Early Change in Quality of Life in the Treatment of Anorexia Nervosa
Abstract
1. Introduction
1.1. Quality of Life
1.2. Early Change
1.3. Aims and Hypotheses
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedure
2.4. Measures
2.5. Data Analyses
3. Results
3.1. Correlations
3.2. Polynomial Regression
3.2.1. End-of-Treatment BMI and PHRQoL
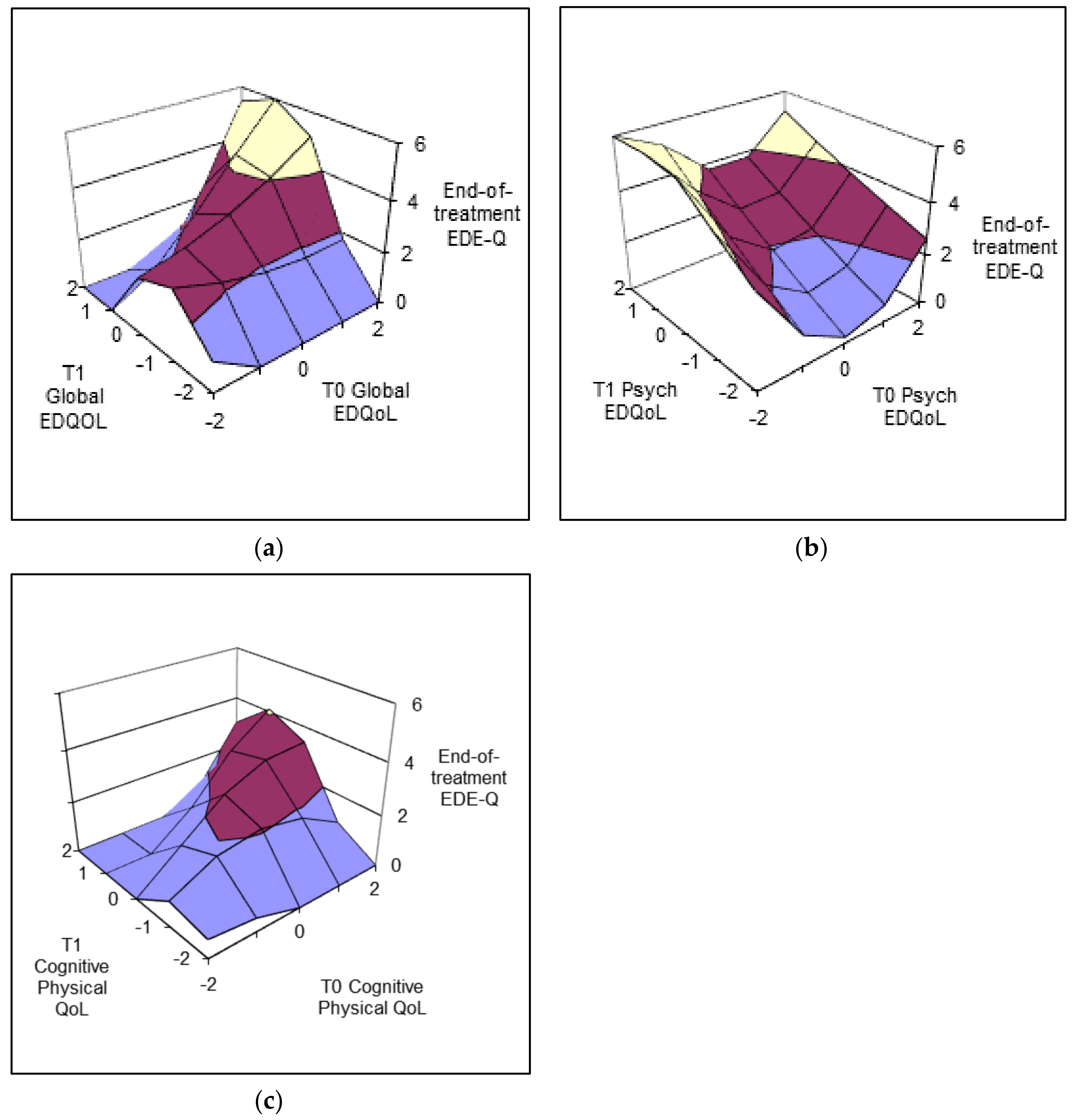
3.2.2. End-of-Treatment EDE-Q—Psychopathology
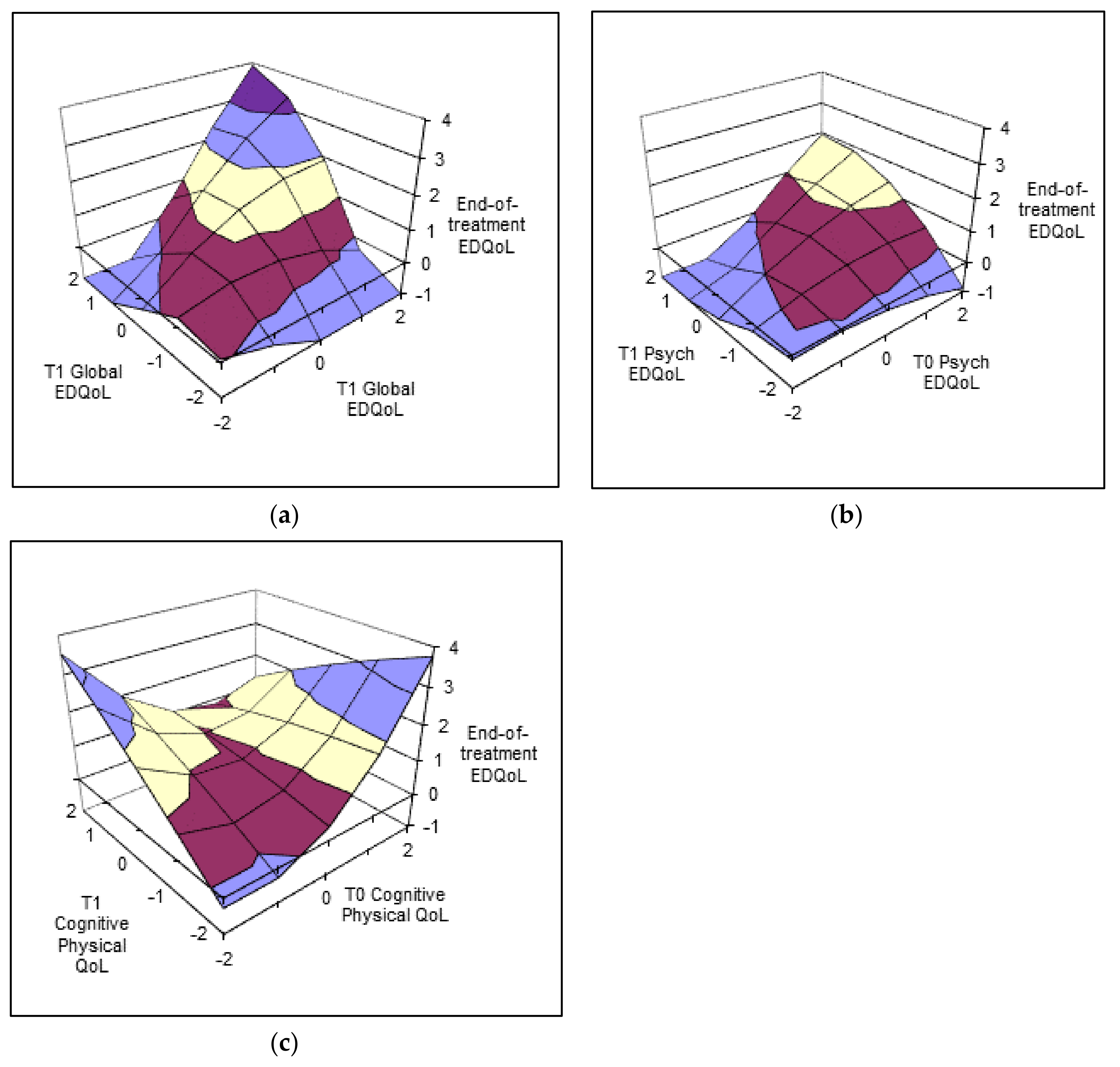
3.2.3. End-of-Treatment EDQoL
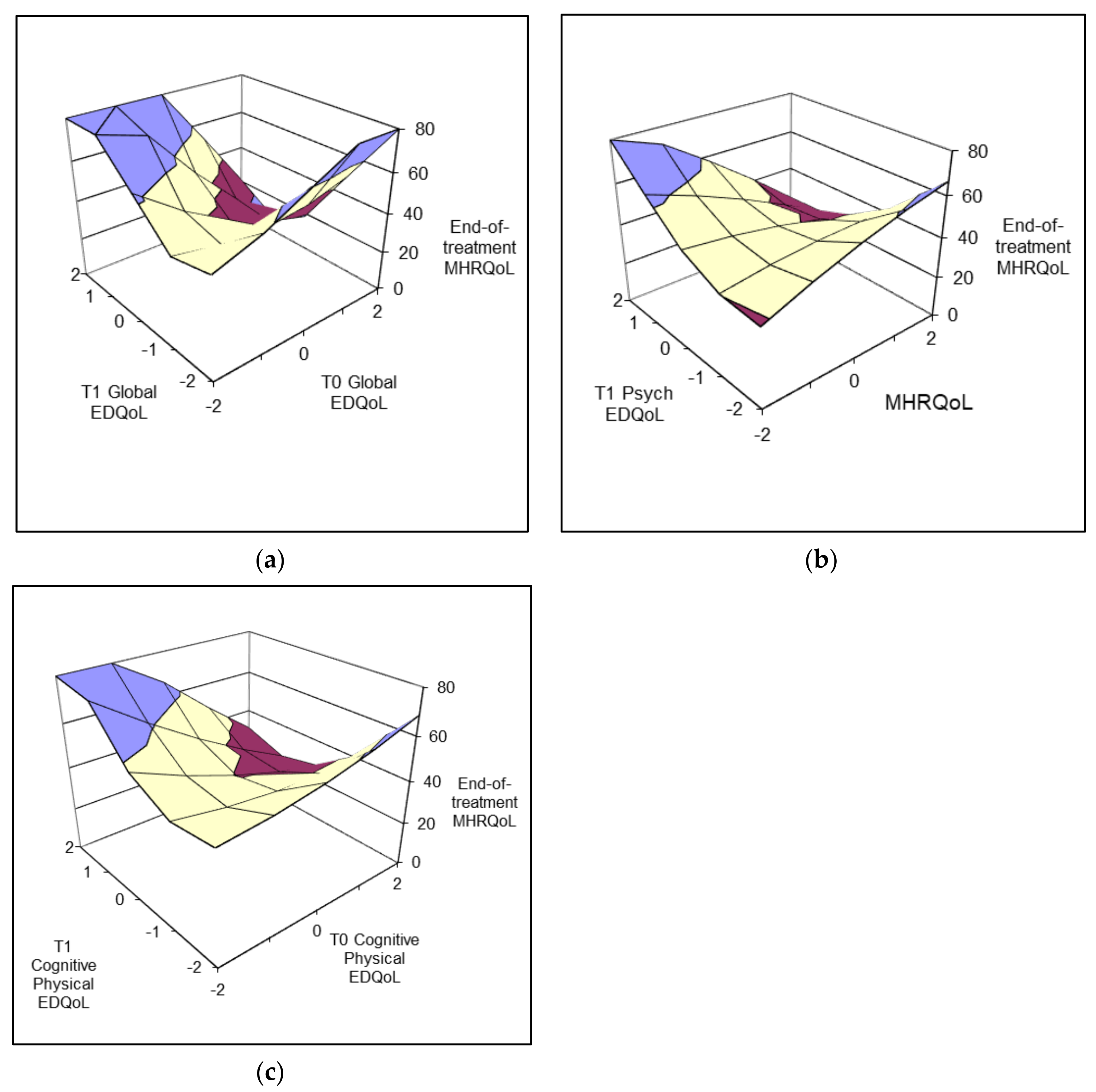
3.2.4. End-of-Treatment MHRQoL
4. Discussion
4.1. General Health-Related Quality of Life
4.2. Eating-Disorder-Specific Quality of Life
4.3. Implications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Response Surface Modelling
Appendix B. Descriptive Statistics for Study Variables
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| Age | 27.38 | 9.22 | 17.72 | 56.74 |
| T3 BMI | 17.76 | 2.99 | 10.70 | 26.46 |
| T3 EDEQ Global | 2.71 | 1.59 | 0.00 | 5.75 |
| T3 EDQoL | 1.05 | 0.86 | −0.95 | 3.69 |
| T3 PHRQoL | 50.89 | 10.18 | 13.11 | 85.86 |
| T3 MHRQoL | 37.38 | 10.82 | 11.48 | 60.45 |
| EDQoL T0 | 1.70 | 0.69 | 0.16 | 3.68 |
| EDQoL T1 | 1.51 | 0.67 | 0.06 | 2.71 |
| EDQoL EC | −0.18 | 0.53 | −2.34 | 1.11 |
| PHRQoL T0 | 46.90 | 10.17 | 19.64 | 65.59 |
| PHRQoL T1 | 47.39 | 11.00 | 20.77 | 69.39 |
| PHRQoL EC | 0.49 | 8.70 | −23.09 | 25.89 |
| MHRQoL T0 | 29.11 | 11.93 | 5.95 | 60.04 |
| MHRQoL T1 | 32.71 | 11.55 | 11.29 | 63.40 |
| MHRQoL EC | 3.60 | 10.02 | −18.89 | 41.21 |
| Psychological T0 | 2.75 | 0.88 | 0.13 | 4.00 |
| Psychological T1 | 2.35 | 0.84 | 0.22 | 4.00 |
| Psychological EC | −0.40 | 0.83 | −3.78 | 1.56 |
| Physical/cognitive T0 | 2.47 | 0.84 | 0.17 | 4.00 |
| Physical/cognitive T1 | 2.04 | 0.84 | 0.00 | 3.67 |
| Physical/cognitive EC | −0.44 | 0.73 | −4.00 | 1.00 |
| Financial T0 | 0.66 | 0.87 | 0.00 | 4.00 |
| Financial T1 | 0.45 | 0.61 | 0.00 | 3.40 |
| Financial EC | −0.21 | 0.82 | −3.55 | 1.60 |
| School/work T0 | 0.89 | 1.00 | 0.00 | 4.00 |
| School/work T1 | 0.76 | 0.79 | 0.00 | 3.40 |
| School/work EC | −0.13 | 0.86 | −3.20 | 2.80 |
| n = 78 | ||||
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- van den Berg, E.; Houtzager, L.; de Vos, J.; Daemen, I.; Katsaragaki, G.; Karyotaki, E.; Cuijpers, P.; Dekker, J. Meta-analysis on the efficacy of psychological treatments for anorexia nervosa. Eur. Eat. Disord. Rev. 2019, 27, 331–351. [Google Scholar] [CrossRef]
- Steinhausen, H.-C. The Outcome of Anorexia Nervosa in the 20th Century. Am. J. Psychiatry 2002, 159, 1284–1293. [Google Scholar] [CrossRef]
- Dobrescu, S.R.; Dinkler, L.; Gillberg, C.; Råstam, M.; Gillberg, C.; Wentz, E. Anorexia nervosa: 30-year outcome. Br. J. Psychiatry 2020, 216, 97–104. [Google Scholar] [CrossRef]
- Eddy, K.T.; Tabri, N.; Thomas, J.J.; Murray, H.B.; Keshaviah, A.; Hastings, E.; Edkins, K.; Krishna, M.; Herzog, D.B.; Keel, P.K.; et al. Recovery From Anorexia Nervosa and Bulimia Nervosa at 22-Year Follow-Up. J. Clin. Psychiatry 2017, 78, 184–189. [Google Scholar] [CrossRef]
- Wonderlich, S.A.; Bulik, C.M.; Schmidt, U.; Steiger, H.; Hoek, H.W. Severe and enduring anorexia nervosa: Update and observations about the current clinical reality. Int. J. Eat. Disord. 2020, 53, 1303–1312. [Google Scholar] [CrossRef]
- Bardone-Cone, A.M.; Hunt, R.A.; Watson, H.J. An overview of conceptualizations of eating disorder recovery, recent findings, and future directions. Curr. Psychiatry Rep. 2018, 20, 79. [Google Scholar] [CrossRef]
- Conti, J.E. Recovering identity from anorexia nervosa: Women’s constructions of their experiences of recovery from anorexia nervosa over 10 years. J. Constr. Psychol. 2018, 31, 72–94. [Google Scholar] [CrossRef]
- Federici, A.; Kaplan, A.S. The patient’s account of relapse and recovery in anorexia nervosa: A qualitative study. European Eating Disorders Review: Prof. J. Eat. Disord. Assoc. 2008, 16, 1–10. [Google Scholar] [CrossRef]
- Jenkins, J.; Ogden, J. Becoming ‘whole’ again: A qualitative study of women’s views of recovering from anorexia nervosa. Eur. Eat. Disord. Rev. 2012, 20, e23–e31. [Google Scholar] [CrossRef]
- Mitchison, D.; Hay, P.; Mond, J.; Slewa-Younan, S. Self-reported history of anorexia nervosa and current quality of life: Findings from a community-based study. Qual. Life Res. 2013, 22, 273–281. [Google Scholar] [CrossRef]
- Mitchison, D.; Morin, A.; Mond, J.; Slewa-Younan, S.; Hay, P. The Bidirectional Relationship between Quality of Life and Eating Disorder Symptoms: A 9-Year Community-Based Study of Australian Women. PLoS ONE 2015, 10, e0120591. [Google Scholar] [CrossRef]
- McIntosh, V.V.; Jordan, J.; Carter, F.A.; Luty, S.E.; McKenzie, J.M.; Bulik, C.M.; Frampton, C.M.; Joyce, P.R. Three Psychotherapies for Anorexia Nervosa: A Randomized, Controlled Trial. Am. J. Psychiatry 2005, 162, 741–747. [Google Scholar] [CrossRef]
- McIntosh, V.V.W.; Jordan, J.; Luty, S.E.; Carter, F.A.; McKenzie, J.M.; Bulik, C.M.; Joyce, P.R. Specialist supportive clinical management for anorexia nervosa. Int. J. Eat. Disord. 2006, 39, 625–632. [Google Scholar] [CrossRef]
- Williams, K.D.; Dobney, T.; Geller, J. Setting the eating disorder aside: An alternative model of care. Eur. Eat. Disord. Rev. 2010, 18, 90–96. [Google Scholar] [CrossRef]
- Nordbø, R.H.S.; Espeset, E.M.S.; Gulliksen, K.S.; Skårderud, F.; Geller, J.; Holte, A. Reluctance to recover in anorexia nervosa. Eur. Eat. Disord. Rev. 2012, 20, 60–67. [Google Scholar] [CrossRef]
- Hay, P.; Chinn, D.; Forbes, D.; Madden, S.; Newton, R.; Sugenor, L.; Touyz, S.; Ward, W. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust. N. Z. J. Psychiatry 2014, 48, 977–1008. [Google Scholar] [CrossRef]
- Wonderlich, S.; Mitchell, J.E.; Crosby, R.D.; Myers, T.C.; Kadlec, K.; LaHaise, K.; Swan-Kremeier, L.; Dokken, J.; Lange, M.; Dinkel, J.; et al. Minimizing and treating chronicity in the eating disorders: A clinical overview. Int. J. Eat. Disord. 2012, 45, 467–475. [Google Scholar] [CrossRef]
- Mond, J.M.; Owen, C.; Hay, P.J.; Rodgers, B.; Beumont, P.J.V. Assessing quality of life in eating disorder patients. Qual. Life Res. 2005, 14, 171–178. [Google Scholar] [CrossRef]
- McHugh, M.D. Readiness for change and short-term outcomes of female adolescents in residential treatment for anorexia nervosa. Int. J. Eat. Disord. 2007, 40, 602–612. [Google Scholar] [CrossRef]
- Grilo, C.M.; Masheb, R.M.; Wilson, G.T. Rapid response to treatment for binge eating disorder. J. Consult. Clin. Psychol. 2006, 74, 602–613. [Google Scholar] [CrossRef]
- Grilo, C.M.; White, M.A.; Wilson, G.T.; Gueorguieva, R.; Masheb, R.M. Rapid response predicts 12-month post-treatment outcomes in binge-eating disorder: Theoretical and clinical implications. Psychol. Med. 2012, 42, 807–817. [Google Scholar] [CrossRef]
- Masheb, R.M.; Grilo, C.M. Rapid response predicts treatment outcomes in binge eating disorder: Implications for stepped care. J. Consult. Clin. Psychol. 2007, 75, 639–644. [Google Scholar] [CrossRef]
- Isserlin, L.; Spettigue, W.; Norris, M.; Couturier, J. Outcomes of inpatient psychological treatments for children and adolescents with eating disorders at time of discharge: A systematic review. J. Eat. Disord. 2020, 8, 32. [Google Scholar] [CrossRef]
- Chang, P.G.R.Y.; Delgadillo, J.; Waller, G. Early response to psychological treatment for eating disorders: A systematic review and meta-analysis. Clin. Psychol. Rev. 2021, 86, 102032. [Google Scholar] [CrossRef]
- Linardon, J.; Brennan, L.; De La Piedad Garcia, X. Rapid response to eating disorder treatment: A systematic review and meta-analysis. Int. J. Eat. Disord. 2016, 49, 905–919. [Google Scholar] [CrossRef]
- Nazar, B.P.; Gregor, L.K.; Albano, G.; Marchica, A.; Coco, G.L.; Cardi, V.; Treasure, J. Early Response to treatment in Eating Disorders: A Systematic Review and a Diagnostic Test Accuracy Meta-Analysis. Eur. Eat. Disord. Rev. 2017, 25, 67–79. [Google Scholar] [CrossRef]
- Vall, E.; Wade, T.D. Predictors of treatment outcome in individuals with eating disorders: A systematic review and meta-analysis. Int. J. Eat. Disord. 2015, 48, 946–971. [Google Scholar] [CrossRef]
- Pellizzer, M.L.; Waller, G.; Wade, T.D. Predictors of outcome in cognitive behavioural therapy for eating disorders: An exploratory study. Behav. Res. Ther. 2019, 116, 61–68. [Google Scholar] [CrossRef]
- Kelly, A.C.; Carter, J.C.; Borairi, S. Are improvements in shame and self-compassion early in eating disorders treatment associated with better patient outcomes? Int. J. Eat. Disord. 2014, 47, 54–64. [Google Scholar] [CrossRef]
- Thompson-Brenner, H.; Shingleton, R.M.; Sauer-Zavala, S.; Richards, L.K.; Pratt, E.M. Multiple measures of rapid response as predictors of remission in cognitive behavior therapy for bulimia nervosa. Behav. Res. Ther. 2015, 64, 9–14. [Google Scholar] [CrossRef]
- Kahn, M.; Brunstein-Klomek, A.; Hadas, A.; Snir, A.; Fennig, S. Early changes in depression predict outcomes of inpatient adolescent anorexia nervosa. Eat. Weight. Disord. Stud. Anorex. Bulim. Obesity 2020, 25, 777–785. [Google Scholar] [CrossRef]
- Macdonald, D.E.; Trottier, K. Rapid improvements in emotion regulation predict eating disorder psychopathology and functional impairment at 6-month follow-up in individuals with bulimia nervosa and purging disorder. Int. J. Eat. Disord. 2019, 52, 962–967. [Google Scholar] [CrossRef]
- Reilly, E.E.; Perry, T.R.; Brown, T.A.; Wierenga, C.E.; Kaye, W.H. Intolerance of Uncertainty and Eating Disorder Symptoms Over the Course of Intensive Treatment. Behav. Ther. 2020, 52, 698–708. [Google Scholar] [CrossRef]
- Tecuta, L.; Tomba, E. Subjective incompetence as a predictor of treatment outcomes in eating disorder outpatients. Psychiatry Res. 2018, 266, 193–198. [Google Scholar] [CrossRef]
- Hay, P.; Touyz, S.; Arcelus, J.; Pike, K.; Attia, E.; Crosby, R.D.; Madden, S.; Wales, J.; La Puma, M.; Heriseanu, A.I.; et al. A randomized controlled trial of the compuLsive Exercise Activity TheraPy (LEAP): A new approach to compulsive exercise in anorexia nervosa. Int. J. Eat. Disord. 2018, 51, 999–1004. [Google Scholar] [CrossRef]
- Young, S.; Touyz, S.; Meyer, C.; Arcelus, J.; Rhodes, P.; Madden, S.; Pike, K.; Attia, E.; Crosby, R.D.; Hay, P. Relationships between compulsive exercise, quality of life, psychological distress and motivation to change in adults with anorexia nervosa. J. Eat. Disord. 2018, 6, 2. [Google Scholar] [CrossRef]
- Pike, K.M.; Walsh, B.T.; Vitousek, K.; Wilson, G.T.; Bauer, J. Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa. Am. J. Psychiatry 2003, 160, 2046–2049. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Engel, S.G.; Wittrock, D.A.; Crosby, R.D.; Wonderlich, S.A.; Mitchell, J.E.; Kolotkin, R.L. Development and psychometric validation of an eating disorder-specific health-related quality of life instrument. Int. J. Eat. Disord. 2006, 39, 62–71. [Google Scholar] [CrossRef]
- Shanock, L.R.; Baran, B.E.; Gentry, W.A.; Pattison, S.C.; Heggestad, E.D. Polynomial regression with response surface analysis: A powerful approach for examining moderation and overcoming limitations of difference scores. J. Bus. Psychol. 2010, 25, 543–554. [Google Scholar] [CrossRef]
- Edwards, J.R.; Parry, M.E. On the use of polynomial regression equations as an alternative to difference scores in organizational research. Acad. Manag. J. 1993, 36, 1577–1613. [Google Scholar] [CrossRef]
- Padierna, A.; Quintana, J.M.; Arostegui, I.; Gonzalez, N.; Horcajo, M.J. The health-related quality of life in eating disorders. Qual. Life Res. 2000, 9, 667–674. [Google Scholar] [CrossRef]
- Bamford, B.; Sly, R. Exploring quality of life in the eating disorders. Eur. Eat. Disord. Rev. 2010, 18, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Weigel, A.; König, H.-H.; Gumz, A.; Löwe, B.; Brettschneider, C. Correlates of health related quality of life in anorexia nervosa. Int. J. Eat. Disord. 2016, 49, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Errichiello, L.; Iodice, D.; Bruzzese, D.; Gherghi, M.; Senatore, I. Prognostic factors and outcome in anorexia nervosa: A follow-up study. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2016, 21, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Padierna, A.; Quintana, J.; Arostegui, I.; Gonzalez, N.; Horcajo, M. Changes in health related quality of life among patients treated for eating disorders. Qual. Life Res. 2002, 11, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Doll, H.A.; Petersen, S.E.; Stewart-Brown, S.L. Eating disorders and emotional and physical well-being: Associations between student self-reports of eating disorders and quality of life as measured by the SF-36. Qual. Life Res. 2005, 14, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Adair, C.E.; Marcoux, G.C.; Cram, B.S.; Ewashen, C.J.; Chafe, J.; Cassin, S.E.; Pinzon, J.; Gusella, J.L.; Geller, J.; Scattolon, Y.; et al. Development and multi-site validation of a new condition-specific quality of life measure for eating disorders. Health Qual. Life Outcomes 2007, 5, 23. [Google Scholar] [CrossRef] [PubMed]
- Castellano, S.; Rizzotto, A.; Neri, S.; Currenti, W.; Guerrera, C.S.; Pirrone, C.; Coco, M.; Di Corrado, D. The Relationship between Body Dissatisfaction and Eating Disorder Symptoms in Young Women Aspiring Fashion Models: The Mediating Role of Stress. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 607–615. [Google Scholar] [CrossRef]
- Touyz, S.; Le Grange, D.; Lacey, H.; Hay, P.; Smith, R.; Maguire, S.; Bamford, B.; Pike, K.M.; Crosby, R.D. Treating severe and enduring anorexia nervosa: A randomized controlled trial. Psychol. Med. 2013, 43, 2501–2511. [Google Scholar] [CrossRef] [PubMed]
| Variables | BMI T3 | EDEQ−0Global T3 | EDQoL T3 | MHRQoL T3 | PHRQoL T3 |
|---|---|---|---|---|---|
| MHRQoL EC | −0.204 | −0.176 | 0.032 | −0.047 | −0.139 |
| PHRQoL EC | 0.158 | 0.279 | −0.028 | −0.122 | 0.141 |
| EDQoL EC | 0.020 | 0.041 | 0.026 | 0.116 | −0.010 |
| Psychological EC | 0.177 | −0.019 | −0.171 | 0.221 | −0.084 |
| Physical/cognitive EC | 0.096 | −0.184 | −0.202 | 0.207 | −0.106 |
| Financial EC | 0.011 | −0.101 | 0.038 | 0.180 | 0.026 |
| School/work EC | 0.076 | −0.078 | −0.171 | 0.203 | 0.154 |
| BMI | EDE-Q | EDQoL | MHRQoL | PHRQoL | |
|---|---|---|---|---|---|
| b (se) | b (se) | b (se) | b (se) | b (se) | |
| Constant | 17.38 (0.48) | 3.25 (0.23) | 1.38 (0.11) | 33.58 (1.51) | 49.78 (1.73) |
| b1: T0 | 0.03 (0.93) | 0.72 (0.46) | 0.56 (0.22) | −11.18 (3.01) | 0.41 (3.32) |
| b2: T1 | −0.98 (1.03) | 0.34 (0.50) | 0.39 (0.24) | 3.89 (3.23) | −1.59 (3.69) |
| b3: T02 | −0.86 (0.96) | 0.10 (0.48) | 0.15 (0.23) | 1.77 (3.10) | −3.39 (3.43) |
| b4: T0 × T1 | 0.05 (2.09) | 0.98 (1.01) | 0.72 (0.49) | −12.13 (6.60) | 0.27 (7.50) |
| b5: T12 | 0.69 (1.33) | −1.06 (0.64) | −0.42 (.31) | 10.80 (4.18) | 3.31 (4.76) |
| R2 | 0.095 | 0.271 ** | 0.385 ** | 0.349 ** | 0.066 |
| Response surface modelling coefficients | |||||
| a1 | - | 1.06 * | 0.95 * | −7.29 ** | - |
| a2 | - | 0.02 | 0.15 | 0.44 | - |
| a3 | - | 0.37 | 0.18 | −15.07 ** | - |
| a4 | - | −1.94 | −1.29 | 24.70 ** | - |
| BMI | EDE-Q | EDQoL | MHRQoL | PHRQoL | |
|---|---|---|---|---|---|
| b (se) | b (se) | b (se) | b (se) | b (se) | |
| Constant | 18.14 (0.52) | 1.91 (0.24) | 0.61 (0.13) | 42.54 (1.64) | 52.51 (1.75) |
| b1: T0 | −2.11 (0.97) | −0.49 (0.44) | 0.53 (0.24) | −4.26 (3.07) | 4.67 (3.27) |
| b2: T1 | 1.13 (0.76) | 0.88 (0.35) | −0.01 (0.19) | 0.47 (2.42) | −4.75 (2.58) |
| b3: T02 | 1.10 (0.68) | 0.72 (0.31) | −0.08 (0.17) | −0.63 (2.17) | −3.64 (2.31) |
| b4: T0 × T1 | −1.73 (1.06) | −0.12 (0.49) | 0.36 (0.26) | −5.64 (3.38) | 3.85 (3.59) |
| b5: T12 | 1.06 (0.63) | 0.02 (0.29) | −0.21 (0.16) | 3.36 (2.00) | −1.68 (2.13) |
| R2 | 0.108 | 0.381 ** | 0.356 ** | 0.365 ** | 0.071 |
| Response surface modelling coefficients | |||||
| a1 | - | 0.39 | 0.51 * | −3.79 | - |
| a2 | - | 0.63 * | 0.07 | −2.90 | - |
| a3 | - | −1.37 | 0.54 | −4.73 | - |
| a4 | - | 0.86 | −0.64 | 8.37 | - |
| BMI | EDE-Q | EDQoL | MHRQoL | PHRQoL | |
|---|---|---|---|---|---|
| b (se) | b (se) | b (se) | b (se) | b (se) | |
| Constant | 18.23 (0.53) | 2.57 (0.27) | 0.83 (0.14) | 39.53 (1.74) | 52.82 (1.81) |
| b1: T0 | 0.39 (0.92) | 0.99 (0.46) | 0.22 (0.24) | −7.37 (3.01) | 2.43 (3.14) |
| b2: T1 | −1.14 (0.86) | −0.43 (0.43) | 0.17 (0.22) | 2.39 (2.82) | −6.03 (2.94) |
| b3: T02 | −1.38 (0.75) | −0.29 (0.38) | 0.34 (0.19) | 0.78 (2.47) | −3.79 (2.57) |
| b4: T0 × T1 | 1.74 (1.46) | 1.02 (0.74) | −0.39 (0.38) | −5.96 (4.78) | 6.87 (4.99) |
| b5: T12 | −0.29 (0.99) | −0.91 (0.50) | −0.03 (0.26) | 5.44 (3.24) | −4.41 (3.38) |
| R2 | 129 | 0.180 * | 0.281 ** | 0.265 ** | 0.112 |
| Response surface modelling coefficients | |||||
| a1 | - | 0.56 | 0.39 * | −4.98 * | - |
| a2 | - | −0.18 | −0.08 | 0.26 | - |
| a3 | - | 1.42 | 0.06 | −9.76 | - |
| a4 | - | −2.21 | 0.70 | 12.18 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Newton, E.D.; Liu, L.; Conti, J.; Touyz, S.; Arcelus, J.; Madden, S.; Pike, K.; Hay, P. Early Change in Quality of Life in the Treatment of Anorexia Nervosa. Psych 2024, 6, 288-304. https://doi.org/10.3390/psych6010018
Newton ED, Liu L, Conti J, Touyz S, Arcelus J, Madden S, Pike K, Hay P. Early Change in Quality of Life in the Treatment of Anorexia Nervosa. Psych. 2024; 6(1):288-304. https://doi.org/10.3390/psych6010018
Chicago/Turabian StyleNewton, Eliza D., Liquan Liu, Janet Conti, Stephen Touyz, Jon Arcelus, Sloane Madden, Kathleen Pike, and Phillipa Hay. 2024. "Early Change in Quality of Life in the Treatment of Anorexia Nervosa" Psych 6, no. 1: 288-304. https://doi.org/10.3390/psych6010018
APA StyleNewton, E. D., Liu, L., Conti, J., Touyz, S., Arcelus, J., Madden, S., Pike, K., & Hay, P. (2024). Early Change in Quality of Life in the Treatment of Anorexia Nervosa. Psych, 6(1), 288-304. https://doi.org/10.3390/psych6010018






