Subjective Happiness and Sleep in University Students with High Myopia
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethical Approval
2.2. Questionnaires
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Verkicharla, P.K.; Ohno-Matsui, K.; Saw, S.M. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol. Opt. 2015, 35, 465–475. [Google Scholar] [CrossRef]
- Rudnicka, A.R.; Kapetanakis, V.V.; Wathern, A.K.; Logan, N.S.; Gilmartin, B.; Whincup, P.H.; Cook, D.G.; Owen, C.G. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: Implications for aetiology and early prevention. Br. J. Ophthalmol. 2016, 100, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Marcus, M.W.; de Vries, M.M.; Junoy Montolio, F.G.; Jansonius, N.M. Myopia as a risk factor for open-angle glaucoma: A systematic review and meta-analysis. Ophthalmology 2011, 118, 1989–1994.e2. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.S.; Teo, K.; Cheung, C.M. Epidemiology and Diagnosis of Myopic Choroidal Neovascularization in Asia. Eye Contact Lens 2016, 42, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Crim, N.; Esposito, E.; Monti, R.; Correa, L.J.; Serra, H.M.; Urrets-Zavalia, J.A. Myopia as a risk factor for subsequent retinal tears in the course of a symptomatic posterior vitreous detachment. BMC Ophthalmol. 2017, 17, 226. [Google Scholar] [CrossRef] [PubMed]
- Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Parental Myopia, Near Work, School Achievement, and Children’s Refractive Error. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3633–3640. [Google Scholar]
- Lim, D.H.; Han, J.; Chung, T.Y.; Kang, S.; Yim, H.W.; Epidemiologic Survey Committee of the Korean Ophthalmologic Society. The high prevalence of myopia in Korean children with influence of parental refractive errors: The 2008–2012 Korean National Health and Nutrition Examination Survey. PLoS ONE 2018, 13, e0207690. [Google Scholar]
- Xiong, S.; Sankaridurg, P.; Naduvilath, T.; Zang, J.; Zou, H.; Zhu, J.; Lv, M.; He, X.; Xu, X. Time spent in outdoor activities in relation to myopia prevention and control: A meta-analysis and systematic review. Acta Ophthalmol. 2017, 95, 551–566. [Google Scholar] [CrossRef]
- Torii, H.; Ohnuma, K.; Kurihara, T.; Tsubota, K.; Negishi, K. Violet Light Transmission is Related to Myopia Progression in Adult High Myopia. Sci. Rep. 2017, 7, 14523. [Google Scholar] [CrossRef]
- Hua, W.J.; Jin, J.X.; Wu, X.Y.; Yang, J.W.; Jiang, X.; Gao, G.P.; Tao, F.B. Elevated light levels in schools have a protective effect on myopia. Ophthalmic Physiol. Opt. 2015, 35, 252–262. [Google Scholar] [CrossRef]
- Norton, T.T.; Siegwart, J.T., Jr. Light levels, refractive development, and myopia--a speculative review. Exp. Eye Res. 2013, 114, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Aetiology and prevention. Prog. Retin. Eye Res. 2018, 62, 134–149. [Google Scholar] [CrossRef]
- Kandel, H.; Khadka, J.; Shrestha, M.K.; Sharma, S.; Neupane Kandel, S.; Dhungana, P.; Pradhan, K.; Nepal, B.P.; Thapa, S.; Pesudovs, K. Uncorrected and corrected refractive error experiences of Nepalese adults: A qualitative study. Ophthalmic Epidemiol. 2018, 25, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Ziaei, H.; Katibeh, M.; Sabbaghi, M.; Yaseri, M.; Eskandari, A. Vision Related Quality of Life in Myopia; Photorefractive Keratectomy versus Nonsurgical Optical Correction. J. Ophthalmic Vis. Res. 2012, 7, 219–224. [Google Scholar] [PubMed]
- Meidani, A.; Tzavara, C.; Dimitrakaki, C.; Pesudovs, K.; Tountas, Y. Femtosecond laser-assisted LASIK improves quality of life. J. Refract. Surg. 2012, 28, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cambrodí, R.J.; Blanes-Mompó, F.J.; García-Lázaro, S.; Piñero, D.P.; Cerviño, A.; Brautaset, R. Visual and optical performance and quality of life after implantation of posterior chamber phakic intraocular lens. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Matsuguma, S.; Negishi, K.; Kawashima, M.; Toda, I.; Ayaki, M.; Tsubota, K. Patients’ satisfaction and subjective happiness after refractive surgery for myopia. Patient Prefer. Adherence 2018, 12, 1901–1906. [Google Scholar] [CrossRef]
- Wong, H.B.; Machin, D.; Tan, S.B.; Wong, T.Y.; Saw, S.M. Visual impairment and its impact on health-related quality of life in adolescents. Am. J. Ophthalmol. 2009, 147, 505–511.e1. [Google Scholar] [CrossRef]
- Morse, J.S.; Schallhorn, S.C.; Hettinger, K.; Tanzer, D. Role of depressive symptoms in patient satisfaction with visual quality after laser in situ keratomileusis. J. Cataract Refract. Surg. 2009, 35, 341–346. [Google Scholar] [CrossRef]
- Lazon de la Jara, P.; Erickson, D.; Erickson, P.; Stapleton, F. Visual and non-visual factors associated with patient satisfaction and quality of life in LASIK. Eye 2011, 25, 1194–1201. [Google Scholar] [CrossRef]
- de la Jara, P.L.; Erickson, D.; Erickson, P.; Stapleton, F. Pre-operative Quality of Life and psychological factors that influence patient decision making in LASIK. Eye 2010, 24, 270–275. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garamendi, E.; Pesudovs, K.; Elliott, D.B. Changes in quality of life after laser in situ keratomileusis for myopia. J. Cataract Refract. Surg. 2005, 31, 1537–1543. [Google Scholar] [CrossRef] [PubMed]
- Takashima, T.; Yokoyama, T.; Futagami, S.; Ohno-Matsui, K.; Tanaka, H.; Tokoro, T.; Mochizuki, M. The quality of life in patients with pathologic myopia. Jpn. J. Ophthalmol. 2001, 45, 84–92. [Google Scholar] [CrossRef]
- Wu, Y.; Ma, Q.; Sun, H.P.; Xu, Y.; Niu, M.E.; Pan, C.W. Myopia and depressive symptoms among older Chinese adults. PLoS ONE 2017, 12, e0177613. [Google Scholar] [CrossRef]
- Jee, D.; Morgan, I.G.; Kim, E.C. Inverse relationship between sleep duration and myopia. Acta Ophthalmol. 2016, 94, e204–e210. [Google Scholar] [CrossRef]
- Ayaki, M.; Torii, H.; Tsubota, K.; Negishi, K. Decreased sleep quality in high myopia children. Sci. Rep. 2016, 6, 33902. [Google Scholar] [CrossRef]
- Kearney, S.; O’Donoghue, L.; Pourshahidi, L.K.; Cobice, D.; Saunders, K.J. Myopes have significantly higher serum melatonin concentrations than non-myopes. Ophthalmic Physiol. Opt. 2017, 37, 557–567. [Google Scholar] [CrossRef]
- Chen, J.C.; Brown, B.; Schmid, K.L. Delayed mfERG responses in myopia. Vis. Res. 2006, 46, 1221–1229. [Google Scholar] [CrossRef]
- Ho, W.; Kee, C.; Chan, H.H. Myopia progression in children is linked with reduced foveal mfERG response. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5320–5325. [Google Scholar] [CrossRef][Green Version]
- Gracitelli, C.P.; Duque-Chica, G.L.; Roizenblatt, M.; de Araújo Moura, A.L.; Nagy, B.V.; de Melo, G.R.; Borba, P.D.; Teixeira, S.H.; Tufik, S.; Ventura, D.F.; et al. Intrinsically photosensitive retinal ganglion cell activity is associated with decreased sleep quality in patients with glaucoma. Ophthalmology 2015, 122, 1139–1148. [Google Scholar] [CrossRef]
- Ayaki, M.; Shiba, D.; Negishi, K.; Tsubota, K. Depressed visual field and mood are associated with sleep disorder in glaucoma patients. Sci. Rep. 2016, 6, 25699. [Google Scholar] [CrossRef] [PubMed]
- Drouyer, E.; Dkhissi-Benyahya, O.; Chiquet, C.; WoldeMussie, E.; Ruiz, G.; Wheeler, L.A.; Denis, P.; Cooper, H.M. Glaucoma alters the circadian timing system. PLoS ONE 2008, 3, e3931. [Google Scholar] [CrossRef] [PubMed]
- Sloane, P.D.; Figueiro, M.; Cohen, L. Light as Therapy for Sleep Disorders and Depression in Older Adults. Clin. Geriatr. 2008, 16, 25–31. [Google Scholar] [PubMed]
- Fernandez, D.C.; Fogerson, P.M.; Lazzerini Ospri, L.; Thomsen, M.B.; Layne, R.M.; Severin, D.; Zhan, J.; Singer, J.H.; Kirkwood, A.; Zhao, H.; et al. Light Affects Mood and Learning through Distinct Retina-Brain Pathways. Cell 2018, 175, 71–84.e18. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Morgan, I.G.; Chen, Q.; Jin, L.; He, M.; Congdon, N. Disordered sleep and myopia risk among Chinese children. PLoS ONE 2015, 10, e0121796. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.W.; Liu, J.H.; Wu, R.K.; Zhong, H.; Li, J. Disordered sleep and myopia among adolescents: A propensity score matching analysis. Ophthalmic Epidemiol. 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Nakade, M.; Takeuchi, H.; Kurotani, M.; Harada, T. Effects of meal habits and alcohol/cigarette consumption on morningness-eveningness preference and sleep habits by Japanese female students aged 18–29. J. Physiol. Anthropol. 2009, 28, 83–90. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Lyubomirsky, S.; Lepper, H.S. A measure of subjective happiness: Preliminary reliability and construct validation. Soc. Indic. Res. 1999, 46, 137–155. [Google Scholar] [CrossRef]
- Mattei, D.; Schaefer, C.E. An investigation of validity of the subjective happiness scale. Psychol. Rep. 2004, 94, 288–290. [Google Scholar] [CrossRef]
- Shimai, S.; Otake, K.; Utsuki, N.; Ikemi, A.; Lyubomirsky, S. Development of a Japanese version of the Subjective Happiness Scale (SHS), and examination of its validity and reliability. Nihon Koshu Eisei Zasshi 2004, 51, 845–853. [Google Scholar] [PubMed]
- Gulati, A.; Sullivan, R.; Buring, J.E.; Sullivan, D.A.; Dana, R.; Schaumberg, D.A. Validation and repeatability of a short questionnaire for dry eye syndrome. Am. J. Ophthalmol. 2006, 142, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Potrebny, T.; Wiium, N.; Lundegard, M.M. Temporal trends in adolescents’ self-reported psychosomatic health complaints from 1980–2016: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0188374. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.J.; Acebo, C.; Carskadon, M.A. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007, 8, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Carskadon, M.A. Sleep in adolescents: The perfect storm. Pediatr. Clin. N. Am. 2011, 58, 637–647. [Google Scholar] [CrossRef] [PubMed]
- Carskadon, M.A. Maturation of Processes Regulating Sleep in Adolescents. Sleep in Children: Developmental Changes in Sleep Patterns; Marcus, C.L., Carroll, J.L., Donnelly, D.F., Loughlin, G.M., Eds.; Informa Healthcare USA, Inc.: New York, NY, USA, 2008; pp. 95–114. [Google Scholar]
- Crowley, S.J.; van Reen, E.; LeBourgeois, M.K.; Acebo, C.; Tarokh, L.; Seifer, R.; Barker, D.H.; Carskadon, M.A. A longitudinal assessment of sleep timing, circadian phase, and phase angle of entrainment across human adolescence. PLoS ONE 2014, 9, e112199. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Chen, S.C. Effects of an irregular bedtime schedule on sleep quality, daytime sleepness, and fatigue among university students in Taiwan. BMC Public Health 2009, 19, 248. [Google Scholar] [CrossRef]
- Kawashima, M.; Uchino, M.; Yokoi, N.; Uchino, Y.; Dogru, M.; Komuro, A.; Sonomura, Y.; Kato, H.; Kinoshita, S.; Mimura, M.; et al. Associations between subjective happiness and dry eye disease: A new perspective from the Osaka study. PLoS ONE 2015, 10, e0123299. [Google Scholar] [CrossRef] [PubMed]
- Adigun, O.T. Self-esteem, self-efficacy, self-concept and intimate image diffusion among deaf adolescents: A structural equation model analysis. Heliyon 2020, 6, e04742. [Google Scholar] [CrossRef] [PubMed]
| High Myopia | Mild Myopia | No Myopia | p-Value (High vs. Mild Myopia) | p-Value (High vs. No Myopia) | |
|---|---|---|---|---|---|
| # of participants | 44 | 86 | 23 | ||
| Age (y) | 21.1 ± 0.1 | 20.7 ± 1.8 | 21.4 ± 1.3 | 0.129 | 0.266 |
| % male | 61.4 | 58.1 | 78.3 | 0.723 | 0.162 |
| Myopic error (D) | −6.62 ± 1.55 | −3.33 ± 1.05 | −0.01 ± 0.06 | <0.001 * | <0.001 * |
| Number of dry eye symptoms | 0.91 ± 0.86 | 0.70 ± 0.75 | 0.48 ± 0.73 | 0.170 | 0.036 * |
| Neuropsychiatric indices | |||||
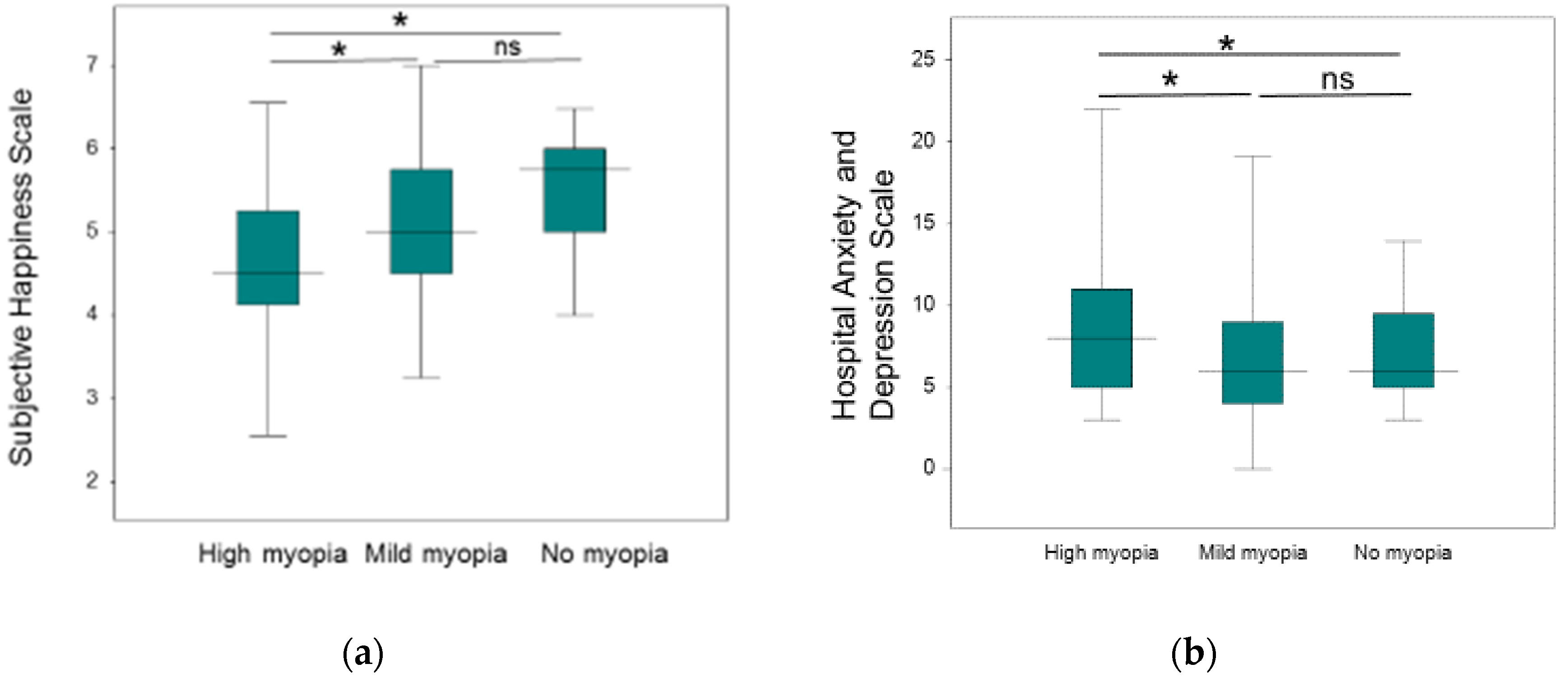
| SHS score | 4.61 ± 0.94 | 5.09 ± 0.91 | 5.49 ± 0.75 | 0.001 * | <0.001 * |
| HADS score | 9.23 ± 4.92 | 7.09 ± 4.83 | 7.39 ± 3.33 | 0.021 * | 0.032 * |
| Anxiety subscore | 4.98 ± 2.68 | 3.76 ± 2.96 | 4.04 ± 1.89 | 0.020 * | 0.104 |
| Depression subscore | 4.25 ± 2.80 | 3.34 ± 2.81 | 3.35 ± 2.01 | 0.082 | 0.135 |
| PSQI global score | 4.80 ± 2.40 | 4.44 ± 2.25 | 4.48 ± 2.17 | 0.419 | 0.587 |
| morningness/eveningness score | 2.34 ± 1.72 | 3.21 ± 2.05 | 3.48 ± 2.11 | 0.012 * | 0.032 * |
| Sleep parameters | |||||
| Bedtime (h:m) | 0:50 ± 0:52 | 0:31 ± 0:53 | 0:38 ± 0:53 | 0.061 | 0.355 |
| Wake-up time (h:m) | 8:17 ± 1:18 | 7:40 ± 1:21 | 8:08 ± 1:28 | 0.013 * | 0.672 |
| Sleep duration (h:m) | 7:06 ± 1:04 | 6:42 ± 1:06 | 6:55 ± 0:47 | 0.125 | 0.658 |
| Sleep latency (h:m) | 0:19 ± 0:20 | 0:17±0:15 | 0:17 ± 0:14 | 0.711 | 0.626 |
| Sleep efficacy (%) | 93.7 ± 8.3 | 94.4 ± 7.6 | 92.4 ± 7.9 | 0.786 | 0.450 |
| Subjective sleep quality score | 0.98 ± 0.63 | 1.01 ± 0.54 | 1.09 ± 0.67 | 0.758 | 0.519 |
| Sleep difficulty score | 0.57 ± 0.50 | 0.53 ± 0.50 | 0.70 ± 0.56 | 0.721 | 0.364 |
| Daytime dysfunction score | 1.09 ± 0.88 | 0.83 ± 0.81 | 0.61 ± 0.78 | 0.100 | 0.026 * |
| Myopia-related parameters | |||||
| Positive family history of myopia (%) A | 88.6 | 86.0 | 65.2 | 0.678 | 0.021 * |
| Screen time on portable phone (h:m/day) | 3:05 ± 1.31 | 2:47 ± 1:53 | 2:29 ± 1:26 | 0.334 | 0.102 |
| Screen time on computer display (h:m/day) | 1:05 ± 1:49 | 0:59 ± 0:11 | 0:55 ± 0:49 | 0.739 | 0.603 |
| Distance from display (cm) | 29.9 ± 10.0 | 28.1 ± 10.3 | 30.5 ± 11.4 | 0.407 | 0.835 |
| Linear Regression | Adjusted for Age and Sex | |||
|---|---|---|---|---|
| β | p-Value | β | p-Value | |
| Age | −0.098 (0.010) | 0.263 | ||
| Sex A | 0.008 (<0.001) | 0.919 | ||
| Model 1: Neuropsychiatric indices | ||||
| SHS | 0.247 (0.061) | 0.005 * | 0.263 (0.069) | 0.003 * |
| HADS | −0.155 (0.024) | 0.078 | −0.153 (0.023) | 0.083 |
| Anxiety | −0.138 (0.019) | 0.117 | −0.145(0.021) | 0.099 |
| Depression | −0.129 (0.017) | 0.143 | −0.122 (0.015) | 0.178 |
| PSQI | −0.022 (<0.001) | 0.797 | −0.029 (<0.001) | 0.740 |
| MES | 0.177 (0.031) | 0.043 * | 0.193 (0.037) | 0.031 * |
| Model 2: Sleep parameters | ||||
| Bedtime | −0.208 (0.043) | 0.017 * | −0.206 (0.042) | 0.019 * |
| Wake-up time | −0.185 (0.034) | 0.034 * | −0.200 (0.040) | 0.024 * |
| Sleep duration | −0.111 (0.012) | 0.207 | −0.123 (0.015) | 0.164 |
| Sleep latency | −0.002 (<0.001) | 0.981 | −0.016 (<0.001) | 0.858 |
| Sleep efficacy | −0.006 (<0.001) | 0.948 | 0.003 (<0.001) | 0.970 |
| Subjective sleep quality score | 0.049 (<0.001) | 0.575 | 0.046 (<0.001) | 0.606 |
| Daytime dysfunction score | −0.116 (0.013) | 0.181 | −0.131 (0.017) | 0.141 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iehisa, I.; Negishi, K.; Sakamoto, R.; Torii, H.; Ayaki, M.; Tsubota, K. Subjective Happiness and Sleep in University Students with High Myopia. Psych 2020, 2, 279-286. https://doi.org/10.3390/psych2040021
Iehisa I, Negishi K, Sakamoto R, Torii H, Ayaki M, Tsubota K. Subjective Happiness and Sleep in University Students with High Myopia. Psych. 2020; 2(4):279-286. https://doi.org/10.3390/psych2040021
Chicago/Turabian StyleIehisa, Ikko, Kazuno Negishi, Reiko Sakamoto, Hidemasa Torii, Masahiko Ayaki, and Kazuo Tsubota. 2020. "Subjective Happiness and Sleep in University Students with High Myopia" Psych 2, no. 4: 279-286. https://doi.org/10.3390/psych2040021
APA StyleIehisa, I., Negishi, K., Sakamoto, R., Torii, H., Ayaki, M., & Tsubota, K. (2020). Subjective Happiness and Sleep in University Students with High Myopia. Psych, 2(4), 279-286. https://doi.org/10.3390/psych2040021






