A Randomized Controlled Clinical Trial on Press, Block Lithium Disilicate, and 3D Printed Partial Crowns in Posterior Teeth: One-Year Recall
Abstract
1. Introduction
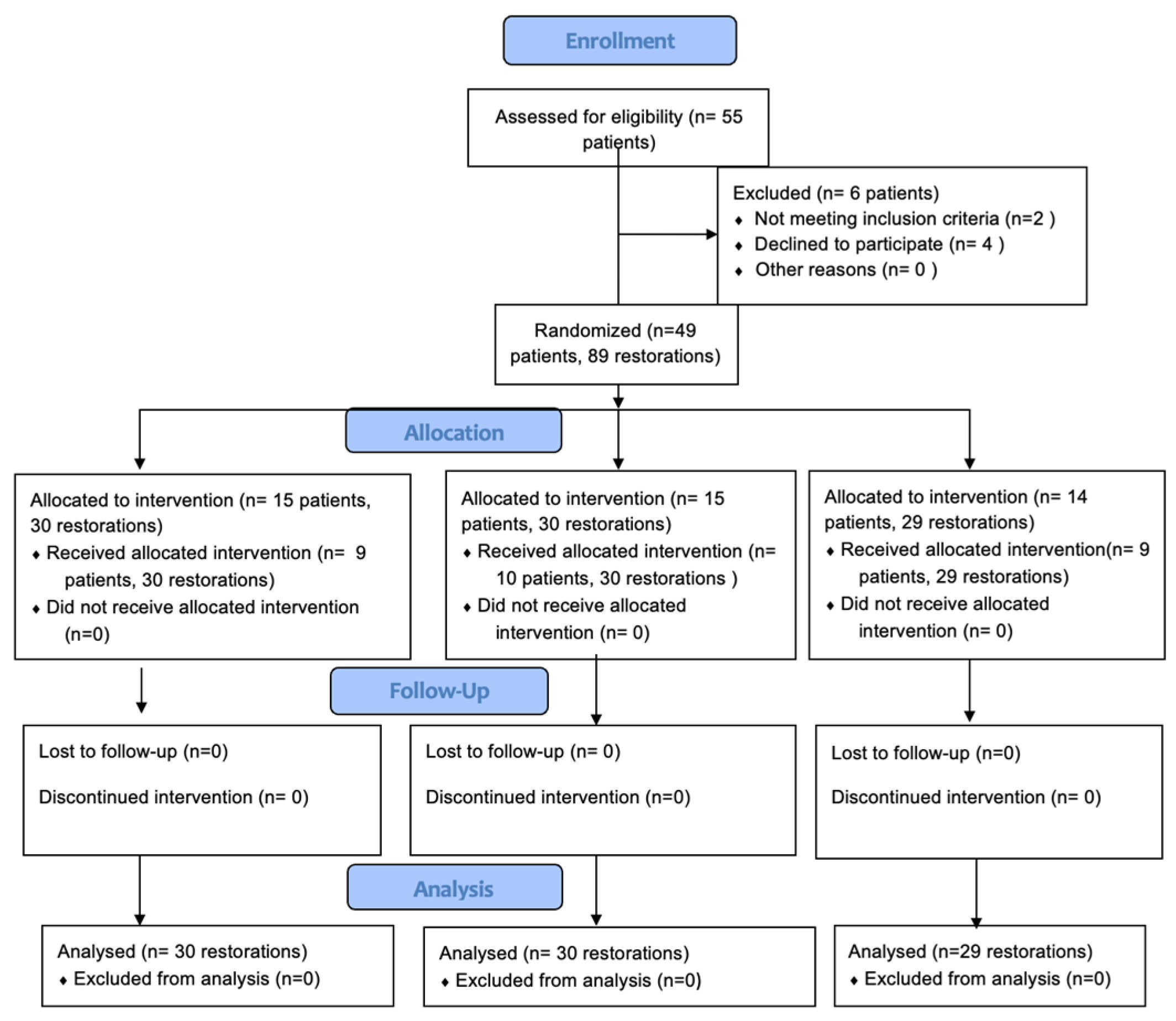
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manhart, J.; Chen, H.Y.; Hamm, G.; Hickel, R. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper. Dent. 2004, 29, 481–508. [Google Scholar] [PubMed]
- Bresser, R.A.; Hofsteenge, J.W.; Wieringa, T.H.; Braun, P.G.; Cune, M.S.; Özcan, M.; Gresnigt, M.M.M. Clinical longevity of intracoronal restorations made of gold, lithium disilicate, leucite, and indirect resin composite: A systematic review and meta-analysis. Clin. Oral. Inv. 2023, 27, 4877–4896. [Google Scholar] [CrossRef]
- Alharbi, A.; Ardu, S.; Bortolotto, T.; Krejci, I. Stain susceptibility of composite and ceramic CAD/CAM blocks versus direct resin composites with different resinous matrices. Odontology 2017, 105, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Wilkins, G.N. 3D printing in dentistry—Exploring the new horizons. J. Dent. Sci. 2021, 16, 1037–1038. [Google Scholar] [CrossRef] [PubMed]
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef] [PubMed]
- Torabi, K.; Farjood, E.; Hamedani, S. Rapid prototyping technologies and their applications in prosthodontics, a review of literature. J. Dent. 2015, 16, 1–9. [Google Scholar]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical Properties of 3D-Printed and Milled Composite Resins for Definitive Restorations: An In Vitro Comparison of Initial Strength and Fatigue Behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef]
- Martín-Ortega, N.; Sallorenzo, A.; Casajús, J.; Cervera, A.; Revilla-León, M.; Gómez-Polo, M. Fracture resistance of additive manufactured and milled implant-supported interim crowns. J. Prosthet. Dent. 2022, 127, 267–274. [Google Scholar] [CrossRef]
- Valenti, C.; Isabella Federici, M.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022, 132, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.; Ender, A.; Egli, G.; Özcan, M.; Mehl, A. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin. Oral Investig. 2019, 23, 2777–2784. [Google Scholar] [CrossRef] [PubMed]
- Corbani, K.; Hardan, L.; Skienhe, H.; Özcan, M.; Alharbi, N.; Salameh, Z. Effect of material thickness on the fracture resistance and failure pattern of 3D-printed composite crowns. Int. J. Comput. Dent. 2020, 23, 225–233. [Google Scholar]
- Casucci, A.; Verniani, G.; Barbieri, A.L.; Ricci, N.M.; Ferrari Cagidiaco, E.; Ferrari, M. Flexural Strength Analysis of Different Complete Denture Resin-Based Materials Obtained by Conventional and Digital Manufacturing. Materials 2023, 16, 6559. [Google Scholar] [CrossRef]
- Cerbino, V.; Verniani, G.; Bonadeo, G.; Ferrari Cagidiaco, E. Dimensional stability of 3D-printed fixed prosthetic restorations. J. Osseointegr. 2022, 15, 79–86. [Google Scholar]
- Çakmak, G.; Steigmeier, D.; Güven, M.E.; Yilmaz, D.; Schimmel, M.; Yoon, H.I.; Yilmaz, B. Fabrication Trueness, Intaglio Surface Adaptation, and Marginal Integrity of Resin-Based Onlay Restorations Fabricated by Additive and Subtractive Manufacturing. Int. J. Prosthodont. 2024, 37, 99–107. [Google Scholar] [CrossRef]
- Cantó-Navés, O.; Michels, K.; Figueras-Alvarez, O.; Fernández-Villar, S.; Cabratosa-Termes, J.; Roig, M. In Vitro Comparison of Internal and Marginal Adaptation between Printed and Milled Onlays. Materials 2023, 16, 6962. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J. Additive Manufacturing for Complete Denture Fabrication: A Narrative Review. J. Prosthodont. 2022, 31, 47–51. [Google Scholar] [CrossRef]
- No-Cortes, J.; Ayres, A.P.; Lima, J.F.; Markarian, R.A.; Attard, N.J.; Cortes, A.R.G. Trueness, 3D Deviation, Time and Cost Comparisons Between Milled and 3D-Printed Resin Single Crowns. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 107–112. [Google Scholar]
- Baldissara, P.; Monaco, C.; Onofri, E.; Fonseca, R.G.; Ciocca, L. Fatigue resistance of monolithic lithium disilicate occlusal veneers: A pilot study. Odontology 2019, 107, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Malament, K.A.; Margvelashvili-Malament, M.; Natto, Z.S.; Thompson, V.; Rekow, D.; Att, W. 10.9-year survival of pressed acid etched monolithic e.max lithium disilicate glass-ceramic partial coverage restorations: Performance and outcomes as a function of tooth position, age, sex, and the type of partial coverage restoration (inlay or onlay). J. Prosthet. Dent. 2021, 126, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Malament, K.A.; Margvelashvili-Malament, M.; Natto, Z.S.; Thompson, V.; Rekow, D.; Att, W. Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: Performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J. Prosthet. Dent. 2021, 126, 533–545. [Google Scholar] [PubMed]
- Ruse, N.D.; Sadoun, M.J. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef] [PubMed]
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Verniani, G.; Ferrari, M.; Manfredini, D.; Ferrari Cagidiaco, E. A Randomized Controlled Clinical Trial on Lithium Disilicate Veneers Manufactured by the CAD–CAM Method: Digital Versus Hybrid Workflow. Prosthesis 2024, 6, 329–340. [Google Scholar] [CrossRef]
- Larson, T.D. The clinical significance of marginal fit. Northwest Dent. 2012, 91, 22–29. [Google Scholar] [PubMed]
- Rocca, G.T.; Krejci, I. Bonded indirect restorations for posterior teeth: From cavity preparation to provisionalization. Quintessence Int. 2007, 38, 371–379. [Google Scholar] [PubMed]
- Rosentritt, M.; Rauch, A.; Hahnel, S.; Schmidt, M. In-vitro performance of subtractively and additively manufactured resin-based molar crowns. J. Mech. Behav. Biomed. Mater. 2023, 141, 105806. [Google Scholar] [CrossRef]
- Çakmak, G.; Donmez, M.B.; de Paula, M.S.; Akay, C.; Fonseca, M.; Kahveci, Ç.; Abou-Ayash, S.; Yilmaz, B. Surface roughness, optical properties, and microhardness of additively and subtractively manufactured CAD-CAM materials after brushing and coffee thermal cycling. J. Prosthodont. 2023. early review. [Google Scholar] [CrossRef]
- Daghrery, A. Color Stability, Gloss Retention, and Surface Roughness of 3D-Printed versus Indirect Prefabricated Veneers. J. Funct. Biomater. 2023, 14, 492. [Google Scholar] [CrossRef]
- Çakmak, G.; Oosterveen-Rüegsegger, A.L.; Akay, C.; Schimmel, M.; Yilmaz, B.; Donmez, M.B. Influence of polishing technique and coffee thermal cycling on the surface roughness and color stability of additively and subtractively manufactured resins used for definitive restorations. J. Prosthodont. 2023, 33, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Bauer, R.; Zacher, J.; Strasser, T.; Schmid, A.; Rosentritt, M. Survival dependence of 3D-printed temporary materials on the filler content. Int. J. Comput. Dent. 2023, 26, 159–166. [Google Scholar] [PubMed]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Prechtel, A.; Stawarczyk, B.; Hickel, R.; Edelhoff, D.; Reymus, M. Fracture load of 3D printed PEEK inlays compared with milled ones, direct resin composite fillings, and sound teeth. Clin. Oral Investig. 2020, 24, 3457–3466. [Google Scholar] [CrossRef] [PubMed]
| Topics | Score | Criteria |
|---|---|---|
| Marginal adaptation (MARA) | Alpha | Margin continuity (without prominence or crack) |
| Bravo | Little discontinuity detectable by explorer, but does not require replacement | |
| Charlie | Prominence or crack; require replacement | |
| Color Alteration (COA) | Alpha | No color alteration close to tooth structure |
| Bravo | Little color alteration, clinically acceptable | |
| Charlie | Esthetically unacceptable | |
| Marginal Discoloration (MARD) | Alpha | No marginal discoloration |
| Bravo | Marginal discoloration | |
| Charlie | Deep discoloration | |
| Restoration Fracture (RESF) | Alpha | No fracture |
| Bravo | Small fracture fragments (1/4 of the restoration) | |
| Charlie | Severe fracture (3/4 of the restoration) | |
| Tooth Fracture (TFRA) | Alpha | No tooth fracture |
| Bravo | Small fracture fragments of tooth fracture (1/4) | |
| Charlie | Severe tooth fracture (1/2) | |
| Restoration wear (RESW) | Alpha | No wear |
| Bravo | Wear | |
| Antagonist Tooth Wear (ANTW) | Alpha | No wear |
| Bravo | Wear | |
| Caries Presence (CARP) | Alpha | Absent |
| Charlie | Present | |
| Postoperative Sensitivity (POSTS) | Alpha | Absent |
| Charlie | Present |
| Topics | Material | Baseline | Time 1 | ||||
|---|---|---|---|---|---|---|---|
| Alpha | Bravo | Charlie | Alpha | Bravo | Charlie | ||
| Marginal adaptation (MARA) | Lisi Press | 30 | / | / | 29 | 1 | / |
| Lisi Blocks | 30 | / | / | 29 | 1 | / | |
| Temp Print | 29 | / | / | 27 | 2 | / | |
| Color Alteration (COA) | Lisi Press | 30 | / | / | 30 | / | / |
| Lisi Blocks | 30 | / | / | 30 | / | / | |
| Temp Print | 27 | 2 | / | 26 | 3 | / | |
| Marginal Discoloration (MARD) | Lisi Press | 30 | / | / | 29 | 1 | / |
| Lisi Blocks | 30 | / | / | 29 | 1 | / | |
| Temp Print | 29 | / | / | 27 | 2 | / | |
| Restoration Fracture (RESF) | Lisi Press | 30 | / | / | 29 | 1 | / |
| Lisi Blocks | 30 | / | / | 29 | 1 | / | |
| Temp Print | 29 | / | / | 29 | / | / | |
| Tooth Fracture (TFRA) | Lisi Press | 30 | / | / | 30 | / | / |
| Lisi Blocks | 30 | / | / | 30 | / | / | |
| Temp Print | 29 | / | / | 29 | / | / | |
| Restoration wear (RESW) | Lisi Press | 30 | / | / | 30 | / | / |
| Lisi Blocks | 30 | / | / | 29 | 1 | / | |
| Temp Print | 29 | / | / | 29 | / | / | |
| Antagonist Tooth Wear (ANTW) | Lisi Press | 30 | / | / | 30 | / | / |
| Lisi Blocks | 30 | / | / | 29 | 1 | / | |
| Temp Print | 29 | / | / | 29 | / | / | |
| Caries Presence (CARP) | Lisi Press | 30 | / | / | 30 | / | / |
| Lisi Blocks | 30 | / | / | 30 | / | / | |
| Temp Print | 29 | / | / | 29 | / | / | |
| Postoperative Sensitivity (POSTS) | Lisi Press | 30 | / | / | 30 | / | / |
| Lisi Blocks | 30 | / | / | 30 | / | / | |
| Temp Print | 29 | / | / | 29 | / | / | |
| PI | PPD | BoP | |
|---|---|---|---|
| Group 1 (Initial LD Press) | 17.5 ± 2.5 a | 2.9 ± 0.5 mm a | 16.1 ± 0.5 a |
| Group 2 (Initial LD Block) | 17.0 ± 1 a | 2.8 ± 0.5 mm a | 16.0 ± 1.2 a |
| Group 3 (Temp Print) | 17.7 ± 1.5 a | 2.9 ± 0.5 mm a | 16.0 ± 1.7 a |
| PI | PPD | BoP | |
|---|---|---|---|
| Group 1 (Initial LiSi Press) | 17.5 ± 2.5 a | 2.9 ± 0.5 mm a | 16.1 ± 0.5 a |
| Group 2 (Initial LiSi Block) | 17.0 ± 1 a | 2.8 ± 0.5 mm a | 16.8 ± 1.2 a |
| Group 3 (Temp Print) | 17.5 ± 1 a | 2.6 ± 1 mm a | 16.3 ± 0.5 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verniani, G.; Casucci, A.; Val, M.; Ruggiero, G.; Manfredini, D.; Ferrari, M.; Ferrari Cagidiaco, E. A Randomized Controlled Clinical Trial on Press, Block Lithium Disilicate, and 3D Printed Partial Crowns in Posterior Teeth: One-Year Recall. Prosthesis 2024, 6, 887-895. https://doi.org/10.3390/prosthesis6040064
Verniani G, Casucci A, Val M, Ruggiero G, Manfredini D, Ferrari M, Ferrari Cagidiaco E. A Randomized Controlled Clinical Trial on Press, Block Lithium Disilicate, and 3D Printed Partial Crowns in Posterior Teeth: One-Year Recall. Prosthesis. 2024; 6(4):887-895. https://doi.org/10.3390/prosthesis6040064
Chicago/Turabian StyleVerniani, Giulia, Alessio Casucci, Matteo Val, Gennaro Ruggiero, Daniele Manfredini, Marco Ferrari, and Edoardo Ferrari Cagidiaco. 2024. "A Randomized Controlled Clinical Trial on Press, Block Lithium Disilicate, and 3D Printed Partial Crowns in Posterior Teeth: One-Year Recall" Prosthesis 6, no. 4: 887-895. https://doi.org/10.3390/prosthesis6040064
APA StyleVerniani, G., Casucci, A., Val, M., Ruggiero, G., Manfredini, D., Ferrari, M., & Ferrari Cagidiaco, E. (2024). A Randomized Controlled Clinical Trial on Press, Block Lithium Disilicate, and 3D Printed Partial Crowns in Posterior Teeth: One-Year Recall. Prosthesis, 6(4), 887-895. https://doi.org/10.3390/prosthesis6040064








