ADHD Assessment Recommendations for Children in Practice Guidelines: A Systematic Review
Abstract
1. Introduction
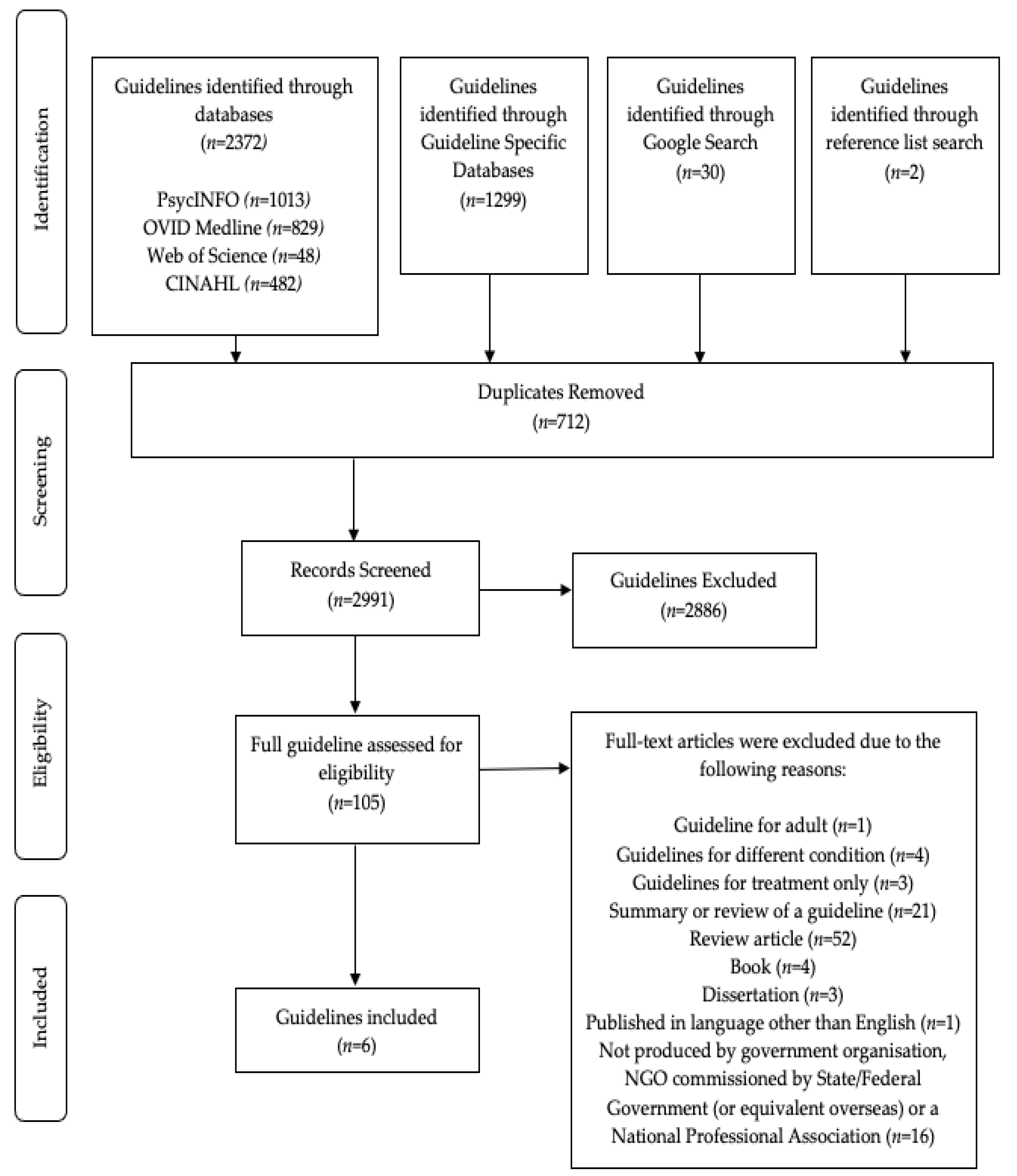
2. Materials and Methods
2.1. Database Search
2.2. Grey Literature
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Screening
2.6. Guideline Quality Assessment Tool: AGREE II
3. Results
3.1. Quality Assessment
3.2. Recommended Assessment Process
3.3. Recommended Co-occurring Process
3.4. Recommended Differential Diagnosis Process
3.5. Content Analysis and Level of Evidence
4. Discussion
4.1. Ratings of Guidelines and Evidence for Recommendations
4.2. Recommended Assessment Process
4.3. Differential Diagnosis Assessment Process
4.4. Co-occurring Assessment Process
4.5. Gaps
4.6. Limitations
4.7. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef] [PubMed]
- Efron, D.; Sciberras, E. The diagnostic outcomes of children with suspected attention deficit hyperactivity disorder following multidisciplinary assessment. J. Paediatr. Child Health 2010, 46, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.N.; Morrill, M.S.; Parente, S.T. Measuring inappropriate medical diagnosis and treatment in survey data: The case of ADHD among school-age children. J. Health Econ. 2010, 29, 657–673. [Google Scholar] [CrossRef] [PubMed]
- Merten, E.C.; Cwik, J.C.; Margraf, J.; Schneider, S. Overdiagnosis of mental disorders in children and adolescents (in developed countries). Child Adolesc. Psychiatry Ment. Health 2017, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.; Corkum, P. ADHD Diagnosis: As simple as administering a questionnaire or a complex diagnostic process? J. Atten. Disord. 2016, 20, 478–486. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Text Revision; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- Barkley, R.A. (Ed.) Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment, 4th ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Carr, A. The Handbook of Child and Adolescent Clinical Psychology; Routledge: New York, NY, USA, 2016. [Google Scholar] [CrossRef]
- Virring, A.; Lambek, R.; Thomsen, P.H.; Moller, L.R.; Jennum, P.J. Disturbed sleep in attention-deficit hyperactivity disorder (ADHD) is not a question of psychiatric comorbidity of ADHD presentation. J. Sleep Res. 2016, 25, 333–340. [Google Scholar] [CrossRef]
- Sciberras, E.; Lycett, K.; Efron, D.; Mensah, R.; Gerner, B.; Hiscock, H. Anxiety in children with attention-deficit/hyperactivity disorder. Pediatrics 2014, 133, 801–808. [Google Scholar] [CrossRef]
- Harpin, V.A. The effect of ADHD on the life of an individual, their family and community from preschool to adult life. Arch. Dis. Child. 2005, 90, 12–17. [Google Scholar] [CrossRef]
- Leitch, S.; Sciberras, E.; Post, B.; Gerner, B.; Rinehart, N.; Nicholson, J.M.; Evans, S. Experience of stress in parents of children with ADHD: A qualitative study. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1690091. [Google Scholar] [CrossRef]
- Clark, L.A.; Cuthbert, B.; Lewis-Fernandez, R.; Narrow, W.E.; Reed, G.M. Three approaches to understanding and classifying mental disorder: ICD-11, DSM-5, and the national institute of mental health’s research domain criteria (RDoC). Psychol. Sci. Public Interest 2017, 18, 72–145. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Khoury, B.; Langer, E.J.; Pagnini, F. The DSM: Mindful science or mindless power? A critical review. Front. Psychol. 2014, 5, 602. [Google Scholar] [CrossRef]
- Van Ewijk, H.; Noordermeer, S.D.S.; Heslenfeld, D.J.; Luman, M.; Hartman, C.A.; Hoekstra, P.J.; Faraone, S.V.; Franke, B.; Buitelaar, J.K.; Oosterlaan, J. The influence of comorbid oppositional defiant disorder on white matter microstructure in attention-deficit/hyperactivity disorder. Eur. Child Adolesc. Psychiatry 2016, 25, 701–710. [Google Scholar] [CrossRef]
- Bishop, C.; Mulraney, M.; Rinehart, N.; Sciberras, E. An examination of the association between anxiety and social functioning in youth with ADHD: A systematic review. Psychiatry Res. 2019, 273, 402–421. [Google Scholar] [CrossRef]
- DuPaul, G.J.; Gormley, M.J.; Laracy, S.D. Comorbidity of LD and ADHD: Implications of DSM-5 for Assessment and Treatment. J. Learn. Disabil. 2013, 46, 43–51. [Google Scholar] [CrossRef]
- McDonald, A.C.; Ejesi, K. When Trauma Mimics ADHD. In ADHD in Adolescents: A Comprehensive Guide; Schonwald, A., Ed.; Springer Nature Switzerland: Cham, Switerland, 2020; pp. 171–185. [Google Scholar] [CrossRef]
- Jerome, D.; Jerome, L. Approach to diagnosis and management of childhood attention deficit hyperactivity disorder. Can. Fam. Physician 2020, 66, 732–736. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7571664/pdf/0660732.pdf (accessed on 7 April 2021).
- Belanger, S.A. Canadian paediatric society clinical practice recommendations for children and adolescents with attention-deficit hyperactivity disorder. Paediatr. Child Health 2018, 23, 431–432. [Google Scholar] [CrossRef]
- Canadian ADHD Resource Alliance. Canadian ADHD Practice Guidelines, 4.1 Edition. 2020. Available online: https://www.caddra.ca/download-guidelines/ (accessed on 11 April 2021).
- Efron, D.; Bryson, H.; Sciberras, E. Children referred for evaluation for ADHD: Comorbidity profiles and characteristics with a positive diagnosis. Child Care Health Dev. 2016, 42, 718–724. [Google Scholar] [CrossRef]
- Luo, Y.; Weibman, D.; Halperin, J.M.; Li, X. A review of heterogeneity in Attention Deficit/Hyperactivity Disorder (ADHD). Front. Hum. Neurosci. 2019, 13, 42. [Google Scholar] [CrossRef]
- Reale, L.; Bartoli, B.; Cartabia, M.; Zanetti, M.; Costantino, M.A.; Canevini, M.P.; Termine, C.; Bonati, M. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur. Child Adolesc. Psychiatry 2017, 26, 1443–1457. [Google Scholar] [CrossRef]
- American Psychiatric Association. DSM-5 Handbook of Differential Diagnosis; American Psychiatric Association Publishing: Washington, DC, USA, 2014. [Google Scholar] [CrossRef]
- Amer, Y.S.; Al-Joudi, H.F.; Varnham, J.L.; Bashiri, F.A.; Hamad, M.H.; Al Salehi, S.M.; Daghash, H.F.; Albatti, T.H.; Saudi ADHD Society. Appraisal of clinical practice guidelines for the management of attention deficit hyperactivity disorder (ADHD) using the AGREE II Instrument: A systematic review. PLoS ONE 2019, 14, e0219239. [Google Scholar] [CrossRef]
- Andrade, B.F.; Courtney, D.; Duda, S.; Aitken, M.; Craig, S.G.; Szatmari, P.; Henderson, J.; Bennett, K. A systematic review and evaluation of clinical practice guidelines for children and youth with disruptive behavior: Rigor of development and recommendations for use. Clin. Child Fam. Psychol. Rev. 2019, 22, 527–548. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The, P.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Pattison, E.; Ure, A.; Mittiga, S.R.; Williams, K.; Freeman, N.F. The feedback session of an autism assessment: A scoping review or clinical practice guideline recommendations. J. Autism Dev. Disord. 2022, 52, 1821–1840. [Google Scholar] [CrossRef]
- NHMRC. Guidelines for Guidelines: Guideline Development Group. 2019. Available online: https://www.nhmrc.gov.au/guidelinesforguidelines/plan/guideline-development-group (accessed on 20 January 2021).
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, version 6.3. Cochrane; Cochrane: London, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 8 June 2022).
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E.; et al. AGREE II: Advancing guideline development, reporting and evaluation in health care. Can. Med. Assoc. J. 2010, 182, E839–E842. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia, Malaysian Psychiatric Association, Academy of Medicine Malaysia. Management of Attention-Deficit Hyperactivity Disorder in Children and Adolescents (Second Edition). 2020. Available online: https://www2.moh.gov.my/moh/resources/MainBanner/2020/Draft_CPG_ADHD_for_Reviewer.pdf (accessed on 21 January 2021).
- Ministry of Health Singapore. Attention Deficit Hyperactivity Disorder, AMS-HOM Clinical Practice Guidelines 1/2014. 2014. Available online: https://www.moh.gov.sg/docs/librariesprovider4/guidelines/adhd-cpg_booklet.pdf (accessed on 21 January 2021).
- National Institute for Health and Clinical Excellence. Attention Deficit Hyperactivity Disorder: Diagnosis and Management. 2018. Available online: https://www.nice.org.uk/guidance/ng87/resources/attention-deficit-hyperactivity-disorder-diagnosis-and-management-pdf-1837699732933 (accessed on 18 January 2021).
- Wolraich, M.L.; Hagan, J.F.; Allan, C.; Chan, E.; Davison, D.; Earls, M.; Evans, S.W.; Flinn, S.K.; Froehlich, T.; Frost, J.; et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 2019, 144, e20192528. [Google Scholar] [CrossRef]
- Barbaresi, W.J.; Campbell, L.; Diekroger, E.A.; Froehlich, T.E.; Liu, Y.H.; O’Malley, E.; Pelham, W.E.; Power, T.J.; Zinner, S.H.; Chan, E. Society for developmental and behavioural pediatrics clinical practice guideline for the assessment and treatment of children and adolescents with complex attention-deficit/hyperactivity disorder. J. Dev. Behav. Pediatr. 2020, 41, 35–57. [Google Scholar] [CrossRef]
- Hohmann, E.; Cote, M.P.; Brand, J.C. Research pearls: Expert consensus based evidence using the Delphi method. Anthroscopy 2018, 34, 3278–3282. [Google Scholar] [CrossRef]
- National Institute for Health and Clinical Excellence. Attention Deficit Hyperactivity Disorder: Diagnosis and Management. 2008. Available online: https://www.nice.org.uk/guidance/cg72 (accessed on 11 September 2021).
- Zand, D.; Diekroger, E.; Koolwijk, I.; Nolan, R.; Augusteyn, M.; Yang, J.; Buttross, S.; Mehlenbeck, R.; Froehlich, T. Clinical Practice Guidelines for the Assessment and Treatment of Children and Adolescents with Complex Attention-Deficit/Hyperactivity Disorder Executive Summary; Society for Developmental and Behavioural Pediatrics: McLean, VA, USA, 2021; Available online: https://sdbp.org/adhd-guideline/cag-guidelines/ (accessed on 22 July 2021).
- The Royal Children’s Hospital Melbourne. Attention Deficit Hyperactivity Disorder (ADHD). 2021. Available online: https://www.rch.org.au/kidsinfo/fact_sheets/Attention_deficit_hyperactivity_disorder_ADHD/ (accessed on 7 June 2022).
- Jaiswal, S.; Valstar, M.F.; Gillot, A.; Daley, D. Automatic detection of ADHD and ASD from expressive behaviour in RGBD data. In Proceedings of the 2017 IEEE 12th International Conference on Automatic Face and Gesture Recognition, Washington, DC, USA, 30 May–3 June 2017; Available online: https://ieeexplore.ieee.org/stamp/stamp.jsp?tp=&arnumber=7961818 (accessed on 19 October 2022).
- Barkley, R.A.; Eme, R. Is neuropscyhological testing useful for any reason in the evaluation of ADHD? ADHD Rep. 2019, 27, 1–8. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Clinical Practice Points on the Diagnosis, Assessment and Management of Attention Deficit Hyperactivity Disorder in Children and Adolescents. 2012. Available online: https://www.nhmrc.gov.au/sites/default/files/images/clinical-practice-points-diagnosis-assessment.pdf (accessed on 22 September 2020).
- Doernberg, E.; Hollander, E. Neurodevelopmental disorders (ASD and ADHD): DSM-5, ICD-10, and ICD-11. CNS Spectr. 2016, 21, 295–299. [Google Scholar] [CrossRef]
- Australian ADHD Professionals Association. Australian Evidence-Based Clinical Practice Guideline for Attention Deficit Hyperactivity Disorder (ADHD). 2022. Available online: https://aadpa.com.au/guideline/ (accessed on 19 October 2022).
- Adams, J.; Hillier-Brown, F.C.; Moore, H.J.; Lake, A.A.; Araujo-Soares, V.; White, M.; Summerbell, C. Searching and synthesising ‘grey literature’ and ‘grey information’ in public health: Critical reflections on three case studies. Syst. Rev. 2016, 5, 164. [Google Scholar] [CrossRef]
- National Health System. Attention Deficit Hyperactivity Disorder (ADHD). 2021. Available online: https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/diagnosis/ (accessed on 8 June 2022).
- Barnes, G.L.; Wretham, A.E.; Sedgwick, R.; Boon, G.; Cheesman, K.; Moghraby, O. Evaluation of a diagnostic ADHD pathway in a community child mental health service in South London. Ment. Health Rev. J. 2020, 25, 1–19. [Google Scholar] [CrossRef]
- Australian Institute of Family Studies. Diagnosis in Child Mental Health. 2018. Available online: https://aifs.gov.au/resources/policy-and-practice-papers/diagnosis-child-mental-health (accessed on 8 June 2022).
- American Psychological Association. Evidence-based practice in psychology. Am. Psychol. 2006, 61, 271–285. [Google Scholar] [CrossRef]
| Concept 1: ADHD | Concept 2: Guideline | Concept 3: School Aged Children |
|---|---|---|
| ADHD | child * | |
| Attention deficit disorder | guideline * | youth * |
| Hyperactivity disorder | Guidance | adolescen * |
| hperactiv * | clinical practice | young people |
| overactiv * | recommendation * | teen * |
| hyperkinetic disorder | school age |
| Organisation (Short Name) | Title | Year of Publication | Country of Origin | Guideline Development Group/Profession |
|---|---|---|---|---|
| AAP | Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents | 2019 | United States of America | Professional association |
| AMS-MOH | AMS-MOH Clinical Practice Guidelines 1/2014 | 2014 | Singapore | Government |
| CADDRA | Canadian ADHD Resource Alliance: Canadian ADHD Practice Guidelines | 2020 | Canada | Professional association |
| MOH/PAK | Management of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents (Second Edition) | 2020 | Malaysia | Government |
| NICE | Attention deficit hyperactivity disorder: diagnosis and management (NG87) | 2018 (Last updated 2019) | United Kingdom | Professional association |
| SDBP | Society for Developmental and Behavioral Pediatrics Clinical Practice Guideline for the Assessment and Treatment of Children and Adolescents with Complex Attention-Deficit/Hyperactivity Disorder | 2020 | United States of America | Professional association |
| Guideline | Domain 1: Scope and Purpose | Domain 2: Stake Holder Involvement | Domain 3: Rigour of Development | Domain 4: Clarity and Presentation | Domain 5: Applicability | Domain 6: Editorial | Overall Assessment | Recommendation |
|---|---|---|---|---|---|---|---|---|
| AAP (2019) | 95 | 83 | 86 | 100 | 63 | 93 | 93 | Strongly Recommend * |
| AMS-MOH (2014) | 98 | 74 | 57 | 98 | 63 | 14 | 71 | Strongly Recommend |
| CADDRA (2020) | 83 | 71 | 33 | 62 | 38 | 71 | 62 | Strongly Recommend |
| MOH/PAK (2020) | 100 | 76 | 74 | 88 | 63 | 57 | 86 | Strongly Recommend |
| NICE (2018) | 95 | 100 | 87 | 80 | 64 | 57 | 86 | Strongly Recommend |
| SDBP (2020) | 100 | 64 | 57 | 98 | 64 | 46 | 86 | Strongly Recommend |
| Guideline | Page Number/s | Recommendations for ADHD Assessment (Level of Evidence) |
|---|---|---|
| CADDRA (2020) | 1–32 | “The clinical interview and evaluation continues to be the mainstay of ADHD diagnosis”. (Literature Review) “Although rating scales are not sufficient to diagnose ADHD … their use to enrich the process of evaluation is widely recommended”. (Single reference) “Psychoeducational evaluations are frequently recommended, these are most useful in situations of diagnostic uncertainty”. (Single reference) Step 1: Information gathering Step 2: Medical review “Exclude any medical causes that can mimic or aggravate ADHD signs or symptoms”. “Review nutrition and lifestyle habits”. “Evaluate potential contraindications to ADHD medications”. Step 3: ADHD specific interview “Discuss patient’s strengths and observe patient during interview”. “Review developmental history and obtain collateral information from parents/caregivers”. “Review the questionnaires used in assessment”. “Consider contributions of other psychiatric, psychosocial factors or learning disorder to the presenting symptoms [see pages 14–32 for further information about differential and co-occurring diagnosis]. Consider specialist referral if necessary”. A flow chart with more detailed information regarding steps 1–3 can be found on pages 7–12 of the guideline. |
| Guideline | Page Number/s | Differential Diagnosis Recommendations (Level of Evidence) | Co-occurring Diagnosis Recommendations (Level of Evidence) |
|---|---|---|---|
| AAP (2019) | 5 | “Rule out any alternative cause” (Grade B, strong recommendation) a Refer to a clinical child psychologist or mental health professional if a distinction cannot be made between ADHD and other mental health disorders | “Screen for comorbid conditions, including emotional or behavioral conditions (e.g., anxiety, depression, oppositional defiant disorder, conduct disorders, substance use), developmental conditions (e.g., learning and language disorders, autism spectrum disorders), and physical conditions (e.g., tics, sleep apnea)” (Grade B, strong recommendation) a |
| AMS-MOH (2014) | 10–15 | “Before diagnosing attention deficit hyperactivity disorder (ADHD), a careful evaluation to exclude psychiatric or medical conditions which can account for ADHD-like symptoms should be performed” (Grade B, Level 2++) a | “Assess a child diagnosed with attention deficit hyperactivity disorder for co-morbid conditions” (Grade C, Level 2+) a |
| CADDRA (2020) | Multiple | “A careful assessment of other possible diagnoses should be undertaken at the time of evaluation” b “A thorough history and full functional review accompanied by a physical examination may highlight underlying physical conditions” b “Psychological testing may be required to address a suspected learning disability or other cognitive challenges” b Details of potential differential conditions, each with a list of overlapping and distinguishing features can be found on page 14–32 of the guideline. c | “An evaluation for ADHD requires screening for possible comorbid disorders and consideration of biological, social, and psychological factors. Consideration of a second opinion or referral to an ADHD specialist should be made if the patient has a clinical history that is complex” b Details of potential co-occurring conditions, each with a list of overlapping and distinguishing features can be found on page 14–32 of the guideline. c |
| MOH/P/PAK (2020) | 3–5 | “A comprehensive physical examination (including vital signs, height and weight) should be performed to exclude physical conditions which mimic ADHD” (Level of evidence based on expert committees, consensus, and case reports) a | “Children with ADHD should be evaluated for co-morbidities” b |
| NICE (2019) | 11–12 | No recommendation provided | “Include an assessment of … coexisting conditions, social, familial and educational or occupational circumstances and physical health. For children and young people, there should also be an assessment of their parents’ or carers’ mental health” b |
| SDBP (2020) | 41–43 | “If ADHD is not confirmed, consideration should be given to other conditions that may present with symptoms similar to ADHD. Identification of these other conditions may require psychological testing, mental health assessment … [or] neuropsychological testing” b1 | “The clinician should … assess for coexisting conditions”. (Grade B) a “ADHD symptoms cannot be evaluated in these children [with an ID, LDs, or ASD] without data from formal cognitive/developmental testing and, in the school-age child, academic achievement testing and assessment of classroom functioning” c “When diagnostic uncertainty remains … children with ADHD should be referred by their primary care clinician for comprehensive assessment” c |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Power, C.; Freeman, N.C.; Costello, S. ADHD Assessment Recommendations for Children in Practice Guidelines: A Systematic Review. Psych 2022, 4, 882-896. https://doi.org/10.3390/psych4040065
Power C, Freeman NC, Costello S. ADHD Assessment Recommendations for Children in Practice Guidelines: A Systematic Review. Psych. 2022; 4(4):882-896. https://doi.org/10.3390/psych4040065
Chicago/Turabian StylePower, Caroline, Nerelie C. Freeman, and Shane Costello. 2022. "ADHD Assessment Recommendations for Children in Practice Guidelines: A Systematic Review" Psych 4, no. 4: 882-896. https://doi.org/10.3390/psych4040065
APA StylePower, C., Freeman, N. C., & Costello, S. (2022). ADHD Assessment Recommendations for Children in Practice Guidelines: A Systematic Review. Psych, 4(4), 882-896. https://doi.org/10.3390/psych4040065






