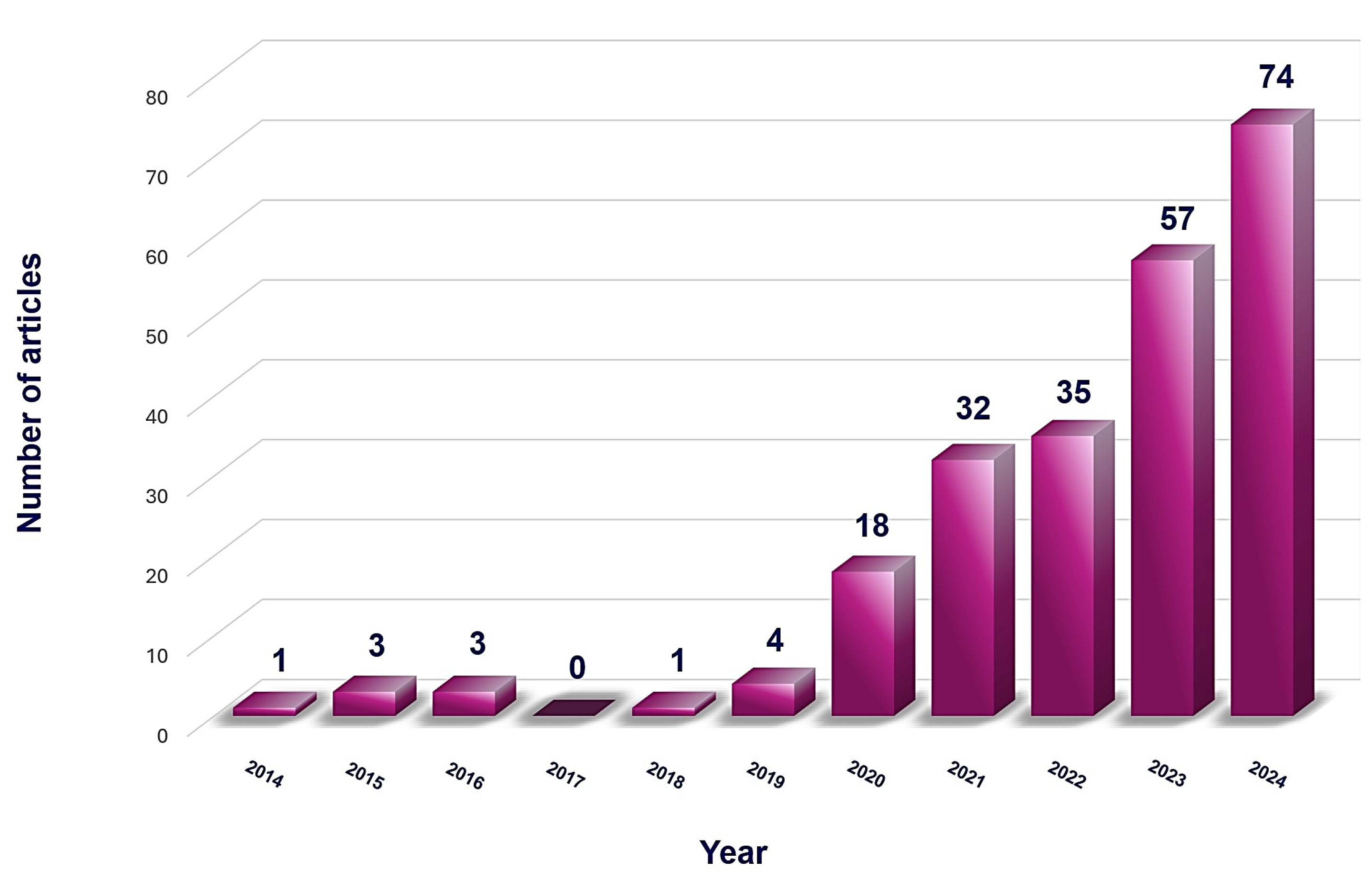
2. Materials and Methods
3. Results
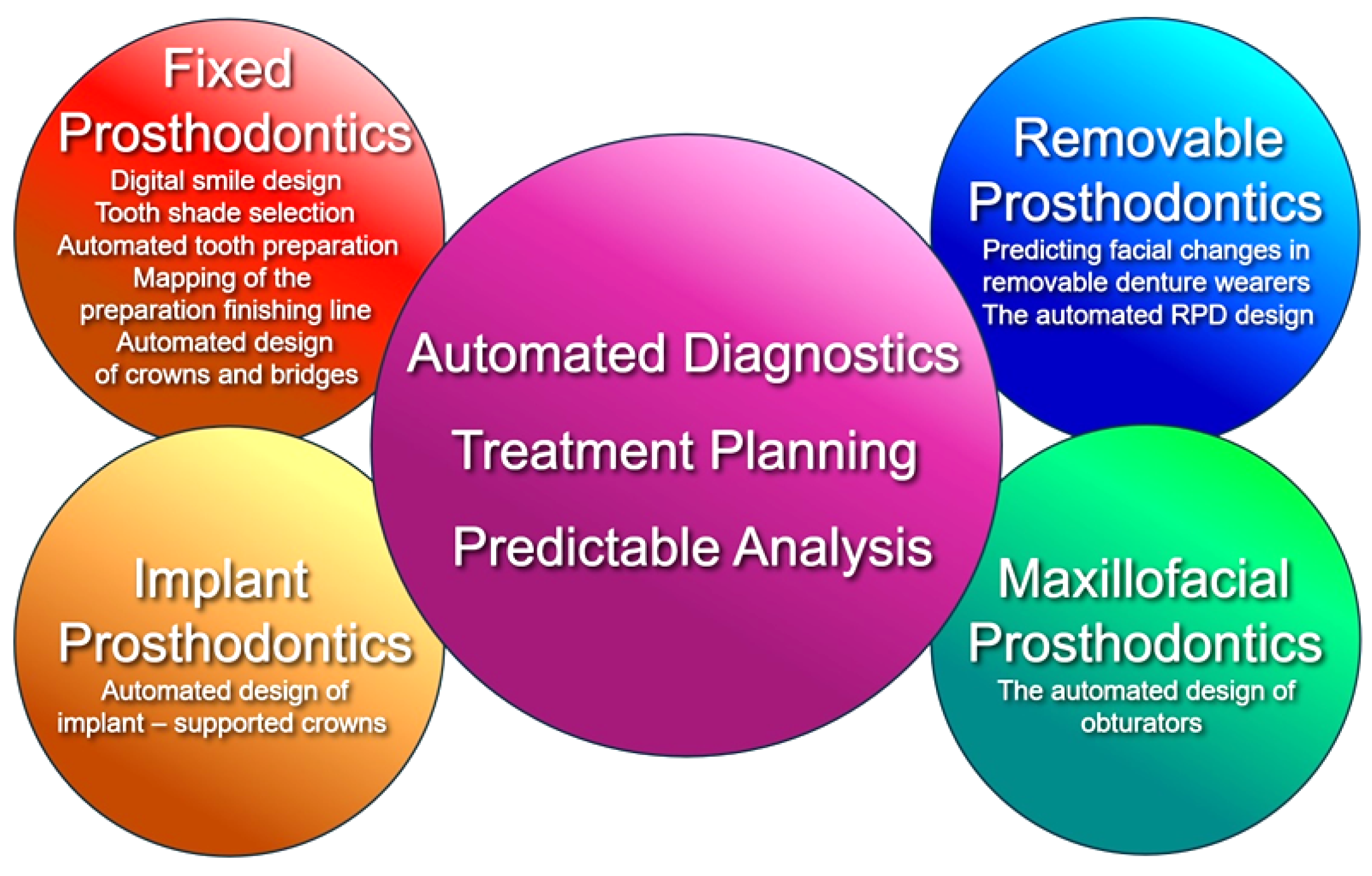
3.1. Main Applications of AI in Prosthodontics
3.2. Common AI Applications Across Prosthodontics Subspecialties
3.2.1. The Automated Diagnostics and Treatment Planning
3.2.2. The Predictable Analysis
3.3. Specific AI Applications Across Prosthodontics Subspecialties
3.3.1. The Fixed Prosthodontics
- The Digital Smile Design
- The Tooth Shade Selection
- The Automated Tooth Preparation
- The Mapping of the Preparation Finishing Line
- The Automated Restoration Design
3.3.2. The Removable Prosthodontics
- The Prediction of Facial Changes in the Removable Denture Wearers
- The Removable Partial Denture Design
3.3.3. The Implant Prosthodontics
3.3.4. The Maxillofacial Prosthodontics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wiens, J.P.; Koka, S.; Graser, G.; White, S.N.; Marinello, C.P.; Curtis, D.A. Academy of Prosthodontics Centennial: The Emergence and Development of Prosthodontics as a Specialty. J. Prosthet. Dent. 2017, 118, 569–572. [Google Scholar] [CrossRef] [PubMed]
- Academy of Prosthodontics. The Glossary of Prosthodontic Terms. J. Prosthet. Dent. 2023, 130, e1–e3. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Fiorillo, L.; Russo, D.; Lanza, A.; D’Amico, C.; Cervino, G.; Meto, A.; Di Francesco, F. Prosthodontic Treatment in Patients with Temporomandibular Disorders and Orofacial Pain and/or Bruxism: A Review of the Literature. Prosthesis 2022, 4, 253–262. [Google Scholar] [CrossRef]
- Hagag, G.; Yoshida, K.; Miura, H. Occlusion, Prosthodontic Treatment, and Temporomandibular Disorders: A Review. J. Med. Dent. Sci. 2000, 47, 61–66. [Google Scholar] [PubMed]
- Manfredini, D.; Poggio, C.E. Prosthodontic Planning in Patients with Temporomandibular Disorders and/or Bruxism: A Systematic Review. J. Prosthet. Dent. 2017, 117, 606–613. [Google Scholar] [CrossRef]
- Cristache, C.M.; Tudor, I.; Moraru, L.; Cristache, G.; Lanza, A.; Burlibasa, M. Digital Workflow in Maxillofacial Prosthodontics—An Update on Defect Data Acquisition, Editing and Design Using Open-Source and Commercial Available Software. Appl. Sci. 2021, 11, 973. [Google Scholar] [CrossRef]
- Spielman, A.I. History of Prosthodontics. In Illustrated Encyclopedia of the History of Dentistry; Harper & Brothers: New York, NY, USA, 2023; Available online: https://historyofdentistryandmedicine.com/ (accessed on 20 August 2024).
- Di Fiore, A.; Brunello, G. Current Trends and Future Directions in Prosthetic and Implant Dentistry in the Digital Era; MDPI: Basel, Switzerland, 2022. [Google Scholar]
- Ding, H.; Wu, J.; Zhao, W.; Matinlinna, J.P.; Burrow, M.F.; Tsoi, J.K.H. Artificial Intelligence in Dentistry—A Review. Front. Dent. Med. 2023, 4, 1085251. [Google Scholar] [CrossRef]
- Castiglioni, I.; Rundo, L.; Codari, M.; Di Leo, G.; Salvatore, C.; Interlenghi, M.; Gallivanone, F.; Cozzi, A.; D’Amico, N.C.; Sardanelli, F. AI applications to medical images: From machine learning to deep learning. Phys. Medica 2021, 83, 9–24. [Google Scholar] [CrossRef]
- Arsiwala-Scheppach, L.T.; Chaurasia, A.; Müller, A.; Krois, J.; Schwendicke, F. Machine Learning in Dentistry: A Scoping Review. J. Clin. Med. 2023, 12, 937. [Google Scholar] [CrossRef]
- Allani, H.; Santos, A.T.; Ribeiro-Vidal, H. Multidisciplinary Applications of AI in Dentistry: Bibliometric Review. Appl. Sci. 2024, 14, 7624. [Google Scholar] [CrossRef]
- Ünsal, G.; Orhan, K. Future Perspectives of Artificial Intelligence in Dentistry. In Artificial Intelligence in Dentistry; Springer: Berlin/Heidelberg, Germany, 2024; pp. 353–364. Available online: https://link.springer.com/chapter/10.1007/978-3-031-43827-1_19 (accessed on 20 August 2024).
- Semerci, Z.M.; Yardımcı, S. Empowering Modern Dentistry: The Impact of Artificial Intelligence on Patient Care and Clinical Decision Making. Diagnostics 2024, 14, 1260. [Google Scholar] [CrossRef] [PubMed]
- Jokstad, A.; Orstavik, J.; Ramstad, T. A definition of prosthetic dentistry. Int. J. Prosthodont. 1998, 11, 295–301. [Google Scholar] [PubMed]
- American College of Prosthodontists. History, Information, and Examination Requirements of the American Board of Prosthodontics. J. Prosthet. Dent. 1984, 52, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Golla, T.; Dreher, M.; Krois, J. Convolutional neural networks for dental image diagnostics: A scoping review. J. Dent. 2019, 91, 103226. [Google Scholar] [CrossRef]
- Orhan, K.; Aksoy, U.; Aksoy, S. Applications of AI in Endodontics and Restorative Dentistry. In Artificial Intelligence in Dentistry; Springer: Berlin/Heidelberg, Germany, 2024; pp. 69–81. [Google Scholar] [CrossRef]
- Hong, J.; Huh, J.-K.; Lee, J.-H. Automated Deep Learning for Classification of Dental Implant Radiographs Using a Large Multi-Center Dataset. Sci. Rep. 2023, 13, 32118. [Google Scholar] [CrossRef]
- Naeimi, S.M.; Darvish, S.; Salman, B.N.; Luchian, I. Artificial Intelligence in Adult and Pediatric Dentistry: A Narrative Review. Bioengineering 2024, 11, 431. [Google Scholar] [CrossRef]
- Cervino, G.; Peditto, M.; Portelli, M.; Militi, A.; Matarese, G.; Fiorillo, L.; Nucera, R.; Oteri, G. The Use of AI for Prosthodontic Restoration: Predictable and Safer Dentistry. Eng. Proc. 2023, 56, 68. [Google Scholar] [CrossRef]
- Revilla-León, M.; Gomez-Polo, M.; Barmak, A.B.; Lois, J.C.; Perez-Barquero, J.A. Accuracy of an Artificial Intelligence-Based Program for Locating the Maxillomandibular Relationship of Scans Acquired by Using Intraoral Scanners. J. Prosthet. Dent. 2024. Online ahead of print. [Google Scholar] [CrossRef]
- Fitzek, S.; Choi, K.-E. Potential Impact and Challenges of Implementing Artificial Intelligence in the Romanian Healthcare System. Postmod. Probl. 2023, 13, 148–192. [Google Scholar] [CrossRef]
- Alshadidi, A.A.F.; Alshahrani, A.A.; Aldosari, L.I.N.; Chaturvedi, S.; Saini, R.S.; Hassan, S.A.B.; Cicciù, M.; Minervini, G. Investigation on the Application of Artificial Intelligence in Prosthodontics. Appl. Sci. 2023, 13, 5004. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, D.-H.; Jeong, S.-N.; Choi, S.-H. Diagnosis and Prediction of Periodontally Compromised Teeth Using a Deep Learning-Based Convolutional Neural Network Algorithm. J. Periodontal Implant. Sci. 2018, 48, 114. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Lee, C.; Karaer, O.; Ban, S.; Mine, A.; Imazato, S. Predicting the Debonding of CAD/CAM Composite Resin Crowns with AI. J. Dent. Res. 2019, 98, 1234–1238. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Stanley, K.; Att, W. Artificial Intelligence in Dentistry: Current Applications and Future Perspectives. Quintessence Int. 2020, 51, 248–257. [Google Scholar]
- Erdemir, U.; Yildiz, E.; Yucel, T. Esthetic Parameters/Smile Design. In Esthetic and Functional Management of Diastema; Erdemir, U., Yildiz, E., Eds.; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar] [CrossRef]
- Jurado, C.A.; Villalobos-Tinoco, J.; Lackey, M.A.; Rojas-Rueda, S.; Robles, M.; Tsujimoto, A. Three Dimensional-Printed Gingivectomy and Tooth Reduction Guides Prior Ceramic Restorations: A Case Report. Dent. J. 2024, 12, 245. [Google Scholar] [CrossRef]
- Ceylan, G.; Sayın Özel, G.; Memişoglu, G.; Emir, F.; Şen, S. Evaluating the Facial Esthetic Outcomes of Digital Smile Designs Generated by Artificial Intelligence and Dental Professionals. Appl. Sci. 2023, 13, 9001. [Google Scholar] [CrossRef]
- Deshmukh, K.; Radke, U.; Deshmukh, S.; Pande, N.; Mowade, T.; Hatmode, T. Role of Digitalization in Smile Designing: A Review. J. Adv. Dent. Pract. Res. 2022, 1, 27–30. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Arzukanyan, A.; Spagnuolo, G.; Cicciù, M. Dental Restorative Digital Workflow: Digital Smile Design from Aesthetic to Function. Dent. J. 2019, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Cofar, F.; Coachman, C. SMILE CLOUD: AI-Powered Digital Smile Design Platform. 2023, Straumann Group. Available online: https://www.straumann.com/us/en/dental-professionals/digital-performance/software/smilecloud.html (accessed on 15 September 2024).
- Costin, L.I.; Vasluianu, R.I.; Baciu, R.-E.; Agop-Forna, D.; Cătălin, T.S.; Forna, C.N. The Integration of Artificial Intelligence in Dental Practice. Rom. J. Oral Rehabil. 2023, 2, 272–279. Available online: http://rjor.ro/wp-content/uploads/2023/07 (accessed on 15 September 2024).
- Buduru, S.; Cofar, F.; Mesaroș, A.; Tăut, M.; Negucioiu, M.; Almășan, O. Perceptions in Digital Smile Design: Assessing Laypeople and Dental Professionals’ Preferences Using an Artificial-Intelligence-Based Application. Dent. J. 2024, 12, 1049. [Google Scholar] [CrossRef] [PubMed]
- Rokhshad, R.; Karteva, T.; Chaurasia, A.; Richert, R.; Mörch, C.M.; Tamimi, F.; Ducret, M. Artificial Intelligence and Smile Design: An e-Delphi Consensus Statement of Ethical Challenges. J. Prosthodont 2024, 33, 730–735. [Google Scholar] [CrossRef]
- Adel, S.M.; Bichu, Y.M.; Pandian, S.M.; Sabouni, W.; Shah, C.; Vaiid, N. Clinical Audit of an Artificial Intelligence (AI) Empowered Smile Simulation System: A Prospective Clinical Trial. Sci. Rep. 2024, 14, 69314. Available online: https://www.nature.com/articles/s41598-024-69314-6.pdf (accessed on 15 September 2024). [CrossRef]
- Jouhar, R.; Ahmed, M.A.; Khurshid, Z. An Overview of Shade Selection in Clinical Dentistry. Appl. Sci. 2022, 12, 6841. [Google Scholar] [CrossRef]
- Kong, H.-J.; Kim, Y.-L. Application of Artificial Intelligence in Dental Crown Prosthesis: A Scoping Review. BMC Oral Health 2024, 24, 937. Available online: https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-024-04657-0 (accessed on 15 September 2024). [CrossRef]
- Özcan, M.; El Mekawy, N.; Emera, R.M.K. Artificial Intelligence Models for Tooth-Supported Fixed and Removable Prosthodontics: A Systematic Review. J. Prosthet. Dent. 2023, 129, 276–292. Available online: https://www.academia.edu/50158192 (accessed on 15 September 2024).
- Shan, T.; Tay, F.R.; Gu, L. Application of artificial intelligence in dentistry. J. Dent. Res. 2021, 100, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Sirintawat, N.; Leelaratrungruang, T.; Poovarodom, P.; Kiattavorncharoen, S.; Amornsettachai, P. The Accuracy and Reliability of Tooth Shade Selection Using Different Instrumental Techniques: An In Vitro Study. Sensors 2021, 21, 7490. [Google Scholar] [CrossRef]
- Kim, M.; Kim, B.; Park, B.; Lee, M.; Won, Y.; Kim, C.-Y.; Lee, S. A Digital Shade-Matching Device for Dental Color Determination Using the Support Vector Machine Algorithm. Sensors 2018, 18, 3051. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, S.H.; Park, S.H. Application of Support Vector Machines in Tooth Shade Selection. J. Dent. Res. 2018, 97, 345–352. [Google Scholar] [CrossRef]
- Takahashi, K.; Nakajima, M.; Sato, T. Deep Learning-Based Tooth Shade Matching Using Convolutional Neural Networks. J. Prosthet. Dent. 2020, 124, 567–574. [Google Scholar] [CrossRef]
- Mehta, R.; Kumar, A.; Goel, M. CNN-Based Automated Tooth Shade Selection System. Int. J. Prosthodont. 2021, 34, 123–130. [Google Scholar] [CrossRef]
- Laws, J. Perceptive’s AI Robot Completes Dental Crown Procedure in 15 Minutes. Newsweek 2023. Available online: https://www.newsweek.com/perceptive-ai-robot-dental-crown-15-minutes-1765432 (accessed on 28 August 2024).
- Sailer, I. Prosthodontics: A Comprehensive Overview; Quintessence Publishing: Chicago, IL, USA; Available online: https://www.quintpub.com/journals/ijp/ (accessed on 28 August 2024).
- Hollenbeck, K. Generative AI for Dental Crown Designs. 3Shape Blog. 2023. Available online: https://www.3shape.com/en-us/blog/2023/generative-ai-for-dental-crown-design (accessed on 28 August 2024).
- Glidewell. Utilizing AI to Produce Better Crowns, Faster. Glidewell Dental. 2020. Available online: https://glidewelldental.com/education/chairside-magazine/volume-15-issue-1/utilizing-ai-to-produce (accessed on 28 August 2024).
- Neocis. Yomi: The First and Only FDA-Cleared Robotic System for Dental Surgery. Neocis. Available online: https://www.neocis.com/yomi/ (accessed on 28 August 2024).
- DentSim: Advanced Dental Training Simulator. Image Navigation. Available online: https://www.image-navigation.com/dentsim/ (accessed on 28 August 2024).
- Tactile Robotics. Robot-Assisted Dental Surgery. Tactile Robotics. Available online: https://www.tactilerobotics.com/dental-surgery/ (accessed on 28 August 2024).
- Aljulayfi, I.S.; Almatrafi, A.H.; Althubaitiy, R.O.; Alnafisah, F.; Alshehri, K.; Alzahrani, B.; Gufran, K. The Potential of Artificial Intelligence in Prosthodontics: A Comprehensive Review. Med. Sci. Monit. 2024, 30, e944310. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Dai, N.; Tian, S.; Yuan, F.; Yu, Q. The Extraction Method of Tooth Preparation Margin Line Based on S-Octree CNN. Int. J. Numer. Method Biomed. Eng. 2019, 35, e3241. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Doe, A. Integration of AI in Dental CAD/CAM Systems. J. Dent. Res. 2023, 102, 567–578. [Google Scholar]
- Müller, H.; Schmidt, K. AI Applications in European Dentistry. Eur. J. Dent. Technol. 2022, 15, 234–245. [Google Scholar]
- Zhang, L.; Wang, Y. Advances in AI for Dental Applications in China. Chin. J. Dent. Res. 2021, 30, 123–134. [Google Scholar]
- Tanaka, M.; Suzuki, T. AI-Driven Innovations in Japanese Dentistry. J. Dent. Sci. Technol. 2020, 18, 45–46. [Google Scholar]
- Mugri, M.H.; Dewan, H.; Sayed, M.E.; Shaabi, F.I.; Hakami, H.I.; Jokhadar, H.F.; Alqahtani, N.M.; Alshahrani, A.A.; Alabdullah, A.S.; Alshehri, A.H.; et al. The Effect of a Digital Manufacturing Technique, Preparation Taper, and Finish Line Design on the Marginal Fit of Temporary Molar Crowns: An In-Vitro Study. Biomedicines 2023, 11, 570. [Google Scholar] [CrossRef]
- Chen, Y.; Lee, J.K.Y.; Kwong, G.; Pow, E.H.N.; Tsoi, J.K.H. Morphology and Fracture Behavior of Lithium Disilicate Dental Crowns Designed by Human and Knowledge-Based AI. J. Mech. Behav. Biomed. Mater. 2022, 131, 105256. [Google Scholar] [CrossRef]
- Hwang, J.-J.; Azernikov, S.; Efros, A.A.; Yu, S.X. Learning Beyond Human Expertise with Generative Models for Dental Restorations. arXiv 2018, arXiv:180400064. [Google Scholar]
- Tian, S.; Wang, M.; Dai, N.; Ma, H.; Li, L.; Fiorenza, L.; Sun, Y.; Li, Y. DCPR-GAN: Dental Crown Prosthesis Restoration Using Two-Stage Generative Adversarial Networks. IEEE J. Biomed. Health Inform. 2021, 26, 151–160. [Google Scholar] [CrossRef]
- Ding, H.; Cui, Z.; Maghami, E.; Chen, Y.; Matinlinna, J.P.; Pow, E.H.N.; Fok, A.S.L.; Burrow, M.F.; Wang, W.; Tsoi, J.K.H. Morphology and Mechanical Performance of Dental Crown Designed by 3D-DCGAN. Dent. Mater. 2023, 39, 320–332. [Google Scholar] [CrossRef] [PubMed]
- Hosseinimanesh, G.; Ghadiri, F.; Guibault, F.; Cheriet, F.; Keren, J. From Mesh Completion to AI Designed Crown. Lect. Notes Comput. Sci. 2023, 14228, 555–565. [Google Scholar]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Gallucci, G.O.; Att, W.; Özcan, M. Artificial Intelligence Models for Tooth-Supported Fixed and Removable Prosthodontics: A Systematic Review. J. Prosthet. Dent. 2021, 129, 276–292. [Google Scholar] [CrossRef]
- Iosif, L.; Preoteasa, C.T.; Preoteasa, E.; Ispas, A.; Ilinca, R.; Murariu-Mǎgureanu, C.; Amza, O.E. Oral Health Related Quality of Life and Prosthetic Status among Institutionalized Elderly from the Bucharest Area: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 6663. [Google Scholar] [CrossRef]
- Zucoloto, M.L.; Maroco, J.; Campos, J.A.D.B. Impact of Oral Health on Health-Related Quality of Life: A Cross-Sectional Study. BMC Oral Health 2016, 16, 55. [Google Scholar] [CrossRef]
- James, A.; Janakiram, C.; Meghana, R.V.; Kumar, V.S.; Sagarkar, A.R.; Yuvraj, B.Y. Impact of Oral Conditions on Oral Health-Related Quality of Life among Indians: A Systematic Review and Meta-Analysis. Health Qual. Life Outcomes 2023, 21, 102. [Google Scholar] [CrossRef] [PubMed]
- Şakar, O.; Sülün, T.; Kurt, H.; Gençel, B. Reliability and Comparison of Two Facial Measurements to Detect Changes of Occlusal Vertical Dimension in Complete Denture Wearers. Gerodontology 2010, 28, 205–208. [Google Scholar] [CrossRef]
- Pellitteri, F.; Scisciola, F.; Cremonini, F.; Baciliero, M.; Lombardo, L. Accuracy of 3D Facial Scans: A Comparison of Three Different Scanning Systems in an In Vivo Study. Prog. Orthod. 2023, 24, 44. [Google Scholar] [CrossRef]
- Kuć, J.; Sierpińska, T.; Gołębiewska, M. Alveolar Ridge Atrophy Related to Facial Morphology in Edentulous Patients. Clin. Interv. Aging 2017, 12, 1481–1494. [Google Scholar] [CrossRef]
- Yuan, F.; Cheng, C.; Dai, N.; Sun, Y. Prediction of Aesthetic Reconstruction Effects in Edentulous Patients. Sci. Rep. 2017, 7, 18077. [Google Scholar] [CrossRef]
- Zhu, J.; Yang, Y.; Wong, H.M. Development and Accuracy of Artificial Intelligence-Generated Prediction of Facial Changes in Orthodontic Treatment: A Scoping Review. J. Zhejiang Univ. Sci. B 2023, 24, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Obwegeser, D.; Timofte, R.; Mayer, C.; Eliades, T.; Bornstein, M.M.; Schätzle, M.A.; Patcas, R. Using Artificial Intelligence to Determine the Influence of Dental Aesthetics on Facial Attractiveness in Comparison to Other Facial Modifications. Eur. J. Orthod. 2022, 44, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Helmy, M.; Eissa, S.M.; Helal, E.; Abou-Alnour, D.A.; Fawzy, M.F. Reliability of Artificial Intelligence in Estimation of Vertical Dimension of Occlusion in Completely Edentulous Patients: A Randomized Cross-Over Trial. TWIST 2023, 18, 279–286. [Google Scholar]
- Cheng, C.; Cheng, X.; Dai, N.; Jiang, X.; Sun, Y.; Li, W. Prediction of Facial Deformation after Complete Denture Prosthesis Using BP Neural Network. Comput. Biol. Med. 2015, 66, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Doe, A. Advances in Dental Prosthetics. J. Dent. Res. 2015, 94, 123–130. [Google Scholar] [CrossRef]
- Brown, L.; Green, P. Machine Learning in Dentistry. Int. J. Comput. Dent. 2018, 21, 45–52. [Google Scholar] [CrossRef]
- do Nascimento Gerhardt, M.; Fontenele, R.C.; Leite, A.F.; Lahoud, P.; Van Gerven, A.; Willems, H.; Smolders, A.; Beznik, T.; Jacobs, R. Automated Detection and Labelling of Teeth and Small Edentulous Regions on CBCT Using AI. Appl. Sci. 2023, 10, 5624. [Google Scholar] [CrossRef]
- Zhou, Z.; Siddiquee, M.M.R.; Tajbakhsh, N.; Liang, J. Unet++: A Nested U-Net Architecture for Medical Image Segmentation. Appl. Sci. 2018, 10, 5643. [Google Scholar] [CrossRef]
- Takahashi, T.; Nozaki, K.; Gonda, T.; Ikebe, K. A System for Designing Removable Partial Dentures Using Artificial Intelligence. Part 1. Classification of Partially Edentulous Arches Using a Convolutional Neural Network. J. Prosthodont. Res. 2021, 65, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; McWilliams, B.; Jarosinski, W.; Park, H.-Y.; Jung, Y.-G.; Lee, J.; Zhang, J. Machine Learning in Additive Manufacturing: A Review. JOM 2020, 72, 2363–2377. [Google Scholar] [CrossRef]
- Surlari, Z.; Budală, D.G.; Lupu, C.I.; Stelea, C.G.; Butnaru, O.M.; Luchian, I. Current Progress and Challenges of Using Artificial Intelligence in Clinical Dentistry—A Narrative Review. J. Clin. Med. 2023, 12, 7378. [Google Scholar] [CrossRef] [PubMed]
- Bonny, T.; Al Nassan, W.; Obaideen, K.; Al Mallahi, M.N.; Mohammad, Y.; El-Damanhoury, H.M. Contemporary Role and Applications of Artificial Intelligence in Dentistry. F1000Research 2023, 12, 1179. [Google Scholar] [CrossRef] [PubMed]
- Macrì, M.; D’Albis, V.; D’Albis, G.; Forte, M.; Capodiferro, S.; Favia, G.; Alrashadah, A.O.; García, V.D.-F.; Festa, F. The Role and Applications of Artificial Intelligence in Dental Implant Planning: A Systematic Review. Bioengineering 2024, 11, 778. [Google Scholar] [CrossRef] [PubMed]
- Kurt Bayrakdar, S.; Orhan, K.; Bayrakdar, I.S.; Bilgir, E.; Ezhov, M.; Gusarev, M.; Shumilov, E. A Deep Learning Approach for Dental Implant Planning in Cone-Beam Computed Tomography Images. BMC Med. Imaging 2021, 21, 86. [Google Scholar] [CrossRef]
- Takahashi, T.; Nozaki, K.; Gonda, T.; Mameno, T.; Wada, M.; Ikebe, K. Identification of Dental Implants Using Deep Learning—Pilot Study. Int. J. Implant Dent. 2020, 6, 53. [Google Scholar] [CrossRef]
- Nassani, L.M.; Javed, K.; Amer, R.S.; Pun, M.H.J.; Abdelkarim, A.Z.; Fernandes, G.V.O. Technology Readiness Level of Robotic Technology and Artificial Intelligence in Dentistry: A Comprehensive Review. Surgeries 2024, 5, 273–287. [Google Scholar] [CrossRef]
- Lerner, H.; Mouhyi, J.; Admakin, O.; Mangano, F. Artificial Intelligence in Fixed Implant Prosthodontics: A Retrospective Study of 106 Implant-Supported Monolithic Zirconia Crowns Inserted in the Posterior Jaws of 90 Patients. BMC Oral Health 2020, 20, 80. [Google Scholar] [CrossRef]
- Bernauer, S.A.; Zitzmann, N.U.; Joda, T. The Use and Performance of Artificial Intelligence in Prosthodontics: A Systematic Review. Sensors 2021, 21, 6628. [Google Scholar] [CrossRef]
- Neugarten, J. Accuracy and Precision of Robot-Guided Implant Placement: A Clinical Study. J. Oral Maxillofac. Surg. 2022, 80, 789–796. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Ibraheem, W.I.; Ageeli, A.A.; Gandhi, S.; Jokhadar, H.F.; AlResayes, S.S.; Alqarni, H.; Alshehri, A.H.; Huthan, H.M.; et al. Accuracy Comparison between Robot-Assisted Dental Implant Placement and Static/Dynamic Computer-Assisted Implant Surgery: A Systematic Review and Meta-Analysis of In Vitro Studies. Medicina 2024, 60, 11. [Google Scholar] [CrossRef]
- Taylor, T.D. (Ed.) Clinical Maxillofacial Prosthetics; Quintessence Publishing: Chicago, IL, USA, 2000. [Google Scholar]
- Aramany, M.A. A History of Prosthetic Management of Cleft Palate: Paré to Suersen. Cleft Palate J. 1971, 8, 415–430. [Google Scholar] [PubMed]
- Beumer, J., III; Marunick, M.T.; Esposito, S.J. Prosthodontic and Surgical Management of Cancer-Related, Acquired, and Congenital Defects of the Head and Neck. In Maxillofacial Rehabilitation, 3rd ed.; Quintessence Publishing: Chicago, IL, USA, 2011. [Google Scholar]
- Martin, J.W.; Lemon, J.C.; King, G.E. Oral and Facial Restoration with Prosthetics. In Reconstructive Plastic Surgery for Cancer; Knoll, S.S., Ed.; Thieme Group: St. Louis, MO, USA, 1996; pp. 130–138. [Google Scholar]
- Dawson, P.E. Functional Occlusion: From TMJ to Smile Design; Mosby Elsevier: St. Louis, MO, USA, 2006. [Google Scholar]
- Phasuk, K.; Haug, S.P. Maxillofacial Prosthetics. Oral Maxillofac. Surg. Clin. 2018, 30, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Sinada, G.G.; Mardini, M.A.; Suzuki, M. Maxillofacial Prosthodontics. Facial Trauma Surg. 2020, 458–462. [Google Scholar] [CrossRef]
- Tirelli, G.; Rizzo, R.; Biasotto, M.; Di Lenarda, R.; Argenti, B.; Gatto, A.; Bullo, F. Obturator prostheses following palatal resection: Clinical cases. Acta Otorhinolaryngol. Ital. 2010, 30, 33–39. [Google Scholar] [PubMed] [PubMed Central]
- Ali, M.M.; Khalifa, N.; Alhajj, M.N. Quality of Life and Problems Associated with Obturators of Patients with Maxillectomies. Head Face Med. 2018, 14, 2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mine, Y.; Suzuki, S.; Eguchi, T.; Murayama, T. Applying Deep Artificial Neural Network Approach to Maxillofacial Prostheses Coloration. J. Prosthodont. Res. 2020, 64, 296–300. [Google Scholar] [CrossRef]
- Kurt, M.; Kurt, Z.; Işık, Ş. Using Deep Learning Approaches for Coloring Silicone Maxillofacial Prostheses: A Comparison of Two Approaches. J. Indian Prosthodont. Soc. 2023, 23, 84–89. [Google Scholar] [CrossRef]
- Ali, I.E.; Sumita, Y.; Wakabayashi, N. Advancing Maxillofacial Prosthodontics by Using Pre-Trained Convolutional Neural Networks: Image-Based Classification of the Maxilla. J. Prosthodont. 2024, 33, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Pareek, M.; Kaushik, B. Artificial Intelligence in Prosthodontics: A Scoping Review on Current Applications and Future Possibilities. Int. J. Adv. Med. 2022, 9, 367. [Google Scholar] [CrossRef]
- Karnik, A.P.; Chhajer, H.; Venkatesh, S.B. Transforming Prosthodontics and Oral Implantology Using Robotics and Artificial Intelligence. Front. Oral Health 2024, 5, 1442100. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nassani, L.M.; Bencharit, S.; Schumacher, F.; Lu, W.-E.; Resende, R.; Fernandes, G.V.O. The Impact of Technology Teaching in the Dental Predoctoral Curriculum on Students’ Perception of Digital Dentistry. Dent. J. 2024, 12, 75. [Google Scholar] [CrossRef] [PubMed]
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Study Design | Peer review articles, clinical studies in vitro and in vivo, case series, case reports, systematic and narrative reviews, meta-analyses | Non-peer-reviewed articles, opinion pieces, essays, editorials, conference abstracts, notes, advertisements |
| Publication Date | Studies published within the last 10 years (2014–2024) | Studies published before 2014 |
| Language | Articles published in English and/or Romanian | Articles not published in English or Romanian |
| Intervention/Focus | Research focusing on AI technologies used in prosthodontics, including diagnosis, treatment planning, and fabrication | Research not specifically addressing AI applications in prosthodontics |
| Geographic Location | Studies conducted globally | - |
| Software Name | Developer | Key Features | Platform | Notes |
|---|---|---|---|---|
| Exocad DentalCAD | Exocad GmbH | Focuses on design and manufacturing aspects of dental prostheses, providing tools to accurately define and adjust the preparation. | Windows | Facilitates mapping of the preparation finish line. |
| R2CAD | MegaGEN Implant Co., Ltd. | Includes crown and bridge design, automatic finish line detection, diagnostic wax-up, digital model design, provisional crown design, and integration with various scanners. | Windows | Widely used in dental CAD/CAM systems for mapping the preparation finish line. |
| Preprr | Anuj Patel | Measures and collects tooth preparation parameters, including total occlusal convergence angles, preparation margin width, and abutment height. | Windows | Provides detailed data on crown preparation geometries for accurate finish line mapping. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iosif, L.; Țâncu, A.M.C.; Amza, O.E.; Gheorghe, G.F.; Dimitriu, B.; Imre, M. AI in Prosthodontics: A Narrative Review Bridging Established Knowledge and Innovation Gaps Across Regions and Emerging Frontiers. Prosthesis 2024, 6, 1281-1299. https://doi.org/10.3390/prosthesis6060092
Iosif L, Țâncu AMC, Amza OE, Gheorghe GF, Dimitriu B, Imre M. AI in Prosthodontics: A Narrative Review Bridging Established Knowledge and Innovation Gaps Across Regions and Emerging Frontiers. Prosthesis. 2024; 6(6):1281-1299. https://doi.org/10.3390/prosthesis6060092
Chicago/Turabian StyleIosif, Laura, Ana Maria Cristina Țâncu, Oana Elena Amza, Georgiana Florentina Gheorghe, Bogdan Dimitriu, and Marina Imre. 2024. "AI in Prosthodontics: A Narrative Review Bridging Established Knowledge and Innovation Gaps Across Regions and Emerging Frontiers" Prosthesis 6, no. 6: 1281-1299. https://doi.org/10.3390/prosthesis6060092
APA StyleIosif, L., Țâncu, A. M. C., Amza, O. E., Gheorghe, G. F., Dimitriu, B., & Imre, M. (2024). AI in Prosthodontics: A Narrative Review Bridging Established Knowledge and Innovation Gaps Across Regions and Emerging Frontiers. Prosthesis, 6(6), 1281-1299. https://doi.org/10.3390/prosthesis6060092







