Abstract
Background: Single-Anastomosis Duodenoileostomy with Sleeve Gastrectomy (SADI-S) has been reported as both a safe and effective surgical procedure. However, these findings have not been directly compared to those of more established and less complex procedures, such as Sleeve Gastrectomy (SG), which remains the most commonly performed technique in Metabolic and Bariatric Surgery (MBS). Objective: This study aimed to assess and contrast the intraoperative and postoperative outcomes between patients who underwent SADI-S and those who underwent SG. Methods: A systematic review and meta-analysis were performed and registered under PROSPERO with the ID CRD42024532504. A comprehensive search strategy was executed on 15 April 2024, covering PubMed, Embase, Cochrane Library, Scopus, Web of Science, and Science Direct from the first reports to March 2024. The search strategy incorporated relevant keywords, including: “SADI-S” OR “Single Anastomosis Duodenal-Ileal bypass” and “Sleeve Gastrectomy”. We included studies comparing adult patients (≥18 years old) undergoing SADI-S and SG, reporting at least one clinical outcome of interest. Results: Five studies published between 2019 and 2023, comprising 3593 patients, were included. Of these, 461 patients (12.8%) underwent SADI-S, while 3132 (87.2%) underwent SG. The mean patient age was 42.96 years, with 89.6% female participants. Patients undergoing SADI-S had a significantly higher Body Mass Index (BMI) than those undergoing SG (Mean: 49.73 ± 8.10 vs. 45.64 ± 7.84; Mean Difference [MD]: 3.83, 95% CI: 0.52–7.14; p = 0.02) and an increased risk of hypertension (OR: 1.38, 95% CI: 1.04–1.84; p = 0.03). SADI-S also resulted in longer operative times (125.63 ± 51.91 min vs. 49.67 ± 26.07 min; MD: 65.97 min, 95% CI: 61.71–70.25; p < 0.001) and length of hospital stay (2.30 ± 2.76 days vs. 1.21 ± 0.81 days; MD: 1.03 days, 95% CI: 0.70–1.37; p < 0.001). Moreover, patients who underwent SADI-S demonstrated a significantly higher risk of postoperative complications, such as readmissions and reinterventions (OR: 3.17, 95% CI: 2.15–4.67; p < 0.001), and experienced greater excess weight loss (MD: 12.42%, 95% CI: 0.92–23.92; p = 0.03). No significant differences were observed between the groups regarding age, sex, or the prevalence of obstructive sleep apnea (OSA). Conclusions: SADI-S appears to be a promising surgical technique for facilitating substantial weight loss in individuals with severe obesity. Given the higher risk of postoperative complications associated with SADI-S, careful evaluation and personalized decision-making for patient selection and education are essential to optimize clinical and safety outcomes.
1. Introduction
The global obesity epidemic presents major health challenges in the twenty-first century. Although lifestyle modifications are fundamental in managing both conditions, their long-term effectiveness can be limited. Metabolic and Bariatric Surgery (MBS), originally intended for weight management, has progressively become a powerful intervention that not only facilitates weight reduction but also contributes to the remission and possible resolution of various obesity-related conditions [1,2]. Various types of MBS procedures are available for clinical application, including Roux-en-Y Gastric Bypass (RYGB), Sleeve Gastrectomy (SG), Biliopancreatic Diversion with Duodenal Switch (BPD-DS), and Adjustable Gastric Band (AGB) [3].
According to the latest reports from the American Society for Metabolic and Bariatric Surgery (ASMBS), Sleeve Gastrectomy (SG) is the most widely performed metabolic and bariatric surgery technique globally [4]. However, the Single-Anastomosis Duodenoileostomy with Sleeve Gastrectomy (SADI-S), a relatively recent addition to MBS procedures, ranks sixth. It was introduced in 2007 and presents itself as a compelling alternative to traditional methods due to its potential benefits [5].
Multiple studies have previously demonstrated that SADI-S is a safe and effective surgical procedure, offering sustained weight loss and a high rate of resolution for obesity-related comorbidities over the mid-to-long term [6,7,8]. Outcomes of patients undergoing SADI-S have been evaluated in comparison to other hypoabsorptive procedures, demonstrating promising results [7].
Despite being performed for over a decade, the outcomes of SADI-S have not been thoroughly and directly compared to those of the widely practiced Sleeve Gastrectomy (SG). This systematic review and meta-analysis sought to evaluate and contrast the intraoperative and postoperative outcomes of patients undergoing SADI-S with those undergoing SG.
To the best of our knowledge, this study is the first to utilize this specific methodology for a direct comparison between SADI-S and SG. By focusing on a direct comparison of outcomes within the same analysis, this research adds to the existing literature by providing insights that may help refine surgical decision-making and contribute to understanding the relative benefits and risks of these techniques.
2. Results
2.1. Studies Selection
The initial search across four databases retrieved a total of 1092 records, of which 421 were identified as duplicates and subsequently removed. Screening of the remaining 671 titles and abstracts led to the selection of 17 studies for full-text evaluation based on predefined inclusion and exclusion criteria. After a comprehensive assessment, data extraction was performed from five eligible English-language articles. The study selection process, along with the reasons for exclusion, is depicted in the PRISMA flowchart (Figure 1), generated using the online tool by Haddaway et al. [9].
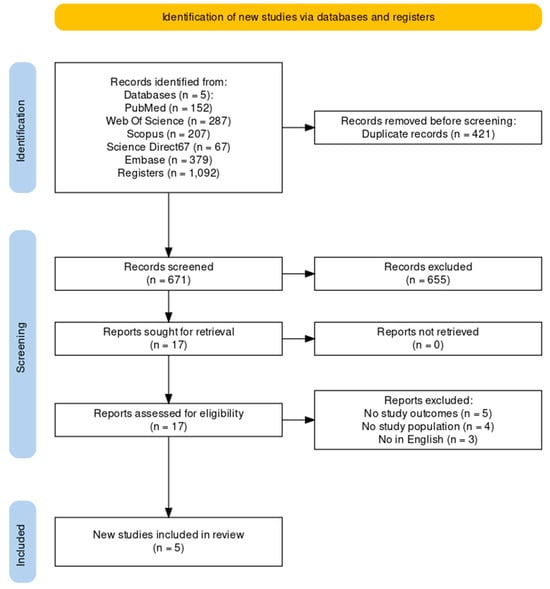
Figure 1.
Search outputs based on PRISMA guidelines [10].
2.2. Study Characteristics
The selected studies were published over a span of four years, from 2019 to 2023. All of them were observational studies, three being cross-sectional and two cohorts, and included patients’ data from one to three years. Three studies were from the USA, and one was from Italy and Romania. A detailed summary of the included studies, along with the characteristics of the study population, is provided in Table 1.

Table 1.
Study characteristics.
2.3. Outcomes of SADI-S and SG
2.3.1. Results of Syntheses
A total of 3593 patients were included in this study, comprising 461 (12.8%) who underwent SADI-S and 3132 (87.2%) who underwent SG. The cohort had a mean age of 42.96 years, with females accounting for an average of 89.6% of the study population.
2.3.2. Age and Sex in Patients Undergoing SADI-S vs. SG
We evaluated the differences in age (Figure 2A) and sex (Figure 2B) in 3593 patients, 461 (12.83%) underwent SADI-S and 3132 (87.17%) underwent SG. A pooled odds ratio was computed to assess the proportion of female patients, while the mean age difference between the two groups was analyzed separately. The findings revealed no statistically significant differences in either parameter.

Figure 2.
Forest plots comparing age (A) and female sex (B) between patients undergoing SADI-S and SG. Panel A presents the mean difference in age, while Panel B shows the odds ratio for female sex.
2.3.3. BMI in Patients Undergoing SADI-S vs. SG
We evaluated the mean difference in BMI among 3547 patients who underwent SADI-S (n = 458, 12.91%) or SG (n = 3089, 87.88%), resulting in patients undergoing SADI-S having a higher BMI than those undergoing SG (MD = 3.83, 95% CI = 0.52–7.14, p = 0.02) (Figure 3).
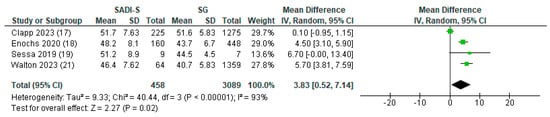
Figure 3.
BMI in patients undergoing SADI-S vs. SG.
2.3.4. Obesity-Associated Diseases in Patients Undergoing SADI-S vs. SG
A pooled odds ratio analysis was conducted for obesity-related comorbidities among 1516 patients, including 234 (15.43%) who underwent SADI-S and 1282 (84.56%) who underwent SG. Hypertension and obstructive sleep apnea (OSA) were the only conditions consistently reported across multiple studies. The analysis revealed that patients undergoing SADI-S had a significantly higher likelihood of hypertension compared to those undergoing SG (OR = 1.38, 95% CI = 1.04–1.84, p = 0.03) (Figure 4A). However, no significant association was observed between the surgical procedure and OSA prevalence (OR = 1.22, 95% CI = 0.92–1.61, p = 0.17) (Figure 4B).
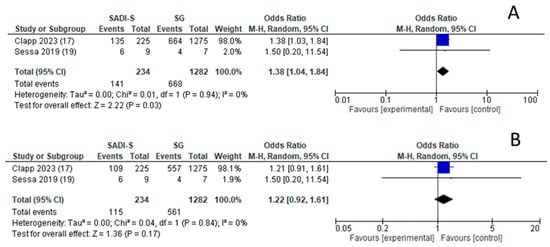
Figure 4.
Obesity-associated diseases in patients undergoing SADI-S vs. SG.
2.3.5. Operating Time (OT) in Patients Undergoing SADI-S vs. SG
We evaluated the mean difference in OT among 2939 patients who underwent SADI-S (n = 298, 10.14%) or SG (n = 2641, 89.86%) resulting in patients undergoing SADI-S having a higher OT with a MD of 65.97 min over SG (95% CI=61.71–70.25, p < 0.001) (Figure 5).
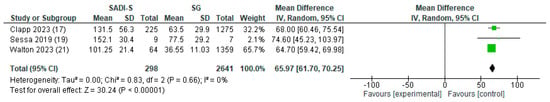
Figure 5.
OT in patients undergoing SADI-S vs. SG.
2.3.6. Length of Stay (LOS) in Patients Undergoing SADI-S vs. SG
The mean difference in length of stay (LOS) was analyzed among 1516 patients, including 234 (15.43%) who underwent SADI-S and 1282 (84.56%) who underwent SG. The results indicated that patients undergoing SADI-S experienced a significantly longer hospital stay, with a mean difference (MD) of 1.03 days compared to SG (95% CI = 0.70–1.37, p < 0.001) (Figure 6).
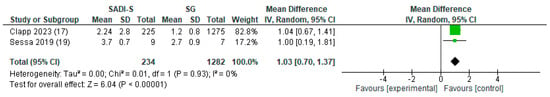
Figure 6.
Length of stay in patients undergoing SADI-S vs. SG.
2.3.7. Postoperative Events in Patients Undergoing SADI-S vs. SG
We evaluated the pooled odds ratio (OR) for postoperative events in the first 30 days postoperative, including complications, readmission, and reoperation. A total of 2923 patients who underwent either SADI-S (n = 289, 9.88%) or SG (n = 2634, 90.11%) were included. Our analysis revealed that patients undergoing SADI-S faced a significantly higher risk of postoperative events compared to those who underwent SG (OR = 3.17, 95% CI = 2.15–4.67, p < 0.001) (Figure 7). However, subgroup analysis indicated that this elevated risk was statistically significant only for readmission, with SADI-S patients demonstrating a greater likelihood of readmission compared to SG patients (OR = 2.14, 95% CI = 1.08–4.26).
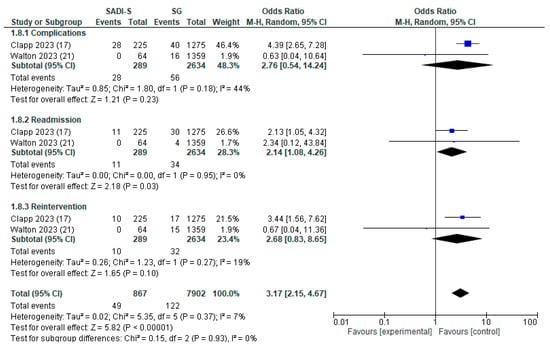
Figure 7.
30 days postoperative events in patients undergoing SADI-S vs. SG.
2.4. %EWL at 2 Years in Patients Undergoing SADI-S vs. SG
We evaluated the mean difference in LOS among 624 patients who underwent SADI-S (n = 169, 27.08%) or SG (n = 455, 72.91%), resulting in patients undergoing SADI-S having a higher %EWL with an MD of 12.42% (95% CI = 0.92–23.92, p = 0.03) at 12 months (Figure 8).
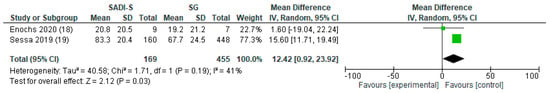
Figure 8.
%EWL at 2 years in patients undergoing SADI-S vs. SG.
2.4.1. Heterogeneity and Risk of Bias Across Studies
The degree of heterogeneity varied across the evaluated outcomes: Age: I2= 71%; percentage of female: I2 = 55%, BMI: I2 = 93%, Hypertension and OSA: I2 = 0%, OT and LOS: I2 = 0%, postoperative events: I2 = 7%, and %EWL: I2 = 41%.
Figure 9 illustrates the comparison-adjusted funnel plots alongside the Egger test results for various outcomes. The Egger test suggested potential publication bias (p < 0.1) in studies evaluating postoperative complications, readmission, and reintervention. However, due to the limited number of studies, the test could not be conducted for %EWL and LOS. For OT, the Egger test did not indicate any evidence of publication bias (p = 0.357).
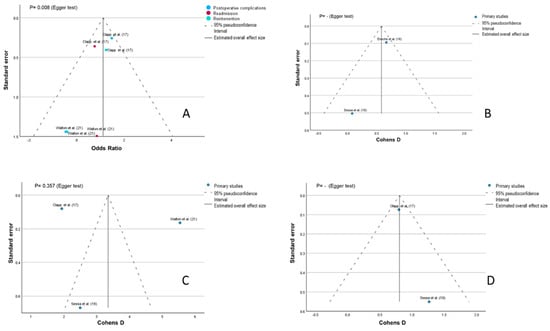
Figure 9.
Funnel plots and Egger test for outcomes based on SADI-S vs. SG (A) postoperative events, (B) %EWL, (C) Operating time, (D) length of stay.
2.4.2. Quality Assessment
The Newcastle–Ottawa Scale assessment results are presented in Table S1 of the Supplementary Materials. Most studies received scores ranging from 6 to 9, with a median score of 7.4, classifying them as good-quality studies.
3. Materials and Methods
3.1. Study Design
A systematic review and meta-analysis were conducted to explore potential differences in intraoperative and postoperative outcomes between SADI-S and SG. The review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the ID CRD42024532504. This study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P 2020) guidelines [16]. Formal ethical approval was not required or feasible, as this study utilized de-identified data from previously published primary studies. The study population comprised patients with severe obesity who underwent metabolic and bariatric surgery (MBS). We analyzed outcomes in patients who underwent SADI-S compared to those who underwent SG alone. The primary outcomes evaluated included length of hospital stay (LOS), operative time (OT), reoperation rates, and the overall incidence of complications.
3.2. Information Sources and Search Strategy
A comprehensive search strategy was designed to explore multiple databases, including PubMed, Embase, Cochrane Library, Scopus, Web of Science, and ScienceDirect. Systematic searches were performed from each database’s inception up to March 2024. The search terms incorporated keywords such as “SADI-S” OR “Single Anastomosis Duodenal-Ileal Bypass” AND “Sleeve Gastrectomy”. A detailed search strategy, along with the full list of search terms, is provided in Table S2 of the Supplementary Materials. The database search was conducted on 15 April 2024.
3.3. Study Selection
Two independent reviewers conducted an initial screening of titles and abstracts to assess relevance based on predefined inclusion and exclusion criteria. Full texts of potentially eligible studies were then reviewed for final inclusion. Any disagreements between reviewers were resolved through discussion or consultation with a third reviewer. Studies were included if they directly compared adult patients (≥18 years) undergoing SADI-S and SG within the same study and reported at least one relevant clinical outcome. Eligible study designs were limited to cohort, case–control, and cross-sectional studies. Exclusion criteria included studies with overlapping populations, non-English publications, and animal studies. No restrictions were imposed on sample size or publication date.
3.4. Data Extraction
Data extraction was performed independently by two reviewers using a standardized Microsoft Excel template. The extracted information included study characteristics (publication year, country of origin, sample size, study design, study period, and type of MBS procedure), patient demographics (age, sex, body mass index [BMI], and obesity-related comorbidities), as well as intraoperative and postoperative outcomes. The assessed outcomes encompassed length of hospital stay, operative time, reoperation and readmission rates, overall complication rate, and percentage of excess weight loss (%EWL).
3.5. Bias and Quality Assessment
The quality of observational studies was assessed using the Newcastle–Ottawa Scale (NOS), with two independent reviewers conducting the evaluations. The NOS assigns a total score ranging from 0 to 9 stars, classifying studies as high quality (7–9), medium quality (4–6), and poor quality (<4) [17]. Any discrepancies between reviewers were resolved through discussion or, if necessary, by consulting a third reviewer.
3.6. Statistical Analysis
Binary outcomes were analyzed using pooled odds ratios (OR) with 95% confidence intervals, while continuous outcomes were evaluated using weighted mean differences (WMD). The results were presented in tabular format, summarizing study and patient characteristics, and visually illustrated through forest plots. Heterogeneity was assessed using the I2 statistic, categorized as follows: substantial (≥75%), moderate (25%–75%), and low (<25%), in accordance with Higgins et al. [18]. A p-value < 0.10 and an I2 > 25% were considered indicative of significant heterogeneity. For pooled outcomes with high heterogeneity, the DerSimonian and Laird random-effects model was employed [19].
Statistical analyses were performed using Review Manager 5.4 (Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) and SPSS V.29. To mitigate potential confounding factors in the comparison between SADI-S and SG, a subgroup analysis was conducted based on postoperative events, including complications, readmission rates, and reintervention rates.
Publication bias was evaluated through visual inspection of funnel plots to assess the symmetry of trial distributions, supplemented by Egger’s test. An asymmetrical funnel plot combined with a p-value < 0.1 on Egger’s test was considered indicative of publication bias [20].
4. Discussion
This systematic review and meta-analysis evaluated preoperative characteristics and surgical outcomes in patients undergoing SADI-S versus SG. The findings from the five included studies indicated that the SG group had significantly shorter operative times, reduced postoperative hospital stays, and fewer readmissions compared to the SADI-S group. However, patients undergoing SADI-S achieved a greater percentage of excess weight loss.
Regarding the operative time, our meta-analysis supports that SG is associated with a shorter operative time than SADI-S. This difference may be attributed to the greater complexity of the SADI-S procedure, which combines a duodenoileal anastomosis with sleeve gastrectomy [21]. Additionally, the surgeon’s learning curve may have influenced these outcomes, as SADI-S is a relatively newer procedure compared to SG, which remains the most frequently performed metabolic and bariatric surgery in the United States [4]. Although there are limited data to establish a definitive learning curve, some studies have suggested the number of cases required to achieve competency and proficiency in SADI-S. Pennestri et al. and Wang et al. reported a learning curve of 50 and 58 cases, respectively, for SADI-S, whereas only 19 cases were needed to achieve a decrease in operative time for SG [22,23].
The prolonged length of stay observed in patients who underwent SADI-S compared to SG might be attributable to the longer operative time associated with this procedure. Longer operative times often correlate with the complexity of surgeries, potentially increasing the risk of intraoperative complications such as bleeding, leaks, or infections [24,25]. Hence, SADI-S could entail complications arising from both the sleeve component and the duodenoileostomy, possibly resulting in a higher cumulative occurrence of complications [21]. These complications may necessitate intensified postoperative monitoring and interventions, extending hospital stays. Moreover, a longer length of stay has been linked to elevated rates of readmissions [26]. Our analysis revealed that patients who underwent SADI-S exhibited higher rates of readmissions compared to those who underwent SG, possibly due to a higher incidence of postoperative complications. However, it is essential to note that, due to a lack of information, we did not specifically analyze individual postoperative outcomes such as bleeding or leaks, which could contribute to the increased readmission rates for SADI-S patients. Furthermore, as these results come from only two studies, it should be considered the possible effect of the specific learning curve of the surgeons in each study that performed the SADI-S. Randomized control trials that study SADI-S postoperative outcomes are imperative to elucidate this aspect further and provide clearer insights into the factors influencing readmission rates following MBS procedures.
The findings of this meta-analysis indicate that the percentage of excess weight loss after one year was greater with SADI-S than with SG. This difference may be attributed to SADI-S combining both hypoabsorptive and restrictive mechanisms, whereas SG primarily relies on restriction, leading to more rapid weight loss in the short term [27]. SADI-S emerges as a compelling option for patients requiring rapid and more significant weight loss to become eligible candidates for additional surgical interventions such as joint replacements, ventral hernia repair, or solid-organ transplantation [28,29,30].
This systematic review contributes to the understanding of the safety and feasibility of SADI-S. In addition, it is the first study of its kind to compare SADI-S and SG with this methodology. However, a key limitation of this review is the relatively small number of studies included. Additionally, since all five studies were observational, there is a clear need for high-quality research to further investigate strategies for optimizing surgical outcomes following SADI-S. In this systematic review, the study population warrants careful consideration, as three of the included studies were conducted in the USA, where BMI tends to be higher compared to European populations [31]. These regional differences emphasize the need to account for demographic and healthcare system variations when applying findings from American cohorts to European clinical practice. Therefore, these differences must be taken into account when conducting a thorough review of the relevant studies. Additionally, substantial heterogeneity was observed among the analyzed studies regarding age, sex, and BMI, which may have limited the identification of statistically significant associations for these variables. Additionally, publication bias was recorded for studies considering postoperative events, while other variables could not be calculated. The limited number of included studies precluded a comprehensive meta-regression or sensitivity analysis to further explore the observed heterogeneity, which may have also impacted the assessment of potential bias.
Future directions and ideas for new research should focus on the analysis of the relationship between SADI-S and other widely performed MBS procedures with multiple mechanisms of action including hypoabsorption, restriction, and hormonal effects on patients at risk due to their severe obesity. These procedures encompass the one-anastomosis gastric bypass (OAGB), the single-anastomosis sleeve ileal bypass (SASI), and the more recently introduced sleeve gastrectomy with transit bipartition.
5. Conclusions
These results suggest that SADI-S is a viable surgical option for achieving significant weight reduction in individuals with severe obesity, presenting a compelling alternative to the more commonly performed SG. However, the associated longer operative times, extended hospital stays, and increased readmission rates should be carefully considered when selecting the optimal bariatric procedure for individual patients. It is imperative to underscore the importance of individualized care. Given the higher risk of postoperative complications associated with SADI-S, careful evaluation and personalized decision-making with wise patient selection and rehabilitation are essential to optimize safety outcomes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/gidisord7020027/s1, Table S1: Quality assessment of included studies based on the Newcastle Ottawa scale. Search Table S2: terms for the meta-analysis in PubMed, Scopus, Web of Science, and Science Direct databases.
Author Contributions
Conceptualization, Y.R.-M. and R.J.O.; methodology, D.C., S.P., W.Y. and L.M.; data curation, Y.R.-M., A.Z., S.R.-C. and V.B.-M.; formal analysis, A.Z., D.S.-M. and A.G.; validation, A.Z., D.S.-M. and A.G.; investigation, Y.R.-M., A.Z., S.R.-C. and V.B.-M.; resources, Y.R.-M.; writing—original draft preparation, Y.R.-M., A.Z., S.R.-C., V.B.-M., D.S.-M. and A.G.; writing—review and editing, A.G., A.E., R.D.-P., D.C., W.Y., L.M., A.A.-M. and R.J.O.; visualization, Y.R.-M. and A.Z.; supervision, W.Y., L.M., A.A.-M. and R.J.O.; project administration, R.J.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Acknowledgments
This study was conducted on behalf of TROGSS—The Robotic Global Surgical Society. We extend our gratitude to the society and its members for their support and commitment to advancing robotic surgical education and research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- American Diabetes Association 7. Obesity Management for the Treatment of Type 2 Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S65–S72. [Google Scholar] [CrossRef] [PubMed]
- Xiao, N.; Ding, Y.; Cui, B.; Li, R.; Qu, X.; Zhou, H.; Au, K.; Fan, X.; Xie, J.; Huang, Y.; et al. Navigating Obesity: A Comprehensive Review of Epidemiology, Pathophysiology, Complications and Management Strategies. TIME 2024, 2, 100090. [Google Scholar] [CrossRef]
- Schauer, P.R.; Kashyap, S.R.; Wolski, K.; Brethauer, S.A.; Kirwan, J.P.; Pothier, C.E.; Thomas, S.; Abood, B.; Nissen, S.E.; Bhatt, D.L. Bariatric Surgery versus Intensive Medical Therapy in Obese Patients with Diabetes. N. Engl. J. Med. 2012, 366, 1567–1576. [Google Scholar] [CrossRef] [PubMed]
- Estimate of Bariatric Surgery Numbers, 2011–2022. Available online: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers/ (accessed on 30 March 2024).
- Cottam, D.; Cottam, S.; Surve, A. Single-Anastomosis Duodenal Ileostomy with Sleeve Gastrectomy “Continued Innovation of the Duodenal Switch”. Surg. Clin. N. Am. 2021, 101, 189–198. [Google Scholar] [CrossRef]
- Esparham, A.; Roohi, S.; Ahmadyar, S.; Dalili, A.; Moghadam, H.A.; Torres, A.J.; Khorgami, Z. The Efficacy and Safety of Laparoscopic Single-Anastomosis Duodeno-Ileostomy with Sleeve Gastrectomy (SADI-S) in Mid- and Long-Term Follow-Up: A Systematic Review. Obes. Surg. 2023, 33, 4070–4079. [Google Scholar] [CrossRef]
- Verhoeff, K.; Mocanu, V.; Zalasky, A.; Dang, J.; Kung, J.Y.; Switzer, N.J.; Birch, D.W.; Karmali, S. Evaluation of Metabolic Outcomes Following SADI-S: A Systematic Review and Meta-Analysis. Obes. Surg. 2022, 32, 1049–1063. [Google Scholar] [CrossRef]
- Ospina Jaramillo, A.; Riscanevo Bobadilla, A.C.; Espinosa, M.O.; Valencia, A.; Jiménez, H.; Montilla Velásquez, M.d.P.; Bastidas, M. Clinical Outcomes and Complications of Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy: A 2-Year Follow-up Study in Bogotá, Colombia. World J. Clin. Cases 2023, 11, 5035–5046. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-Compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. PRISMA-P Group Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Clapp, B.; Corbett, J.; Jordan, M.; Portela, R.; Ghanem, O.M. Single-Anastomosis Duodenoileal Bypass with Sleeve in the United States: A First Comparative Safety Analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program Database. Surg. Obes. Relat. Dis. 2023, 19, 11–17. [Google Scholar] [CrossRef]
- Enochs, P.; Bull, J.; Surve, A.; Cottam, D.; Bovard, S.; Bruce, J.; Tyner, M.; Pilati, D.; Cottam, S. Comparative Analysis of the Single-Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy (SADI-S) to Established Bariatric Procedures: An Assessment of 2-Year Postoperative Data Illustrating Weight Loss, Type 2 Diabetes, and Nutritional Status in a Single US Center. Surg. Obes. Relat. Dis. 2020, 16, 24–33. [Google Scholar] [CrossRef]
- Sessa, L.; Guidone, C.; Gallucci, P.; Capristo, E.; Mingrone, G.; Raffaelli, M. Effect of Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy on Glucose Tolerance Test: Comparison with Other Bariatric Procedures. Surg. Obes. Relat. Dis. 2019, 15, 1091–1097. [Google Scholar] [CrossRef]
- Soroceanu, R.P.; Timofte, D.V.; Danila, R.; Timofeiov, S.; Livadariu, R.; Miler, A.A.; Ciuntu, B.M.; Drugus, D.; Checherita, L.E.; Drochioi, I.C.; et al. The Impact of Bariatric Surgery on Quality of Life in Patients with Obesity. J. Clin. Med. 2023, 12, 4225. [Google Scholar] [CrossRef]
- Walton, G.F.; Broussard, T.D. Evaluation of Alternate Laparoscopic Stapling Device for Bariatric Surgery. Surg. Laparosc. Endosc. Percutan Tech. 2023, 33, 505–510. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Ottawa Hospital Research Institute. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 4 April 2024).
- Higgins, J.P.T.; Thompson, S.G. Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Chu, H. Quantifying Publication Bias in Meta-Analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef]
- Abi Mosleh, K.; Belluzzi, A.; Jawhar, N.; Marrero, K.; Al-Kordi, M.; Hage, K.; Ghanem, O.M. Single Anastomosis Duodenoileostomy with Sleeve: A Comprehensive Review of Anatomy, Surgical Technique, and Outcomes. Curr. Obes. Rep. 2024, 13, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Pennestrì, F.; Sessa, L.; Prioli, F.; Gallucci, P.; Ciccoritti, L.; Greco, F.; De Crea, C.; Raffaelli, M. Robotic vs. Laparoscopic Approach for Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy: A Propensity Score Matching Analysis. Updates Surg. 2023, 75, 175–187. [Google Scholar] [CrossRef]
- Wang, L.; Yu, Y.; Wang, J.; Li, S.; Jiang, T. Evaluation of the Learning Curve for Robotic Single-Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy. Front. Surg. 2022, 9, 969418. [Google Scholar] [CrossRef] [PubMed]
- Reames, B.N.; Bacal, D.; Krell, R.W.; Birkmeyer, J.D.; Birkmeyer, N.J.O.; Finks, J.F. Influence of Median Surgeon Operative Duration on Adverse Outcomes in Bariatric Surgery. Surg. Obes. Relat. Dis. 2015, 11, 207–213. [Google Scholar] [CrossRef]
- Cheng, H.; Clymer, J.W.; Po-Han Chen, B.; Sadeghirad, B.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged Operative Duration Is Associated with Complications: A Systematic Review and Meta-Analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Lois, A.W.; Frelich, M.J.; Sahr, N.A.; Hohmann, S.F.; Wang, T.; Gould, J.C. The Relationship between Duration of Stay and Readmissions in Patients Undergoing Bariatric Surgery. Surgery 2015, 158, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Pernaute, A.; Rubio Herrera, M.A.; Pérez-Aguirre, E.; García Pérez, J.C.; Cabrerizo, L.; Díez Valladares, L.; Fernández, C.; Talavera, P.; Torres, A. Proximal Duodenal-Ileal End-to-Side Bypass with Sleeve Gastrectomy: Proposed Technique. Obes. Surg. 2007, 17, 1614–1618. [Google Scholar] [CrossRef] [PubMed]
- García Ruiz de Gordejuela, A.; Ibarzabal, A.; Osorio, J. Bariatric Surgery and Solid-Organ Transplantation. Transplant. Proc. 2022, 54, 87–90. [Google Scholar] [CrossRef]
- Veilleux, E.; Lutfi, R. Obesity and Ventral Hernia Repair: Is There Success in Staging? J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 896–899. [Google Scholar] [CrossRef]
- Gu, A.; Cohen, J.S.; Malahias, M.-A.; Lee, D.; Sculco, P.K.; McLawhorn, A.S. The Effect of Bariatric Surgery Prior to Lower-Extremity Total Joint Arthroplasty: A Systematic Review. HSS J. 2019, 15, 190–200. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).