Abstract
Background/Aims: The purpose of this study was to determine the factors affecting positive diagnostic yields in patients with obscure gastrointestinal bleeding (OGIB) according to the guideline of small bowel capsule endoscopy (SBCE). Method: Patients with a complaint of melena or hematochezia who were admitted were consecutively enrolled. In patients with gastrointestinal bleeding, examination was performed according to the guideline. When OGIB was suspected, SBCE was performed. Patients were categorized into two subgroups based on the SBCE results: a positive group (n = 78) and a negative group (n = 67). Results: The rate of the positive diagnostic yield of SBCE was 53.8% (78/145). In patients over 60 years, the diagnostic yield was 61.5%, which was higher than in patients younger than 60 years (40.7%). In the multivariate analysis, there was a significant difference in the positive diagnostic yield in the patients aged over 60 years (p < 0.01). Factors related to the procedure and clinical characteristics also showed significant differences in the positive predictive rates according to the degree of bowel preparation, small bowel transit time, and transfusion requirements. Conclusions: SBCE could be recommended as a diagnostic tool for OGIB, especially in those with old ages (>60 years) and those who need transfusion, because of its relatively high diagnostic yields in these populations. Proper bowel preparation and a prolonged small bowel transit time may have clinical significance in relation to the positive diagnostic yield of SBCE in patients with OGIB.
1. Introduction
Gastrointestinal bleeding (GIB) is common in emergency rooms and outpatient clinics. It can be overt or occult. Overt GIB is defined as gastrointestinal hemorrhage presenting as visible blood or altered blood (e.g., coffee-ground emesis or melena) per the mouth or rectum. On the other hand, occult or obscure GI bleeding (OGIB) is defined as bleeding that is invisible to the patient or physician, resulting in iron deficiency anemia with or without a positive fecal occult blood test [1]. In most patients with GIB, a series of tests are performed to identify the cause of the bleeding. These tests include esophago-gastroduodenoscopy, colonoscopy, push enteroscopy, and radiologic tests such as contrast-enhanced computed tomography, red blood cell scans, angiograms, and Meckel scans. Despite these investigations, the source of the bleeding may not be identified in some cases. OGIB is defined as persistent or recurrent bleeding for which the cause cannot be found on routine initial evaluation using endoscopy or radiographic examination [1]. The causes of OGIB vary by age and other comorbidities.
Small bowel bleeding accounts for a large proportion of OGIB [2]. Nevertheless, studies on small bowel bleeding are somewhat limited. In the last two decades, small bowel capsule endoscopy (SBCE) has been an easy and comfortable way to visually observe the small intestine mucosa compared to conventional small intestine-related examinations. Therefore, it has become the most commonly used test method for diagnosing small bowel diseases. SBCE is the recommended first-line diagnostic tool because of its non-invasiveness and high diagnostic yield [3,4,5]. Because SBCE is a relatively new technique, there are limited data on its effectiveness in evaluating OGIB [6,7,8,9]. In previous studies, the diagnostic yields of SBCE in those with overt and occult bleeding were 88 and 48%, respectively [4,10,11]. The factors involved in the positive diagnostic yields of SBCE for OGIB include the examination time from symptom onset to SBCE, hemoglobin level, transfusion volume, advanced age, anticoagulant use, and liver disease.
Since 2015, several guidelines for GIB have been introduced [12,13,14,15]. Since most of the studies were conducted before the publication of these guidelines, it seems necessary to research results after the publication of the guidelines. Upper gastrointestinal endoscopy and colonoscopy are performed first. Gastrointestinal obstruction can be confirmed by abdominal computed tomography. Angiography is then performed for those with overt bleeding and unstable vital signs. SBCE is then performed for the remaining overt bleeding with stable vital sign or OGIB. In this study, we tried to find out the diagnostic yields of SBCE according to guidelines, such as the American College of Gastroenterology (ACG) 2015 [Reference 12]. We also tried to find the factors affecting the diagnostic yield of SBCE in patients with OGIB. Our intention was to provide factors to increase the diagnostic yield, to properly treat, and to make the decision to perform SBCE for cases with OGIB, such as a decision about the necessity of SBCE.
2. Results
- (1)
- Baseline demographics and clinical characteristics
A total of 310 patients with GI bleeding in the emergency or gastroenterology department from January 2020 to December 2022 were retrospectively reviewed. Patients with known Crohn’s disease (n = 29) and patients with ongoing or overt GI bleeding (n = 85) were excluded. SBCE was performed for patients with occult or obscure GI bleeding (n = 148). Among them, 3 patients who could not swallow the capsule (n = 2) or did not have transmit images due to poor sensor attachment (n = 1) during the examination were excluded. Finally, 145 patients were enrolled and their results were reviewed. A retrospective record analysis was then performed (Figure 1).
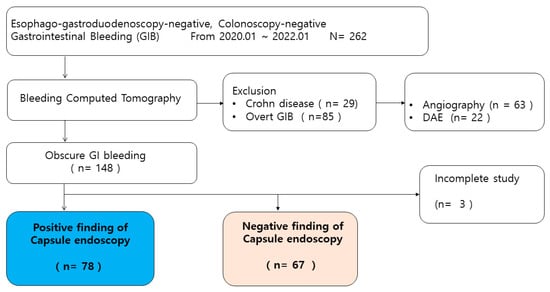
Figure 1.
Flow chart showing the selection of subjects for this study.
- (2)
- Diagnostic yield
The rate of the positive diagnostic yield of SBCE was 53.8% (78/145). Erosions, ulcers, angiodysplasia, and tumors could be the bleeding focus. Figure 2 shows the proportion of positive findings. The frequencies of erosions, ulcers, angiodysplasia, and tumors were 21.8% (17/78), 59.0% (46/78), 20.5% (16/78), and 1.3% (1/78), respectively. Ulcers with active bleeding and red blood clots were detected. Ulcers with a clean base considered the bleeding focus were included. Active bleeding in angiodysplasia was also detected. The tumor was a Y-III polyp of 5 mm in the proximal jejunum (Figure 2).
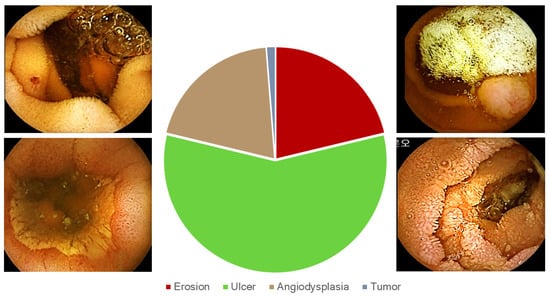
Figure 2.
Types and frequencies of positive findings of bleeding stigma and lesions.
- (3)
- Univariate analysis
Table 1 and Table 2 show the univariate analysis of the demographics and clinical characteristics/procedure-related factors. There was no significant difference in body mass index (kg/m2), smoking, alcohol, pre-diagnosed diabetes mellitus, NSAID, ECOG, ESRD, interval from event to evaluation, whether the 1st attack, anemia, thrombocytopenia, transfusion requirement, degree of preparation, or time to duodenum with observation for ampulla of Vater (AoV) between SBCE-positive and -negative groups. The degree of bowel preparation affected the diagnostic yield of SBCE (p < 0.01). The time from duodenum to cecum, which was considered as SBTT, was significantly longer in the positive group than in the negative group (p = 0.01). When the small bowel transit time was more than 7 h, the diagnostic yield was 63.8% (37/58), compared to 47.1% (41/87) when it was less than 7 h. The rebleeding rates did not show significant differences between the two groups (15.4% vs. 10.4%). In the positive group, only three cases obtained a different diagnosis upon examination (two additional small bowel ulcers, one gastric angiodysplasia). The remaining patients were suspected of rebleeding due to existing lesions, and all of them recovered with conservative treatment. In the negative group, rebleeding occurred in 7 out of 67 cases. Through additional examinations, the bleeding foci were confirmed in five individuals. Among them, two cases were small bowel angiodysplasia, and three individuals were diagnosed with colon diverticular bleeding. The remaining two cases were long-term warfarin user. In patients over 60 years, the diagnostic yield was 61.5% (56/91), which was higher than in patients younger than 60 years (40.7%, 22/54).

Table 1.
Baseline demographics of the patients with obscure gastrointestinal bleeding.

Table 2.
Baseline clinical characteristics and procedure-related factors.
- (4)
- Multivariate analysis
When we set the cut-off value to be 60 years old for age, there was a significant difference in the age factor (>60 years) between the positive group and the negative group (OR: 2.810, 95% CI: 1.077–7.330, p = 0.03 for age; Table 3). In addition, there were significant differences in the degree of bowel preparation, SBTT, and red blood cell transfusion requirement between the two groups (Table 4). Especially, when we set a cut-off of more than 7 h for the SBTT, the differences between the two groups were definitely significant (OR: 2.358, 95% CI: 1.100–5.055, p = 0.02 for SBTT).

Table 3.
Multivariate analysis of demographics.

Table 4.
Multivariate analysis of clinical characteristics and procedure-related factors.
3. Materials and Methods
- (1)
- Patients
This study was approved by the Institutional Review Board of St. Vincent’s Hospital, The Catholic University of Korea (approval no. VC22RISI0303). We retrospectively reviewed the charts of patients who were referred for evaluation at St. Vincent’s Hospital, College of Medicine, the Catholic University of Korea. Patients with GIB who visited the emergency room and gastroenterology department from January 2020 to December 2022 were consecutively enrolled. Esophagogastroduodenoscopy and colonoscopy were performed to find the site of bleeding in all subjects. The following procedures were performed for cases where no specific site of bleeding was found. According to the guideline in ACG 2015, bleeding computed tomography was performed to exclude ongoing or overt GIB to identify the site of the bleeding before conventional angiography. Because CT had improved detection capability for small bowel masses, especially mural-based lesions, CT scans were performed before SBCE in patients not only with overt bleeding but also inflammatory bowel disease, previous small bowel surgery, and/or suspected small bowel stenosis. When ongoing or overt GIB was confirmed on CT scan, angiography was performed if the vital signs were unstable, while device-assisted enteroscopy was performed if the vital signs were stable. When we were not able to find the bleeding focus through other tests, we performed SBCE for small bowel study. The SBCE equipment was a PillCamTM SB 3 system (Medtronic, Minneapolis, MN, USA). It is recommended that bowel preparation should be performed with polyethylene glycol (PEG) 2 L and simethicone, so the bowel preparation was performed with CoolPrep® (PEG and ascorbic acid, Taejoon Pharm, Seoul, Republic of Korea). Patients had two sachets of powder with 1 L of water each at 9 p.m. the day before the exam and 6 a.m. on the exam day.
- (2)
- Definitions
End-stage renal disease (ESRD) was defined as patients undergoing kidney replacement therapy, including maintenance hemodialysis. The degree of physical activity was determined according to the Eastern Cooperative Oncology Group (ECOG) scale. The global degree of cleanliness of the small intestine and the colon was evaluated [16]: (1) Poor—Intestinal content impeding evaluation, (2) Fair—Liquid or solid intestinal content allowing evaluation, (3) Good—No intestinal content or some located in the terminal ileum and/or cecum, and (4) Excellent—No intestinal content in any part of the small intestinal tract (including ileum) or the cecum. A transfusion requirement meant red blood cell transfusion was actually performed. The target hemoglobin was 7 g/dL in hemodynamically stable patients, 8/dL in those with pre-existing cardiovascular disease, and 10 g/dL in those with ongoing bleeding or hemodynamically instability. Positive findings of recent bleeding stigmata and lesions were explainable bleeding, such as erosion, ulcer, angiodysplasia, and tumor. According to the Saurin classification, P1 and P2 lesions were included [17].
- (3)
- Factors—Demographic factors and clinical characteristics
Many factors were considered, including patients’ demographic factors and factors related to clinical characteristics and procedures. The demographic factors included gender, age, height, weight, body mass index (kg/m2) smoking, alcohol, pre-diagnosed diabetes mellitus, antithrombotic drugs (anti-platelet drug, including aspirin or clopidogrel, new oral anticoagulants (NOAC), warfarin, cilostazol), nonsteroidal anti-inflammatory drugs (NSAIDs), ECOG scale, and ESRD. The factors related to clinical characteristics and procedures included the interval from bleeding to evaluation, the 1st attack of symptoms, presence of anemia, thrombocytopenia, transfusion requirement, degree of preparation, time to duodenum, time from duodenum to cecum, observation for ampulla of Vater, and recurrence of symptoms. We manually reported the time of initial detection in the duodenum and the time of first entry into the cecum by reviewing the SBCE recording. The time from duodenum to cecum was considered the small bowel transit time (SBTT). We reported the time between the first duodenal image and the last small-intestinal image in patients in whom the capsule did not reach the cecum.
- (4)
- Quality assessment
Gastroenterology specialists reviewed the SBCE. To overcome any inter-observer variation, one author (Hong K) reviewed all the SBCEs again. The remaining author (Lim NR) and corresponding author (Chung WC) reviewed the positive results of SBCE and discussed whether lesions were stigmata or not.
- (5)
- Statistical analysis
All the statistical analyses were performed with the SPSS program (SPSS version 25.0; IBM, Chicago, IL, USA). Levene’s test was used to examine whether the continuous variables were normally distributed. Values are expressed as the mean ± standard deviation. Student’s T-test was used to contrast the differences for the continuous variables. Categorical variables were tested by a Chi-square test or a logistic regression model. A p-value < 0.05 was considered significant.
4. Discussion
Even with recent advances in endoscopic hemostasis, such as topical hemostatic agents or Doppler endoscopic probe, gastrointestinal bleeding remains a major cause of morbidity and mortality worldwide [18]. Therapeutic methods are limited in obscure GIB, especially small intestine bleeding. It seems necessary to improve the diagnostic yield of examination, which is the aim of this study.
In this study, the diagnostic yield was 53.8%, comparable to previous studies [4,5,17]. The yield of SBCE has been reported to range from 35% to 80% in clinical trials and from 40% to 75% in real-life settings [4,5]. In the process of analysis, it is important to note that the diagnosis rates of SBCE in overt GIB and OGIB should be considered separately. Clinical selection may be of great importance as the diagnostic positivity rate in OGIB is approximately 50%, whereas the diagnostic rate of SBCE in overt GIB is relatively higher and within an acceptable range. Therefore, it might be necessary to determine an appropriate indication and consider clinical application.
We tried to find independent factors for improving the positive yield in OGIB settings. In our results, good bowel preparation, age over 60 years, SBTT of more than 7 h, and transfusion requirement were significant independent factors in the multivariate analysis. It was obvious that bowel preparation was an essential factor for optimal observation. Previously, there was controversy about the necessity of administering a colon cleanser before SBCE. Several studies have reported that administration of a colon cleanser does not facilitate observation of small intestine mucosa [16,19]. On the other hand, there is a concern that colon-cleansing agents can increase the rate of oversight of SBCE by influencing the movement of the small intestine [16,19]. By analyzing evidence from several studies, guidelines for bowel preparation using SBCE have been presented. The European Society of Gastrointestinal Endoscopy summarized the issues of preparation using SBCE in 2013 [20] and declared technical aspects of SBCE in 2018 [21]. It has recommended that bowel preparation should be performed with polyethylene glycol (PEG) 2 L and simethicone. When choosing a laxative, PEG is recommended first. PEG, vitamin C, and sodium picosulfate can then be considered. In previous studies, neither the PEG solutions improved the diagnostic rate nor the meta-analysis showed an improvement in the diagnostic rate [19,22]. There was no difference in the resolution, diagnosis rate, or complete examination rate of SBCE compared to 2 L even when the amount was increased to 4 L in PEG bowel preparation [23,24,25,26]. Several factors, such as comorbidity and ECOG status, might affect the preparation level. However, in our results, these turned out to not be significant for the diagnostic yields of SBCE. Gender and disease pathology are unlikely to influence the quality of small bowel clearance. Recently, a few studies have investigated the relation between SBTT and diagnostic yield and found that a slow SBTT can lead to a better diagnostic yield [27,28,29,30,31]. One study has shown that an SBTT of 6 h or more is associated with an increase in diagnostic yield and that prokinetics might adversely affect the ability of SBCE to detect important intestinal pathologies [25]. Another study has examined the effects of various methods of small bowel preparation on SBTT and the quality of visualization of the entire small bowel mucosa and found that erythromycin can markedly reduce the gastric emptying time, although it has a negative effect on the quality of the image in the small intestine [27]. In addition, preparation of elderly subjects with PEG or sodium phosphate negatively affected the SBTT [27].
Several studies have reported that maintaining or delaying the SBTT for a certain time can increase the diagnosis rate of SBCE [28,29]. However, a standard time for the SBTT has not yet been suggested. In the present study, statistical processing was performed by setting the average value of the SBTT for target patients. It was found that the diagnosis rate increased when the SBTT was more than 7 h. Whether the diagnosis rate of SBCE can be increased if the SBTT is artificially increased needs to be addressed in the future. More research is needed on the appropriate measurement tool for bowel preparation and the timing of bowel preparation. In addition, the best bowel preparation should be a customized bowel preparation, considering the patient’s condition.
The age factor affected the SBTT in the present study. It also independently affected the SBCE results in the multivariate analysis. A previous multicenter study using a large number of patients has shown similar results [21]. However, whether the test was performed according to guidelines and the outcome of the disease were unknown. Previous studies on SBCE diagnosis rates have also reported that age-related factors can affect the diagnosis rates of SBCE [32,33]. It should be noted that it is difficult for elderly patients to swallow capsules. In addition, the battery is discharged before the capsule can reach the cecum. Moreover, capsule retention can occur in some cases. These are important issues to be addressed in the future [34]. SBCE should be performed more cautiously in relatively younger patients because the detection rate is low in younger patients. Clinically, a ‘wait and see’ strategy can be primarily considered for young patients who come to the hospital with mild symptoms.
The most important factor predicting significant findings was the need for blood transfusion. However, in previous studies, these results came from a state in which neither overt nor OGIB was distinguished [35,36,37]. Although it is natural to perform SBCE in areas with high transfusion requirements for overt or ongoing bleeding, it is noteworthy that the diagnostic positive rate of SBCE is high in areas with high transfusion requirements even for OGIB, as shown in our study results. The high positive predictive rate in patients with transfusion requirements might be related to the severity of the lesion. However, whether or not NSAIDs or antithrombotics were used did not show statistically significant differences in our results.
Although the optimal timing of the SBCE procedure is not yet known, a recent meta-analysis has revealed a clear role of SBCE for small bowel studies in the initial evaluation of OGIB in that it can influence the subsequent therapeutic intervention and prognosis [3]. The diagnostic yield of SBCE was 59.1% in the first 48 h and 18.9% in the first 72 h [3,38]. A previous study has shown that early deployment of SBCE within 3 days of hospitalization can lead to higher diagnostic outcomes, higher treatment intervention rates, and shorter lengths of stay [39]. In our results, the absolute time difference was not statistically significant because most cases were performed within 72 h. If SBCE could be performed as an urgent emergency within 24 h of symptom attack, whether or not the diagnostic value of SBCE would increase merits a further study.
In this study, we conducted analyses of various variables and aimed to evaluate significant factors using multivariate analysis, intending to apply them to clinical practice. This was a single-center, retrospective study that might have introduced an element of bias. Moreover, the sample size of the study was relatively small. Therefore, further larger, randomized, prospective studies are required.
In conclusion, good bowel preparation, SBTT, age, and transfusion requirement were pivotal factors affecting the diagnostic yield of SBCE in OGIB. SBCE could be considered a diagnostic tool in OGIB, especially in old ages and those who need transfusion. Moreover, enhancing bowel preparation is suggested to improve the diagnostic yield of capsule endoscopy. A well-designed prospective study is needed to clarify these factors and efforts to improve these factors should be considered in consecutive prospective studies.
Author Contributions
Conceptualization, W.C.C.; methodology, W.C.C.; validation, W.C.C., K.Y.H. and N.R.L.; formal analysis, W.C.C. and N.R.L.; investigation, K.Y.H.; data curation, K.Y.H.; writing—original draft preparation, K.Y.H.; writing—review and editing, N.R.L.; visualization, W.C.C.; supervision, W.C.C.; project administration, W.C.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and it was approved by the Institutional Review Board of St. Vincent’s Hospital, The Catholic University of Korea (approval no. VC22RISI0303, 15 December 2022).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study.
Data Availability Statement
The data are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gralnek, I.M. Obscure-overt gastrointestinal bleeding. Gastroenterology 2005, 128, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Ohmiya, N. Management of obscure gastrointestinal bleeding: Comparison of guidelines between Japan and other countries. Dig. Endosc. 2020, 32, 204–218. [Google Scholar] [CrossRef] [PubMed]
- Estevinho, M.M.; Pinho, R.; Fernandes, C.; Rodrigues, A.; Ponte, A.; Gomes, A.C.; Afecto, E.; Correia, J.; Carvalho, J. Diagnostic and therapeutic yields of early capsule endoscopy and device-assisted enteroscopy in the setting of overt GI bleeding: A systematic review with meta-analysis. Gastrointest. Endosc. 2022, 95, 610–625.e9. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, D.; Ohmiya, N.; Nakamura, M.; Honda, W.; Shirai, O.; Itoh, A.; Hirooka, Y.; Niwa, Y.; Maeda, O.; Ando, T.; et al. Outcome after enteroscopy for patients with obscure GI bleeding: Diagnostic comparison between double-balloon endoscopy and videocapsule endoscopy. Gastrointest. Endosc. 2009, 69, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Uchida, G.; Nakamura, M.; Yamamura, T.; Furukawa, K.; Kawashima, H.; Honda, T.; Ishigami, M.; Fujishiro, M. Systematic review and meta-analysis of the diagnostic and therapeutic yield of small bowel endoscopy in patients with overt small bowel bleeding. Dig. Endosc. 2021, 33, 66–82. [Google Scholar] [CrossRef] [PubMed]
- Costamagna, G.; Shah, S.K.; Riccioni, M.E.; Foschia, F.; Mutignani, M.; Perri, V.; Vecchioli, A.; Brizi, M.G.; Picciocchi, A.; Marano, P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology 2002, 123, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.S.; Swain, P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: Results of a pilot study. Gastrointest. Endosc. 2002, 56, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Ell, C.; Remke, S.; May, A.; Helou, L.; Henrich, R.; Mayer, G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy 2002, 34, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Adler, D.G.; Knipschield, M.; Gostout, C. A prospective comparison of capsule endoscopy and push enteroscopy in patients with GI bleeding of obscure origin. Gastrointest. Endosc. 2004, 59, 492–498. [Google Scholar] [CrossRef]
- Viazis, N.; Anastasiou, J.; Karamanolis, D.G. Small bowel capsule endoscopy for the investigation of obscure gastrointestinal bleeding: When we should do it and what should we expect. Acta Gastroenterol. Belg. 2016, 79, 355–362. [Google Scholar]
- Westerhof, J.; Weersma, R.K.; Koornstra, J.J. Investigating obscure gastrointestinal bleeding: Capsule endoscopy or double balloon enteroscopy? Neth. J. Med. 2009, 67, 260–265. [Google Scholar]
- Gerson, L.B.; Fidler, J.L.; Cave, D.R.; Leighton, J.A. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am. J. Gastroenterol. 2015, 110, 1265–1287, quiz 1288. [Google Scholar] [CrossRef] [PubMed]
- Pennazio, M.; Spada, C.; Eliakim, R.; Keuchel, M.; May, A.; Mulder, C.J.; Rondonotti, E.; Adler, S.N.; Albert, J.; Baltes, P.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2015, 47, 352–376. [Google Scholar] [CrossRef]
- Yamamoto, H.; Ogata, H.; Matsumoto, T.; Ohmiya, N.; Ohtsuka, K.; Watanabe, K.; Yano, T.; Matsui, T.; Higuchi, K.; Nakamura, T.; et al. Clinical Practice Guideline for Enteroscopy. Dig. Endosc. 2017, 29, 519–546. [Google Scholar] [CrossRef]
- Pennazio, M.; Rondonotti, E.; Despott, E.J.; Dray, X.; Keuchel, M.; Moreels, T.; Sanders, D.S.; Spada, C.; Carretero, C.; Cortegoso Valdivia, P.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2022. Endoscopy 2023, 55, 58–95. [Google Scholar] [CrossRef] [PubMed]
- Pons Beltran, V.; Carretero, C.; Gonzalez-Suarez, B.; Fernandez-Urien, I.; Munoz-Navas, M. Intestinal preparation prior to capsule endoscopy administration. World J. Gastroenterol. 2008, 14, 5773–5775. [Google Scholar] [CrossRef] [PubMed]
- Saurin, J.C.; Delvaux, M.; Gaudin, J.L.; Fassler, I.; Villarejo, J.; Vahedi, K.; Bitoun, A.; Canard, J.M.; Souquet, J.C.; Ponchon, T.; et al. Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: Blinded comparison with video push-enteroscopy. Endoscopy 2003, 35, 576–584. [Google Scholar] [CrossRef]
- Facciorusso, A.; Straus Takahashi, M.; Eyileten Postula, C.; Buccino, V.R.; Muscatiello, N. Efficacy of hemostatic powders in upper gastrointestinal bleeding: A systemic review and meta-analysis. Dig. Liver Dis. 2019, 51, 1633–1640. [Google Scholar] [CrossRef]
- Gkolfakis, P.; Tziatzios, G.; Dimitriadis, G.D.; Triantafyllou, K. Meta-analysis of randomized controlled trials challenging the usefulness of purgative preparation before small-bowel video capsule endoscopy. Endoscopy 2018, 50, 671–683. [Google Scholar] [CrossRef]
- Mathus-Vliegen, E.; Pellise, M.; Heresbach, D.; Fischbach, W.; Dixon, T.; Belsey, J.; Parente, F.; Rio-Tinto, R.; Brown, A.; Toth, E.; et al. Consensus guidelines for the use of bowel preparation prior to colonic diagnostic procedures: Colonoscopy and small bowel video capsule endoscopy. Curr. Med. Res. Opin. 2013, 29, 931–945. [Google Scholar] [CrossRef]
- Rondonotti, E.; Spada, C.; Adler, S.; May, A.; Despott, E.J.; Koulaouzidis, A.; Panter, S.; Domagk, D.; Fernandez-Urien, I.; Rahmi, G.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy 2018, 50, 423–446. [Google Scholar] [CrossRef]
- Pons Beltran, V.; Gonzalez Suarez, B.; Gonzalez Asanza, C.; Perez-Cuadrado, E.; Fernandez Diez, S.; Fernandez-Urien, I.; Mata Bilbao, A.; Espinos Perez, J.C.; Perez Grueso, M.J.; Arguello Viudez, L.; et al. Evaluation of different bowel preparations for small bowel capsule endoscopy: A prospective, randomized, controlled study. Dig. Dis. Sci. 2011, 56, 2900–2905. [Google Scholar] [CrossRef]
- Kim, K.O.; Jang, B.I. Lessons from korean capsule endoscopy multicenter studies. Clin. Endosc. 2012, 45, 290–294. [Google Scholar] [CrossRef]
- Albert, J.; Gobel, C.M.; Lesske, J.; Lotterer, E.; Nietsch, H.; Fleig, W.E. Simethicone for small bowel preparation for capsule endoscopy: A systematic, single-blinded, controlled study. Gastrointest. Endosc. 2004, 59, 487–491. [Google Scholar] [CrossRef]
- Viazis, N.; Sgouros, S.; Papaxoinis, K.; Vlachogiannakos, J.; Bergele, C.; Sklavos, P.; Panani, A.; Avgerinos, A. Bowel preparation increases the diagnostic yield of capsule endoscopy: A prospective, randomized, controlled study. Gastrointest. Endosc. 2004, 60, 534–538. [Google Scholar] [CrossRef] [PubMed]
- van Tuyl, S.A.; den Ouden, H.; Stolk, M.F.; Kuipers, E.J. Optimal preparation for video capsule endoscopy: A prospective, randomized, single-blind study. Endoscopy 2007, 39, 1037–1040. [Google Scholar] [CrossRef] [PubMed]
- Fireman, Z.; Paz, D.; Kopelman, Y. Capsule endoscopy: Improving transit time and image view. World J. Gastroenterol. 2005, 11, 5863–5866. [Google Scholar] [CrossRef]
- Buscaglia, J.M.; Kapoor, S.; Clarke, J.O.; Bucobo, J.C.; Giday, S.A.; Magno, P.; Yong, E.; Mullin, G.E. Enhanced diagnostic yield with prolonged small bowel transit time during capsule endoscopy. Int. J. Med. Sci. 2008, 5, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Arieira, C.; Dias de Castro, F.; Boal Carvalho, P.; Rosa, B.; Moreira, M.J.; Cotter, J. Small-bowel transit time in capsule endoscopy: A determinant factor for the diagnosis of small-bowel bleeding. Rev. Esp. Enferm. Dig. 2021, 113, 709–713. [Google Scholar] [CrossRef]
- Blanco Velasco, G.; Perez Rodriguez, M.; Alvarez Licona, N.E. Small bowel transit time of capsule endoscopy as a factor for the detection of lesions in potential small bowel bleeding. Rev. Esp. Enferm. Dig. 2019, 111, 696–698. [Google Scholar] [CrossRef]
- Girelli, C.M.; Soncini, M.; Rondonotti, E. Implications of small-bowel transit time in the detection rate of capsule endoscopy: A multivariable multicenter study of patients with obscure gastrointestinal bleeding. World J. Gastroenterol. 2017, 23, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, K.; Sato, H.; Yokomichi, H.; Tsuchiya, A.; Yoshida, T.; Kawata, Y.; Mizusawa, T.; Yokoyama, J.; Terai, S. Variation in small bowel transit time on capsule endoscopy. Ann. Transl. Med. 2020, 8, 348. [Google Scholar] [CrossRef] [PubMed]
- Fireman, Z.; Kopelman, Y.; Friedman, S.; Ephrath, H.; Choman, E.; Debby, H.; Eliakim, R. Age and indication for referral to capsule endoscopy significantly affect small bowel transit times: The given database. Dig. Dis. Sci. 2007, 52, 2884–2887. [Google Scholar] [CrossRef] [PubMed]
- Orlando, G.; Luppino, I.M.; Lerose, M.A.; Gervasi, R.; Amato, B.; Silecchia, G.; Puzziello, A. Feasibility of capsule endoscopy in elderly patients with obscure gastrointestinal bleeding. An up-to-date report. BMC Surg. 2012; 12, (Suppl. S1), S30. [Google Scholar] [CrossRef]
- Ribeiro, I.; Pinho, R.; Rodrigues, A.; Marques, J.; Fernandes, C.; Carvalho, J. Obscure gastrointestinal bleeding: Which factors are associated with positive capsule endoscopy findings? Rev. Esp. Enferm. Dig. 2015, 107, 334–339. [Google Scholar] [PubMed]
- Estevez, E.; Gonzalez-Conde, B.; Vazquez-Iglesias, J.L.; de Los Angeles Vazquez-Millan, M.; Pertega, S.; Alonso, P.A.; Clofent, J.; Santos, E.; Ulla, J.L.; Sanchez, E. Diagnostic yield and clinical outcomes after capsule endoscopy in 100 consecutive patients with obscure gastrointestinal bleeding. Eur. J. Gastroenterol. Hepatol. 2006, 18, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Singeap, A.M.; Cojocariu, C.; Girleanu, I.; Huiban, L.; Sfarti, C.; Cuciureanu, T.; Chiriac, S.; Stanciu, C.; Trifan, A. Clinical Impact of Small Bowel Capsule Endoscopy in Obscure Gastrointestinal Bleeding. Medicina 2020, 56, 548. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Marshall, C.; Chaudhuri, B.; Okoli, C.; Foley, A.; Person, S.D.; Bhattacharya, K.; Cave, D.R. Timing of video capsule endoscopy relative to overt obscure GI bleeding: Implications from a retrospective study. Gastrointest. Endosc. 2013, 77, 761–766. [Google Scholar] [CrossRef]
- Yamada, A.; Watabe, H.; Kobayashi, Y.; Yamaji, Y.; Yoshida, H.; Koike, K. Timing of capsule endoscopy influences the diagnosis and outcome in obscure-overt gastrointestinal bleeding. Hepatogastroenterology 2012, 59, 676–679. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).