The IADC Grief Questionnaire as a Brief Measure for Complicated Grief in Clinical Practice and Research: A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Instruments
2.3. Data Analysis
3. Results
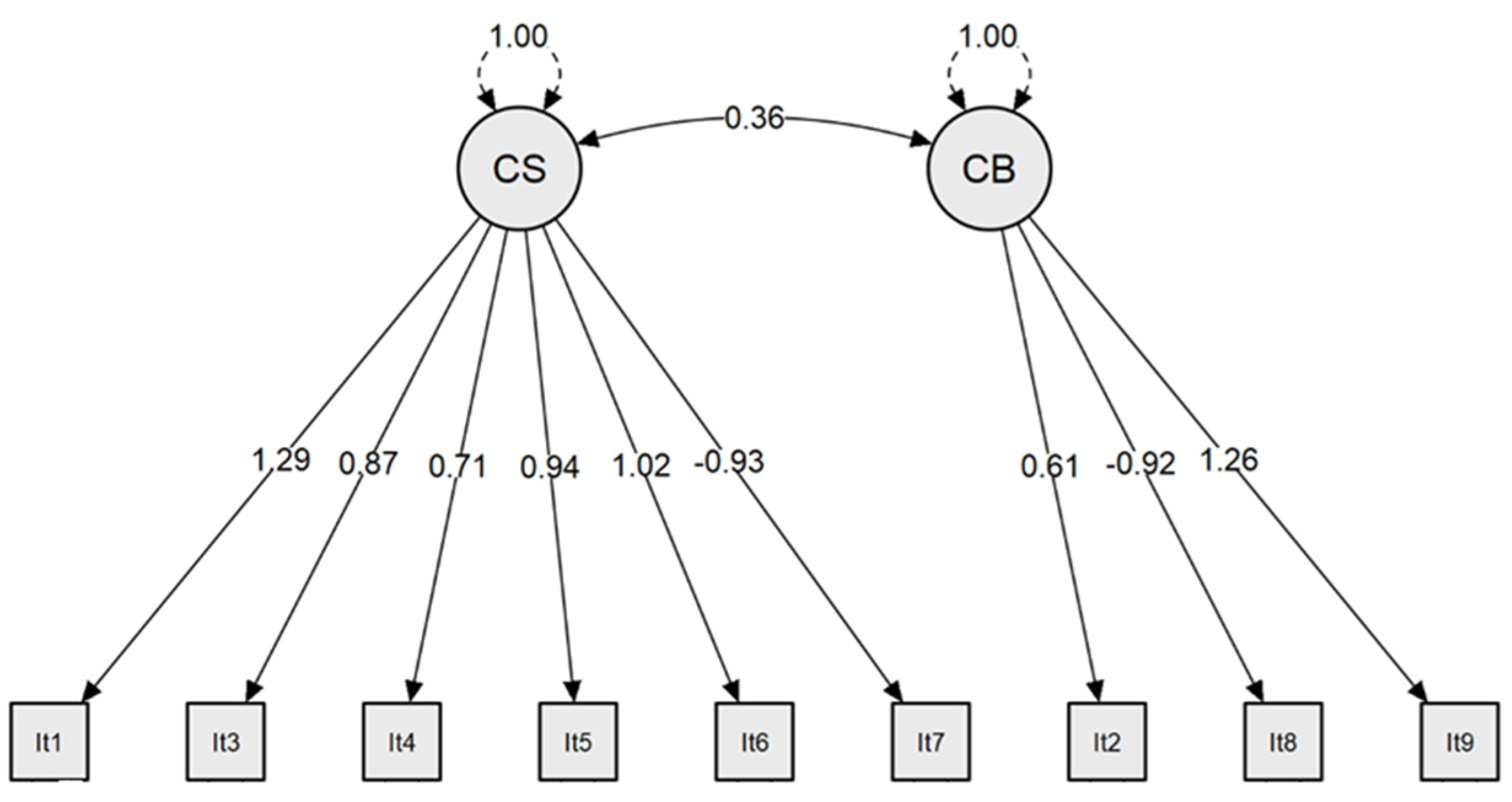
3.1. Dimensionality
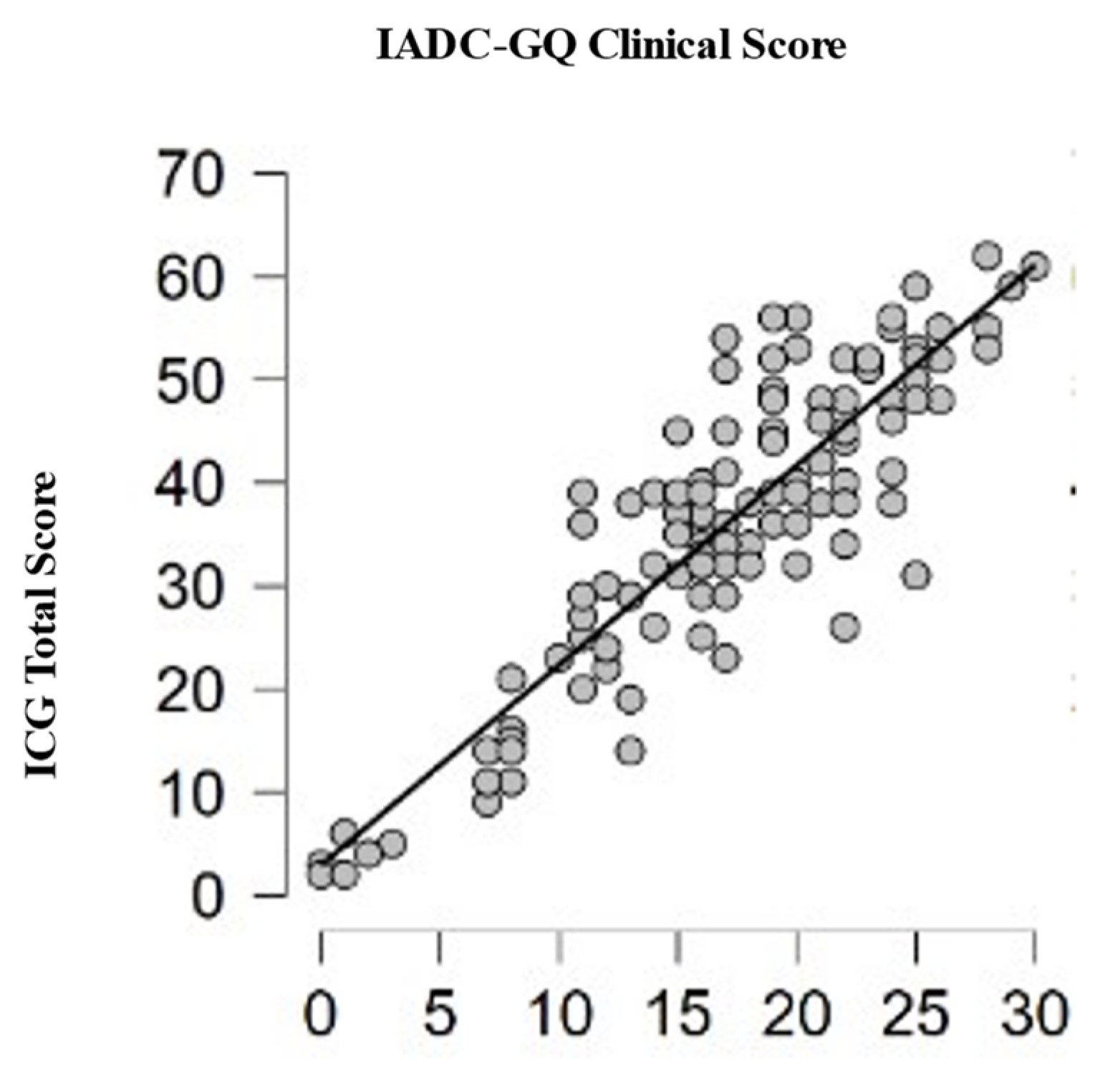
3.2. Reliability and Validity
3.3. Previous Experience of After-Death Communication (ADC) and Complicated Grief (CG)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Prigerson, H.G.; Maciejewski, P.K.; Reynolds, C.F., 3rd; Bierhals, A.J.; Newsom, J.T.; Fasiczka, A.; Frank, E.; Doman, J.; Miller, M. Inventory of Complicated Grief: A Scale to Measure Maladaptive Symptoms of Loss. Psychiatry Res. 1995, 59, 65–79. [Google Scholar] [CrossRef]
- Horowitz, M.J.; Bonanno, G.A.; Holen, A. Pathological Grief: Diagnosis and Explanation. Psychosom. Med. 1993, 55, 260–273. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, M.J.; Siegel, B.; Holen, A.; Bonanno, G.A.; Milbrath, C.; Stinson, C.H. Diagnostic Criteria for Complicated Grief Disorder. Am. J. Psychiatry 1997, 154, 904–910. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Szuhany, K.L.; Malgaroli, M.; Miron, C.D.; Simon, N.M. Prolonged Grief Disorder: Course, Diagnosis, Assessment, and Treatment. Focus Am. Psychiatr. Publ. 2021, 19, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Maercker, A.; Lalor, J. Diagnostic and Clinical Considerations in Prolonged Grief Disorder. Dialogues Clin. Neurosci. 2012, 14, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Bergsmark, L.P.S.; Ramsing, F. Which Considerations Are Lost When Debating the Prolonged Grief Disorder Diagnosis? Theory Psychol. 2023, 33, 856–872. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic And Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR); American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2022. [Google Scholar] [CrossRef]
- Maciejewski, P.K.; Maercker, A.; Boelen, P.A.; Prigerson, H.G. “Prolonged Grief Disorder” and “Persistent Complex Bereavement Disorder”, but Not “Complicated Grief”, Are One and the Same Diagnostic Entity: An Analysis of Data from the Yale Bereavement Study. World Psychiatry 2016, 15, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Zisook, S.; Pies, R.; Corruble, E. When Is Grief a Disease? Lancet 2012, 379, 1590. [Google Scholar] [CrossRef]
- Hilberdink, C.E.; Ghainder, K.; Dubanchet, A.; Hinton, D.; Djelantik, A.A.A.M.J.; Hall, B.J.; Bui, E. Bereavement Issues and Prolonged Grief Disorder: A Global Perspective. Glob. Ment. Health 2023, 10, e32. [Google Scholar] [CrossRef]
- Lundorff, M.; Holmgren, H.; Zachariae, R.; Farver-Vestergaard, I.; O’Connor, M. Prevalence of Prolonged Grief Disorder in Adult Bereavement: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2017, 212, 138–149. [Google Scholar] [CrossRef]
- Djelantik, A.A.A.M.J.; Smid, G.E.; Mroz, A.; Kleber, R.J.; Boelen, P.A. The Prevalence of Prolonged Grief Disorder in Bereaved Individuals Following Unnatural Losses: Systematic Review and Meta Regression Analysis. J. Affect. Disord. 2020, 265, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Eisma, M.C.; Lenferink, L.I.M.; Chow, A.Y.M.; Chan, C.L.W.; Li, J. Complicated Grief and Post-Traumatic Stress Symptom Profiles in Bereaved Earthquake Survivors: A Latent Class Analysis. Eur. J. Psychotraumatol. 2019, 10, 1558707. [Google Scholar] [CrossRef]
- Marques, L.; Bui, E.; LeBlanc, N.; Porter, E.; Robinaugh, D.; Dryman, M.T.; Nadal-Vicens, M.; Worthington, J.; Simon, N. Complicated Grief Symptoms in Anxiety Disorders: Prevalence and Associated Impairment. Depress. Anxiety 2013, 30, 1211–1216. [Google Scholar] [CrossRef]
- Mash, H.B.H.; Fullerton, C.S.; Shear, M.K.; Ursano, R.J. Complicated Grief and Depression in Young Adults: Personality and Relationship Quality. J. Nerv. Ment. Dis. 2014, 202, 539–543. [Google Scholar] [CrossRef]
- O’Connor, M.; Lasgaard, M.; Shevlin, M.; Guldin, M.-B. A Confirmatory Factor Analysis of Combined Models of the Harvard Trauma Questionnaire and the Inventory of Complicated Grief-Revised: Are We Measuring Complicated Grief or Posttraumatic Stress? J. Anxiety Disord. 2010, 24, 672–679. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sung, S.C.; Dryman, M.T.; Marks, E.; Shear, M.K.; Ghesquiere, A.; Fava, M.; Simon, N.M. Complicated Grief among Individuals with Major Depression: Prevalence, Comorbidity, and Associated Features. J. Affect. Disord. 2011, 134, 453–458. [Google Scholar] [CrossRef]
- Faschingbauer, T.R.; Devaul, R.A.; Zisook, S. Development of the Texas Inventory of Grief. Am. J. Psychiatry 1977, 134, 696–698. [Google Scholar] [CrossRef] [PubMed]
- Neimeyer, R.A. Complicated Grief: Assessment and Intervention. In APA Handbook of Trauma Psychology: Trauma Practice; Gold, S.N., Ed.; American Psychological Association: Washington, DC, USA, 2017; pp. 343–362. [Google Scholar] [CrossRef]
- Schakowski, A.; Tönnies, J.; Friederich, H.-C.; Hartmann, M.; Haun, M.W. The Inventory of Complicated Grief-A Systematic Psychometric Review and Conceptual Replication Study of the Structural Validity. Assessment 2023, 30, 1418–1434. [Google Scholar] [CrossRef]
- Hinton, D.E.; Peou, S.; Joshi, S.; Nickerson, A.; Simon, N.M. Normal Grief and Complicated Bereavement among Traumatized Cambodian Refugees: Cultural Context and the Central Role of Dreams of the Dead. Cult. Med. Psychiatry 2013, 37, 427–464. [Google Scholar] [CrossRef]
- Steffen, E.; Coyle, A. Sense of Presence Experiences and Meaning-Making in Bereavement: A Qualitative Analysis. Death Stud. 2011, 35, 579–609. [Google Scholar] [CrossRef]
- Streit-Horn, J. A Systematic Review of Research on After-Death Communication; University of North Texas: Denton, TX, USA, 2011. [Google Scholar]
- Woollacott, M.; Roe, C.A.; Cooper, C.E.; Lorimer, D.; Elsaesser, E. Perceptual Phenomena Associated with Spontaneous Experiences of After-Death Communication: Analysis of Visual, Tactile, Auditory and Olfactory Sensations. Explore 2022, 18, 423–431. [Google Scholar] [CrossRef]
- Guggenheim, B.; Guggenheim, J. Hello from Heaven: A New Field of Research-After-Death Communication Confirms That Life and Love Are Eternal; Bantam Books: New York, NY, USA, 1995. [Google Scholar]
- Houck, J.A. The Universal, Multiple, and Exclusive Experiences of after-Death Communication. J. Near-Death Stud. 2005, 24, 117–127. [Google Scholar] [CrossRef]
- Gariglietti, K.; Allison, J.A. Laypersons’ Perceptions of after-Death Communication. J. Pers. Interpers. Loss 1997, 2, 71–82. [Google Scholar] [CrossRef]
- Beischel, J. Spontaneous, Facilitated, Assisted, and Requested After-Death Communication Experiences and Their Impact on Grief. Threshold. J. Interdiscip. Conscious. Stud. 2019, 3, 1–32. [Google Scholar]
- Keen, C.; Murray, C.D.; Payne, S. A Qualitative Exploration of Sensing the Presence of the Deceased Following Bereavement. Mortality 2013, 18, 339–357. [Google Scholar] [CrossRef]
- LaGrand, L.E. The Nature and Therapeutic Implications of the Extraordinary Experiences of the Bereaved. J. Near-Death Stud. 2005, 24, 3–20. [Google Scholar]
- Haraldsson, E. Popular Psychology, Belief in Life after Death and Reincarnation in the Nordic Countries, Western and Eastern Europe. Nord. Psychol. 2006, 58, 171–180. [Google Scholar] [CrossRef]
- Burton, J. Contact with the Dead: A Common Experience? Fate 1982, 35, 65–73. [Google Scholar]
- Castelnovo, A.; Cavallotti, S.; Gambini, O.; D’Agostino, A. Post-Bereavement Hallucinatory Experiences: A Critical Overview of Population and Clinical Studies. J. Affect. Disord. 2015, 186, 266–274. [Google Scholar] [CrossRef]
- Haraldsson, E. Cases of the Reincarnation Type and the Mind–Brain Relationship. In Exploring Frontiers of the Mind-Brain Relationship. Mindfulness in Behavioral Health; Moreira-Almeida, A., Santana Santos, F., Eds.; Springer: New York, NY, USA, 2012; pp. 215–231. [Google Scholar] [CrossRef]
- Kalish, R.A.; Reynolds, D.K. Phenomenological Reality and Post-Death Contact. J. Sci. Study Relig. 1973, 12, 209–221. [Google Scholar] [CrossRef]
- Datson, S.L.; Marwit, S.J. Personality Constructs and Perceived Presence of Deceased Loved Ones. Death Stud. 1997, 21, 131–146. [Google Scholar] [CrossRef]
- LaGrand, L.E. Messages and Miracles: Extraordinary Experiences of the Bereaved; Llewellyn Publications: Woodbury, MN, USA, 2000. [Google Scholar]
- Penberthy, J.K.; Pehlivanova, M.; Kalelioglu, T.; Roe, C.A.; Cooper, C.E.; Lorimer, D.; Elsaesser, E. Factors Moderating the Impact of After Death Communications on Beliefs and Spirituality. OMEGA-J. Death Dying 2021, 87, 884–901. [Google Scholar] [CrossRef]
- Hastings, A. Effects on Bereavement Using a Restricted Sensory Environment (Psychomanteum). J. Transpers. Psychol. 2012, 44, 1–25. [Google Scholar]
- Exline, J.J. Psychopathology, Normal Psychological Processes, or Supernatural Encounters? Three Ways to Frame Reports of after-Death Communication. Spiritual. Clin. Pract. 2021, 8, 164–176. [Google Scholar] [CrossRef]
- Kamp, K.S.; O’Connor, M.; Spindler, H.; Moskowitz, A. Bereavement Hallucinations after the Loss of a Spouse: Associations with Psychopathological Measures, Personality and Coping Style. Death Stud. 2019, 43, 260–269. [Google Scholar] [CrossRef]
- Pait, K.C.; Exline, J.J.; Pargament, K.I.; Zarrella, P. After-Death Communication: Issues of Nondisclosure and Implications for Treatment. Religions 2023, 14, 985. [Google Scholar] [CrossRef]
- Klass, D.; Silverman, P.R.; Nickman, S. (Eds.) Continuing Bonds: New Understandings of Grief (Death Education, Aging and Health Care), 1st ed.; Routledge/Taylor & Francis Group: New York, NY, USA, 1996. [Google Scholar]
- Beischel, J.; Mosher, C.; Boccuzzi, M. The Possible Effects on Bereavement of Assisted After-Death Communication during Readings with Psychic Mediums: A Continuing Bonds Perspective. Omega 2015, 70, 169–194. [Google Scholar] [CrossRef] [PubMed]
- Bowlby, E.J.M. Loss-Sadness and Depression: Attachment and Loss; Pimlico: London, UK, 1998; Volume 3. [Google Scholar]
- Root, B.L.; Exline, J.J. The Role of Continuing Bonds in Coping with Grief: Overview and Future Directions. Death Stud. 2014, 38, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hewson, H.; Galbraith, N.; Jones, C.; Heath, G. The Impact of Continuing Bonds Following Bereavement: A Systematic Review. Death Stud. 2023; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Botkin, A. Induced after Death Communication: A Miraculous Therapy for Grief and Loss, Reprint ed.; Hampton Roads Publishing: Newburyport, MA, USA, 2005. [Google Scholar]
- Hannah, M.T.; Botkin, A.L.; Marrone, J.G.; Streit-Horn, J. Induced After-Death Communication: An Update. J. Near-Death Stud. 2013, 31, 213–220. [Google Scholar]
- Yamamoto, J.O.E.; Okonogi, K.; Iwasaki, T.; Yoshimura, S. Mourning in Japan. Am. J. Psychiatry 1969, 125, 1660–1665. [Google Scholar] [CrossRef]
- Rees, W.D. The Hallucinations of Widowhood. Br. Med. J. 1971, 4, 37–41. [Google Scholar] [CrossRef]
- Anderson, W.G.; Arnold, R.M.; Angus, D.C.; Bryce, C.L. Posttraumatic Stress and Complicated Grief in Family Members of Patients in the Intensive Care Unit. J. Gen. Intern. Med. 2008, 23, 1871–1876. [Google Scholar] [CrossRef]
- Shear, K.; Frank, E.; Houck, P.R.; Reynolds, C.F., 3rd. Treatment of Complicated Grief: A Randomized Controlled Trial. JAMA 2005, 293, 2601–2608. [Google Scholar] [CrossRef] [PubMed]
- Zisook, S.; Shear, M.K.; Reynolds, C.F.; Simon, N.M.; Mauro, C.; Skritskaya, N.A.; Lebowitz, B.; Wang, Y.; Tal, I.; Glorioso, D.; et al. Treatment of Complicated Grief in Survivors of Suicide Loss: A HEAL Report. J. Clin. Psychiatry 2018, 79, 17m11592. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Shear, M.K.; Massimetti, G.; Wall, M.; Mauro, C.; Gemignani, S.; Conversano, C.; Dell’Osso, L. Validation of the Italian Version Inventory of Complicated Grief (ICG): A Study Comparing CG Patients versus Bipolar Disorder, PTSD and Healthy Controls. Compr. Psychiatry 2014, 55, 1322–1329. [Google Scholar] [CrossRef]
- Prigerson, H.G.; Boelen, P.A.; Xu, J.; Smith, K.V.; Maciejewski, P.K. Validation of the New DSM-5-TR Criteria for Prolonged Grief Disorder and the PG-13-Revised (PG-13-R) Scale. World Psychiatry 2021, 20, 96–106. [Google Scholar] [CrossRef]
- Lenferink, L.I.M.; Eisma, M.C.; Smid, G.E.; de Keijser, J.; Boelen, P.A. Valid Measurement of DSM-5 Persistent Complex Bereavement Disorder and DSM-5-TR and ICD-11 Prolonged Grief Disorder: The Traumatic Grief Inventory-Self Report Plus (TGI-SR+). Compr. Psychiatry 2022, 112, 152281. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Stroebe, W.; van de Schoot, R.; Schut, H.; Abakoumkin, G.; Li, J. Guilt in Bereavement: The Role of Self-Blame and Regret in Coping with Loss. PLoS ONE 2014, 9, e96606. [Google Scholar] [CrossRef] [PubMed]
- Wagner, B.; Hofmann, L.; Grafiadeli, R. The Relationship between Guilt, Depression, Prolonged Grief, and Posttraumatic Stress Symptoms after Suicide Bereavement. J. Clin. Psychol. 2021, 77, 2545–2558. [Google Scholar] [CrossRef]
- Joa, B.; Newberg, A.B. Neuropsychological Comparison of Guilt and Grief: A Review of Guilt Aspects in Prolonged Grief Disorder. Omega 2023, 87, 591–613. [Google Scholar] [CrossRef] [PubMed]
- Draper, P.; Holloway, M.; Adamson, S. A Qualitative Study of Recently Bereaved People’s Beliefs about Death: Implications for Bereavement Care. J. Clin. Nurs. 2014, 23, 1300–1308. [Google Scholar] [CrossRef] [PubMed]
- Benore, E.R.; Park, C.L. Death-Specific Religious Beliefs and Bereavement: Belief in an Afterlife and Continued Attachment. Int. J. Psychol. Relig. 2004, 14, 1–22. [Google Scholar] [CrossRef]
- Field, N.P.; Filanosky, C. Continuing Bonds, Risk Factors for Complicated Grief, and Adjustment to Bereavement. Death Stud. 2010, 34, 1–29. [Google Scholar] [CrossRef]
- Ito, M.; Nakajima, S.; Fujisawa, D.; Miyashita, M.; Kim, Y.; Shear, M.K.; Ghesquiere, A.; Wall, M.M. Brief Measure for Screening Complicated Grief: Reliability and Discriminant Validity. PLoS ONE 2012, 7, e31209. [Google Scholar] [CrossRef]
| Categories | N | % | |
|---|---|---|---|
| Gender | Female | 102 | 90.27% |
| Male | 11 | 9.73% | |
| Education | Primary school | 1 | 0.88% |
| Secondary school | 57 | 50.44% | |
| Bachelor’s degree | 55 | 48.67% | |
| Ongoing treatment with various psychotropic drugs | Yes | 24 | 21.24% |
| No | 89 | 78.76% | |
| Previous ADC experiences | Yes | 27 | 23.89% |
| No | 86 | 76.11% | |
| Importance of spirituality in life | Not at all important | 2 | 1.77% |
| Slightly important | 4 | 3.54% | |
| Neutral | 11 | 9.73% | |
| Moderately important | 35 | 30.97% | |
| Very important | 61 | 53.98% | |
| Gender of the deceased | Female | 57 | 50.44% |
| Male | 56 | 49.56% | |
| Deceased’s relation to the bereaved | Child | 25 | 22.12% |
| Parent | 43 | 38.05% | |
| Spouse/partner | 23 | 20.35% | |
| Sibling | 7 | 6.19% | |
| Other family member | 11 | 9.73% | |
| Close friend | 1 | 0.88% | |
| Pet | 3 | 2.65% | |
| Cause of death | Disease | 80 | 70.80% |
| Accident | 22 | 19.47% | |
| Suicide | 8 | 7.08% | |
| Murder | 3 | 2.65% |
| Items | Factor | |
|---|---|---|
| 1 | 2 | |
| 0.789 | |
| 0.503 | |
| Rank the intensity of each feeling you have associated with your loss: | ||
| 0.620 | |
| 0.440 | |
| 0.671 | |
| 0.579 | |
| −0.610 | |
| −0.653 | |
| 0.657 | |
| Age of Participants | Age of the Deceased | ICG Total Score | IADC-GQ Clinical Score | IADC-GQ Continuing Bond | |
|---|---|---|---|---|---|
| M | 51.02 | 51.49 | 35.47 | 16.78 | 10.62 |
| SD | 12.15 | 25.92 | 14.61 | 6.63 | 3.54 |
| Min. | 21.69 | 0.30 | 2.00 | 0.00 | 1.00 |
| Max | 80.64 | 99.32 | 62.00 | 30.00 | 15.00 |
| Variable | ICG Total Score | IADC-GQ Clinical Score | IADC-GQ Continuing Bond |
|---|---|---|---|
| ICG Total Score | - | ||
| IADC-GQ Clinical Score | 0.880 *** | - | |
| IADC-GQ Continuing Bond | 0.124 | 0.162 | - |
| Group | Mean | SD | SE | |
|---|---|---|---|---|
| ICG Total Score | 1 | 32.48 | 13.84 | 2.66 |
| 2 | 36.41 | 14.79 | 1.60 | |
| IADC-GQ Clinical Score | 1 | 16.41 | 6.48 | 1.25 |
| 2 | 16.90 | 6.70 | 0.72 | |
| IADC-GQ Continuing Bond | 1 | 11.89 | 2.69 | 0.52 |
| 2 | 10.22 | 3.70 | 0.40 | |
| ICG Total Score | 1 | 32.48 | 13.84 | 2.66 |
| 2 | 36.41 | 14.79 | 1.60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Antoni, F.; Lalla, C. The IADC Grief Questionnaire as a Brief Measure for Complicated Grief in Clinical Practice and Research: A Preliminary Study. Psych 2024, 6, 196-209. https://doi.org/10.3390/psych6010012
D’Antoni F, Lalla C. The IADC Grief Questionnaire as a Brief Measure for Complicated Grief in Clinical Practice and Research: A Preliminary Study. Psych. 2024; 6(1):196-209. https://doi.org/10.3390/psych6010012
Chicago/Turabian StyleD’Antoni, Fabio, and Claudio Lalla. 2024. "The IADC Grief Questionnaire as a Brief Measure for Complicated Grief in Clinical Practice and Research: A Preliminary Study" Psych 6, no. 1: 196-209. https://doi.org/10.3390/psych6010012
APA StyleD’Antoni, F., & Lalla, C. (2024). The IADC Grief Questionnaire as a Brief Measure for Complicated Grief in Clinical Practice and Research: A Preliminary Study. Psych, 6(1), 196-209. https://doi.org/10.3390/psych6010012





