1. Introduction
Population demographics show that overall edentulism is decreasing in the aging population due to improved prophylaxis and care, while the proportion of partially edentulous individuals is increasing as a result of longer life expectancy, increasing population aging, and the fact that more teeth are retained at older age due to improved oral health care and prevention [
1,
2,
3,
4,
5].
Posterior molars are more likely to be lost than anterior teeth [
1,
5], resulting in remaining anterior dentition with bilateral edentulous posterior areas typically classified as Kennedy Class I [
6]. The prosthetic gold standard for the treatment of cases with bilateral free-end situations are removable partial dentures (RPDs) with clasps, not at least due to the fact that fixed restorations with dental implants are often considered too costly, time-consuming, and invasive, particularly when additional augmentative measures are required [
4]. In contrast, RPD treatment is minimally invasive, cost-effective, and patients can be provided with dentures in a timely manner [
2,
3,
4].
RPDs with clasps in a Kennedy Class I situation are often associated with technical or biological complications due to the lack of posterior support [
7] and frequent requirement of adjustments such as relining or fracture repair [
8]. For instance, in a prospective study over 2 years, clasp-supported RPDs in Kennedy Class I situations showed partial non-occlusion in 35% of prostheses at 6 months, which increased to over 50% at 2 years in function [
9]. In this context, various groups of authors reported that the reduction in residual ridge height is closely related to edentulism and denture use [
10], and that non-denture wearers tend to have more residual edentulous ridge tissue compared to denture wearers. [
11]. In a retrospective study of Kennedy Class II patients (unilateral free-end) using cone-beam computed tomography (CBCT) analyses, vertical and horizontal alveolar bone resorption in the edentulous sites was higher in RPD wearers than in patients without RPDs [
12]. Thus, the alveolar ridge in the saddle region appears to be more susceptible to resorption due to the pressure load exerted by the prosthetic saddle. It can therefore be expected that improperly fitted RPDs will transfer even more unfavorable forces to the alveolar ridge, which may lead to further progression of resorption of the residual ridge [
4].
A retrospective study reported that approximately 40% of partial dentures are no longer in use within 5 years [
13] because of factors such as socio-demographics, pain, and esthetics [
2]. Several reviews relate this to incorrect or inaccurate planning and execution in the fabrication of RPDs [
2,
4]. Considering that the number of partially edentulous patients will increase and that not every patient will receive fixed implant restorations for financial reasons or due to other factors such as a loss of several teeth and/or severe soft and hard tissue loss, it is necessary to give more importance to the topic of RPD [
2,
4]. Therefore, to optimize general RPD and minimize potentially damaging forces on abutment teeth and supporting tissues, at a minimum, the improved planning of denture design in conjunction with accurate assessment of tooth status, positions, and preparation, as well as patient education, consistent follow-up, and further development of new fabrication technologies and materials are required [
2].
Provided that the RPD saddles are extended to rest at the retromolar pads, alveolar ridge resorption due to non-physiological loading is deemed to be minimized [
14] Additional implants in the posterior region of RPDs, also known as implant-assisted removable partial dentures (IARPDs), have been described to improve function and stability [
5,
15]. According to a recent systematic review, conversion from conventional RPDs to IARPDs by subsequent implant placement and integration into the prosthesis, lead to an improvement in overall oral function (mastication, pronunciation, and esthetics) in partially edentulous Class I mandibular Kennedy patients. There was also a significant improvement in patient-reported outcome measures (PROMs), particularly in the field of physical pain and psychological impairment, and masticatory performance improved significantly in terms of maximum bite force, active occlusal contact area and mandibular jaw movement [
16]. Another recent systematic review also reported that IARPDs showed favorable clinical outcomes and significantly higher patient satisfaction than before treatment and compared to conventional RPDs [
17]. According to this review, stud attachments were most commonly used in IARPDs, and the different attachment systems did not affect implant survival or patient satisfaction [
17]. However, both reviews addressed a lack of high-quality long-term RCT studies and a need for an IARPD treatment protocol based on well-structured, long-term clinical trials, in which implant location, type, and size, as well as type of attachment, metal framework design, and surgical and loading protocols are determined [
16,
17].
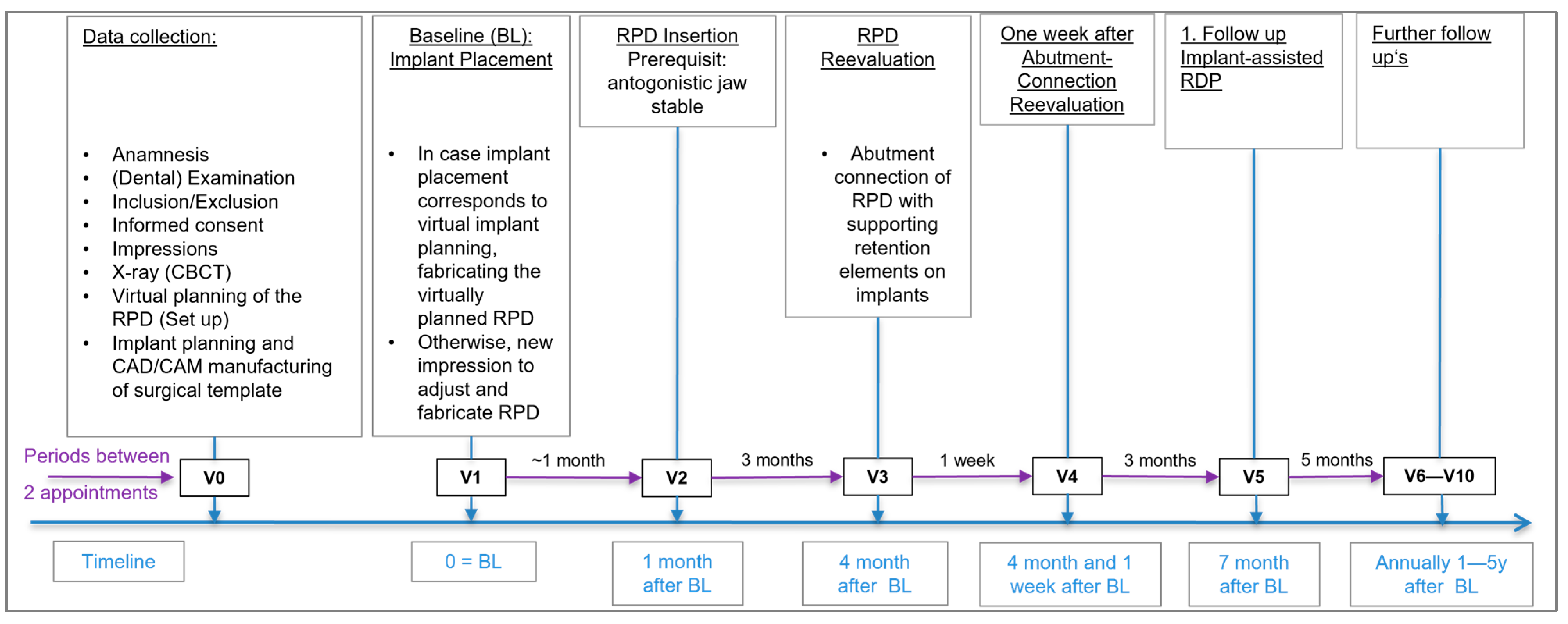
In light of these findings, a multicenter RCT was designed to evaluate the effect of additional implants in Kennedy Class I patients in terms of PROMs and cost–benefit analyses comparing maintenance care costs (initially and during long-term follow-up) for the treatment of partially edentulous patients with two additional posterior implants using two types of attachments that either support or retain RPDs. The case report presented here is part of this ongoing multicenter study and is intended to illustrate the clinical digital workflow and technical protocol for restoring a Kennedy Class I situation with a conventional RPD taking into account direct or later implant placement using ultra-short implants for additional support or retention in the posterior region.
2. Detailed Case Description
A 52-year-old male patient introduced himself to the University Center for Dental Medicine Basel (UZB) with the request for a prosthetic rehabilitation. He was in general good health, had never smoked, and related previous tooth loss to caries lesions. Initial periodontal and radiographic screening revealed healthy conditions of the remaining dentition with severe tooth wear and a collapsed bite (
Figure 1).
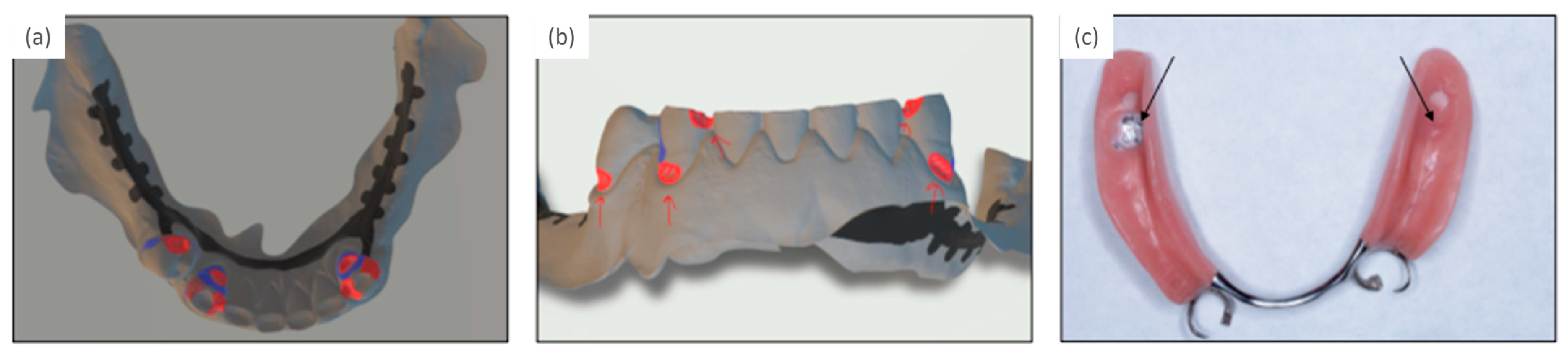
Due to the complex intermaxillary situation requiring an increase in the vertical dimension of occlusion (VDO), an overdenture prosthesis with anterior post copings and a clasp at the intact left premolar was planned in the maxilla, while a clasp-retained RPD was indicated in the mandible. The intact anterior dentition in the mandible determined the occlusal plane, and the increase in VDO was planned in the maxilla, which was restored first providing a diagnostic set-up in the mandible. For the RDP in the mandible, intraoral scans with and without the set-up were analyzed with a software program (3Shape Dental Manager, Copenhagen, Denmark), which enabled an exact planning of the prosthesis path of insertion and the position of the retentive clasp undercuts at the abutment teeth. This digital analysis replaced the traditional way with mounting casts in a surveyor to determine the path of insertion and undercuts at the abutment teeth (
Figure 2a,b). Required occlusal rest cavities were prepared and a new intraoral scan was taken, which in turn was incorporated into the further planning. The RPD was then designed in the planning software and configured with 2 clasps at the most distal abutment teeth and an extension of the bilateral saddles to ensure support on the retromolar pads. In addition, the housings in the metal framework were scheduled for later implant healing abutments or retention elements in the area of the second molars (
Figure 2c).
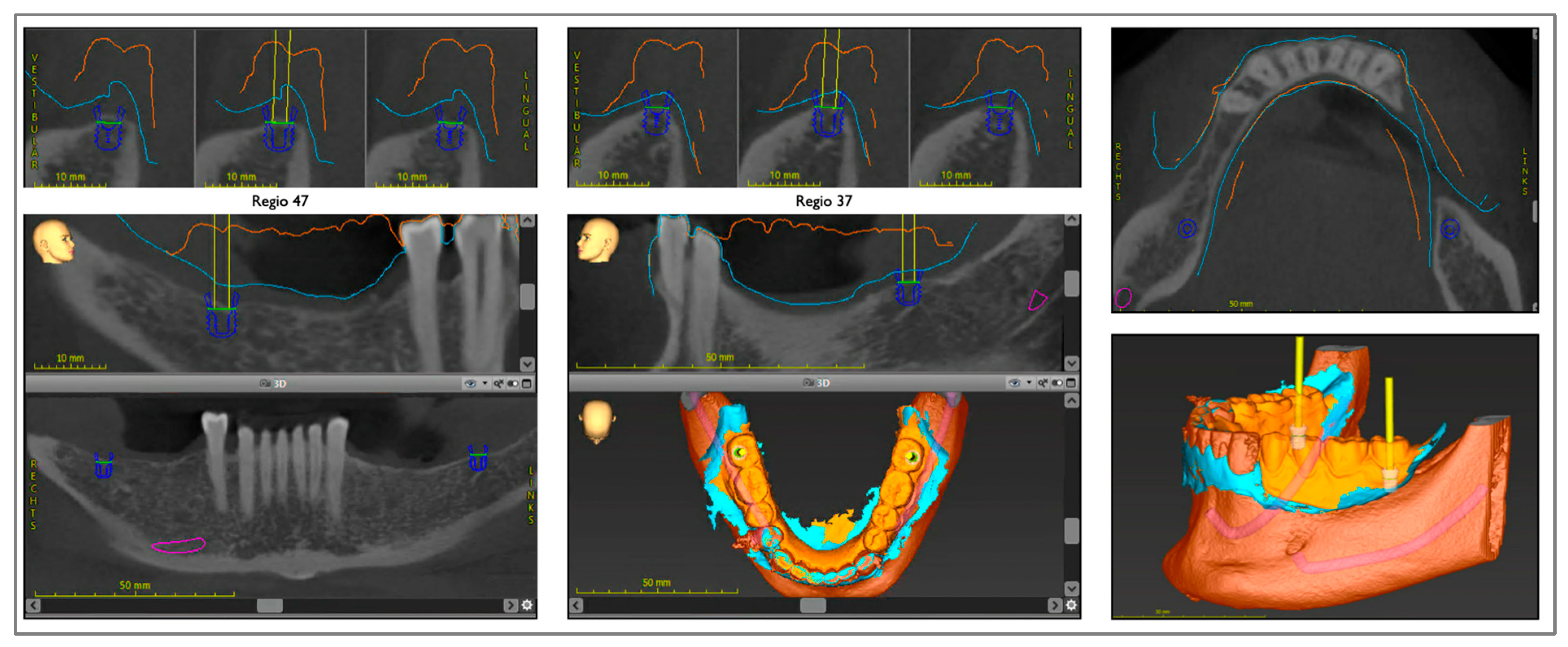
At the same time, two implants were planned using the coDiagnostiX
® software (Version 10.7.0, Straumann AG, Basel, Switzerland). Therefore, the intraoral scan of the analog tooth set-up (
Figure 3) or a virtual set-up of the previously planned denture design were imported for orientation. This scan of the set-up and the intraoral scan of the mandible without set-up were overlaid with the CBCT data (
Figure 3). By switching between the prosthetic planning software (3Shape Dental Manager, version 2.21.2.2 (2021-1), Copenhagen, Denmark) and the implant planning software (coDiagnostiX
®, Straumann AG, Basel, Switzerland), the implant axes and positions were aligned according to the path of insertion of the RPD, and the housings in the virtual RPD were planned accordingly. Subsequently, the surgical guide for navigated implant placement was fabricated by 3D printing (Rapidshape P-Series, Straumann AG; Basel, Switzerland).
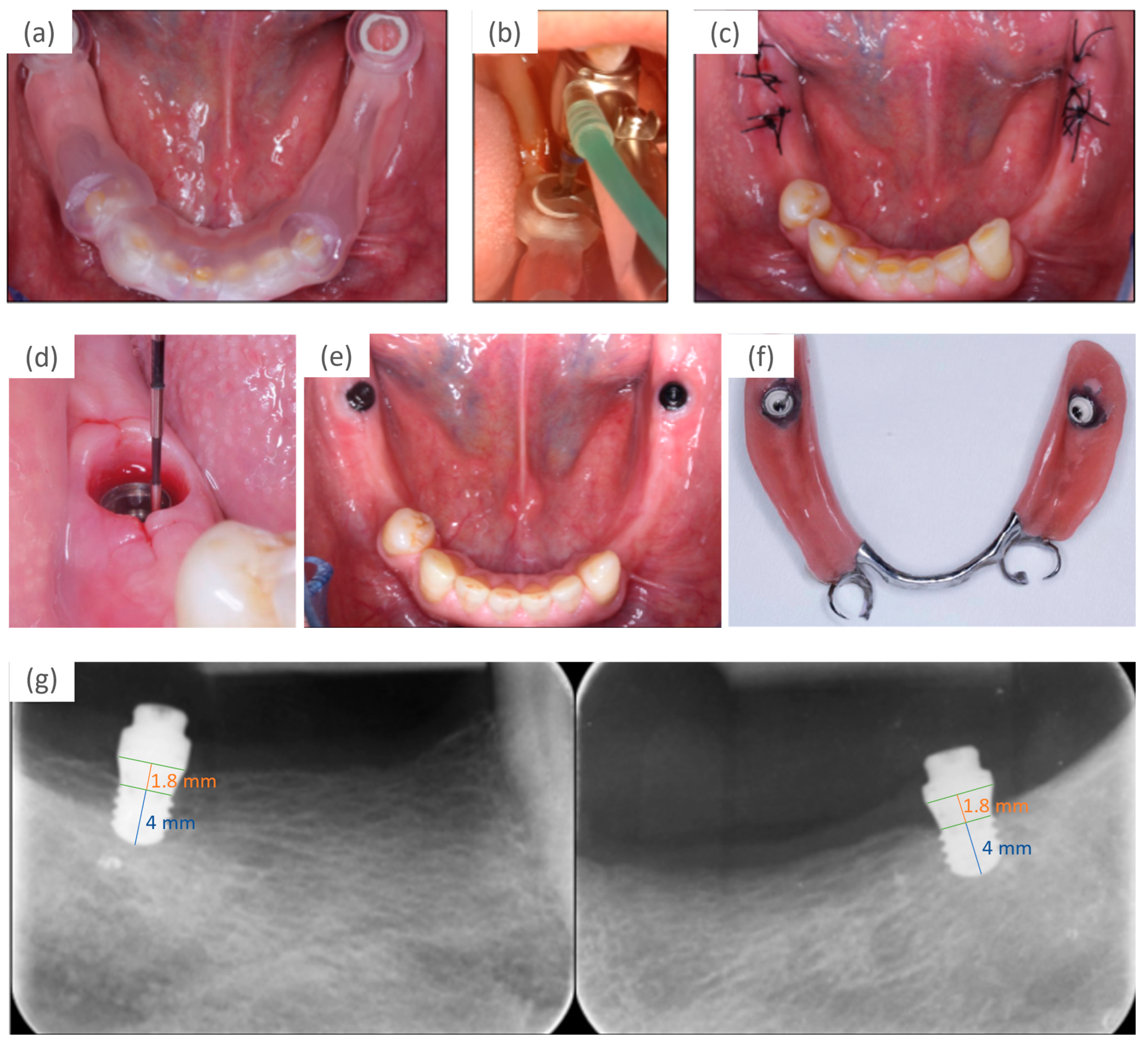
Implant placement was performed fully guided with the printed surgical guide (
Figure 4a). Two ultra-short tissue-level implants with a diameter of 4.1 mm and 4 mm intraosseous length (Straumann AG, Basel) were inserted in the posterior molar region (
Figure 4b) and left for submerged healing; in the case of an existing interims prosthesis, the saddles have to be relieved in the wound area (
Figure 4c).
When the fully navigated implant placement corresponded to the virtual implant planning, the virtually planned prosthesis was fabricated using a chromium-cobalt restoration by a milling process in a high precision milling machine (PFM 4024-5D, Primacon, Peissenberg, Germany) completed with denture teeth and the prostheses saddle. The RPD was incorporated after completion of wound healing approximately 3 weeks after surgery. In the event of significant manual corrections of the implant position, a new intraoral scan or an analog impression has to be taken to visualize the approximate implant position. The virtual RPD planning can be adjusted accordingly, and the prosthesis fabricated.
Following a 3-month submerged implant healing period, abutment connection was conducted, and retention elements were inserted (Novaloc, Straumann;
Figure 4d–g). The height of the elements were selected taking into account the height of the mucosal peri-implant tissues and the vertical space (
Figure 4d). Matrices were fixed in the RPD using self-curing methylmethacrylate resin (Unifast Trad, GC Europe AG, Luzern, Switzerland) (
Figure 4f). The patient’s perception of the RPD before and after connection to the implant was assessed with questionnaires on function, stability, and satisfaction [
18]; the OHIP-G14 and masticatory performance with a color mixing ability test [
19]. Based on these, the patient indicated a beneficial impact on his perception and function after prosthetic rehabilitation with implant retention.
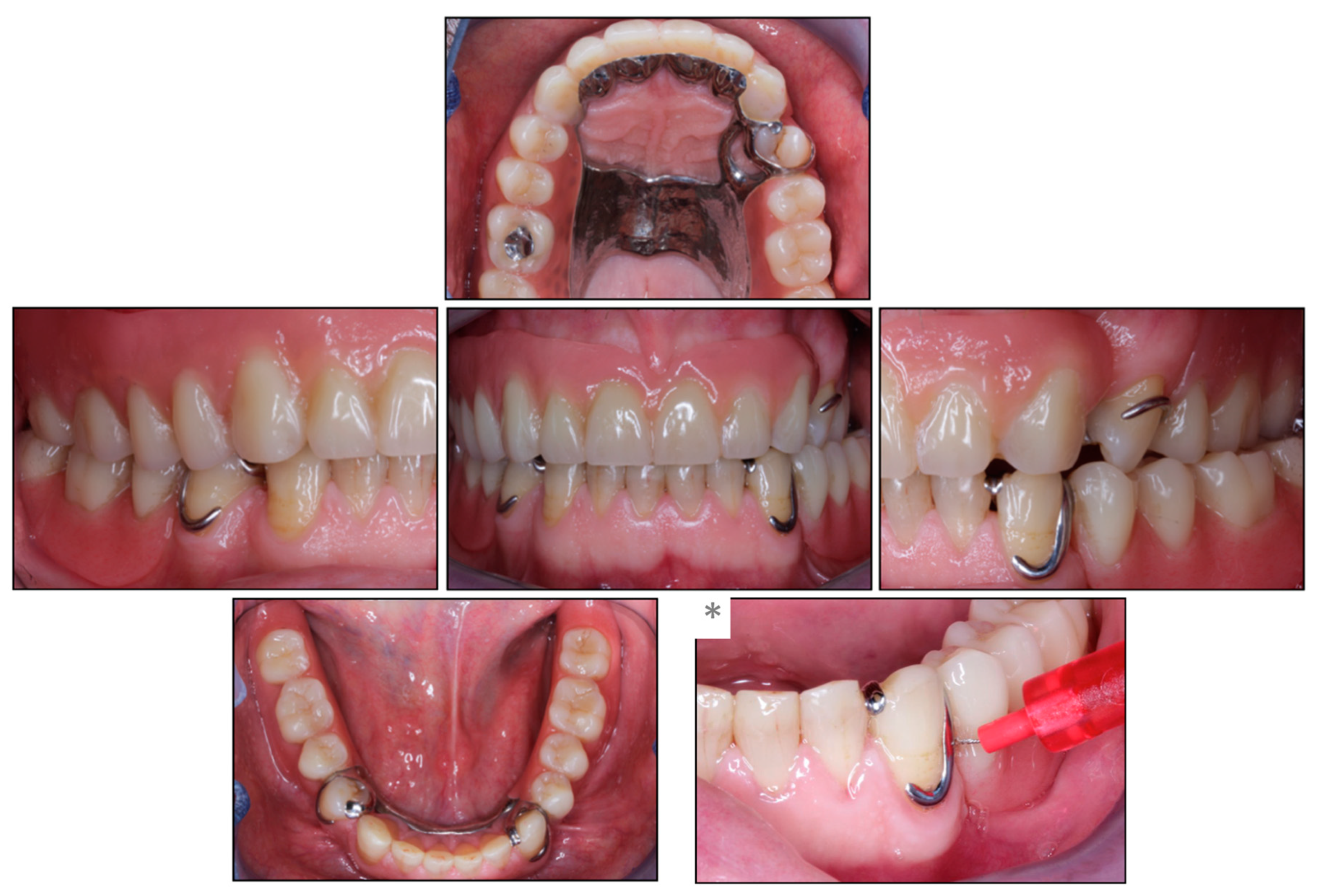
Figure 5 shows the patient’s completed prosthetic restoration in both jaws (
Figure 5) and
Figure 6 provides an overview of the patient’s clinical treatment schedule (
Figure 6).
3. Discussion
The presented case report described a partially edentulous Class I Kennedy patient restored with an RPD and a fully guided surgical protocol using ultra-short implants in the posterior regions.
The advanced atrophy of the mandibular alveolar crest can be challenging in clinical practice due to lack of bone and proximity to anatomically vulnerable structures such as the nervus alveolaris inferior in the mid-posterior part of the mandible or the sinus in the posterior part of the maxilla. The use of ultrashort implants simplifies implant placement because invasive bone augmentation procedure is usually not required, and burden and costs are reduced, while still providing the benefit of support or retention of the RPD. Furthermore, in the case of technical or biological complications, the ultra-short implant design simplifies implant removal if required, keeping the intervention minimally invasive and enable a back-off strategy at any point of therapy [
20,
21]. The tissue-level implant design initially intended for an unsubmerged healing protocol seems to be advantageous due to the ease of maintenance, particularly in the posterior regions, which are difficult to access for personal oral hygiene [
22]. The use of ultra-short 4 mm implants are primarily considered in severely reduced alveolar ridges. Certainly, the described concept of IARPD can also be implemented if according to implant planning longer implants are feasible without further bone augmentation.
The long-term performance of the ultra-short implants used in this study remains to be evaluated during follow-up. In a study using IARPDs in Kennedy Class I situations, in which 6-mm-long and 4.1-mm-wide implants were used together with longer and narrower implants, the mean marginal bone loss (MBL) after one year of function was reported 1.10+/−0.53 mm for the 6mm long implants [
23], which is critical for ultra-short implants. In this study, free-end saddles were retained on 4 implants with locators, of which the posterior ones measured 6 mm length [
23]. According to a finite element analysis study, implants in IARPDs are subjected to high stresses, which is why it was recommended to reduce stress by, among other things, using more than one implant to support a free end saddle [
24]. No data from clinical studies with IARPDs are available reporting about the retention elements applied in the current ongoing study. Using healing abutments for RPD support, their loosening has been frequently reported as a common technical complication, which can be easily remedied [
16]. The most important issue seems to be that the alveolar ridge remains more stable with the implant in situ. In case of implant loss, posterior ultra-short implants can be easily replaced at the same or an adjacent distal site. To enable implant replacement and avoiding subsequent prosthesis remake, an extended housing should be incorporated into the metal framework in the saddle area during initial IARPD fabrication. Even when the patient is against an IARPD treatment and prefers a simple RPD at the beginning, it still may be beneficial to incorporate a wide housing in the framework to enable implant placement at a later timepoint without weakening the prosthesis stability.
Treatment in the present case was performed according to the described protocol without any significant deviation, i.e., solely based on the intraoral scans, the virtual prosthesis and implant planning, with fully navigated implant insertion and subsequent prosthesis fabrication using a digitally milled chromium-cobalt restoration completed with denture teeth. The prosthesis could be inserted and subsequently “connected” with the retention elements selected intraorally according to the height of the healed peri-implant mucosal tissues and the available vertical space, and matrices inserted chairside.
Patient-centered outcomes were measured with the Oral Health Impact Profile (OHIP) and the assessment of chewing efficiency and evaluation of implant survival/success will be followed up over five years in function. As this study is still ongoing, the long-term results of all the included patients are to be awaited. Nonetheless, this specific case showed promising results in terms of patients’ perception of function and oral health (OHQoL-G14) comparing conventional RDPs to implant-supported RDPs with retentive components in posterior sites of Kennedy Class I or, as in other examined individuals in this study, with implant healing abutments for prosthesis support. Personal oral hygiene was easily conducted with and without the prostheses in place (
Figure 5,*) and the amount of maintenance care requirements were rated as low.