Abstract
The number of people with diabetes is rising day-by-day, which also raises the incidence of diabetic ulcers, sensation loss in the foot’s plantar area, and in extreme instances, amputations. Using customized shoes, unloading orthoses, insoles, and other strategies may help control these issues to some degree. In this work, a novel modular diabetic insole was designed and fabricated to effectively offload the abnormal or peak plantar pressures in diabetic patients. The pressure values in the plantar region were quantified using an in-house-developed plantar pressure-measuring insole consisting of force sensitive resistor (FSR) sensors. The effectiveness of the modular diabetic insole was tested qualitatively and quantitatively. The qualitative performance of the insole was reported using Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) in terms of subjective parameters like comfort, ease of use, effectiveness, etc. and calculated as 4.7 ± 0.18. Thereafter, the wearable pressure-measuring insole was used to investigate the feasibility of modular insole for the plantar pressure offloading during standing and walking conditions. It was observed that the maximum average zonal pressure (AZP) was reduced by up to 99% from 121.30 ± 3.72 kPa to 0.22 ± 0.18 kPa for the standing condition whereas it was reduced to 6.76 ± 2.03 kPa from 197.71 ± 3.21 kPa with a percentage value of 96% for the walking condition. In conclusion, the findings of this work validate the effectiveness of the modular diabetic insole as an intervention tool for diabetic foot ulcer prevention.
1. Introduction
With 382 million cases globally, diabetes is one of the main causes of chronic illness and limb loss. It is estimated that 592 million instances of diabetes will be recorded by 2035 [1,2,3]. Diabetic foot disease is widespread, and as the population ages and the obesity pandemic persists, so too will its frequency. Peripheral diabetic neuropathy is a condition that affects the nerves of the feet in patients with diabetes. Due to this condition, patients may experience a loss of sensation in their feet, which makes them unable to feel pain or discomfort. As a result, they may suffer from repetitive minor injuries caused by internal factors such as calluses, nails, or foot deformities, and external factors such as shoes, burns, or foreign bodies. These injuries often go unnoticed at the time of occurrence due to the lack of sensation in the feet and can eventually lead to foot ulceration [4,5,6]. Diabetic foot ulcers (DFUs) are only one of the many problems that may occur in diabetic patients. These are a prevalent consequence of diabetes mellitus that has been on the rise in recent decades. It is estimated that about 5% of all patients with diabetes have a history of foot ulceration, while the lifetime risk of diabetic patients developing this complication is 15% [7,8]. It was reported in the literature that an estimated 80% of lower limb amputations resulting from diabetes were preceded by the development of foot ulcers. Foot ulcers are a common complication of diabetes and typically occur due to a combination of factors such as nerve damage, poor circulation, and high blood sugar levels. These ulcers are usually induced by acute, repeated, or thermal damage and appear in the regions of peak mechanical stress [9,10].
An early diagnosis and medication can help mitigate and prevent ulceration, but it is possible only in a non-neuropathic foot, i.e., before the ulcer starts to protrude but the tissue starts to produce pain. However, diagnosis becomes extremely complicated and difficult in cases with peripheral neuropathy in the foot, which has been observed to be a common occurrence in diabetic patients. Common interventions for protruding diabetic ulcers include pressure offloading techniques such as using crutches, special foot orthotics, and custom pressure offloading insoles. Conservative orthotic care may be used to unload a foot ulcer, allowing the patient to continue being somewhat active [11]. By considerably reducing plantar pressure, these orthotic devices relieve tension at the afflicted area and aid in the healing of ulceration [12]. The goal of the medical intervention is to reallocate the pressure at the plantar fascia that is responsible for ulcers. For this reason, a range of materials with varying density, cushioning effect, and shock absorption may be used to create the foot orthoses, allowing them to be customized to the patient’s specifications. When opposed to prefabricated orthoses, customized foot orthoses provide superior therapy because they make complete contact with the plantar area of the foot [13,14,15,16].
Diabetes patients have increased plantar pressures [17,18], which may result in ulceration or re-ulceration at new places. Previous research [18,19,20,21,22] has shown that lowering plantar pressure may successfully lower the diabetic population’s risk of these issues. Sutkowska et al. [23] studied the medical records of a diabetic group and observed significant variation in the plantar pressure across the patients. The forefoot and heel were shown to be areas of elevated plantar pressure in a study by Caselli et al. [24] on under-foot pressure in a diabetic population. Increasing pressure was found to be correlated with an increase in the severity of neuropathic disease. A force-measuring platform was used in research by Cock et al. [25] to determine the centre of pressure and plantar pressure. The findings of the work quantified a significant difference in the result values across different gait phases of participants. In recent studies, sensor-based insoles were more attractive than platform solutions because patients may use them outside of the clinic to capture data over time [26,27]. Several such studies evaluated shoe-based pressure measurement devices during walking or running, in contrast to platform systems [28,29]. The majority of these devices included numerous sensing locations and a wireless data transmission protocol. Force-sensitive resistors or piezoresistive materials were often utilized to provide the flexibility of the sensors [30,31].
It was found in the literature that the custom pressure offloading insoles offered the same benefits as the total contact cast, i.e., TCC, without most of its demerits. When used in combination with stable walking shoes, custom-made insoles have been found to offer a range of benefits for the foot compared to prefabricated insoles. Specifically, while prefabricated insoles are able to provide overall good cushioning outcomes, custom insoles have been shown to also reduce pressure in the heel region effectively, making walking more comfortable and less likely to cause discomfort or pain. Additionally, custom insoles have been shown to significantly offload plantar pressure in both the forefoot and rearfoot regions of the foot, which has not been observed in prefabricated insoles. Thus, custom insoles can help to reduce the pressures at the important foot locations and thereby minimize the risk of injury or discomfort and support overall foot health [32,33,34]. However, producing custom insoles is a tedious process requiring significant attention to detail [35,36]. A skilled clinician and technician is required to scan the patient’s feet, model the insole via a parametric computer-aided design (CAD) tool, and produce the finished product in a small workshop using various fabrication techniques. The entire process takes several days, failing to provide a prompt solution of isolating and offloading pressure from the ulceration prone zone. Additionally, such a set up incurs significant capital, increasing the cost of the insole as well as follow-up treatment [17,37,38,39,40]. To overcome these challenges, a novel customized and cost-effective, nearly standardized insole is needed, which can offload pressure effectively from any given region on the plantar surface of the diabetic foot. Moreover, the insole must have comfort and shock attenuation properties, especially at the heel, and support the whole plantar region of the foot. The proposed work plan was focused on the development and validation of a customized insole to offload plantar pressure and reduce pain, as an ulceration prevention measure, which can be an effective ulcer intervention during wound care, and as a postoperative medical care or intervention.
2. Materials and Methods
The modular diabetic insole works on removing supporting segments to generate a void under the ulcerated region for offloading pressure. This section describes the design, fabrication, pressure measurement device, and testing protocol of the modular diabetic pressure offloading insole.
2.1. Geometrical Modelling and Design of Modular Insole
A standard UK-8 insole size was considered to design and fabricate the proposed insole. Using SolidWorks 2021 (Dassault Systèmes, Paris, France), the outer boundary of the mid-frame insole was generated in conformance with the Mondopoint system as outlined in ISO 9407:2019 [41]. Figure 1 shows the components of the modular insole, namely, the mid-frame and 14 unique moulded silicone rubber inserts. In line with literature studies [19,42] that outlined the most common regions exhibiting abnormal or peak plantar pressures in diabetic patients, the internal area of the mid-frame was segmented into 14 regions, as illustrated in Figure 2.
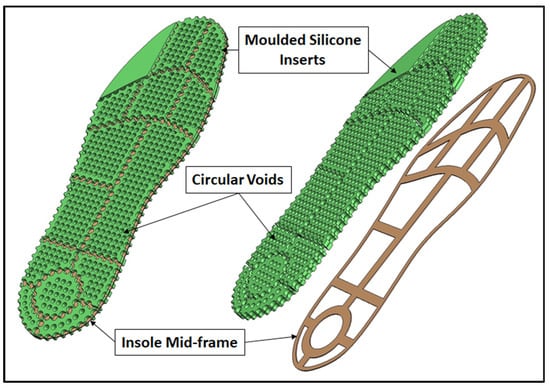
Figure 1.
Design of modular diabetic pressure offloading insole.
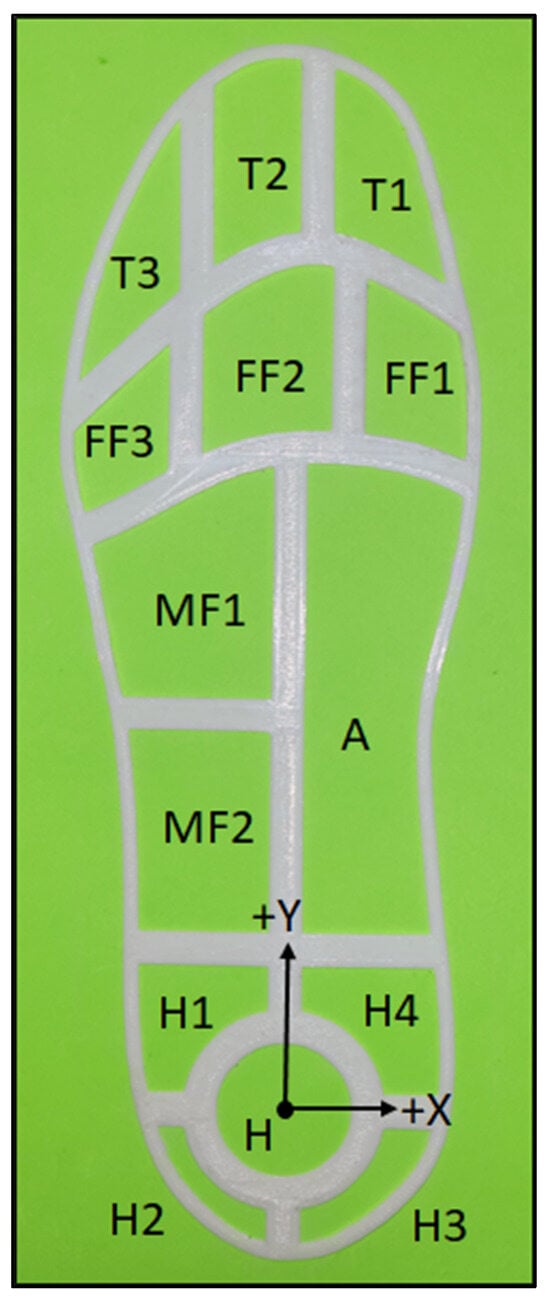
Figure 2.
Segments of the mid-frame of the modular diabetic insole.
In the toe region of the foot, area T1 supported the hallux, area T2 supported the second toe, and area T3 supported toes 3–5. The forefoot region was divided into three segments, i.e., medial forefoot (FF1), central forefoot (FF2), and lateral forefoot (FF3). The lateral midfoot region was divided into two segments, namely MF1 and MF2, the latter lying closer to the heel region. A single segment denoted by A supported the insole area under the medial midfoot region. The heel region was divided into a total of five segments, with H1 and H2 on the lateral side of the foot, H3 and H4 on the medial side of the foot, and H in the central part of the heel region at the ball of the foot. Each segmented region in the mid-frame housed its respective moulded silicone insert, designed to be individually removable and reattachable. The mid-frame was 0.6 mm thick and 3D-printed using an Ender-3 S1 Pro (Shenzhen Creality 3D Technology Co, Ltd., China). Since the mid-frame is subjected to large stretching and bending stresses during walking, thermoplastic polyurethane (TPU) of Shore hardness 95A was selected to sustain the considered stress scenarios. The inserts were designed with grooves with widths and depths of 0.6 mm and 3 mm, respectively. The groove was cut along each insert’s periphery, midway through the thickness of the insert, as shown in Figure 3. The groove allowed the inserts to be locked in the corresponding segments in the mid-frame. All inserts had an overall thickness of 6 mm, which was found to be sufficient to maintain a gap between the floor of the shoe and the plantar surface of the foot during maximum compression of the insole.
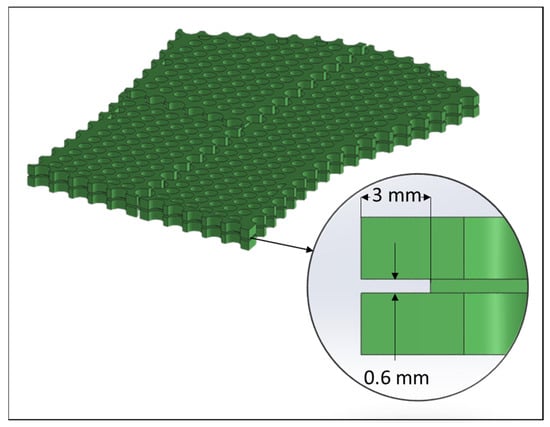
Figure 3.
Groove geometry in the silicone inserts.
As shown in Figure 1, cylindrical voids were designed to facilitate better insole compression. The through-hole circular voids were homogeneously spaced, 4.5 mm apart in both the horizontal and vertical directions, such that each insert had roughly a 45% void density by volume. Additionally, this improved the breathability and cushioning properties when compared with a moulded silicone rubber insole with no voids. The inserts were made of liquid silicone rubber (LSR) of Shore 10A hardness (Chemzest Enterprises, Chennai, India). Silicone rubber was used because of its ease of manufacturing, bioinert properties, and excellent wear-resistant properties. Figure 4 shows the 3D-printed two-part split moulds used to develop the inserts for the modular insole.
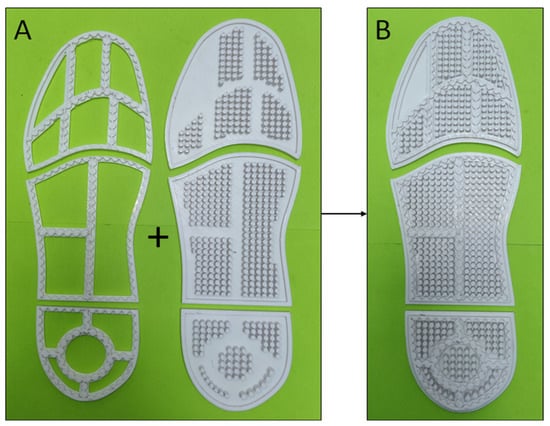
Figure 4.
Three-dimensional-printed two-part split moulds for silicone insert moulding; (A, Left) mould wall with groove forming geometry, (A, Right) mould base with circular void-forming geometry; (B)—assembled mould for fabrication.
The assembled insole was placed inside a zipped pouch made of a soft and stretchable fabric, stitched in the shape of the insole. This helped in reducing friction between the foot and the insole, improving comfort, and abating further risk of ulceration by preventing a direct contact of the silicone inserts with the plantar surface of the foot. The pouch would also comply with changes in dimensions over the truncated region of the modular insole when compressed and flexed during ambulation. Figure 5 shows the procedure for using the modular diabetic insole.
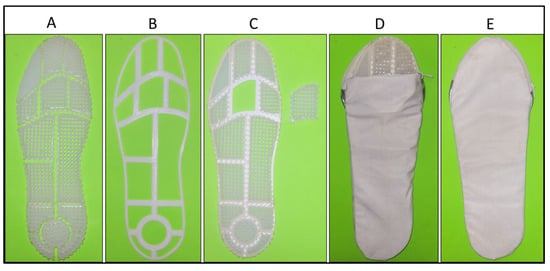
Figure 5.
(A) Fourteen silicone inserts; (B) mid-frame; (C) silicone inserts assembled with FF2 region truncated as an example; (D) modular insole placed in the pouch; (E) pouch zip closed for placing inside the shoe.
2.2. Plantar Pressure-Measuring Insole
A wearable plantar pressure-measuring insole was developed to validate the extent of pressure offloading offered by the modular insole after removing any insert. The insole consisted of force sensitive resistor (FSR) sensors (Interlink Electronics, Inc., California, USA) placed in the centres of 11 segments of the diabetic insole. The FSR sensor had an effective sensing region constrained within a diameter of 12.5 mm. Regions T3, H2, and H3 were not probed as the areas were too small or the regions would show insignificant pressure magnitudes for the occurrence or progression of the ulceration [19,42]. Table 1 shows the location of the centre of each sensor in the pressure-measuring insole with the centre of segment H as the origin (Figure 2).

Table 1.
Location of sensor centres in the pressure-measuring insole.
Figure 6 shows the pressure-measuring insole with electronic hardware and FSR sensors. One side of the FSR sensors was pasted on a 2 mm thick ethylene-vinyl acetate (EVA) foam sheet cut in the shape of a UK-8-size insole. Similarly, the other face of the sensors was covered with a 0.6 mm thick 3D printed-PLA sheet, which provided the FSR sensors with a solid reactive surface for accurate data acquisition. All sensors were connected to the microcontroller board (Teensy 4.1 Development Board, PJRC.COM, LLC., Sherwood, OR, USA) through a voltage divider circuit [43,44]. A 20-band flat ribbon cable (FRC) was used to connect the sensors in the insole to the electronics hardware. The microcontroller board was fixed inside a simple cardboard box which was tied onto the volunteer’s leg using a Velcro strap during all trials in this study.
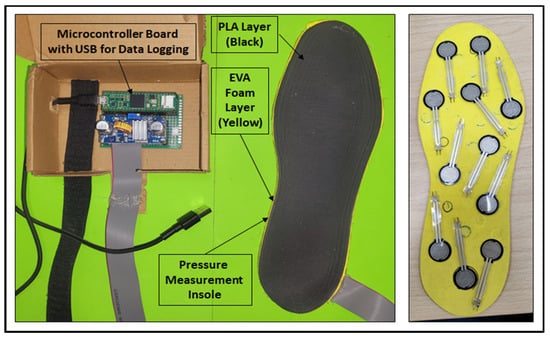
Figure 6.
Pressure-measuring insole with the wearable electronics hardware (left); internal layout of FSR sensors sandwiched between the EVA (Yellow) and PLA (Black) layers (right).
2.3. Data Measurement
The code was written and compiled in the Arduino Integrated Development Environment (IDE). The sensor data were polled at a maximum rate of approximately 5000 complete scans per second, where a complete scan was defined as the time it took the microcontroller to complete one iteration of the entire code and finally display the conditioned values of each sensor. For quantitative trials, two types of data were computed for each of the 11 probed regions, i.e., the running average of plantar pressures at a sampling rate of 20 ms per scan and the maximum values of pressures per sensor that occurred anytime during the time period of the trial. During trials, the pressure-measuring insole was placed under the modular insole inside the shoe, the data were displayed on the serial monitor in the Arduino IDE software (ver. 2.3.2) and the computed data were recorded from the microcontroller board to a laptop via a USB cable.
2.4. Demographics
The modular diabetic insole was tested quantitatively and qualitatively to assess its performance. The cohort for testing the modular insole consisted of 10 healthy participants with a foot size of UK 8. All participants were male, between the ages of 22 years and 32 years. The weight ranged from 55 kg to 90 kg, with an average weight of 68 kg. No participants had any external injury in the foot and no foot deformations or abnormalities were present. As this design was an initial proof-of-concept model, it was deemed safer to study its performance and effects on healthy participants prior to testing on diabetic patients to get rudimentary performance metrics for the insole. This would also allow the design to be significantly improved based on the feedback from this study, leading to more accurate results during clinical trials in the future. The study was approved by the Ethical Committee of the Indian Institute of Technology Delhi (IIT-Delhi, New Delhi, India). The volunteers provided a signed consent form before the study was conducted.
2.5. Qualitative Tests
Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) [45,46,47] was used to ascertain the qualitative performance of the insole. The user’s satisfaction with the modular insole was evaluated using the device subscale of the QUEST 2.0 questionnaire. It is an eight-item instrument for judging an assistive device’s subjective parameters like comfort, ease of use, effectiveness, etc. All such parameters are scored on a scale of 1 to 5, where 5 indicates high satisfaction, and 1 indicates complete dissatisfaction. Initially, participants were asked to wear the footwear with a generic EVA insole to create a baseline of comfort against which the comfort of the proposed insole was marked. The qualitative study was then performed through two cases, Q1 and Q2. The first case (Q1) recorded QUEST scores for the modular insole with all inserts included in the mid-frame for each participant. The second case (Q2) involved all participants scoring the performance of the modular insole with each of the 14 inserts removed one at a time. Different movements like walking, jumping, and jogging were used to evaluate parameters like cushioning in different regions of the insole, fit of the insole, noticeability of different inserts, noticeability of the truncated region, etc. The overall QUEST scores were compared for Q1 and Q2, indicating the feasibility of the insole in providing satisfactory comfort even after inserts were removed for offloading pressure.
2.6. Quantitative Tests
The wearable pressure-measuring insole was used to test the modular insole for the feasibility of plantar pressure offloading during standing (referred to as case S) and walking (referred to as case W). The test setup included a pair of shoes with their original insole removed and replaced with the pressure-measuring insole stacked under the modular diabetic insole. In both cases, S and W, every participant first tested the modular insole with all inserts attached, hereby referred to as S (full) and W (full). Following this, 9 out of the 14 total inserts (T1, FF1, FF2, FF3, MF1, MF2, H1, H4, and H) were removed one at a time, and plantar pressures were recorded for each subcase per participant. During offloading trials, S or W followed by the insert name was used to refer to the removed insert for the trials, e.g., W (FF2) would refer to the trial during walking with insert FF2 removed for offloading in that region. Inserts T2 and A were excluded from the removal trials as they exhibited very low magnitudes of pressures for both cases S and W. However, pressures under inserts T2 and A were still recorded for S (full) and W (full). Therefore, each participant was subjected to a total of 10 trials for each case, S and W. For each trial in case S, participants were directed to stand straight as they normally would for a duration of 5 s. The pressure-measuring insole computed the average zonal pressure (AZP) values for each of the 11 probed zones using the running average algorithm. For case W, the volunteers were asked to walk freely and normally for a duration of 20 s while wearing the test setup. During this period, the pressure-measuring insole recorded and displayed the maxima of pressures at each of the 11 probed zones. The modular insole was considered feasible if the pressure values at the truncated segment were extremely low. This translated to the plantar surface of the foot not touching the floor of the shoe, leading to efficient pressure offloading in the desired region. Figure 7 shows the participants wearing the test setup during the various trials.

Figure 7.
Volunteer wearing insole (inside shoe) and microcontroller using a Velcro strap during the qualitative and quantitative trials.
3. Results
3.1. QUEST 2.0 Score
The feasibility of the modular diabetic insole as a wearable intervention device was evaluated by checking the extent of comfort and other user-oriented parameters occurring during static and dynamic scenarios by means of the QUEST 2.0 questionnaire. For case Q1, a QUEST 2.0 score of 4.71 ± 0.17 was obtained. For case Q2, the QUEST 2.0 score was 4.69 ± 0.19. Therefore, the overall QUEST 2.0 score for the complete insole was 4.7 ± 0.18. Table 2 and Table 3 show the individual scores given by the participants for both cases Q1 and Q2, respectively.

Table 2.
QUEST 2.0 scores on the device’s subscale for case Q1 (standing).

Table 3.
QUEST 2.0 scores on the device’s subscale for case Q2 (walking).
The total QUEST 2.0 score for the performance of the insole was between four and five, which indicated very high user satisfaction. There was not much difference between the overall scores of Q1 and Q2. This indicated that even though there was some perceived drop in comfort in Q2 compared to Q1, it was not major, and that some participants preferred the offloaded case over case Q1. All participants confirmed that the used insole provided a high degree of comfort to the foot.
Certain points of feedback for the modular diabetic insole gained through trials Q1 and Q2 were noteworthy. All of the participants highly favoured the cushioning effect of the insole during walking, specifically at the forefoot and the ball of the foot (segments FF1-3 and H, respectively). This positive response validated that the use of circular voids in all the inserts tended to increase the perceived comfort of the insole. For Q2, truncated regions at FF1, FF2, FF3, H1, and H4 were completely unnoticeable by the participants, possibly due to ample support from the surrounding regions. The edges of the inserts surrounding the truncated region were also not noticeable and did not give rise to any discomfort. For inserts T1 and T2 removed in case Q2, the empty space was only felt if the participant voluntarily lowered the toes in the void, which was understandable. For truncated regions at MF1, MF2 and H, the voids were mildly noticeable due to their relatively larger surface area and higher concentration of pressures, respectively. However, voids in those regions were not deemed uncomfortable.
Voids generated by removing inserts T3, H2, and H3 were completely imperceptible owing to their small surface areas and locations. Region T3 generally provided extremely minor reaction pressures during walking or other movements during ambulation. The area of the foot in contact with this region was also very small (toes 3–5), which was also why this insert was excluded from the circular void design for simplification purposes. Segments H2 and H3 generally did not come in contact with the foot. However, their contribution in supporting the foot became apparent when insert H was removed. Although small in area, they had the crucial role of supporting the heel region in case insert H was removed, especially during the heel strike. This would not allow the ball of the foot to touch the floor of the shoe, in effect, offloading pressure from region H. All participants could easily use the insole due to its intuitive design and construction. Extracting and reattaching any insert in the mid-frame of the insole was successfully carried out by all participants. Inserting the assembled insole in the pouch was also easily performed by inverting the empty pouch before placing it inside. The pouch was stitched to be ambidextrous, making it even simpler to use. The participants also placed and removed the insole from the footwear without any hassle.
These results indicated that the modular diabetic insole was delicate on the feet and could be prescribed as an assistive intervention device for diabetic foot ulcer care. The insole could also be used as a general-purpose comfort insole and in cases of nondiabetic foot ulceration.
3.2. Extent and Feasibility of Pressure Offloading
The pressures were recorded under 11 regions of the modular insole with the help of the pressure-measuring insole for cases S and W, as mentioned previously. Pressure values from respective trials for all 10 participants were averaged, called the average zonal pressure (AZP).
3.2.1. Pressure Offloading during Standing
Table 4 below shows the AZP values for the group of nine offloaded cases during the standing condition.

Table 4.
Average zonal pressure values for the cohort for the 9 offloaded cases (standing).
Figure 8 shows the pressure values in the 11 probed regions of the modular diabetic insole for case S. Corresponding AZP values (kPa) across all 10 participants were averaged and are presented in the figure along with their standard deviation (kPa). Figure 8A shows the AZP values for S (full). On the other hand, Figure 8B only shows the offloaded AZP values, which occurred when the corresponding insert was removed while all other inserts were attached.
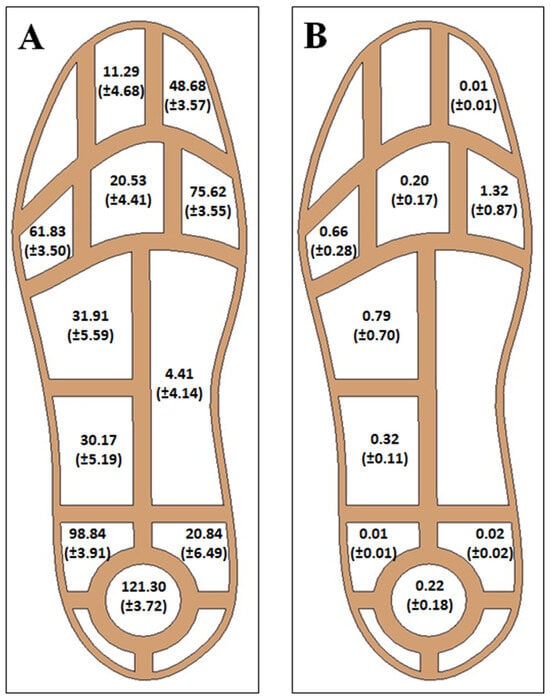
Figure 8.
Average zonal pressure (AZP) values for case S (mean ± S.D.) in kPa; (A) AZP values in 11 regions with all inserts attached in the mid-frame for S (Full); (B) offloaded AZP values in the nine regions with the corresponding inserts removed.
For trial S (full) (Figure 8A), the maximum AZP value occurred in region H with a magnitude of 121.30 ± 3.72 kPa, whereas the minimum magnitude of the AZP manifested in region A with a magnitude of 4.41 ± 4.14 kPa. Since the magnitude of the AZP at inserts T2 and A were very low, contributing only about 2.15% and 0.84% of the total pressure recorded, respectively, trials S (T2) and S (A) were not considered. In the offloaded case, as shown in Figure 8B, the percentage decrease in pressure ranged from 98.25% to 99.99% in segments FF1 and H1, respectively. The maximum pressure in Figure 8B occurred in segment FF1 with an AZP value of 1.32 ± 0.87 kPa. Since AZP values in all other regions were less than that in FF1, it was validated that the plantar surface of the foot did not come into contact with the floor of the shoe during standing, in effect, offloading all the pressure from the individual segmented regions.
3.2.2. Pressure Off-loading during Walking
Table 5 below shows the AZP values for the nine offloaded cases during walking.

Table 5.
Average zonal pressure values for the cohort for the 9 offloaded cases (walking).
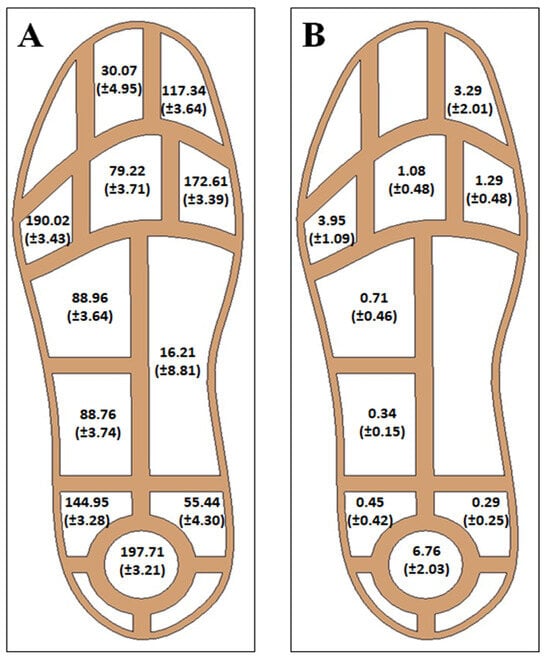
Figure 9.
Average zonal pressure (AZP) values for case W (mean ± S.D.) in kPa; (A) AZP values in 11 regions with all inserts attached in the mid-frame for W (full); (B) offloaded AZP values in the 9 regions with the corresponding inserts removed.
For trial W (full) as shown in Figure 9A, the maximum AZP value was observed in region H with a magnitude of 197.71 ± 3.21 kPa, whereas the smallest AZP value was observed in region A with a magnitude of 16.21 ± 8.81 kPa. Since the magnitude of the AZP at inserts T2 and A were very low, contributing only about 2.55% and 1.37% of the total pressure recorded, respectively, they were not considered for removal in the consequent pressure offloading trials.
For the offloaded cases as shown in Figure 9B, the percentage decrease in pressure ranged from 96.58% to 99.69% in segments H and H1, respectively. The maximum pressure in Figure 9B occurred in segment H with an AZP value of 6.76 ± 2.03 kPa. This suggested that for W (H), some contact was prevalent between the ball of the foot and the floor of the shoe during heel strike. Moreover, regions T1 and FF3 showed the next highest-pressure regions with magnitudes of 3.29 ± 2.01 kPa and 3.95 ± 1.09 kPa, respectively. Although minor in magnitude, there was evidence of a similar contact in segments FF3 and T1, mostly during the foot-off phase of the gait cycle. It was understandable that such contact would occur at T1 due to the dexterity of metatarsal joints during walking. Considering the observed results and feedback of the participants, the modular insole was still able to provide sufficient pressure offloading in all nine regions (96.58–99.69%).
A few limitations of the modular diabetic insole emerged during the study. As supported by the results for case W (H), there was evidence that the heel, at the ball of the foot, was majorly in contact with the floor of the shoe, most probably during the heel strike phase of the gait. This effect could be mitigated by reducing the radius of the silicone insert at H along with a subsequent increase in the areas of inserts H1–4. Another limitation was that a small percentage of shoes were not able to accommodate the insole due to its relatively larger thickness (6 mm) as compared to prefabricated general insoles (~1–2 mm). More data would be required to optimize the thicknesses in the different segmented regions of the insole to enable a better generalized fit. Lastly, the modular diabetic insole should be prescribed for longer trial periods to assess all nuances in comfort and performance.
4. Conclusions
In conclusion, the developed novel modular insole was able to effectively offload plantar pressure, which would be beneficial for individuals with diabetic ulcers and also to prevent ulceration progression. The pressure measurement device, which was fabricated to map the real-time pressure readings during standing and walking, successfully differentiated between the plantar pressure observed in the standing and walking participants, respectively. The quantitative and qualitative assessment showed the effectiveness of the insole in offloading the peak plantar pressure region or tentative ulceration progression region. The recorded values of average zonal pressure at different locations across the different plantar regions during standing and walking conditions confirmed a significant offloading of peak pressure ranging from ~96–99%. The methodology and findings reported in this work would be indispensable for providing guidelines and strategies to medical practitioners and researchers to minimize ulceration progression. Also, it would be beneficial for diabetic patients for a timely analysis of pressure zones of their plantar fascia and possible ulceration or reoccurrence.
Author Contributions
D.B.: methodology, software, formal analysis, investigation, validation, writing—original draft, and writing—review and editing; G.S.: formal analysis, data curation, investigation, and writing—review and editing; S.G.: methodology, data curation, investigation, and formal analysis; A.C.: conceptualization, formal analysis, supervision, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Ethical Committee of Indian Institute of Technology, Delhi (IIT-Delhi).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to them being large datasets; however, data are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hingorani, A.; Lamuraglia, G.M.; Henke, P.; Meissner, M.H.; Loretz, L.; Zinszer, K.M.; Driver, V.R.; Frykberg, R.; Carman, T.L.; Marston, W.; et al. The Management of Diabetic Foot: A Clinical Practice Guideline by the Society for Vascular Surgery in Collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J. Vasc. Surg. 2016, 63, 3S–21S. [Google Scholar] [CrossRef]
- Tesfaye, S.; Stevens, L.K.; Stephenson, J.M.; Fuller, J.H.; Plater, M.; Ionescu-Tirgoviste, C.; Nuber, A.; Pozza, G.; Ward, J.D. Prevalence of Diabetic Peripheral Neuropathy and Its Relation to Glycaemic Control and Potential Risk Factors: The EURODIAB IDDM Complications Study. Diabetologia 1996, 39, 1377–1384. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Ashe, H.A.; Parnell, L.N.; Fernando, D.J.S.; Tsigos, C.; Young, R.J.; Ward, J.D.; Boulton, A.J.M. The Prevalence of Foot Ulceration and Its Correlates in Type 2 Diabetic Patients: A Population-Based Study. Diabet. Med. 1994, 11, 480–484. [Google Scholar] [CrossRef] [PubMed]
- Boulton, A.J.M. The Diabetic Foot: From Art to Science. The 18th Camillo Golgi Lecture. Diabetologia 2004, 47, 1343–1353. [Google Scholar] [CrossRef]
- Prompers, L.; Huijberts, M.; Apelqvist, J.; Jude, E.; Piaggesi, A.; Bakker, K.; Edmonds, M.; Holstein, P.; Jirkovska, A.; Mauricio, D.; et al. High Prevalence of Ischaemia, Infection and Serious Comorbidity in Patients with Diabetic Foot Disease in Europe. Baseline Results from the Eurodiale Study. Diabetologia 2007, 50, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Boulton, A.J.M. The Diabetic Foot—An Update. Foot Ankle Surg. 2008, 14, 120–124. [Google Scholar] [CrossRef]
- Abbott, C.A.; Carrington, A.L.; Ashe, H.; Bath, S.; Every, L.C.; Griffiths, J.; Hann, A.W.; Hussein, A.; Jackson, N.; Johnson, K.E.; et al. The North-West Diabetes Foot Care Study: Incidence of, and Risk Factors for, New Diabetic Foot Ulceration in a Community-Based Patient Cohort. Diabet. Med. 2002, 19, 377–384. [Google Scholar] [CrossRef]
- Lauterbach, S.; Kostev, K.; Kohlmann, T. Prevalence of Diabetic Foot Syndrome and Its Risk Factors in the UK. J. Wound Care 2013, 19, 333–337. [Google Scholar] [CrossRef]
- Ulbrecht, J.S.; Cavanagh, P.R.; Caputo, G.M. Foot Problems in Diabetes: An Overview. Clin. Infect. Dis. 2004, 39 (Suppl. S2), S73–S82. [Google Scholar] [CrossRef]
- Chen, W.M.; Lee, T.; Lee, P.V.S.; Lee, J.W.; Lee, S.J. Effects of Internal Stress Concentrations in Plantar Soft-Tissue—A Preliminary Three-Dimensional Finite Element Analysis. Med. Eng. Phys. 2010, 32, 324–331. [Google Scholar] [CrossRef]
- Chantelau, E.; Haage, P. An Audit of Cushioned Diabetic Footwear: Relation to Patient Compliance. Diabet. Med. 1994, 11, 114–116. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Harding, K.G. Diabetic Foot Ulcers. Lancet 2003, 361, 1545–1551. [Google Scholar] [CrossRef] [PubMed]
- Janisse, D.; Janisse, E. Pedorthic Management of the Diabetic Foot. Prosthet. Orthot. Int. 2015, 39, 40–47. [Google Scholar] [CrossRef]
- Hawke, F.; Burns, J.; Radford, J.A.; du Toit, V. Custom-made Foot Orthoses for the Treatment of Foot Pain. Cochrane Database Syst. Rev. 2008, 16, CD006801. [Google Scholar] [CrossRef] [PubMed]
- Trotter, L.C.; Pierrynowski, M.R. Ability of Foot Care Professionals to Cast Feet Using the Nonweightbearing Plaster and the Gait-Referenced Foam Casting Techniques. J. Am. Podiatr. Med. Assoc. 2008, 98, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Pallari, J.H.P.; Dalgarno, K.W.; Munguia, J.; Muraru, L.; Peeraer, L.; Telfer, S.; Woodburn, J. Design and additive fabrication of foot and ankle-foot orhtoses. In Proceedings of the 2010 International Solid Freeform Fabrication Symposium, Austin, TX, USA, 9–11 August 2010. [Google Scholar]
- Chhikara, K.; Gupta, S.; Chanda, A. Development of a Novel Foot Orthosis for Plantar Pain Reduction. Mater. Today Proc. 2022, 62, 3532–3537. [Google Scholar] [CrossRef]
- Bus, S.A.; Armstrong, D.G.; van Deursen, R.W.; Lewis, J.E.A.; Caravaggi, C.F.; Cavanagh, P.R. IWGDF Guidance on Footwear and Offloading Interventions to Prevent and Heal Foot Ulcers in Patients with Diabetes. Diabetes Metab. Res. Rev. 2016, 32, 25–36. [Google Scholar] [CrossRef]
- Gupta, S.; Singh, G.; Chanda, A. Prediction of Diabetic Foot Ulcer Progression: A Computational Study. Biomed. Phys. Eng. Express 2021, 7, 065020. [Google Scholar] [CrossRef]
- Dunn, J.E.; Link, C.L.; Felson, D.T.; Crincoli, M.G.; Keysor, J.J.; McKinlay, J.B. Prevalence of Foot and Ankle Conditions in a Multiethnic Community Sample of Older Adults. Am. J. Epidemiol. 2004, 159, 491–498. [Google Scholar] [CrossRef]
- Garrow, A.P.; Silman, A.J.; Macfarlane, G.J. The Cheshire Foot Pain and Disability Survey: A Population Survey Assessing Prevalence and Associations. Pain 2004, 110, 378–384. [Google Scholar] [CrossRef]
- Hendry, G.J.; Fenocchi, L.; Woodburn, J.; Steultjens, M. Foot Pain and Foot Health in an Educated Population of Adults: Results from the Glasgow Caledonian University Alumni Foot Health Survey. J. Foot Ankle Res. 2018, 11, 48. [Google Scholar] [CrossRef]
- Sutkowska, E.; Sutkowski, K.; Sokołowski, M.; Franek, E.; Dragan, S. Distribution of the Highest Plantar Pressure Regions in Patients with Diabetes and Its Association with Peripheral Neuropathy, Gender, Age, and BMI: One Centre Study. J. Diabetes Res. 2019, 2019, 7395769. [Google Scholar] [CrossRef]
- Caselli, A.; Pham, H.; Giurini, J.M.; Armstrong, D.G.; Veves, A. The Forefoot-to-Rearfoot Plantar Pressure Ratio Is Increased in Severe Diabetic Neuropathy and Can Predict Foot Ulceration. Diabetes Care 2002, 25, 1066–1071. [Google Scholar] [CrossRef]
- De Cock, A.; Vanrenterghem, J.; Willems, T.; Witvrouw, E.; De Clercq, D. The Trajectory of the Centre of Pressure during Barefoot Running as a Potential Measure for Foot Function. Gait Posture 2008, 27, 669–675. [Google Scholar] [CrossRef]
- Taborri, J.; Rossi, S.; Palermo, E.; Patanè, F.; Cappa, P. A Novel HMM Distributed Classifier for the Detection of Gait Phases by Means of a Wearable Inertial Sensor Network. Sensors 2014, 14, 16212–16234. [Google Scholar] [CrossRef] [PubMed]
- Di Rosa, M.; Hausdorff, J.M.; Stara, V.; Rossi, L.; Glynn, L.; Casey, M.; Burkard, S.; Cherubini, A. Concurrent Validation of an Index to Estimate Fall Risk in Community Dwelling Seniors through a Wireless Sensor Insole System: A Pilot Study. Gait Posture 2017, 55, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Shu, L.; Hua, T.; Wang, Y.; Li, Q.; Feng, D.D.; Tao, X. In-Shoe Plantar Pressure Measurement and Analysis System Based on Fabric Pressure Sensing Array. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 767–775. [Google Scholar] [CrossRef]
- Cui, T.; Yang, L.; Han, X.; Xu, J.; Yang, Y.; Ren, T. A Low-Cost, Portable, and Wireless In-Shoe System Based on a Flexible Porous Graphene Pressure Sensor. Materials 2021, 14, 6475. [Google Scholar] [CrossRef] [PubMed]
- Pappas, I.P.I.; Popovic, M.R.; Keller, T.; Dietz, V.; Morari, M. A Reliable Gait Phase Detection System. IEEE Trans. Neural Syst. Rehabil. Eng. 2001, 9, 113–125. [Google Scholar] [CrossRef]
- Tee, K.S.; Javahar, Y.S.H.; Saim, H.; Zakaria, W.N.W.; Khialdin, S.B.M.; Isa, H.; Awad, M.I.; Soon, C.F. A Portable Insole Pressure Mapping System. TELKOMNIKA (Telecommun. Comput. Electron. Control) 2017, 15, 1493–1500. [Google Scholar] [CrossRef]
- Hellstrand Tang, U.; Zügner, R.; Lisovskaja, V.; Karlsson, J.; Hagberg, K.; Tranberg, R. Comparison of Plantar Pressure in Three Types of Insole given to Patients with Diabetes at Risk of Developing Foot Ulcers—A Two-Year, Randomized Trial. J. Clin. Transl. Endocrinol. 2014, 1, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Collings, R.; Freeman, J.; Latour, J.M.; Paton, J. Footwear and Insole Design Features for Offloading the Diabetic at Risk Foot—A Systematic Review and Meta-Analyses. Endocrinol. Diabetes Metab. 2021, 4, e00132. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.Q.; Li, P.L.; Yick, K.L.; Li, N.W.; Jiao, J. Effects of Contoured Insoles with Different Materials on Plantar Pressure Offloading in Diabetic Elderly during Gait. Sci. Rep. 2022, 12, 1–10. [Google Scholar] [CrossRef]
- Mandolini, M.; Brunzini, A.; Germani, M. A Collaborative Web-Based Platform for the Prescription of Custom-Made Insoles. Adv. Eng. Inform. 2017, 33, 360–373. [Google Scholar] [CrossRef]
- Paton, J.S.; Stenhouse, E.A.; Bruce, G.; Zahra, D.; Jones, R.B. A Comparison of Customised and Prefabricated Insoles to Reduce Risk Factors for Neuropathic Diabetic Foot Ulceration: A Participant-Blinded Randomised Controlled Trial. J. Foot Ankle Res. 2012, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Lin, J.; Xu, X.; Ma, Z.; Tang, L.; Sun, C.; Li, D.; Liu, C.; Zhong, Y.; Wang, L. Design and 3D Printing of Adjustable Modulus Porous Structures for Customized Diabetic Foot Insoles. Int. J. Lightweigh Mater. Manuf. 2019, 2, 57–63. [Google Scholar] [CrossRef]
- Anderson, J.; Williams, A.E.; Nester, C. Development and Evaluation of a Dual Density Insole for People Standing for Long Periods of Time at Work. J. Foot Ankle Res. 2020, 13, 1–13. [Google Scholar] [CrossRef]
- Demers, L.; Weiss-Lambrou, R.; Demers, L.; Ska, B. Development of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST). Assist. Technol. 1996, 8, 3–13. [Google Scholar] [CrossRef]
- Ledoux, W.R.; Shofer, J.B.; Cowley, M.S.; Ahroni, J.H.; Cohen, V.; Boyko, E.J. Diabetic Foot Ulcer Incidence in Relation to Plantar Pressure Magnitude and Measurement Location. J. Diabetes Complicat. 2013, 27, 621–626. [Google Scholar] [CrossRef]
- ISO 9407:2019; Footwear Sizing—Mondopoint System of Sizing and Marking. International Organization for Standardization: Geneva, Switzerland, 2019.
- Singh, G.; Gupta, S.; Chanda, A. Biomechanical Modelling of Diabetic Foot Ulcers: A Computational Study. J. Biomech. 2021, 127, 110699. [Google Scholar] [CrossRef]
- Li, N.; Yang, D.; Jiang, L.; Liu, H.; Cai, H. Combined Use of FSR Sensor Array and SVM Classifier for Finger Motion Recognition Based on Pressure Distribution Map. J. Bionic Eng. 2012, 9, 39–47. [Google Scholar] [CrossRef]
- Manna, S.K.; Hannan Bin Azhar, M.A.; Greace, A. Optimal Locations and Computational Frameworks of FSR and IMU Sensors for Measuring Gait Abnormalities. Heliyon 2023, 9, e15210. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Ballard, D.H. Feasibility of Customized Pillboxes to Enhance Medication Adherence: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2022, 103, 2288–2295. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, K.E.C.; Gois Júnior, M.B.; Sá, K.N. Translation and Validation of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) into Portuguese. Rev. Bras. Reumatol. Engl. Ed. 2014, 54, 260–267. [Google Scholar] [CrossRef]
- Chhikara, K.; Gupta, S.; Bose, D.; Kataria, C.; Chanda, A. Development and Trial of a Multipurpose Customized Orthosis for Activities of Daily Living in Patients with Spinal Cord Injury. Prosthesis 2023, 5, 467–479. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).