Abstract
Home care and telemedicine are crucial for physical and mental health. Although there is a lot of information on these topics, it is scattered across various sources, making it difficult to identify key contributions and authors. This study conducts a scientometric analysis to consolidate the most relevant information. The methodology is divided into two parts: first, a scientometric mapping that analyzes scientific production by country, journal, and author; second, the identification of prominent contributions using the Tree of Science (ToS) tool. The goal is to identify trends and support decision-making in the health sector by providing guidelines based on the most relevant research.
1. Introduction
According to the World Health Organization (WHO), homecare and telemedicine consist of bringing medical services home in cases where there are difficulties for patients to be transferred to hospitals and medical clinics [1]. Some of the factors that may require care at home are long distances, transportation difficulties in some territories, overcrowding and insufficient resources in hospital centers, and the risk involved in moving high-risk patients from one place to another for their medical treatments. Home care should be part of the integral and permanent health services that must be provided to patients in their homes. These services aim to improve, maintain, or care for the health of human beings in such a way that patients can preserve their independence and reduce the negative impact of the disease. Within home care, services such as promotion, prevention, cure, and rehabilitation can be included [2]. On the other hand, telehealth requires information and communication technologies to transfer medical information for the delivery of clinical and educational services. It attempts to overcome the challenges of healthcare delivery due to time, distance, and difficult terrain, enabling cost-effectiveness and better access in both developed and developing world settings [3]. Pacis et al. [4] expressed the need to incorporate new technologies into medicine. They classified the use of these new technologies into four groups: patient monitoring, healthcare information technology, intelligent assistance diagnostics, and information analysis collaboration. Thus, telemedicine includes various applications and services delivered through telephone lines, two-way video, e-mail, smart phones, wireless devices, and other forms of telecommunication technologies. In addition, telemedicine is successfully used in a wide range of medical specialties [5]. In recent years, there has been increasing interest in the development of precision medicine, telehealth, and telemedicine approaches that focus on the prevention and treatment of various pathologies. Such is the case of cardiovascular medicine, in which telemedicine is applied to all stages of disease development and is defined as telecardiology [6].
Currently, telemedicine is used in patients with heart failure to monitor the daily curves of body weight, blood pressure, O2 saturation, heart rate/heart rhythm of patients, and the direct or indirect invasive reassessment of left atrial pressure as a turning point for therapy adjustment. Similarly, in patients with systemic hypertension, who need diagnosis, follow-up, and adjustment of therapy, ambulatory blood pressure monitoring is performed. Also, to support diagnosis in patients with arrhythmia including emergency calls in life-threatening situations such as ventricular tachycardia or debilitating conditions such as atrial fibrillation, ECG monitoring and treatment changes are performed [7]. The development of robotics has contributed not only to patient monitoring but also to advancements in telesurgery. Telesurgery is a process where a surgeon can remotely operate a robot via an Internet connection to perform surgery on a patient in another location. With this technology, the surgeon can obtain real-time images remotely and perform the operation using the corresponding equipment [8].
However, despite advances in the fields of telemedicine, home monitoring, and telehealth worldwide, challenges still arise, which relate to the application and validity of findings and the limited sample sizes in existing telehealth research, the cultural and socioeconomic factors of the population, inadequate infrastructure, insufficient funding, inadequate computer systems, lack of connectivity, and the technical knowledge required for the implementation of these technologies [9].
Then, bearing in mind that it is necessary to continually know the state of research progress in topics as important as homecare using new technologies, the objective of this review is to use scientometric methodologies to identify authors, journals, countries, and trends in this field. To achieve this scientometric review, a keyword search equation was used in the Web of Science (WoS) and Scopus databases. From this search, it is possible to extract the most relevant documents and citations on the subject of homecare and telemedicine. Subsequently, the results obtained from WoS and Scopus were joined into a single database to later apply the Tree of Science (ToS) tool and identify the most relevant contributions over time, using the Tosr R package in this case; finally, a scientometric analysis was carried out to determine statistics and research trends in the field of home care and telemedicine. Undoubtedly, the field of telemedicine and remote patient monitoring has seen exponential growth, particularly in the follow-up of cardio–cerebrovascular diseases. This scientometric review aims to comprehensively explore the role of home monitoring tools in the follow-up of patients with cardio–cerebrovascular diseases in the post-COVID era. Our study focuses on examining current trends, identifying relevant research areas, and assessing the impact of these technologies on crucial aspects such as cardiovascular health management and promotion. In addition to analyzing scientific production in this field, we will focus our study on the practical integration of these tools in specific patient follow-up applications, seeking to understand their tangible impact on the experience and management of these diseases. Finally, our goal is to present a holistic view of the relationship between home monitoring tools and the management of cardio–cerebrovascular diseases in the post-COVID era, highlighting their relevance in the current health landscape. The research question guiding our work is as follows: What are the most prominent trends in scientific research related to home monitoring tools for patients with cardio–cerebrovascular diseases in the post-COVID era? This paper is organized into three sections. Initially, the methodology is presented, which includes a step-by-step explanation of the identification and selection of articles and their corresponding scientometric analysis. Subsequently, in the Results part, the scientometric components are shown and studied, including a documentary analysis, which is distributed according to the analogy of the Tree of Science (ToS)—roots, trunk, and branches—while also presenting an analysis of the most relevant results. Finally, the conclusions of the review are presented.
2. Theoretical Information
2.1. Cardio–Cerebrovascular Diseases: Definition and Characteristics
Cardio–cerebrovascular diseases are a group of disorders that affect the heart and blood vessels, including those supplying blood to the brain. These diseases are characterized by their ability to significantly alter cardiovascular and cerebral function, which can result in acute events such as myocardial infarctions (heart attacks) and cerebrovascular accidents [10]. A key feature of these diseases is their progressive and often silent nature, as they can develop over years without showing obvious symptoms. They are generally associated with damage or deterioration of arteries and veins due to processes such as atherosclerosis, which is the accumulation of cholesterol plaques and other substances on the walls of blood vessels. These diseases can be classified into several types, including the following:
Coronary Artery Disease: Affects the arteries that supply blood to the heart muscle. Examples include angina pectoris and myocardial infarction [11].
Cerebrovascular Disease: Involves disorders that affect cerebral blood flow, such as ischemic and hemorrhagic stroke [12].
Peripheral Vascular Disease: Affects blood vessels outside of the heart and brain [13].
Heart Failure: A condition where the heart does not pump blood efficiently [14]. Symptoms of cardio–cerebrovascular diseases can vary depending on the specific type and severity of the disease. However, some common symptoms include chest pain, difficulty breathing, weakness or numbness on one side of the body, difficulty speaking, and sudden loss of vision. Diagnosis is made through a combination of clinical assessment, imaging studies such as echocardiograms or magnetic resonance imaging, and laboratory tests such as cholesterol analysis and markers of inflammation. The progression of these diseases often follows a course that worsens over time, especially if risk factors such as high blood pressure, high cholesterol, diabetes, smoking, and obesity are not controlled. Early prevention and treatment are key to altering the trajectory of these diseases, including lifestyle changes and, in some cases, medication or surgical interventions.
2.2. Traditional Management of Cardio–Cerebrovascular Diseases
In the field of cardio–cerebrovascular diseases, traditional management focuses on a combination of pharmacological strategies and lifestyle modifications, emphasizing the importance of regular monitoring and addressing various challenges in its implementation. Standard treatments for these diseases often include a variety of medications. Antihypertensives are used to control high blood pressure, a key risk factor for both types of diseases [15]. Statins and other lipid-lowering agents play a crucial role in reducing cholesterol levels and preventing atherosclerosis. Anticoagulants and antiplatelet agents are commonly prescribed to prevent the formation of blood clots, which can lead to serious cardiovascular events. In cases of heart failure, specific medications such as ACE inhibitors and beta-blockers are essential for improving cardiac function.
In addition to pharmacotherapy, managing these diseases involves significant attention to lifestyle changes. Patients are encouraged to adopt a healthy diet, engage in regular exercise, quit smoking, and limit alcohol consumption [16]. These measures not only assist in treatment but are also fundamental in the prevention of these diseases.
Regular monitoring is a cornerstone in managing cardio–cerebrovascular diseases. This process includes periodic visits to the doctor, constant monitoring of blood pressure and cholesterol levels, and, in some cases, imaging tests to assess the progression of the disease. This ongoing monitoring is vital for adjusting treatments to the individual needs of the patient and for early detection of any signs of worsening, which can be crucial in preventing complications.
However, the traditional management of these diseases faces several challenges. One of the most notable is long-term adherence to treatment by patients [17]. The chronic nature of these diseases requires a continuous commitment to medication and lifestyle changes, which can be difficult to maintain for some patients. Additionally, the identification and management of medication side effects, as well as coordination between different specialists in cases of complex diseases, can further complicate treatment.
2.3. Home Monitoring Tools: Technologies and Applications
In the field of cardio–cerebrovascular disease research, home monitoring tools represent a significant advancement, facilitating the ongoing management of these conditions. These technologies, ranging from sensors to mobile apps and telemedicine platforms, have revolutionized the way patients and healthcare professionals interact and manage the treatment and monitoring of these diseases [18]. Home monitoring tools are diversified into several categories:
Health Sensors: These devices can be wearables such as smartwatches and fitness bracelets, which monitor vital parameters such as heart rate, blood pressure, and blood oxygen levels. Some are equipped with advanced capabilities, like arrhythmia detection or sleep monitoring [19].
Mobile Applications: There are numerous apps designed to help patients manage their cardiovascular health. These apps can remind users to take their medications, provide educational information, record and analyze health data, and even allow direct communication with healthcare professionals [20].
Telemedicine Platforms: These systems enable remote interaction between patients and healthcare providers. Through telemedicine, patients can have virtual consultations, share data collected by their monitoring devices, and receive counseling and treatment adjustments without the need for in-person visits [21].
The operation of these tools is based on the collection and analysis of health data in real-time or near real-time. Wearable health sensors continuously gather data on heart rate and blood pressure, providing valuable insights into the patient’s cardiovascular condition in their everyday life. This allows for early detection of potential issues, such as the onset of cardiac arrhythmias or changes in blood pressure. Mobile apps play a crucial role in personal health management [22]. They can help patients follow a medication regimen, monitor their diet and exercise, and keep a record of their symptoms and progress. Additionally, these apps can analyze the collected data and provide useful insights for both the patient and their medical team.
Telemedicine platforms, in turn, extend the reach of healthcare systems to patients in their homes. They facilitate communication and information exchange, which is especially valuable for patients with reduced mobility or those living in remote areas. These tools not only enhance the effectiveness of monitoring and treating cardio–cerebrovascular diseases but also empower patients to manage their health, thus promoting greater adherence to treatments and a healthy lifestyle. However, it is important to consider challenges such as data privacy, the accuracy of devices, and effective integration with existing healthcare systems to maximize their potential.
2.4. Advantages of Home Monitoring in Disease Management
One of the major advantages of home monitoring is the ability to detect subtle changes in a patient’s health that may indicate the development or worsening of a disease. In the case of cardiovascular diseases, regular monitoring of blood pressure and heart rate can alert both patients and doctors to the risk of hypertension or arrhythmias before they become serious issues. This allows for early interventions, such as adjustments in medication or lifestyle changes, which can prevent major complications like heart attacks or strokes. Home monitoring also has a positive impact on the quality of life and autonomy of patients [23]. By being able to actively manage their health in a familiar environment, patients often feel greater control over their illness, which in turn can improve their emotional and psychological well-being. This autonomy is especially valuable for older individuals or those with limited mobility, as it allows them to maintain their independence and reduce their dependence on caregivers or family members.
Another important advantage of home monitoring is the reduction in the need for hospital visits, which in turn can significantly decrease the costs associated with healthcare. By monitoring and effectively managing chronic diseases at home, patients can avoid unnecessary hospitalizations, which not only relieves the burden on health systems but also reduces expenses for patients and their families [24]. Moreover, during health crises such as a pandemic, home monitoring helps minimize the risk of exposure to infections in hospital settings.
2.5. Artificial Intelligence and the Internet of Things
The convergence of Artificial Intelligence (AI) and the Internet of Things (IoT) is revolutionizing the field of remote patient monitoring for cardio–cerebrovascular diseases. These technologies enable continuous and real-time supervision, which is essential for the early detection of adverse events and the optimization of medical therapy. The application of AI in monitoring cardio–cerebrovascular diseases includes machine learning and deep learning algorithms that analyze large volumes of data from multiple sources. These algorithms can identify complex patterns and predict potential risks with increasing accuracy. For example, predictive models can analyze variations in blood pressure, heart rate, and other biomarkers to anticipate episodes such as strokes or heart failures [25]. Additionally, AI plays a crucial role in the customization of treatment. Based on each patient’s medical history and response to treatment, intelligent systems can adjust medication dosages and recommend lifestyle changes to improve cardiovascular health.
On the other hand, IoT provides the necessary infrastructure for the effective deployment of monitoring solutions. Devices such as smartwatches, fitness bracelets, and blood pressure monitors are equipped with sensors that collect physiological data and transmit it to centralized platforms. This constant flow of information allows doctors and patients to receive real-time alerts and act quickly on any anomalies. Additionally, the integration of IoT devices in the home, such as smart scales and voice assistants, facilitates the monitoring of weight and medication adherence, which are crucial for managing cardiovascular and cerebrovascular diseases. The synergy between AI and IoT creates an advanced and highly interconnected monitoring ecosystem. AI leverages data collected by IoT devices to improve prediction models and tailor interventions more effectively. Likewise, this integration allows for the development of advanced alert systems that can predict and prevent complications before they become critical emergencies [26]. The combination of artificial intelligence and the Internet of Things is laying the foundation for a future where home monitoring of patients with cardio–cerebrovascular diseases is more proactive, personalized, and effective. This technology not only improves the quality of life for patients but also optimizes healthcare system resources by reducing the frequency of hospital visits and the duration of hospital stays.
3. Contribution and Evolution over Time
For many years, various methods have been identified in medicine for performing effective diagnostics and treatments to address different pathologies. The purpose of the study in this literature review is to focus precisely on how a line of work centered around data processing can contribute and add value to medical developments aimed at improving the quality of life of patients. The evolution of publications related to this topic is closely linked to the development of computer science and data mining. As shown in Figure 1 one can observe the evolution of articles published from 2000 to 2020, spanning two comparative decades. During the first 10 years, 2000–2010, there was a scant and emerging number of publications related to the study topic (12 publications), primarily due to the lack of computer developments that could support these various applications. Later, from 2011 to 2018, there was a significant advance that allowed for new ways to integrate IoT to provide solutions in medicine and care (99 publications), resulting in a 900% increase. The COVID-19 pandemic was a catalyst that enabled the widespread acceptance of using technologies for remote patient care, which in turn led to a significant global increase in publications, as can be seen in the last years, 2019–2022, with 190 publications, achieving a 191% increase in scientific production from the previous period, see Figure 1.
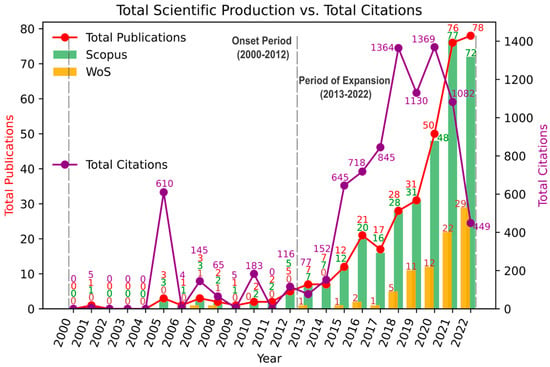
Figure 1.
Total Scientific Production vs. Total Citations.
Growth Phase (2000–2010): It is important to note that the scarce number of publications is mainly due to the incipient development and unification of remote sensor technology applied to medicine. During this period, 12 articles were published, of which 10 were published in the Scopus database and 2 in WoS. The lack of publications during this study period allows us to identify that these articles have many citations (1012). The most cited article in this period was by Lin [27], which describes the development of a portable healthcare system based on integrated fabric sensors, supporting many processes of remote patient care using data such as electrocardiograms, respiration, and activity. This article currently has 589 citations, accounting for more than 50% of the citations from the first decade of development in this research theme, making it highly relevant. Among the most notable contributions to this research topic in this phase are, see Table 1:

Table 1.
Significant contributions in the field of remote medical technology from 2001 to 2009.
Initial development phase (2010–2018): From 2010 to 2018, there was a notable increase in publications related to this line of research. A total of 99 articles were published, of which 69 are referenced in the Scopus database and 30 in the WoS database, with 2553 citations. Significant advancements were made during this period in using the Internet of Things to identify and treat various pathologies, especially those related to cardio–cerebrovascular diseases. The most outstanding work during this period was by researcher Yildirin [34], who implemented convolutional networks to analyze signals from long-duration ECGs to detect cardiac arrhythmias, see Table 2.

Table 2.
Significant contributions in the field of remote medical technology from 2010 to 2018.
Incremental Development Phase (2019-today): As previously described, this research topic is currently very relevant due to the external push generated by the COVID-19 pandemic, particularly in developments related to cardiac pathologies, a significant comorbidity for deterioration and cause of death in many patients worldwide. Consequently, the scientific community focused on creating numerous devices and mechanisms to safeguard patients with cardiac issues. As a result, 190 articles were published, significantly exceeding the publication volume of nearly two decades, with 63 of these articles indexed in the WoS database and 127 in the Scopus database. The most notable work during this period is by researcher Fan [42], with 246 citations, who focused his research on the development of clothing containing washable sensors for precise monitoring of epidermal physiological signals. These garments allow for the simultaneous tracking of arterial pulse waves and respiratory signals, see Table 3.

Table 3.
Significant contributions in the field of remote medical technology from 2019 to today.
4. Methods
4.1. Search Chain
To conduct the scientometric analysis focused on the use of support technologies for monitoring patients at home, using the Internet of Things and the models based on machine learning to make significant contributions to the care and quality of life of patients, a process of consultation and classification of articles published in the WoS and Scopus databases is carried out. These two databases have been used due to their wide acceptance in the scientific community, and they aggregate many bibliographic resources internationally. The results issued by these databases have been analyzed by different tools such as Bibliometrix [47] and the Tosr package, which has provided a global view of the different relationships between authors and their references worldwide. Specifically, this review article has provided a global view of how the use of technology can contribute to the monitoring of various cardio–cerebrovascular pathologies and can help determine what the barriers, challenges, and trends are in this type of solution.
In Table 4, the different concepts that are part of the search chain used for this scientometric review, which is associated with the use of machine learning techniques for home monitoring of patients with cardio–cerebrovascular diseases, can be identified. The keywords used in the search equation were as follows: (“telehealth” OR “homecare” OR “Telemedicine” OR “Teleconsultation” OR “Home health care” OR “In-home care” OR “Home care services”) and (“machine learning” OR “iot” OR “wearable”) and (“cardiovascular” OR “cerebrovascular”), which allowed the selection of 95 records in the WoS database and 366 in the Scopus database, obtaining a total of 462 files. After reducing file duplicity, an optimized search of 376 documents was achieved. Delving into the typology, we detail the following distribution: scientific articles (163, 43.1%), Review Paper (108, 28.5%), Conference Paper (66, 17.41%), Editorial (12, 3.7%), Book Chapter (8, 2.11%), Note (7, 1.85%), Conference Review (5, 1.32%), Letters (4, 1.06%), Early Access (3, 0.79%), Editorial Material (1, 0.26%), Erratum (1, 0.26%), and Short Survey (1, 0.26%) see Table 4.

Table 4.
Search results for the parameters in the databases.
To conduct the scientometric analysis focused on the use of support technologies for monitoring patients at home using the Internet of Things and models based on machine learning, clear inclusion and exclusion criteria were defined. Regarding the inclusion criteria, articles that specifically addressed the use of these technologies applied to cardio–cerebrovascular pathologies were considered. Only publications indexed in the WoS and Scopus databases were included due to their wide acceptance in the scientific community and their capacity to aggregate bibliographic resources internationally. The types of documents included scientific articles, reviews, conference papers, editorials, book chapters, notes, conference reviews, letters, early access articles, editorial material, errata, and short surveys. Additionally, the documents had to contain specific keywords in the search equation such as “telehealth”, “homecare”, “telemedicine”, “teleconsultation”, “home health care”, “in-home care”, “home care services”, “machine learning”, “IoT”, “wearable”, “cardiovascular”, and “cerebrovascular”. The publication period was also considered to ensure the relevance of the data and trends investigated. On the other hand, articles that did not focus on the use of IoT and machine learning for home monitoring of patients or that were not related to cardio–cerebrovascular pathologies were excluded. Duplicated documents between the WoS and Scopus databases were removed to maintain an optimized set of documents. Additionally, non-scientific documents such as news articles, non-peer-reviewed opinion pieces, and non-academic publications were excluded. Sources not indexed in WoS or Scopus that did not meet the required quality and scientific rigor standards were also discarded. Finally, publications in languages not accessible to the research team were excluded unless reliable translations were available. These criteria ensured the inclusion of high-quality and relevant literature, providing a comprehensive and accurate view of the use of advanced technologies in the home monitoring of patients with cardio–cerebrovascular diseases, identifying key barriers, challenges, and trends in this field.
To achieve these objectives, the methodology based on the metaphor of the Tree of Science was used, which provides information focused on two perspectives. Firstly, it describes detailed information associated with the most representative authors in the research line, along with analysis by country, journals, and number of citations. Additionally, it also provides relevant details on the evolution of the study topic, allowing us to understand how it has matured over time and thus identify knowledge gaps and potential contributions for future work.
4.2. Tree of Science
Tree of Science (ToS) is a web platform for searching scientific literature created at the National University of Colombia. This tool is designed to facilitate the search for relevant literature using graphic algorithms that present results through a tree metaphor. The platform can be used to recommend relevant literature through scientometric techniques, measure the impact of articles, journals, and institutions, and map scientific areas, thus facilitating the classification of search results [48]. It is based on graph theory metrics, with which articles in a field of knowledge are visualized as the roots, trunk, and leaves of a tree, placing each article according to certain characteristics. Classic articles with key research information are in the roots. The trunk represents research that fosters growth in the field or is considered structural publications. The leaves contain recently published articles that are highly connected to the trunk and roots [49].
This platform was specifically developed for literary searches in Web Of Science and Scopus, where search strings defined for the research are entered [50]. After obtaining the results, the articles from both Web of Science (WoS) and Scopus were downloaded. These files were then uploaded to ToS (http://tos.manizales.unal.edu.co, accessed on: 3 May 2024). With these data, ToS produced the results in the form of a tree: root, trunk, and leaves [51].
In addition to obtaining the tree, the tool allows for the analysis of the most cited articles, the countries where research has been developed, the most relevant journals, the leading authors in the area, and the collaboration networks that have been established on the topic. A large network is constructed from the reference citations where articles are represented by nodes and references by edges. The algorithm filters the network by eliminating articles with one citation and zero references to other articles. In addition to this, ToS extracts the most connected subnet, representing it in a larger form to eliminate small islands in the research topic. It is applied with a clean citation network to identify subcommunities of densely connected nodes (clusters) [49].
4.3. Scientometric Analysis
Scientometrics is based on the quantitative analysis of scientific production, aiming to investigate the development, structure, dynamics, trends, and relationships of scientific practice [52]. Scientometrics is useful for quantitatively analyzing and understanding the scientific output of a research topic and identifying emerging areas of science. With the advancement of technology, it is now possible to apply scientometric techniques in various research fields, such as health, artificial intelligence, home care, and cardiovascular diseases [53].
In the case of this review, the search for analysis was conducted between 2001 and 2023 in the Web Of Science and Scopus databases, using the previously mentioned search string, which initially yielded 462 files and 376 after deduplication. The scientometric analysis was performed using the R tool with its Bibliometrix and Tosr packages version 4.3.1 (Beagle Scouts), which were used for the scientific mapping that includes citation analysis, authors, words, country production, collaboration networks, and journals [27]. The analysis of the most relevant literature was carried out through the implementation of a mature data preprocessing process developed by Core of Science, following the PRISMA method (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [34], to select documents that are most aligned with the theme of the review, see Figure 2.
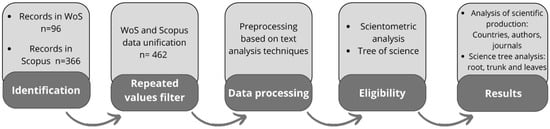
Figure 2.
PRISMA flow diagram.
5. Results
5.1. Country Analysis
Cardio–cerebrovascular diseases are among the leading causes of mortality worldwide and thus impose a significant budgetary burden on the healthcare system. That is why, from different sectors, there is a search for solutions focused on different phases or stages of the disease, whether in the early detection of symptoms to ensure a treatment that can support the non-deterioration of the patient’s health, in the intermediate phase where it is possible to identify how to monitor treatments administered by health personnel to ensure a halt in the deterioration of health, or in the critical phase where alarm protocols are defined for exhaustive monitoring of the critical condition of patients. Technology is a highly relevant ally in these processes, having become a crucial support in all phases of medical intervention, which is why this country analysis seeks to identify which countries have had significant development in the implementation of different applications associated with technology for these types of pathologies.
As can be seen in Table 5, the countries leading scientific production are those traditionally characterized as world leaders in technological development. The United States is the main producer of articles in this line, with 106 representing 25.79% of global scientific production. Additionally, it is the country with the highest number of citations at 3258. Of the one hundred six publications, fifty-eight are in Q1 journals (55%), fourteen in Q2 (13%), six in Q3 (6%), and one in Q4 (1%). Among these publications, the article by Bobak J. Mortazavi et al. [29] stands out; they conduct an analysis based on machine learning to analyze variables related to the readmission process of patients with heart failure.

Table 5.
Production by Countries.
The second country in terms of scientific publications is the Asian giant China, with 46 publications (11.19%), which is still quite far behind the United States in terms of publication level. China is not only the second country with the highest number of publications but also with the highest number of citations at 1248. Of the forty-six publications, sixteen are in Q1 (35%), eleven in Q2 (24%), four in Q3 (9%), and one in Q4 (2%). The work of Fan et al. [54] stands out again; it is a highly cited article related to the use of clothing, and it uses textiles to analyze different risk factors in patients.
The third representative country is Italy, where 33 publications (8.03%) have been made, and it is also the third country with the highest citation index at 940 (11.32%). Italy, being one of the countries most affected by being the epicenter of COVID-19 in Europe, stimulated the generation of new products and processes based on technology for these types of pathologies that directly impact the survival of patients with COVID-19. Of the thirty-three publications, eight are in Q1 journals (24%), seven in Q2 (21%), three in Q3 (9%), and one in Q4 (3%). The article by Paradiso et al. [55] is also highlighted, who, like the most notable author in China, shows the application of textiles using sensors to detect risk factors in cardiovascular patients.
The fourth representative country is the United Kingdom, which has 21 publications (5.11%). Additionally, it is also the fourth country with the highest number of citations at 370 (4.46%). Of the 21 publications, 14 are in Q1 journals (67%), 2 in Q2 392 (10%), and 2 in Q3 (10%). The most representative article is by Michael V. McConnell et al. [56], who analyzes the viability of obtaining lifestyle measures using an app developed for mobile devices. The fifth country in scientific publications is India, with 20 publications (4.87%); however, being the fifth country in the number of publications, the citations have been lower, ranking eighth at 88 (1.06%). Of the twenty publications, two are in Q1 (10%), one in Q3 (5%), and five in Q4 (25%). The work of D. Sobya [57] is highlighted, which shows the development of a wireless monitoring system based on ECG signals, combining the use of IoT for real-time data acquisition.
The sixth country in scientific publications is Germany, with 16 publications (3.89%); however, it is the penultimate country in terms of publications. Of the sixteen publications, five are in Q1 (31%), three in Q2 (19%), and four in Q3 (25%). The work of Shannon Wongvibulsin [58] is highlighted; it disseminates a systematic review of digital health in the cardiac patient rehabilitation processes. The seventh country with the most scientific production is Australia, with 14 publications (3.41%), and it is also the seventh in terms of citation index at 123 (1.48%). The most notable work is that of Santoso [59], who has reviewed the development of indoor environments for remote patient monitoring, showcasing different works that are important for the development of future applications.
The eighth country with the highest number of publications is Korea, with 14 (3.41%); it is important to note that even when it has a smaller number of publications, they have been well received by the scientific community, ranking as the sixth country in citations at 204 (2.46%). The article by Sang Hoon Chae [60] is highlighted, which shows the development and clinical evaluation of a web-based upper limb home rehabilitation system using a smartwatch and a machine learning model for survivors of chronic cerebrovascular accidents. The ninth country in publications is Canada, with 11 publications (2.68%), but it is important to note that they rank sixth in citations at 167 (2.01%). Of the eleven articles, five are published in Q1 journals (45%), one in Q2 (9%), and one in Q3 (9%). Among the published articles, the article by Lee H Schwamm [61] stands out, who proposes interesting recommendations concerning the application of teleassistance for cardiovascular patients.
Finally, France is the last country in producing articles related to this theme with 9 (2.19%) and is also coincidentally the last country in the citation index at 78 (0.94%). Of the nine published articles, two are in Q1 journals (22%) and two in Q2 (22%). Among the published articles, a literary review by Emmanuel Andrès [62] stands out; the review analyzes different perspectives of telemedicine applications in chronic cardiac conditions.
Figure 3 shows the scientific collaboration network among countries. It depicts six communities, with the largest comprising mainly the USA, Australia, China, and Belgium. An example of this scientific collaboration is the work on the adoption of digital devices in the field of telemedicine and artificial intelligence [61]. The communities by size graph display the size of the six communities, where community 1 has 20 countries and community 2 has 12. The nodes and links through the time figure show that until 2011, the academic community was working in isolation without creating links between countries. However, since 2012, the proportion of links began to grow significantly, and by 2021, the proportion of new countries starting research on telemedicine and artificial intelligence was surpassed.
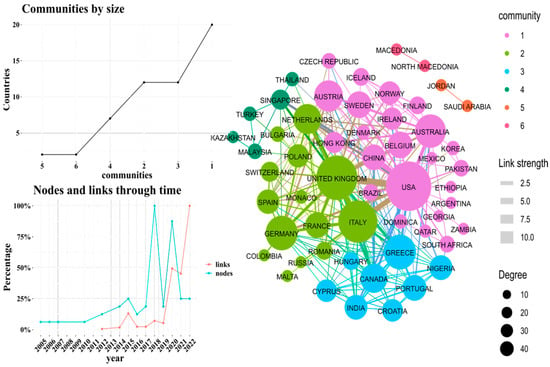
Figure 3.
Country collaboration network.
In the first community (pink), led by the United States, there are significant contributions from authors in this country with authors in Australia and Austria. Many of the works in this community are focused on IoT-based developments to detect risk factors associated with cardiac arrhythmia. Highlighted in this community are works relating to authors from countries like the USA and Australia, such as Ali [63], who presents a system that allows real-time assistance for continuous ECG monitoring and arrhythmia detection. Similarly, Christophe Leclercq [64] implements artificial intelligence to detect heart failure, with researchers from both the USA and Austria. As for the second community (green), led by European countries, the United Kingdom has had the most collaborations, specifically with authors from Italy and Germany, focusing on the use of mobile devices to support remote treatment and detection processes for cardiac arrhythmia. The work of Larissa Fabritz [56] stands out, showing how wearable devices can be used to monitor adult patients for cardiac arrhythmia.
The third community is led by Greece, where joint work has been developed with authors from countries like Canada and Nigeria, with significant systematic reviews of the literature analyzing different risk factors for cardiovascular diseases in older adults. Among the most representative works are those of Guasti [65], who analyzes how teleassistance can help prevent cardiovascular diseases in older adults, and Wongvibulsin [66], who examines how remote monitoring can support cardiac rehabilitation of patients. The fourth community is led by Singapore, where joint work has been conducted with authors from Thailand and Turkey, addressing issues related to user perceptions of using sensors to monitor relevant health indicators. The work of Rama Greenfield [44] is highlighted, analyzing truck drivers’ perceptions of using wearable devices to improve their health monitoring indicators.
5.2. Analysis by Journals
In the analysis of journals conducted, 83 indexed journals were found that feature publications related to the theme. Out of these, 20 journals contain articles only in the Scopus database and 74 in WoS. It is noted that from the 83 journals, only 10 are selected for the analysis shown in Table 6, considering the highest indices of impact factor, H-index, and Quartile. In addition, it is clarified that the journals analyzed are indexed journals. However, there may be relevant research on home care for cardiovascular diseases in journals that are not registered.

Table 6.
Production by Journals.
Regarding Table 6, which is organized by the order of the number of publications, the International Journal Of Environmental Research And Public Health has the highest number of publications related to the main theme of the review. This journal, from Switzerland, is multidisciplinary, open access, covers areas of environmental health and public health, and links disciplines such as biology, biochemistry, biotechnology, cellular and molecular biology, chemistry, computer science, ecology, engineering, epidemiology, genetics, immunology, microbiology, oncology, pathology, pharmacology, and toxicology. Despite having the highest number of publications, this journal is in the Q2 quartile and has an H-index of 167, a low value compared to other journals in the table that have fewer articles published on the main topic.
Regarding the impact factor, the journal with the highest value in this aspect (6.43) is the UK journal The Lancet Digital Health, which is open access, Q1 quartile, and focuses on decision sciences, health information management, and health informatics. Despite its impact factor, this journal has only four publications in the area of the review and an H-index of forty-eight, which indicates that it does not have a high number of citations. On the other hand, in second place, with 2.08, is the Journal Of The American Heart Association, also from the UK, open access and whose thematic areas focus on cardiology and cardiovascular medicine; this journal is in the Q1 quartile and has an H-index of 118, making it a relevant journal given its impact and citation level. In third place regarding the impact factor is the Journal Of Medical Internet Research, a journal from Canada is open access and focuses on emerging technologies, medical devices, applications, engineering and computer applications for patient education, prevention, population health, and clinical care. It belongs to the Q1 quartile and has an H-index of 178, the second-highest of the journals analyzed.
In terms of the H-index value, the journal Sensors, with an index of 219, has the highest citation index compared to the journals analyzed in this review. This open-access journal from Switzerland has seven publications on the main topic, but despite having the highest H-index and being in the Q1 quartile, it has a low impact factor. Finally, although the American journal IEEE Journal Of Biomedical And Health Informatics does not have the highest indexes of publications, impact factor, and H-index, the values in these last two factors are of interest given that it is a journal with a high number of citations and impact, making it an interesting journal for publishing research in the field of telemedicine focused on cardiovascular diseases.
In Figure 4, we can observe the citation network of the journals where three groups or communities are identified, interlinked by specific themes. Community or group 1 focuses mainly on the use of artificial intelligence as a telemedicine tool for cardiovascular diseases, with journals such as J MED INTERNET RES and STROKE standing out, which have published works like the one by Eunjeong Park [67], who developed an automatic classification system for cardiovascular accident symptoms through machine learning to assess motor weakness and NIHSS and MRC scores for four limbs. On the other hand, community 2 focuses on themes related to digital tools for the remote control of cardiovascular diseases, with the most impactful journals being CIRCULATION and J AM COLL CARDIOL, among which a strong link is observed and publications like the one by Karim Bayoumy [39], focused on the study of smart wearable devices for cardiovascular care.
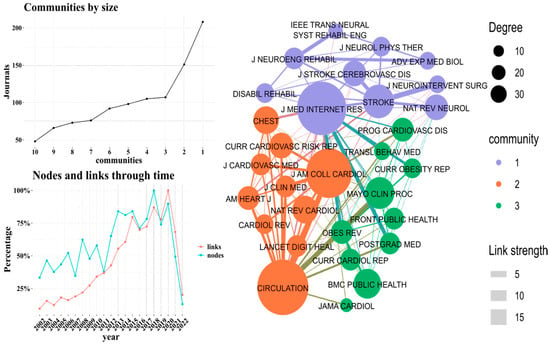
Figure 4.
Journal collaboration network.
Lastly, community 3 bases its research on themes such as the study of lifestyles related to cardiovascular diseases and telemedicine linked to them, highlighting journals like MAYO CLIN PROC and BMC PUBLIC HEALTH, where works are found such as the one published by Sarah Edney [68], which conducts a review of digital interventions aimed at movement behaviors and their influence on health. Figure 4 also shows the behavior of the nodes and the links of the journals over time, with 2018 being the year in which the highest percentage of articles were published and 2020 seeing the most collaborations among journals on the subject. Conversely, in the years 2021 and 2022, there is a significant decrease in both the percentage of citations and cooperation networks, which may be due to a decline in telemedicine research in the years following the pandemic or a shift in thematic focus for the collaboration of the journals.
5.3. Analysis by Authors
To conduct the author analysis, two sessions will be held: (i) Initially presenting researchers with the highest output in the field of homecare and telemedicine; (ii) In the second part, an analysis of the academic collaboration networks of the researchers (ego network) is carried out. According to Table 4, of the top ten researchers, four are from the United States; the others are from Korea, Australia, China, and Germany. Among the researchers, Martin and Turakhia, both from the United States, show the highest productivity, with 9 and 6 publications, respectively. Martin S has published works like the randomized clinical trial of a fully automated mobile health (mHealth) intervention with tracking and text messaging components to increase physical activity [69], which, according to Google Scholar, has 264 citations.
On the other hand, Turakhia M, together with MCCONNELL [27], conducted a review on advances in mobile health with mobile and wearable devices to assess and promote physical activity and fitness and to monitor heart rate and rhythm for the detection and treatment of atrial fibrillation, which has 124 citations. However, even though the authors have the highest productivity in this case, it is noteworthy that authors such as Hindricks G and Lin C, from Germany and Australia, respectively, have a higher Scopus Index. Hindricks has a total of 150,716 citations, an H-index of 111, and has recently published works like the TeleWear project [27], which involves integrating health data collected by mobile devices and mHealth-guided standardized measurement for patients with cardiovascular diseases. As for Lin C, according to Google Scholar, he has an H-index of 91 due to the 35,179 citations his publications have received, among which is the research article describing an intelligent telecardiology system using a wireless and portable ECG to detect atrial fibrillation [27], see Table 7.

Table 7.
Production by authors.
Figure 5 displays a personal scientific collaboration network among the most productive researchers in the field of homecare and telemedicine. In this network, a large component connects most researchers, indicating a high level of interdisciplinary and multi-institutional collaboration. This suggests a well-integrated and active research community where knowledge exchange and co-authorship are common. Professor Lovell, despite his significant contribution in terms of publication numbers, appears isolated from the main component. This could be due to various reasons, such as specialization in a unique subfield of telemedicine or homecare, or it may reflect geographical or institutional differences that limit collaboration. It is also possible that his collaborations are with researchers or institutions not included in the underlying dataset or not as active in the same thematic area.
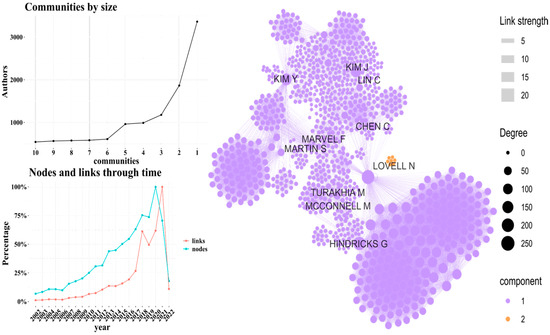
Figure 5.
Author collaboration network.
The main component shows a pattern of collaboration where researchers tend to work together or with colleagues who are already connected in the network. This is a typical characteristic of scientific collaboration networks, where existing collaboration encourages new connections, often referred to as the “small world” phenomenon in social networks. The presence of a “large component” means that there is a path of collaboration linking almost all researchers, facilitating the diffusion of knowledge and potential for joint projects. These connection patterns reflect not only current professional relationships but also may indicate emerging research areas and trends in homecare and telemedicine.
6. Tree of Science Analysis
Using the metaphor of the “Tree of Science”, we can examine the trajectory of the Internet of Things (IoT) in the context of patient care for cardio–cerebrovascular diseases over time. In this analysis, we focus our attention on the roots of the tree, a period during which this technology faced significant challenges due to low technological adoption, see Figure 6.
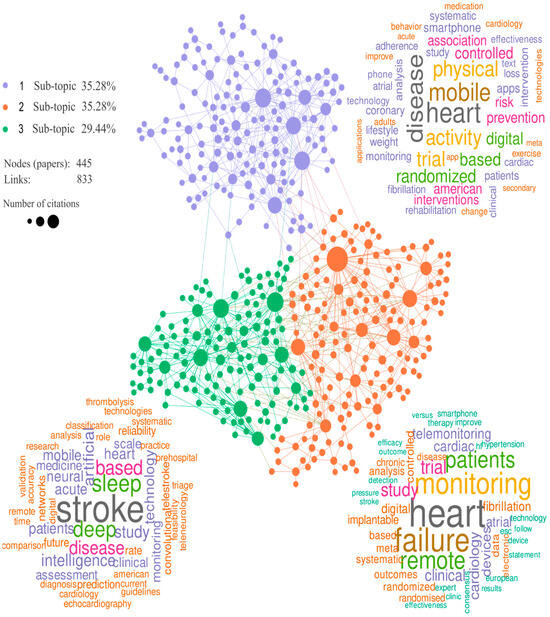
Figure 6.
Tree of Science representation.
6.1. Root: The Evolution of IoT in Patient Care for Cardio–Cerebrovascular Diseases
Using the “Tree of Science” metaphor, we can explore the trajectory of the Internet of Things (IoT) in patient care for cardio–cerebrovascular diseases over time. In this analysis, we focus on the roots of the tree, a period during which this technology encountered significant challenges due to low technological adoption. During a substantial period, the adoption of IoT in healthcare faced notable resistance to change globally. Healthcare systems and professionals tended to cling to traditional methods, often overlooking the potential advantages of technology. This reluctance to adopt IoT solutions for patient care limited the capacity for innovation in healthcare. Furthermore, another key factor was the availability and appropriation of the necessary technological resources. Internet connectivity and the proliferation of connected medical devices became essential for the success of IoT in patient care for cardio–cerebrovascular diseases. Reliable connectivity allowed real-time data transmission and communication between medical devices and healthcare systems, which significantly improved patient care and monitoring. As these barriers have been eliminated, IoT has flourished in the healthcare sector, improving the quality of care and offering new opportunities for monitoring and treating patients with cardiac and cerebrovascular conditions. Therefore, the theoretical foundations for many of the solutions currently in use were laid.
Among the most notable contributions is the work of Perez [70], who focuses on a large-scale evaluation of the use of a smartwatch for atrial fibrillation detection. Atrial fibrillation is a common and potentially dangerous cardiac arrhythmia that can increase the risk of stroke and other cardiovascular complications. Early detection of atrial fibrillation is essential for providing appropriate treatment and preventing serious complications. In this study, the authors conducted extensive research evaluating the performance of a smartwatch in detecting atrial fibrillation in a large number of participants. A large-scale approach was used to collect portable electrocardiogram data generated by the smartwatch, aiming to determine its ability to identify episodes of atrial fibrillation compared to traditional detection methods. The study’s results provide valuable insight into the effectiveness of smartwatch technology in detecting cardiac conditions, specifically atrial fibrillation. This is important in the context of cardiovascular health, as it may offer an early detection tool that could be widely accessible for continuous monitoring of individuals’ cardiac health. Meanwhile, Chow [71] focuses on a randomized clinical trial investigating the impact of lifestyle-focused text messages on modifying risk factors in patients with coronary disease. Coronary disease is a common and potentially serious cardiac condition associated with modifiable risk factors, such as diet, physical activity, smoking, and elevated blood pressure. Modifying these risk factors is crucial for reducing the risk of subsequent cardiovascular events in patients with coronary disease. In this study, the researchers conducted a clinical trial where patients with coronary disease were randomly assigned to two groups: one that received lifestyle-focused text messages as part of a behavioral health intervention and a control group that did not receive these messages. The text messages included reminders and advice related to diet, exercise, weight control, and stress management. The study’s goal was to assess whether the text message intervention had a significant impact on modifying risk factors compared to the control group. Parameters such as blood pressure, body mass index (BMI), physical activity, and other health indicators related to coronary disease were measured. The study’s results provided evidence that lifestyle-focused text messages can have a positive effect on modifying risk factors in patients with coronary disease. This text messaging-based intervention approach proved effective in promoting healthy behavioral changes and improving disease management.
Other authors, like Burke [72], address the increasing relevance of mobile applications and devices in promoting cardiovascular health, highlighting how these technologies can empower consumers to manage and control risk factors such as blood pressure, physical activity, diet, and weight. The scientific statement provides a comprehensive review of the existing scientific literature and underscores the importance of mobile applications, health monitoring devices, online platforms, and telemedicine in promoting cardiovascular health and preventing heart disease, thus supporting the growing role of mobile technology in enhancing the population’s cardiovascular health. Figure 7 and Table 8 illustrate the evolution of personal health monitoring devices during the early years of the 21st century, highlighting key technological advancements from 2000 to 2004.
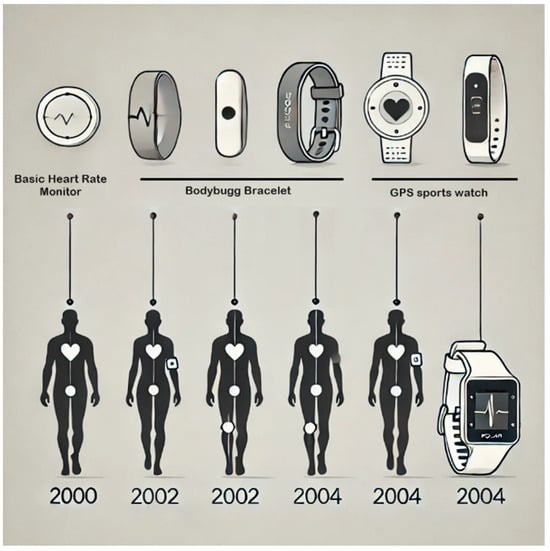
Figure 7.
First developments.

Table 8.
The beginnings.
6.2. Evolution of IoT Technology in Cardiovascular Patient Monitoring
The evolution of IoT (Internet of Things) technology in monitoring cardiovascular patients has significantly revolutionized healthcare and the management of cardiovascular diseases. This advanced technology enables the real-time collection of vital patient data such as heart rate, blood pressure, oxygen saturation, and other key parameters through connected medical devices. This information is remotely transmitted to healthcare professionals and healthcare systems, allowing constant monitoring and a quick response to any changes in the patient’s condition. Furthermore, the implementation of wearable devices and smart sensors has empowered patients, allowing them to actively participate in managing their cardiovascular health. This technological evolution not only improves the quality of care but also reduces medical costs, minimizes the need for unnecessary hospitalizations, and ultimately saves lives by providing more proactive and personalized care to those with cardiovascular conditions. During this stage of evolution, various authors made significant contributions that enabled the development of various solutions that have directly impacted the quality of life of treated patients.
Lobelo, F [76] focused on the integration of software applications and wearable health devices (mHealth) to support assessment, advice, and interventions to reduce the risk of cardiovascular diseases. In this context, the article addresses the growing adoption of mobile and wearable technologies in the health sector, especially in promoting physical activity and preventing cardiovascular diseases. It proposes a framework that seeks to leverage these technological tools to improve physical activity assessment, provide personalized advice, and design effective interventions to reduce the risk of heart disease. The article highlights the importance of this integration in modern healthcare and emphasizes the potential of mobile technologies to drive a positive change in lifestyle and cardiovascular health.
Rawstorn [77] focuses on designing and developing content for an innovative mobile health (mHealth) platform for exercise-based cardiac rehabilitation. The article discusses creating a cardiac tele-rehabilitation system that allows patients to carry out rehabilitation programs remotely using mobile devices and mHealth technology. It describes the design and development process of the platform, which includes specific content for cardiac rehabilitation, such as exercise programs, health monitoring, and virtual counseling. The article highlights the importance of this technology in expanding access to cardiac rehabilitation and improving patient adherence to these essential programs for recovery after cardiovascular events.
On the other hand, Alshurafa [78] focuses on the application of remote monitoring technology for patient health management and assesses this technology’s efficacy in predicting positive or negative health outcomes. The study uses health data collected from patients over a month, along with baseline data before the start of monitoring. The goal is to develop a predictive model that can identify which patients are more likely to experience health improvements through remote monitoring. This approach has significant implications for personalized healthcare and chronic disease management using remote monitoring technology.
Figure 8 and Table 9 present a clear and concise outline of the evolution of IoT technology in cardiovascular patient monitoring from 2006 to 2018. Through a timeline, key milestones are highlighted in three distinct phases, showing the progression from wearable devices and mobile health technologies through the consolidation of tele-rehabilitation systems to the implementation of smart sensors and the development of predictive models for personalized care. This visual representation provides an overview of how these innovations have transformed cardiovascular health management over the years.
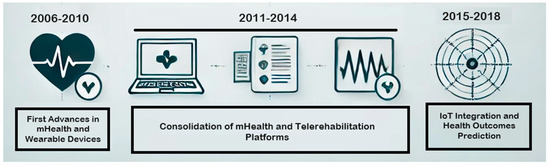
Figure 8.
IoT Technology in Cardiovascular Patient Monitoring.

Table 9.
Advancements in mHealth, wearable devices, and consolidation of tele-rehabilitation Platforms.
6.3. Branch 1: Mobile Applications for the Prevention of Heart Disease Risk and Physical Health Management
In the current digital era, mobile applications have become fundamental allies in healthcare, playing a vital role in preventing heart diseases and managing physical health. These innovative technological tools offer individuals the ability to monitor and enhance their cardiovascular well-being from the convenience of their devices. With a growing awareness of the importance of maintaining a healthy heart and preventing cardiovascular conditions, mobile applications provide information, real-time tracking, and personalized advice, empowering users to make informed decisions about their health. This topic has seen a high level of commitment from many researchers worldwide who have focused their efforts on developing solutions that can contribute to the prevention of complications associated with heart diseases.
Authors like Gardner [88] have focused on the development of an affordable foot sensor printed with ink, coupled with the implementation of machine learning techniques. This device aims to contribute to telemedicine and health monitoring in an accessible and effective manner. The article describes how this sensor is built and integrated into telemedicine devices to allow the continuous monitoring of patient health, especially in areas where resources are limited. The focus on ink sensor printing opens new possibilities for more economical and widely accessible healthcare solutions. Seetharam [89] focuses on the use of emerging technologies in the field of echocardiography. The article explores how mobile health, telemedicine, and artificial intelligence are being applied to enhance and optimize the acquisition and analysis of echocardiographic images. These technologies allow greater accessibility to cardiac care, diagnosis, and patient monitoring in remote settings or areas with limited resources. Additionally, the article examines how artificial intelligence is used to automate the interpretation of echocardiographic images, which can lead to more accurate diagnoses and more efficient medical care in cardiology. In summary, the article highlights the importance of the convergence of these technologies in improving cardiac care and clinical decision-making.
On the other hand, Hinchliffe [90] addresses the relationship between obesity and cardiovascular problems, exploring the essential role that digital health technology can play in the care and management of obesity, a major risk factor for cardiovascular diseases. The article examines how digital health solutions, such as mobile apps, tracking devices, and online programs, can provide effective tools for weight management and promoting healthier lifestyles. It also discusses how these technologies can contribute to the prevention of cardiovascular diseases by helping individuals manage their weight, exercise regularly, and improve their overall health. In summary, the article emphasizes the importance of digital health in combating obesity and its positive impact on reducing the risk of cardiovascular diseases.
In recent years, mobile applications have played a crucial role in transforming cardiovascular health care. Since 2018, we have witnessed a rapid evolution in how these technologies not only monitor patient health but also predict, diagnose, and prevent heart diseases. This timeline illustrates the key technological milestones achieved between 2018 and 2024, highlighting significant advances in areas such as artificial intelligence, telemedicine, and personalized health care, see Figure 9 and Table 10.
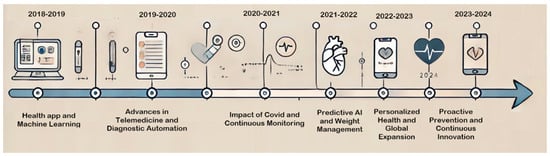
Figure 9.
Evolution of Mobile Applications for the Prevention of Heart Disease Risk.

Table 10.
Milestone of Mobile Applications for the Prevention of Heart Disease Risk.
6.4. Branch 2: Remote Cardiac Monitoring Devices for Clinical Tracking of Cardiovascular Patients
Remote Cardiac Monitoring Devices (RCMDs) play a vital role in the clinical care of patients with cardiovascular diseases, and their increasing adoption has transformed how these conditions are approached and managed. In a world where cardiovascular diseases are among the main causes of morbidity and mortality, remote monitoring offers a series of crucial advantages that have revolutionized cardiovascular health care. One of the most significant aspects of the importance of RCMDs lies in their ability to detect cardiac issues early. Heart diseases, including atrial fibrillation and other arrhythmias, can present subtle or intermittent symptoms that often go unnoticed in conventional medical care. However, these devices allow continuous monitoring and, therefore, early identification of any abnormalities, which in turn facilitates a more timely and accurate diagnosis. This early detection is crucial, as appropriate treatment in the early stages can make a difference in the prognosis and quality of life of the patient. In addition to early detection, RCMDs provide the possibility of constant and comprehensive monitoring of patients with chronic cardiovascular diseases. For those living with long-term cardiac conditions, remote monitoring becomes an essential tool for continuously assessing their health status. Physicians can access real-time data on heart rate, blood pressure, and other relevant parameters, allowing them to make informed decisions about adjustments in treatment, medication, and lifestyle for their patients. This level of control and monitoring not only improves clinical care but also empowers patients to actively participate in their care and decision-making. Mobility and accessibility are key features of RCMDs as they allow patients to keep a constant record of their cardiovascular health from the comfort of their home or wherever they are. This eliminates the need for frequent visits to medical centers, which in turn reduces the financial burden and stress associated with travel. Additionally, in emergency situations, these devices can automatically alert healthcare professionals, which could be crucial for saving lives. Another significant advantage is the customization capability that RCMDs offer. Each patient can benefit from a monitoring approach tailored to their specific needs, meaning that the most relevant data for their condition can be recorded and analyzed. This ensures more accurate care and a more effective intervention when necessary. In this line of work, various advances in technological development have been made.
Moghadam [103] focuses on the development and validation of an automated monitoring system based on deep learning to assess cortical activity in neonates. Monitoring brain activity in premature or neurologically at-risk newborns is crucial for identifying potential health issues and providing early and appropriate medical care. The tool developed in this study uses electroencephalography (EEG) to record the electrical activity of neonates’ brains. What distinguishes this research is the application of advanced deep learning techniques to automatically classify and analyze brain activity patterns, reducing the need for manual interpretation by specialists. The article describes in detail the methodology used, including the construction of a classification model based on deep neural networks and its training with neonatal EEG data. Additionally, an external validation of the model is performed using an independent cohort of neonatal patients, which strengthens the reliability of the results. The relevance of this study lies in its contribution to the field of neonatal care and evidence-based medicine. The automation of EEG analysis can accelerate the detection of neurological issues in neonates and, ultimately, improve medical care and clinical outcomes. The article provides a comprehensive overview of the methodology and results, making it a valuable contribution to medical research and high-quality neonatal care.
Meanwhile, Shiwani [104] addresses a highly relevant topic in the field of healthcare and cardiovascular disease management. This study focuses on the review and analysis of recent technologies that allow continuous monitoring of health and mobility indicators in patients with cardiovascular diseases. Traditionally, this monitoring was performed in periodic clinical settings, which limited the amount of data available and made it difficult to detect early changes in patients’ health. The article examines a range of innovative technologies and devices that have emerged in recent years to address this challenge. These devices can range from wearable sensors and remote monitoring devices to mobile apps and cloud platforms. Their main goal is to enable the continuous collection of data related to the health and mobility of patients with cardiovascular diseases. The review provides a detailed overview of the current technologies available and how they are applied to measure key indicators, such as heart rate, blood pressure, physical activity, and other health-related parameters. Additionally, the advantages and challenges associated with implementing these technologies in clinical care and cardiovascular disease management are discussed. The importance of this article lies in its contribution to improving medical care for patients with heart diseases. Continuous monitoring and the availability of real-time data can facilitate more timely and personalized intervention, which ultimately can improve patients’ quality of life and reduce the risk of complications. This study provides valuable insights for healthcare professionals, researchers, and technology developers interested in monitoring cardiovascular diseases.
Sheikh [105] focuses on a fundamental aspect of cardiovascular health: blood pressure variability and its relevance in clinical practice. The study addresses a topic of great importance, as blood pressure is a key indicator of cardiovascular health, and its variability can have significant implications for the diagnosis and management of cardiovascular diseases. The article begins by exploring the evolution in our understanding of blood pressure variability over time, from early clinical observations to current advances in measuring and analyzing this variability. It highlights how blood pressure variability has evolved from being an underestimated concept in the past to being recognized as an important factor in assessing cardiovascular risk. The study analyzes the clinical importance of blood pressure variability in various contexts, including predicting cardiovascular events, assessing treatment response, and its impact on brain health. Additionally, the tools and techniques available for measuring and quantifying blood pressure variability in clinical practice are discussed, which can help healthcare professionals make more informed decisions about patient management. A significant part of the article focuses on future perspectives in the field of blood pressure variability. Emerging research areas and advanced technologies that are enabling more accurate and continuous monitoring of blood pressure, such as wearable devices and telemedicine, are highlighted. These advancements promise more personalized medical care and a better understanding of blood pressure dynamics over time.
Figure 10 and Table 11 illustrate the evolution of Remote Cardiac Monitoring Devices (RCMD) technology from 2018 to 2024, highlighting key advancements that have transformed cardiovascular care. During this period, the technology has seen consolidation, with innovations improving accessibility and personalized care. The mass adoption driven by the COVID-19 pandemic underscored the importance of RCMDs, enabling continuous and remote care. As technology advances, there has been an increased emphasis on the integration of artificial intelligence and proactive prevention, marking a shift toward more comprehensive and personalized management of cardiovascular health.
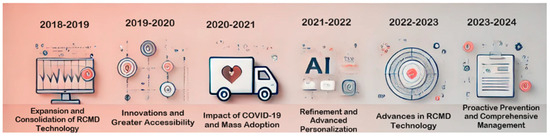
Figure 10.
Evolution of Remote Cardiac Monitoring Devices for clinical tracking of cardiovascular patients.

Table 11.
Timeline analysis of Remote Cardiac Monitoring Devices (RCMDs).
6.5. Branch 3: Deep Sleep-Based Technological Heart Monitoring for Stroke-Related Diseases
Deep sleep-based technological heart monitoring plays a crucial role in the care of stroke-related diseases due to a series of interconnected factors that positively impact patients’ cardiovascular health. Firstly, this monitoring mode is essential for the early detection of sleep disorders, such as sleep apnea, which can disrupt the deep sleep cycle, alter blood pressure regulation, and significantly increase the risk of stroke. Detecting these disorders during deep sleep provides a crucial opportunity for their timely diagnosis and treatment. Moreover, during this sleep phase, the heart may experience cardiac arrhythmias that, if not identified and appropriately treated, can contribute to the development of strokes and other severe cardiovascular problems.
Heart monitoring devices enable the early detection of abnormal heart rhythm patterns, allowing for immediate medical intervention and the implementation of appropriate treatment. Additionally, continuous monitoring during deep sleep offers a comprehensive assessment of a patient’s cardiovascular risk by measuring heart rate variability, providing valuable information about the health of the autonomic nervous system and the risk of cardiovascular events, such as strokes. For patients who have survived a stroke, technological heart monitoring is essential to prevent recurrent cerebrovascular events. Constant monitoring can identify signs of risk and allow health professionals to adjust treatment and provide specific recommendations to reduce the risk of a second stroke. Moreover, this type of monitoring offers long-term care and continuous tracking of patients’ cardiovascular health, facilitating the early identification of any changes in their condition and the adaptation of their care plan.
Lastly, but importantly, technological heart monitoring during deep sleep can significantly improve patients’ quality of life. It provides patients and their doctors with peace of mind knowing that proactive steps are being taken to protect their cardiovascular health, which can reduce the anxiety and stress associated with the risk of stroke and ultimately enhance their overall well-being. In summary, deep sleep-based technological heart monitoring is an essential tool in the prevention, diagnosis, and treatment of stroke-related diseases. It offers a unique window into the heart’s functioning during a critical sleep phase and allows for more personalized and effective care for patients at risk of stroke or those who have experienced a cerebrovascular event, which can have a significant impact on their quality of life and well-being.
Among the most notable works in this subline, those carried out by Doobie [117] address the relationship between physical activity, obesity, and the use of technology in health services, focusing on sleep analysis in cardiovascular patients. Obesity is a significant risk factor for cardiovascular diseases, and physical activity is a crucial strategy for preventing and treating obesity, as well as improving cardiovascular health. However, for exercise programs to be effective, it is essential to monitor and assess patients’ progress, and this is where technology comes into play. Sleep analysis plays a crucial role in this context, as inadequate or interrupted sleep can contribute to obesity and increase the risk of cardiovascular diseases. Technology offers tools such as wearable sleep monitoring devices and mobile apps that can help patients track their sleep patterns and identify potential issues, such as sleep apnea, which may be related to obesity and cardiovascular diseases. The article also discusses how technology can be used to create personalized exercise programs and monitor the physical activity of patients with obesity and cardiovascular diseases. Physical tracking devices, such as smartwatches and activity sensors, allow the recording of the amount of exercise performed, heart rate, and other relevant parameters, providing health professionals with valuable information to tailor exercise programs according to the individual needs of each patient.
Itchhaporia [118] focuses on the digital transformation in medicine and how it can improve quality of life, longevity, and health equity. Although the article does not explicitly mention sleep and cardiovascular diseases, it is relevant in this context. The digital transformation in medicine encompasses a wide range of technologies and approaches that have a significant impact on healthcare and the management of chronic diseases, including cardiovascular diseases. One area where technology has proven particularly useful is in monitoring and managing cardiovascular diseases, and this is where it relates to sleep. Sleep quality is essential for cardiovascular health. Sleep disorders, such as sleep apnea, can increase the risk of cardiovascular diseases, including hypertension and heart disease. Digital technology, such as sleep monitoring devices and mobile apps, allows patients and doctors to assess and manage sleep patterns effectively. These devices can record sleep duration, heart rate during sleep, and other relevant data, providing valuable information to identify sleep-related problems associated with cardiovascular health. Additionally, telemedicine and virtual medical consultations, which are part of the digital transformation in medicine, allow patients to access medical care and evaluate their sleep issues conveniently and efficiently. This is especially important for individuals who may have difficulty accessing traditional healthcare, thus contributing to health equity.
Rosenberger [119] focuses on a study that investigates sleep behavior, sedentary behavior, and physical activity over a 24 h period using nine wearable devices (wearables). The study focuses on the use of wearable technology to assess and understand sleep patterns and physical activity in a daily living environment. The nine wearable devices used in the study are used to collect data on the sleep, inactivity, and physical activity of participants over a full day. The main objective of the study is to provide a detailed and accurate insight into how people sleep, how much time they spend in sedentary behaviors, and how much time they dedicate to physical activity throughout the day. These data are crucial for understanding the health and wellness habits of individuals and can be useful for health professionals, researchers, and physicians. The article focuses on the importance of using wearable devices as valuable tools for monitoring and real-time data collection on sleep behavior and physical activity. The information obtained through these devices can help individuals make informed decisions about their lifestyle and health.
Figure 11 and Table 12 illustrate the evolution of deep sleep-based cardiac monitoring from 2018 to 2024. Over these six key years, important milestones are highlighted in the consolidation and expansion of this technology, advancing toward innovation, personalization, and accelerated digital transformation. Technological refinement and continuous evaluation enabled sustained global expansion, culminating in a proactive approach to the prevention and comprehensive management of cardiovascular health. This visual representation summarizes how these developments have transformed cardiac monitoring, improving the precision and scope of patient care.
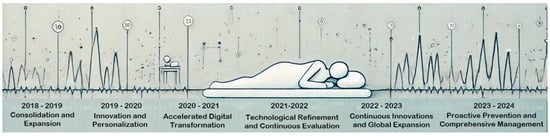
Figure 11.
Evolution of deep sleep-based technological heart monitoring for stroke-related diseases.

Table 12.
Timeline analysis of the evolution of deep sleep-based cardiac monitoring technology for stroke-related diseases.
7. Discussion
7.1. Technological Challenges
The review presents research that includes telehealth and the use of technological tools for the monitoring and treatment of diseases. However, it is still necessary to solve the problems related to the cybersecurity of medical devices linked to telehealth. In the case of IoT implementation in healthcare, recent research conducted in the U.S. concluded that 75% of IoT medical devices had known security breaches. Additionally, there is a lack of adequate guidance and regulation for these devices, an issue that policymakers around the world must address to prevent the vulnerability of new digital health solutions to cyberattacks [90].
Another challenge in telehealth relates to telerobotics. The lack of relevant clinical experience and the uncharted legal territory for telerobotics in real life may represent significant and potentially fatal barriers to its widespread implementation [126]. Adoption of the technologies also becomes a challenge, as the elderly population with limited information literacy finds it difficult to adopt and use telehealth tools. The availability and accessibility of tracking and monitoring technologies in the markets is another challenge. Another problem to be addressed is the handling of large volumes of data in both data mining and analysis [127]. There are also limitations related to the monitoring sensors, which include lack of control over ambient temperature, obstruction of signals, poor contact between sensors and skin, sensors that record activity but do not take into account the time that participants are resting or practicing sedentary activities, and results that cannot be generalized to all patients, since the individuals in the sample considered in the study may be in more or less advanced stages of the disease [128].
7.2. Data Security
The use of telemedicine raises a number of new issues and challenges related to its implementation or the regulations governing it, including the protection of medical record data containing patients’ personal data. This makes patient security and privacy a critical issue in telemedicine given such risks as the theft of patient security data, including text, audio, and image/video data. This is of particular concern when sensitive patient data such as histories of sexually transmitted diseases and mental disorders are involved [129,130]. Studies by various authors have analyzed the privacy and security challenges and risk factors of telehealth, finding three main factors. The first is the environmental factor related to the lack of private space for some populations and the difficulty of sharing information remotely in confidential conversations. The second is the technological factor including data security issues, which limited Internet access and technology. The third is the operational factor related to accessibility to technology [131].
Seeking solutions to these challenges, Nittari et al. propose informed consent inserted in the patient’s electronic record [132]. Hua Zhang et al. propose a scheme that integrates a data hiding algorithm into the telemedicine system for the protection of patient information [95]. Jing has reviewed the security problems at the application, transport, and network layers, stating that the direction to overcoming the security problems in telemedicine is to research on lightweight algorithms to maximize security with fewer resource usage considerations. Yan et al. suggested various methods, such as data cryptography and authentication protocols, as a solution to reduce security threats. On the other hand, Zhang et al. proposed an approach to use biometrics derived from the patient’s body to generate high-quality but different random numbers at each step as a key to protect wireless communication. Komal has used an intrusion detection system (IDS) as a tool to monitor traffic and protect the cloud [133].
7.3. Post-COVID Impacts
The COVID-19 pandemic was an exceptional, unforeseen, and unexpected event that marked a milestone in world history. This event set a precedent in various fields, especially in the area of health, since it caused profound changes in hospital facilities as well as in their organization. It also brought to light the deficiencies of hospital and territorial systems in all their articulations [134]. This event, in addition to altering healthcare, generated an accelerated development of telemedicine and its services. Since before the pandemic, in the last decade, many telemedical services have been gaining ground, including tools such as teleconsultations, electronic prescriptions, teleradiology, and telecardiology. However, these digital telemedical technologies had low market penetration, and there was a lack of user awareness [135]. As the pandemic progressed, there was increased interest from physicians and healthcare in increasing telemedicine and the use of handheld devices in patient care [136].
The above can be analyzed with research such as that of Lilas Dagher et al., in which they developed a cardiovascular clinic patient survey to assess the challenges and opportunities of digital health adoption during the COVID-19 pandemic. This study found that only 10.8% of participating patients reported using telemedicine for clinical care prior to the onset of COVID-19. Post-pandemic, a significant increase of 24.3% of patients were found to initiate telemedicine use. Additionally, when asked about barriers to care alleviated by telemedicine, the majority of participants recorded that telemedicine helped overcome challenges in finding reliable physicians (75.2%), resolving transportation issues (67.9%), and maintaining social distancing measures (63.3%) [137]. With the successful implementation and deployment of these emerging technologies during the evolution of the pandemic and acceptance by users, the burden on healthcare systems can be reduced, and clinical outcomes can be improved by timely intervention, identifying any deterioration and exacerbation at an early stage; diagnosis and treatment can be rapid with detection of suspected and asymptomatic/presymptomatic cases; and contacts between medical personnel and patients can be minimized by remote monitoring and care. Because of this, the use of telemedicine holds great promise for reducing costs, promoting patient follow-up and prevention, and combating pandemics such as COVID-19 [137].
7.4. Socioeconomic Factors
According to Lilas Dagher et al., there are significant demographic differences in current and previous use of portable health devices and telemedicine, as well as in attitudes toward these digital health tools. In this research, it is observed that prior to COVID-19, there were no statistical differences in telemedicine use among the different demographic groups of participants. However, it was determined that patients with a higher educational level and younger patients made more frequent use of telemedicine. This is due to greater economic barriers that have generated a lower educational level and lower accessibility to the Internet, as well as the ease with which young people adapt to technology. In addition, the perceived cost-benefit ratio and literacy [138,139]. The economic and technological development gaps between developed and developing countries also generate limitations and challenges in the use of digital health. One of the main barriers is the lower public spending on health compared to developed countries. Low literacy rates, a lack of trained and qualified personnel for the implementation of digital health services, and a lack of availability of digital tools and services such as cell phones, computer systems, and Internet connections in rural and remote areas make these systems work suboptimally. Therefore, it is necessary to analyze the environmental factors for the implementation of telehealth [140,141].
8. Conclusions
The evolution of Internet of Things (IoT) technologies in monitoring cardiovascular patients has been transformative, revolutionizing the prevention and management of cardiovascular diseases. However, to maximize the impact of these innovations, it is crucial to provide clear recommendations for future research and practical implementation.
Continuous and Specific Technological Improvement: Although current technologies have proven effective in early detection and continuous monitoring, future research must focus on improving the accuracy and predictive capabilities of these devices. This could include the development of more sophisticated artificial intelligence and machine learning algorithms that not only identify risks but also predict the onset of cardiovascular events with greater precision.
Expansion of Access and Global Adoption: The integration of advanced technologies in cardiovascular monitoring must be accessible to a global audience, especially in regions with limited resources. Future research should explore ways to reduce the production and distribution costs of these devices, as well as ensure their interoperability across different healthcare systems.
Practical Application in Healthcare: To maximize the benefits of these technologies, it is essential that healthcare professionals are trained in their use. Medical institutions should develop training programs that include the management of IoT devices and real-time data interpretation to optimize clinical decision-making and reduce the need for invasive interventions.
Interdisciplinary Research for Continuous Innovation: Promoting collaboration between disciplines such as biomedical engineering, computer science, and medicine will be crucial in driving innovation in this field. This collaboration can accelerate the development of more advanced technologies and ensure that solutions are both scientifically sound and clinically applicable.
Ethics and Data Security: As monitoring technologies become more ubiquitous, future research must address ethical and data security concerns. It is vital to develop robust protocols that protect patient privacy while maximizing the value of the data collected to improve health outcomes.
Long-Term Impact Evaluation: Longitudinal studies are needed to evaluate the long-term impact of these technologies on cardiovascular health. This research will help refine clinical practice recommendations and identify areas where adjustments are needed to improve outcomes.
Author Contributions
Conceptualization, E.R.-P.; methodology, L.V.T.-B.; software, M.A.P.-M.; validation, M.A.U.-T.; formal analysis, S.B.-A.; writing—original draft preparation, P.P.A.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. WHO Global Observatory for eHealth. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. 2010, 2, 938–950. Available online: https://iris.who.int/handle/10665/44497 (accessed on 1 May 2024).
- Heratanti, N.; Rambi, A.; Syarifurrahman, I. The Telehealth Effectiveness in Home Care Services: A Systematic Review. STRADA J. Ilm. Kesehat. 2021, 10, 1057–1065. [Google Scholar] [CrossRef]
- Patel, P.; Dhindsa, D.; Eapen, D.J.; Khera, A.; Gulati, M.; Stone, N.J.; Yancy, C.W.; Rumsfeld, J.S.; Sperling, L.S. Optimizing the Potential for Telehealth in Cardiovascular Care (in the Era of COVID-19): Time Will Tell. Am. J. Med. 2021, 134, 945–951. [Google Scholar] [CrossRef] [PubMed]
- Pacis, D.; Subido, J.; Bugtai, N. Trends in telemedicine utilizing artificial intelligence. AIP Conf. Proc. 2018, 1933, 040009. [Google Scholar] [CrossRef]
- Mohammadzadeh, N.; Rezayi, S.; Tanhapour, M.; Saeedi, S. Telecardiology interventions for patients with cardiovascular Disease: A systematic review on characteristics and effects. Int. J. Med. Inform. 2022, 158, 104663. [Google Scholar] [CrossRef]
- Battineni, G.; Sagaro, G.G.; Chintalapudi, N.; Amenta, F. The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review. J. Pers. Med. 2021, 11, 658. [Google Scholar] [CrossRef]
- Ghilencea, L.-N.; Chiru, M.-R.; Stolcova, M.; Spiridon, G.; Manea, L.-M.; Stănescu, A.-M.A.; Bokhari, A.; Kilic, I.D.; Secco, G.G.; Foin, N.; et al. Telemedicine: Benefits for Cardiovascular Patients in the COVID-19 Era. Front. Cardiovasc. Med. 2022, 9, 868635. [Google Scholar] [CrossRef]
- Saragih, I.D.; Schorr, E.; Porta, C.M.; Batubara, S.O.; Lee, B. Effects of telehealth-assisted interventions for secondary prevention of cardiovascular disease: A systematic review and meta-analysis. J. Clin. Nurs. 2023, 32, 3613–3629. [Google Scholar] [CrossRef]
- Alarabyat, I.A.; Al-Nsair, N.; Alrimawi, I.; Al-Yateem, N.; Shudifat, R.M.; Saifan, A.R. Perceived barriers to effective use of telehealth in managing the care of patients with cardiovascular diseases: A qualitative study exploring healthcare professionals’ views in Jordan. BMC Health Serv. Res. 2023, 23, 452. [Google Scholar] [CrossRef]
- Jing, L.; Chen, T.; Yang, Z.; Dong, W. Association of the blood levels of specific volatile organic compounds with nonfatal cardio-cerebrovascular events in US adults. BMC Public Health 2024, 24, 616. [Google Scholar] [CrossRef]
- Komilovich, E.; Khalimovich, M. Nursing care for coronary artery disease, Angina Pectoris. J. New Century Innov. 2024, 46, 86–94. [Google Scholar]
- Lo, E.; Faraci, F. Mechanisms in Cardiovascular and Cerebrovascular Disease. Circ. Res. 2024, 134, 615–617. [Google Scholar] [CrossRef] [PubMed]
- McGinigle, K. Peripheral Vascular Disease. Prim. Care Clin. Off. Pract. 2024, 51, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Bourazana, A.; Xanthopoulos, A.; Briasoulis, A.; Magouliotis, D.; Spiliopoulos, K.; Athanasiou, T.; Triposkiadis, F. Artificial Intelligence in Heart Failure: Friend or Foe? Life 2024, 14, 145. [Google Scholar] [CrossRef] [PubMed]
- Qiu, R.; Wan, S.; Zhong, C.; Han, S.; He, T.; Huang, Y.; Shang, H. Core outcome sets for myocardial infarction in clinical trials of traditional Chinese medicine and Western medicine. J. Evid. -Based Med. 2024, 17, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Gao, Z.; Li, Y.; Mei, S.; Tian, S.; Wu, G.; Qin, K. Double closed-loop feedback control strategy for enhanced external counterpulsation to regulate hemodynamic response of human common carotid artery. Biomed. Signal Process. Control 2024, 91, 105914. [Google Scholar] [CrossRef]
- Li, B.; Liu, Y.; Li, G.; Zhang, Z.; Feng, Y.; Mao, B. A real-time patient-specific treatment strategy for enhanced external counterpulsation. Int. J. Numer. Methods Biomed. Eng. 2024, 40, e3808. [Google Scholar] [CrossRef]
- Guo, S.; Han, L.; Guo, Y. Standards Related to Smart Medicine. In Advanced Technologies in Healthcare: AI, Signal Processing. Digital Twins and 5G; Springer Nature: Singapore, 2024; pp. 155–170. [Google Scholar]
- Wichaiyo, S.; Koonyosying, P.; Morales, N. Functional Roles of Furin in Cardio-Cerebrovascular Diseases. ACS Pharmacol. Transl. Sci. 2024, 7, 570–585. [Google Scholar] [CrossRef]
- Zhang, J.; Fan, X.; Xu, Y.; Wang, K.; Xu, T.; Han, T.; Jin, L. Association between inflammatory biomarkers and mortality in individuals with type 2 diabetes: NHANES 2005–2018. Diabetes Res. Clin. Pract. 2024, 209, 111575. [Google Scholar] [CrossRef]
- Addissouky, T.; El-Sayed, I.; Ali, M.; Wang, Y.; El-Baz, A.; Elarabany, N.; Khalil, A. Shaping the future of cardiac wellness: Exploring revolutionary approaches in disease management and prevention. J. Clin. Cardiol. 2024, 5, 6–29. [Google Scholar] [CrossRef]
- Kossi, O.; Bonnechere, B.; Agbetou, M.; Somasse, R.; Hokpo, A.; Houehanou, Y.; Mandigout, S. Relationships between cardiorespiratory fitness, physical activity practices, and functional outcomes one-year post-stroke in northern Benin: A case–control study. Top. Stroke Rehabil. 2024, 31, 104–115. [Google Scholar] [CrossRef]
- Pejovic, S.; Vgontzas, A.; Fernandez-Mendoza, J.; He, F.; Li, Y.; Karataraki, M.; Bixler, E. Insomnia with objective but not subjective short sleep duration is associated with incident cardiovascular and/or cerebrovascular disease. J. Clin. Sleep Med. 2024, 20, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Huan, J.; Zhu, L.; Xu, J.; Song, K. The neutrophil percentage-to-albumin ratio is an independent risk factor for poor prognosis in peritoneal dialysis patients. Ren. Fail. 2024, 46, 2294149. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Yi, W.; Occhipinti, E.; Dai, Y.; Gao, S.; Occhipinti, L. A roadmap for the development of human body digital twins. Nat. Rev. Electr. Eng. 2024, 1, 199–207. [Google Scholar] [CrossRef]
- Hu, L.; Zhang, M.; Hu, P.; Zhang, J.; Niu, C.; Lu, X.; Ma, Y. Dual-channel hypergraph convolutional network for predicting herb–disease associations. Brief. Bioinform. 2024, 25, bbae067. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.T.; Chang, K.C.; Lin, C.L.; Chiang, C.C.; Lu, S.W.; Chang, S.S.; Lin, B.S.; Liang, H.Y.; Chen, R.J.; Lee, Y.T.; et al. An intelligent telecardiology system using a wearable and wireless ECG to detect atrial fibrillation. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 726–733. [Google Scholar] [CrossRef]
- Wilson, L.; Ho, P.; Bengston, K.; Dadd, M.; Chen, F.; Huynh, C.; Gill, R. The CSIRO hospital without walls home telecare system. In Proceedings of the Seventh Australian and New Zealand Intelligent Information Systems Conference, Perth, WA, Australia, 18–21 November 2001; pp. 43–46. [Google Scholar]
- Paradiso, R.; Loriga, G.; Taccini, N. A wearable health care system based on knitted integrated sensors. IEEE Trans. Inf. Technol. Biomed. 2005, 9, 337–344. [Google Scholar] [CrossRef]
- Villalba, E.; Arredondo, M.; Moreno, A.; Salvi, D.; Guillen, S. User Interaction Design and Development of a Heart Failure Management System based on Wearable and Information Technologies. In Proceedings of the International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; pp. 400–403. [Google Scholar] [CrossRef]
- Zheng, J.W.; Zhang, Z.B.; Wu, T.H.; Zhang, Y. A wearable mobihealth care system supporting real-time diagnosis and alarm. Med. Biol. Eng. Comput. 2007, 45, 877–885. [Google Scholar] [CrossRef]
- Taccini, N.; Loriga, G.; Pacelli, M.; Paradiso, R. Wearable monitoring system for chronic cardio-respiratory diseases. In Proceedings of the 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–25 August 2008; pp. 3690–3693. [Google Scholar] [CrossRef]
- Villalba, E.; Salvi, D.; Peinado, I.; Ottaviano, M.; Arredondo, T. Validation Results of the User Interaction in a Heart Failure Management System. In Proceedings of the International Conference on eHealth, Telemedicine, and Social Medicine, Cancun, Mexico, 1–7 February 2009; pp. 81–86. [Google Scholar] [CrossRef]
- Yildirim, O.; Plawiak, P.; Tan, R.; Acharya, U. Arrhythmia detection using deep convolutional neural network with long duration ECG signals. Comput. Biol. Med. 2018, 102, 411–420. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, Z.; Tang, Y.; Zhao, M.; Chen, S.; Hou, J.; Ke, M. The development of Diabetics-oriented Telemedical Information System. In Proceedings of the IEEE International Conference on Information and Automation, Shenzhen, China, 6–8 June 2011; pp. 720–725. [Google Scholar] [CrossRef]
- Lobodzinski, S.; Laks, M. New devices for very long-term ECG monitoring. Cardiol. J. 2012, 19, 210–214. [Google Scholar] [CrossRef]
- Lee, B.; Kim, K.; Ku, B.; Jang, J.; Kim, J. Prediction of body mass index status from voice signals based on machine learning for automated medical applications. Artif. Intell. Med. 2013, 58, 51–61. [Google Scholar] [CrossRef]
- Huang, A.; Chen, C.; Bian, K.; Duan, X.; Chen, M.; Gao, H. WE-CARE: An Intelligent Mobile Telecardiology System to Enable mHealth Applications. IEEE J. Biomed. Health Inf. 2014, 18, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.; Feldman, D.; Blumenthal, R.; Jones, S.; Post, W.; McKibben, R. MActive: A Randomized Clinical Trial of an Automated mHealth Intervention for Physical Activity Promotion. J. Am. Heart Assoc. 2015, 4, e002239. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, J.; Downing, N.; Bucholz, E.; Dharmarajan, K.; Manhapra, A.; Li, S. Analysis of Machine Learning Techniques for Heart Failure Readmissions. Circulation 2016, 9, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Vegesna, A.; Tran, M.; Angelaccio, M.; Arcona, S. Remote Patient Monitoring via Non-Invasive Digital Technologies: A Systematic Review. Telemed. E-Health 2017, 23, 3–17. [Google Scholar] [CrossRef]
- Fan, W.; He, Q.; Meng, K.; Tan, X.; Zhou, Z.; Zhang, G. Machine-knitted washable sensor array textile for precise epidermal physiological signal monitoring. Sci. Adv. 2020, 6, eaay2840. [Google Scholar] [CrossRef]
- Shan, R.; Sarkar, S.; Martin, S. Digital health technology and mobile devices for the management of diabetes mellitus: State of the art. Diabetologia 2019, 62, 877–887. [Google Scholar] [CrossRef]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G.; et al. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- Yang, S.; Lv, S.; Zhang, W.; Cui, Y. Microfluidic Point-of-Care (POC) Devices in Early Diagnosis: A Review of Opportunities and Challenges. Sensors 2022, 22, 1620. [Google Scholar] [CrossRef]
- Brunetti, N.; Curcio, A.; Nodari, S.; Parati, G.; Carugo, S.; Molinari, M. The Italian Society of Cardiology and Working Group on Telecardiology and Informatics 2023 updated position paper on telemedicine and artificial intelligence in cardiovascular disease. J. Cardiovasc. Med. 2023, 24, e168–e177. [Google Scholar] [CrossRef]
- Zuluaga, M.; Robledo, S.; Arbelaez-Echeverri, O.; Osorio-Zuluaga, G.A.; Duque-Méndez, N. Tree of Science—ToS: A web-based tool for scientific literature recommendation. Search less, research more! Issues Sci. Technol. Librariansh. 2022. [Google Scholar] [CrossRef]
- Robledo, S.; Zuluaga, M.; Valencia-Hernandez, L.; Arbelaez-Echeverri, O.; Duque, P.; Alzate-Cardona, J. Tree of Science with Scopus: A Shiny Application. Issues Sci. Technol. Librariansh. 2022. [Google Scholar] [CrossRef]
- Valencia-Hernandez, D.; Robledo, S.; Pinilla, R.; Duque, N.; Olivar-Tost, G. SAP Algorithm for Citation Analysis: An improvement to Tree of Science. Ing. E Investig. 2020, 40, 45–49. [Google Scholar] [CrossRef]
- Grisales-Aguirre, A.M.; Robledo, S.; Zuluaga, M. Topic Modeling: Perspectives From a Literature Review. IEEE Access 2023, 11, 4066–4078. [Google Scholar] [CrossRef]
- Michán, L.; Muñoz-Velasco, I. Cienciometría para ciencias médicas: Definiciones, aplicaciones y perspectivas. Investig. En. Educ. Médica 2013, 2, 100–106. [Google Scholar] [CrossRef]
- Robledo, P.; Duque, A.; Aguirre, G. Word of Mouth Marketing: A Scientometric Analysis. J. Scientometr. Res. 2023, 11, 436–446. [Google Scholar] [CrossRef]
- Duran-Aranguren, D.; Robledo, S.; Gomez-Restrepo, E.; Arboleda-Valencia, J.; Tarazona, N. Scientometric Overview of Coffee By-Products and Their Applications. Molecules 2021, 26, 7605. [Google Scholar] [CrossRef]
- McConnell, M.; Shcherbina, A.; Pavlovic, A.; Homburger, J.; Goldfeder, R.; Waggot, D. Feasibility of obtaining measures of lifestyle from a smartphone app: The MyHeart Counts Cardiovascular Health Study. JAMA Cardiol. 2017, 2, 67–76. [Google Scholar] [CrossRef]
- Sobya, D.; Muruganandham, S.; Nallusamy, S.; Chakraborty, P. Wireless ECG monitoring system using IoT based signal conditioning module for real time signal acquisition. Indian J. Public Health Res. 2018, 9, 294–299. [Google Scholar] [CrossRef]
- Wongvibulsin, S.; Habeos, E.; Huynh, P.; Xun, H.; Shan, R.; Porosnicu-Rodriguez, K. Digital health interventions for cardiac rehabilitation: Systematic literature review. J. Med. Internet Res. 2021, 23, e18773. [Google Scholar] [CrossRef]
- Santoso, F.; Redmond, S. Indoor location-aware medical systems for smart homecare and telehealth monitoring: State-of-the-art. Physiol. Meas. 2015, 36, R53. [Google Scholar] [CrossRef]
- Chae, S.; Kim, Y.; Lee, K.; Park, H. Development and clinical evaluation of a web-based upper limb home rehabilitation system using a smartwatch and machine learning model for chronic stroke survivors: Prospective comparative study. JMIR Mhealth Uhealth 2020, 8, e17216. [Google Scholar] [CrossRef]
- Schwamm, L.; Chumbler, N.; Brown, E.; Fonarow, G.; Berube, D.; Nystrom, K. Recommendations for the implementation of telehealth in cardiovascular and stroke care: A policy statement from the American Heart Association. Circulation 2017, 135, e24–e44. [Google Scholar] [CrossRef] [PubMed]
- Andres, E.; Talha, S.; Zulfiqar, A.; Hajjam, M.; Ervé, S.; Hajjam, J. Current research and new perspectives of telemedicine in chronic heart failure: Narrative review and points of interest for the clinician. J. Clin. Med. 2018, 7, 544. [Google Scholar] [CrossRef] [PubMed]
- Leclercq, C.; Witt, H.; Hindricks, G.; Katra, R.; Albert, D.; Belliger, A. Wearables, telemedicine, and artificial intelligence in arrhythmias and heart failure: Proceedings of the European Society of Cardiology Cardiovascular Round Table. Europace 2022, 24, 1372–1383. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Naing, H.; Yaqub, R. An IoT assisted real-time high CMRR wireless ambulatory ECG monitoring system with arrhythmia detection. Electronics 2021, 10, 1871. [Google Scholar] [CrossRef]
- Fabritz, L.; Connolly, D.; Czarnecki, E.; Dudek, D.; Zlahoda-Huzior, A.; Guasch, E. Remote Design of a Smartphone and Wearable Detected Atrial Arrhythmia in Older Adults Case Finding Study: Smart in OAC–AFNET 9. Front. Cardiovasc. Med. 2022, 9, 585. [Google Scholar] [CrossRef]
- Guasti, L.; Dilaveris, P.; Mamas, M.; Richter, D.; Christodorescu, R.; Lumens, J.; Cowie, M. Digital health in older adults for the prevention and management of cardiovascular diseases and frailty. A clinical consensus statement from the ESC Council for Cardiology Practice/Taskforce on Geriatric Cardiology, the ESC Digital Health Committee and the ESC Working Group on e-Cardiology. ESC Heart Fail. 2022, 9, 2808–2822. [Google Scholar] [CrossRef]
- Greenfield, R.; Busink, E.; Wong, C.; Riboli-Sasco, E.; Greenfield, G.; Majeed, A. Truck drivers’ perceptions on wearable devices and health promotion: A qualitative study. BMC Public Health 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Park, E.; Lee, K.; Han, T.; Nam, H. Automatic Grading of Stroke Symptoms for Rapid Assessment Using Optimized Machine Learning and 4-Limb Kinematics: Clinical Validation Study. J. Med. Internet Res. 2020, 22, e20641. [Google Scholar] [CrossRef]
- Edney, S.; Chua, X.; Muller, A.; Kui, K.; Muller-Riemenschneider, F. MHealth interventions targeting movement behaviors in Asia: A scoping review. Obes. Rev. 2022, 23, e13396. [Google Scholar] [CrossRef]
- McConnell, M.; Turakhia, M.; Harrington, R.; King, A.; Ashley, E. Mobile Health Advances in Physical Activity, Fitness, and Atrial Fibrillation. J. Am. Coll. Cardiol. 2018, 71, 2691–2701. [Google Scholar] [CrossRef] [PubMed]
- Leiner, J.; König, S.; Mouratis, K.; Kim, I.; Schmitz, P.; Joshi, T.; Schanner, C.; Wohlrab, L.; Hohenstein, S.; Pellissier, V.; et al. A Digital Infrastructure for Cardiovascular Patient Care Based on Mobile Health Data and Patient-Reported Outcomes: Concept Details of the Helios TeleWear Project Including Preliminary Experiences. JMIR Form. Res. 2023, 7, e41115. [Google Scholar] [CrossRef]
- Perez, M.; Mahaffey, K.; Hedlin, H.; Rumsfeld, J.; Garcia, A.; Ferris, T. Large-scale assessment of a smartwatch to identify atrial fibrillation. N. Engl. J. Med. 2019, 381, 1909–1917. [Google Scholar] [CrossRef]
- Chow, C.; Redfern, J.; Hillis, G.; Thakkar, J.; Santo, K.; Hackett, M. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: A randomized clinical trial. Jama 2015, 314, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.; Ma, J.; Azar, K.; Bennett, G.; Peterson, E.; Zheng, Y. Current science on consumer use of mobile health for cardiovascular disease prevention: A scientific statement from the American Heart Association. Circulation 2015, 132, 1157–1213. [Google Scholar] [CrossRef]
- Ge, Z.; Prasad PW, C.; Costadopoulos, N.; Alsadoon, A.; Singh, A.K.; Elchouemi, A. Evaluating the accuracy of wearable heart rate monitors. In Proceedings of the 2016 2nd International Conference on Advances in Computing, Communication, & Automation (ICACCA)(Fall), Bareilly, India, 30 September–1 October 2016; pp. 1–6. [Google Scholar]
- Zao, J.K.; Fan, S.C.; Wen, M.H.; Hsu, C.T.; Hung, C.H.; Hsu, S.H.; Chuang, M.C. Activity-oriented design of Health Pal: A smart phone for elders’ healthcare support. EURASIP J. Wirel. Commun. Netw. 2007, 2008, 1–10. [Google Scholar] [CrossRef][Green Version]
- Snyder, N.C.; Willoughby, C.A.; Smith, B.K. Comparison of the Polar V800 and the Garmin Forerunner 230 to predict VO2max. J. Strength Cond. Res. 2021, 35, 1403–1409. [Google Scholar] [CrossRef]
- Lobelo, F.; Kelli, H.; Tejedor, S.; Pratt, M.; McConnell, M.; Martin, S.S. The wild wild west: A framework to integrate mHealth software applications and wearables to support physical activity assessment, counseling and interventions for cardiovascular disease risk reduction. Prog. Cardiovasc. Dis. 2016, 58, 584–594. [Google Scholar] [CrossRef]
- Rawstorn, J.; Gant, N.; Meads, A.; Warren, I.; Maddison, R. Remotely delivered exercise-based cardiac rehabilitation: Design and content development of a novel mHealth platform. JMIR Mhealth Uhealth 2016, 4, e5501. [Google Scholar] [CrossRef]
- Alshurafa, N.; Sideris, C.; Pourhomayoun, M.; Kalantarian, H.; Sarrafzadeh, M.; Eastwood, J. Remote health monitoring outcome success prediction using baseline and first month intervention data. IEEE J. Biomed. Health Inform. 2016, 21, 507–514. [Google Scholar] [CrossRef]
- Paul-Chima, U.O.; Ugo, A.E.; Ben, O.M.; Ikechukwu, E.S.; Ejim, U.D. Integrating Wearable Health Monitoring Devices with IoT for Enhanced Personal Health Management: A Comprehensive Review. Data Process. 2024, 12, 13. [Google Scholar]
- Liaqat, M.; Mushtaq, M.; Jamil, A.; Mushtaq, M.M.; Ali, H.; Anwar, R.; Raza, A.; Aslam, A.; Tariq, T.; Hussain, M.; et al. Mobile Health Interventions: A Frontier for Mitigating the Global Burden of Cardiovascular Disease. Cureus 2024, 16, e62157. [Google Scholar] [CrossRef]
- Pepera, G.; Antoniou, V.; Su, J.J.; Lin, R.; Batalik, L. Comprehensive and personalized approach is a critical area for developing remote cardiac rehabilitation programs. World J. Clin. Cases 2024, 12, 2009. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Cheyney, M.; May, M.A.; Bovbjerg, M.L. Patient Experiences with an mHealth App for Complex Chronic Disease Care: Connections Despite Lack of Traditional Clinical Interactions. Patient Exp. J. 2024, 11, 97–106. [Google Scholar] [CrossRef]
- Cerfoglio, S.; Verme, F.; Capodaglio, P.; Rossi, P.; Cvetkova, V.; Boldini, G.; Galli, M.; Cimolin, V. Motor and Respiratory Tele-Rehabilitation in Patients with Long COVID-19 after Hospital Discharge: An Interventional Study. Life 2024, 14, 864. [Google Scholar] [CrossRef] [PubMed]
- Magnuson, K.I.; Li, K.; Beuley, G.; Ryan-Pettes, S.R. The Use of Non-Commercial Parent-Focused mHealth Interventions for Youth Behavior Problems: A Systematic Review. Available online: https://pdfs.semanticscholar.org/0200/3c52169f74e3977818568af8e8afe9b15bb7.pdf (accessed on 1 May 2024).
- Tejashwini, C.; Kumar, G.S.; Shekhar, R. Smart Pregnancy Watch with Location-Based Emergency Messaging, a Comprehensive Solution for Maternal Health Care. In International Conference on Microelectronics, Electromagnetics and Telecommunication; Springer Nature: Singapore, 2023; pp. 267–278. [Google Scholar]
- Ansar Bukhari, A.A. Leveraging Predictive Analytics for Enhanced Remote Patient Monitoring in Chronic Disease Management. Available online: https://www.researchgate.net/profile/Asad-Abbas-35/publication/382853000_Leveraging_Predictive_Analytics_for_Enhanced_Remote_Patient_Monitoring_in_Chronic_Disease_Management/links/66af248c2361f42f23b197f2/Leveraging-Predictive-Analytics-for-Enhanced-Remote-Patient-Monitoring-in-Chronic-Disease-Management.pdf (accessed on 1 May 2024).
- Fareed Musa, N.A. Real-Time Health Insights and Predictive Analytics in AI-Driven Healthcare. Available online: https://www.researchgate.net/profile/Nadeem-Ahmad-44/publication/382853336_Real-time_Health_Insights_and_Predictive_Analytics_in_AI-driven_Healthcare/links/66af301a51aa0775f268b0f8/Real-time-Health-Insights-and-Predictive-Analytics-in-AI-driven-Healthcare.pdf (accessed on 1 May 2024).
- Gardner, S.; Porbanderwala, A.; Haider, M. An Affordable Inkjet-Printed Foot Sole Sensor and Machine Learning for Telehealth Devices. IEEE Sens. Lett. 2023, 7, 1–4. [Google Scholar] [CrossRef]
- Seetharam, K.; Kagiyama, N.; Sengupta, P. Application of mobile health, telemedicine and artificial intelligence to echocardiography. Echo Res. Pract. 2019, 6, R41–R52. [Google Scholar] [CrossRef]
- Hinchliffe, N.; Capehart, M.; Bewick, M.; Feenie, J. The potential role of digital health in obesity care. Adv. Ther. 2022, 39, 4397–4412. [Google Scholar] [CrossRef]
- Rajapaksha, S.; Abhayarathne, W.J.A.; Kumari, S.G.K.; De Silva, M.V.L.U.; Wijesuriya, W.M.S.M. A Mobile Application to Predict and Manage High Blood Pressure and Personalized Recommendations. In Proceedings of the 2019 International Conference on Advancements in Computing (ICAC), Malabe, Sri Lanka, 5–7 December 2019; pp. 422–426. [Google Scholar]
- Chaithra, N.; Jha, J.; Sayal, A.; Gangodkar, A.R. 2 Internet of Medical Things with Artificial Intelligence for Improved Healthcare Systems. In Smart Healthcare Systems: AI and IoT Perspectives; CRC Press: Boca Raton, FL, USA, 2024. [Google Scholar]
- Arefin, S. Leveraging AI for Healthcare Advancement in Africa. Acad. J. Sci. Technol. 2024, 7, 1–11. [Google Scholar]
- Bobet, D.; Shabir, G. The Future of Chronic Disease Management: AI-Driven Healthcare and Predictive Analytics. Available online: https://www.researchgate.net/profile/Ghulam-Shabir-18/publication/382853264_The_Future_of_Chronic_Disease_Management_AI-driven_Healthcare_and_Predictive_Analytics/links/66af2d6f299c327096ac1e1f/The-Future-of-Chronic-Disease-Management-AI-driven-Healthcare-and-Predictive-Analytics.pdf (accessed on 1 May 2024).
- Hogan, T.P.; Sherman, S.E.; Dardashti, N.; McMahon, N.; Slightam, C.; Zulman, D.M. Realizing Virtual Care in VA: Supporting the Healthcare System’s Journey Towards Enhanced Access, Engagement, and Outcomes. J. Gen. Intern. Med. 2024, 39 (Suppl. 1), 1–4. [Google Scholar] [CrossRef]
- Selin, R.; Bandur, P.M.; Manggul, M.S. Comprehensive Midwifery Care In Pregnancy With Hepatitis B: Case Study. In Prosiding Seminar Internasional Scope of Practice of Nursing and Midwifery; Ruteng: Flores, Indonesia, 2023; Volume 1, No. 1, pp. 51–59. Available online: https://jurnal.unikastpaulus.ac.id/index.php/ispnm/article/view/2505 (accessed on 1 May 2024).
- Koloi, A.; Loukas, V.S.; Hourican, C.; Sakellarios, A.I.; Quax, R.; Mishra, P.P.; Lehtimäki, T.; Raitakari, O.T.; Papaloukas, C.; Bosch, J.A.; et al. Predicting early-stage coronary artery disease using machine learning and routine clinical biomarkers improved by augmented virtual data. Eur. Heart J.-Digit. Health 2024, ztae049. [Google Scholar] [CrossRef]
- Marcus, C. 11 Digital management of childhood obesity. BMJ Paediatr. Open 2024, 8. [Google Scholar] [CrossRef]
- Angelini, C.I. Development of the precision diagnostics and treatment for duchenne/becker muscular dystrophy. Front. Neurol. 2024, 15, 1396816. [Google Scholar] [CrossRef] [PubMed]
- Sáez Carazo, M. Empowering Cardiovascular Disease Diagnosis with Machine and Deep Learning Approaches. 2024. Available online: http://his.diva-portal.org/smash/record.jsf?pid=diva2%3A1883247&dswid=553 (accessed on 1 May 2024).
- Rawat, B.S.; Srivastava, A.; Garg, N. Health Monitoring Transforming Using IoT: A Review. In Proceedings of the 2024 IEEE International Conference on Computing, Power and Communication Technologies (IC2PCT), Greater Noida, India, 9–10 February 2024; Volume 5, pp. 17–22. [Google Scholar]
- Rojas-Valverde, D. Understanding Sports-Related Health Issues. J. Funct. Morphol. Kinesiol. 2024, 9, 136. [Google Scholar] [CrossRef]
- Moghadam, S.; Airaksinen, M.; Nevalainen, P.; Marchi, V.; Hellstrom-Westas, L.; Stevenson, N. An automated bedside measure for monitoring neonatal cortical activity: A supervised deep learning-based electroencephalogram classifier with external cohort validation. Lancet Digit. Health 2022, 4, e884–e892. [Google Scholar] [CrossRef]
- Shiwani, M.; Chico, T.; Ciravegna, F.; Mihaylova, L. Continuous Monitoring of Health and Mobility Indicators in Patients with Cardiovascular Disease: A Review of Recent Technologies. Sensors 2023, 23, 5752. [Google Scholar] [CrossRef]
- Sheikh, A.; Sobotka, P.; Garg, I.; Dunn, J.; Minhas, A.; Shandhi, M. Blood Pressure Variability in Clinical Practice: Past, Present and the Future. J. Am. Heart Assoc. 2023, 12, e029297. [Google Scholar] [CrossRef]
- Han, S.; Rezaee, M.; Roghanchi, P. Effect of physicochemical properties on critical sinking and attachment of respirable coal mine dust impacting on a water surface. Chem. Eng. Sci. 2024, 120588. [Google Scholar] [CrossRef]
- Ahuja, A.; Agrawal, S.; Acharya, S.; Reddy, V.; Batra, N.; Reddy, V.; Batra, N. Strategies for Cardiovascular Disease Prevention in Type 1 Diabetes: A Comprehensive Review. Cureus 2024, 16, e66420. [Google Scholar] [CrossRef]
- Subasi, A.; Bandic, L.; Qaisar, S.M. Cloud-based health monitoring framework using smart sensors and smartphone. In Innovation in Health Informatics; Academic Press: Cambridge, MA, USA, 2020; pp. 217–243. [Google Scholar]
- Ahmad, I.; Asghar, Z.; Kumar, T.; Li, G.; Manzoor, A.; Mikhaylov, K.; Shah, S.A.; Höyhtyä, M.; Reponen, J.; Huusko, J.; et al. Emerging technologies for next generation remote health care and assisted living. IEEE Access 2022, 10, 56094–56132. [Google Scholar] [CrossRef]
- Urbano, M.C.A.; Arellano, R.A.; Dizon, S.R.; Foja, N.D.; Galgana, J.; Terrado, L.G.; Tuazon, P.N.; Navidad, F. Preferences of Medical Technology Students on COVID-19 Personal Preventive Behaviors and University Safety Protocols: A Conjoint Analysis. J. Med. Univ. St. Tomas 2024, 8, 1362–1370. [Google Scholar] [CrossRef]
- Zhao, M.; Song, J.; Zhou, D.; Song, J. Advancements in Anthracycline-Induced Cardiotoxicity Research: A Cross-Sectional Analysis of Interventional Clinical Trials from the International Clinical Trial Registration Platform. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4915063 (accessed on 1 May 2024).
- Garcia, M.C.A. Predictive Model for Coal Workers Pneumoconiosis (CWP) Risk in the US. Master’s Thesis, New Mexico Institute of Mining and Technology, Socorro, NM, USA, 2024. [Google Scholar]
- Jung, C.; Wolff, G.; Wernly, B.; Bruno, R.R.; Franz, M.; Schulze, P.C.; Silva, J.N.A.; Silva, J.R.; Bhatt, D.L.; Kelm, M. Virtual and augmented reality in cardiovascular care: State-of-the-art and future perspectives. Cardiovasc. Imaging 2022, 15, 519–532. [Google Scholar]
- Vervoort, D.; Swain, J.D.; Pezzella, A.T.; Kpodonu, J. Cardiac surgery in low-and middle-income countries: A state-of-the-art review. Ann. Thorac. Surg. 2021, 111, 1394–1400. [Google Scholar] [CrossRef]
- Nazi, F.; Abbas, A. Personalized Medicine and Health Data Integration: Transforming Chronic Disease Monitoring with AI. Available online: https://www.researchgate.net/profile/Asad-Abbas-35/publication/382853245_Personalized_Medicine_and_Health_Data_Integration_Transforming_Chronic_Disease_Monitoring_with_AI/links/66af28aa299c327096ac1dc9/Personalized-Medicine-and-Health-Data-Integration-Transforming-Chronic-Disease-Monitoring-with-AI.pdf (accessed on 1 May 2024).
- Alradwan, I.; ALFayez, N.; Alomary, M.N.; Alshehri, A.A.; Aodah, A.H.; Almughem, F.A.; Alsulami, K.A.; Aldossary, A.M.; Alawad, A.O.; Tawfik, Y.M.; et al. Emerging Trends and Innovations in the Treatment and Diagnosis of Atherosclerosis and Cardiovascular Disease: A Comprehensive Review towards Healthier Aging. Pharmaceutics 2024, 16, 1037. [Google Scholar] [CrossRef]
- Dobbie, L.; Tahrani, A.; Alam, U.; James, J.; Wilding, J.; Cuthbertson, D. Exercise in obesity—The role of technology in health services: Can this approach work? Curr. Obes. Rep. 2021, 11, 93–106. [Google Scholar] [CrossRef]
- Itchhaporia, D.; Baliga, R.; Bossone, E. Digital Transformation in Medicine to Enhance Quality of Life, Longevity, and Health Equity. Heart Fail. Clin. 2022, 18, xi–xiii. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, M.; Buman, M.; Haskell, W.; McConnell, M.; Carstensen, L. 24 hours of sleep, sedentary behavior, and physical activity with nine wearable devices. Med. Sci. Sports Exerc. 2016, 48, 457–465. [Google Scholar] [CrossRef]
- Perez-Pozuelo, I.; Zhai, B.; Palotti, J.; Mall, R.; Aupetit, M.; Garcia-Gomez, J.M.; Taheri, S.; Guan, Y.; Fernandez-Luque, L. The future of sleep health: A data-driven revolution in sleep science and medicine. NPJ Digit. Med. 2020, 3, 42. [Google Scholar] [CrossRef]
- de Zambotti, M.; Goldstein, C.; Cook, J.; Menghini, L.; Altini, M.; Cheng, P.; Robillard, R. State of the science and recommendations for using wearable technology in sleep and circadian research. Sleep 2023, 47, zsad325. [Google Scholar] [CrossRef]
- Ditschman, E. Am I Ready to Use a Portable Artificial Kidney or a Wearable Artificial Kidney? Kidney360 2024, 5, 1035–1036. [Google Scholar] [CrossRef]
- Khera, R.; Oikonomou, E.K.; Nadkarni, G.N.; Morley, J.R.; Wiens, J.; Butte, A.J.; Topol, E.J. Transforming Cardiovascular Care With Artificial Intelligence: From Discovery to Practice: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2024, 84, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Pizzoli SF, M.; Durosini, I.; Strika, M.; Pravettoni, G. Artificial intelligence and digital worlds: New frontiers of integration between AI and other technological tools. In Artificial Intelligence for Medicine; Academic Press: Cambridge, MA, USA, 2024; pp. 63–72. [Google Scholar]
- Hrabovska, N.; Kajati, E.; Zolotova, I. A validation study to confirm the accuracy of wearable devices based on health data analysis. Electronics 2023, 12, 2536. [Google Scholar] [CrossRef]
- Rabinovich, E.P.; Capek, S.; Kumar, J.S.; Park, M.S. Tele-robotics and artificial-intelligence in stroke care. J. Clin. Neurosci. 2020, 79, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, M.A.; Qureshi, K.N.; Jeon, G.; Piccialli, F. Vida asistida por el entorno basada en aprendizaje profundo para la autogestión de afecciones cardiovasculares. Neural Comput. Appl. 2022, 34, 10449–10467. [Google Scholar] [CrossRef]
- Souza, J.; Escadas, S.; Baxevani, I.; Rodrigues, D.; Freitas, A. Smart Wearable Systems for the Remote Monitoring of Selected Vascular Disorders of the Lower Extremity: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 15231. [Google Scholar] [CrossRef] [PubMed]
- Yuninda, S.P.; Aga Pasma, S.; Mantoro, T. Patient Data Security in Telemedicine Services from Data Misuse in Health Practice. In Proceedings of the 2022 IEEE 8th International Conference on Computing, Engineering and Design (ICCED), Sukabumi, Indonesia, 28–29 July 2022; pp. 1–4. [Google Scholar] [CrossRef]
- Basatneh, R.; Najafi, B.; Armstrong, D.G. Health Sensors, Smart Home Devices, and the Internet of Medical Things: An Opportunity for Dramatic Improvement in Care for the Lower Extremity Complications of Diabetes. J. Diabetes Sci. Technol. 2018, 12, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Houser, S.H.; Flite, C.A.; Foster, S.L. Privacy and Security Risk Factors Related to Telehealth Services—A Systematic Review. Perspect. Health Inf. Manag. 2023, 20, 1f. [Google Scholar] [PubMed] [PubMed Central]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. E-Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef]
- Zhang, H.; Sun, S.; Meng, F. A high-capacity and reversible patient data hiding scheme for telemedicine. Biomed. Signal Process. Control 2022, 76, 103706. [Google Scholar] [CrossRef]
- Razali, R.A.; Jamil, N. A Quick Review of Security Issues in Telemedicine. In Proceedings of the 2020 8th International Conference on Information Technology and Multimedia (ICIMU), Selangor, Malaysia, 24–26 August 2020; pp. 162–165. [Google Scholar] [CrossRef]
- Caldarola, P.; Murrone, A.; Roncon, L.; Di Pasquale, G.; Tavazzi, L.; Amodeo, V.; Aspromonte, N.; Cipriani, M.; Di Lenarda, A.; Domenicucci, S.; et al. ANMCO POSITION PAPER: The reorganization of cardiology in times of the SARS-CoV-2 pandemic. Eur. Heart J. Suppl. 2021, 23, C154–C163. [Google Scholar] [CrossRef] [PubMed]
- Kańtoch, E.; Kańtoch, A. Cardiovascular and Pre-Frailty Risk Assessment during Shelter-In-Place Measures Based on Multimodal Biomarkers Collected from Smart Telemedical Wearables. J. Clin. Med. 2021, 10, 1997. [Google Scholar] [CrossRef] [PubMed]
- Dagher, L.; Nedunchezhian, S.; El Hajjar, A.H.; Zhang, Y.; Deffer, O., Jr.; Russell, A.; Pottle, C.; Marrouche, N. A cardiovascular clinic patients’ survey to assess challenges and opportunities of digital health adoption during the COVID-19 pandemic. Cardiovasc. Digit. Health J. 2022, 3, 31–39. [Google Scholar] [CrossRef]
- Ding, X.; Clifton, D.; Ji, N.; Lovell, N.H.; Bonato, P.; Chen, W.; Yu, X.; Xue, Z.; Xiang, T.; Long, X.; et al. Wearable Sensing and Telehealth Technology with Potential Applications in the Coronavirus Pandemic. IEEE Rev. Biomed. Eng. 2020, 14, 48–70. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, A.; Patel, S.; Dubey, K. Digital cardiovascular care in COVID-19 pandemic: A potential alternative? J. Cardiac. Surg. 2020, 35, 3545–3550. [Google Scholar] [CrossRef] [PubMed]
- Roberto Cesar, M.O.; German, L.B.; Paola Patricia, A.C.; Eugenia, A.R.; Elisa Clementina, O.M.; Jose, C.O.; Marlon Alberto, P.M.; Fabio Enrique, M.P.; Margarita, R.V. Method Based on Data Mining Techniques for Breast Cancer Recurrence Analysis. In Advances in Swarm Intelligence. ICSI 2020; Tan, Y., Shi, Y., Tuba, M., Eds.; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2020; Volume 12145. [Google Scholar] [CrossRef]
- Echeverri-Ocampo, I.; Urina-Triana, M.; Ariza, P.P.; Mantilla, M. El trabajo colaborativo entre ingenieros y personal de la salud para el desarrollo de proyectos en salud digital: Una visión al futuro para lograr tener éxito. Arch. Venez. De Farmacol. Y Ter. 2018, 37, 400–405. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).