Metoclopramide in Gastroparesis: Its Mechanism of Action and Safety Profile
Abstract
1. Introduction
2. Mechanism of Action
2.1. Summary of D2 Antagonism
- CTZ—D2 receptors are found in the CTZ in the area postrema of the fourth ventricle. The area lies outside the blood–brain barrier and is therefore susceptible to drugs or toxins that can initiate vomiting. Metoclopramide is able to achieve its antiemetic effect specifically by inhibiting the vomiting pathway (CTZ). Irritant stimuli from the GI tract travel via visceral afferent nerves to the central nervous vagal motor neurons causing salivation, gastric relaxation, retrograde small bowel contractions, diaphragmatic contraction, and opening of the esophageal hiatus. By exhibiting D2 antagonism, metoclopramide is able to prevent the aforementioned cascade of events.
- Striatal Effects—D2 receptors are found in the indirect striatopallidal projection, which are pathways that regulate the basal ganglia output to control movement. Therefore, extrapyramidal side effects including tardive dyskinesia can occur with metoclopramide.
- Pineal Gland—Metoclopramide also blocks D2 receptors in the pineal gland, resulting in increased release of prolactin which can result in hypogonadism.
- GI tract—Dopaminergic effects on the GI tract include decreased lower esophageal sphincter (LES) pressure, decreased antral muscle contractility, decreased coordination of gastroduodenal motility, and delayed gastric emptying. This effect is inhibited by the pre and postsynaptic antidopaminergic action of metoclopramide. It should be remembered that metoclopramide was first approved for gastroesophageal reflux disease (GERD) based on its ability to increase LES pressure which helps reduce reflux symptoms.
2.2. Summary of 5HT4 Agonist Activity
2.3. Summary of 5HT3 Antagonism
3. Pharmacokinetics
4. Metoclopramide Uses
5. Formulations of Metoclopramide
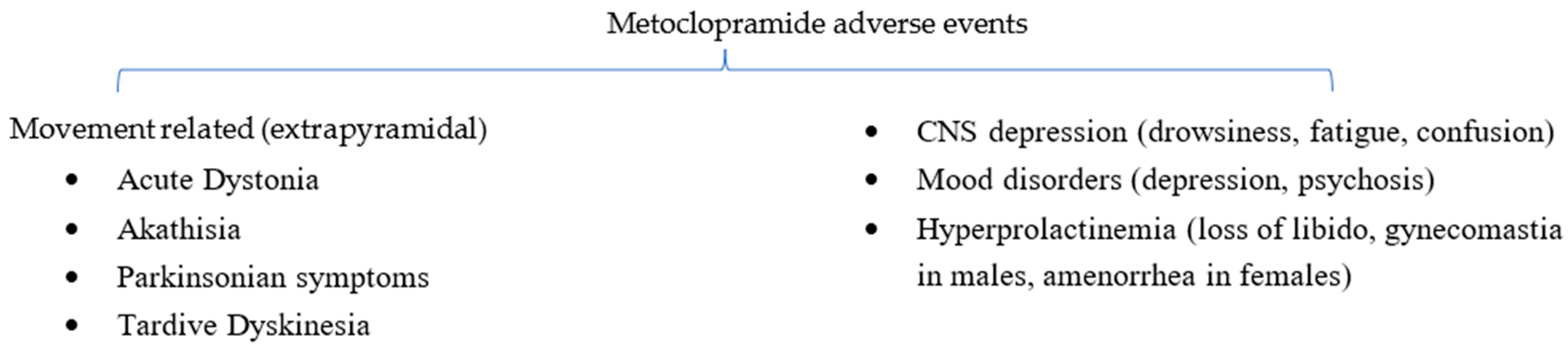
6. Metoclopramide Adverse Events
6.1. Acute Dystonic Reactions
6.2. Akathisia
6.3. Parkinsonian Symptoms
6.4. Tardive Dyskinesia
6.5. Alternative Gastroparesis Treatment Options
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sanger, G.J. Metoclopramide: A template for drug discovery. J. Drug. Des. Res. 2017, 4, 1031. [Google Scholar]
- Lee, A.; Kuo, B. Metoclopramide in the treatment of diabetic gastroparesis. Expert Rev. Endocrinol. Metab. 2010, 5, 653–662. [Google Scholar] [CrossRef]
- World Health Organization. WHO Model List of Essential Medicines. 2021. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02 (accessed on 1 May 2023).
- Smith, L.; Fisher, M.; McKay, G. Metoclopramide. Pract. Diab. Int. 2011, 28, 187–188. [Google Scholar] [CrossRef]
- Al-Saffar, A.; Lennernäs, H.; Hellström, P.M. Gastroparesis, metoclopramide, and tardive dyskinesia: Risk revisited. Neurogastroenterol. Motil. 2019, 31, e13617. [Google Scholar] [CrossRef]
- Van Der Padt, A.; Van Schaik, R.H.N.; Sonneveld, P. Acute dystonic reaction to metoclopramide in patients carrying homozygous cytochrome P450 2D6 genetic polymorphisms. Neth. J. Med. 2006, 64, 160–162. [Google Scholar]
- Bateman, D.N. Clinical Pharmacokinetics of Metoclopramide. Clin. Pharmacokinet. 1983, 8, 523–529. [Google Scholar] [CrossRef]
- O’Brien, M.E.; Cullen, M.H.; Woodroffe, C.M.; Kelly, K.; Burman, C.; Palmer, K.T.; Stuart, N.S.; Blackledge, G.R.; A Sharpe, J. The role of metoclopramide in acute and delayed chemotherapy induced emesis: A randomised double blind trial. Br. J. Cancer 1989, 60, 759–763. [Google Scholar] [CrossRef]
- Abas, M.N.; Tan, P.C.; Azmi, N.; Omar, S.Z. Ondansetron Compared with Metoclopramide for Hyperemesis Gravidarum: A randomized controlled trial. Obstet. Gynecol. 2014, 123, 1272–1279. [Google Scholar] [CrossRef]
- Tan, P.C.; Khine, P.P.; Vallikkannu, N.; Omar, S.Z. Promethazine Compared with Metoclopramide for Hyperemesis Gravidarum: A randomized controlled trial. Obstet. Gynecol. 2010, 115, 975–981. [Google Scholar] [CrossRef]
- Aurora, S.K.; Kori, S.H.; Barrodale, P.; McDonald, S.A.; Haseley, D. Gastric Stasis in Migraine: More Than Just a Paroxysmal Abnormality During a Migraine Attack. Headache 2006, 46, 57–63. [Google Scholar] [CrossRef]
- Yalcin, H.; Okuyucu, E.E.; Ucar, E.; Duman, T.; Yilmazer, S. Changes in liquid emptying in migraine patients: Diagnosed with liquid phase gastric emptying scintigraphy. Intern. Med. J. 2012, 42, 455–459. [Google Scholar] [CrossRef]
- Najjar, M.; Hall, T.; Estupinan, B. Metoclopramide for Acute Migraine Treatment in the Emergency Department: An Effective Alternative to Opioids. Cureus 2017, 9, e1181. [Google Scholar] [CrossRef]
- Akiyama, M.; Yanagisawa, T.; Yuza, Y.; Yokoi, K.; Ariga, M.; Fujisawa, K.; Hoshi, Y.; Eto, Y. Successful treatment of Diamond-Blackfan anemia with metoclopramide. Am. J. Hematol. 2005, 78, 295–298. [Google Scholar] [CrossRef]
- Isola, S.; Hussain, A.; Dua, A.; Singh, K.; Adams, N. Metoclopramide. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519517/ (accessed on 1 May 2023).
- Parkman, H.P.; Carlson, M.R.; Gonyer, D. Metoclopramide nasal spray is effective in symptoms of gastroparesis in diabetics compared to conventional oral tablet. Neurogastroenterol. Motil. 2013, 26, 521–528. [Google Scholar] [CrossRef]
- Ormrod, D.; Goa, K.L. Intranasal Metoclopramide. Drugs 1999, 58, 315–322. [Google Scholar] [CrossRef]
- Ehrenpreis, E.D.; Deepak, P.; Sifuentes, H.; Devi, R.; Du, H.; Leikin, J.B. The Metoclopramide Black Box Warning for Tardive Dyskinesia: Effect on Clinical Practice, Adverse Event Reporting, and Prescription Drug Lawsuits. Am. J. Gastroenterol. 2013, 108, 866–872. [Google Scholar] [CrossRef]
- Jolliet, P.; Nion, S.; Allainveyrac, G.; Tilloyfenart, L.; Vanuxeem, D.; Berezowski, V.; Cecchelli, R. Evidence of lowest brain penetration of an antiemetic drug, metopimazine, compared to domperidone, metoclopramide and chlorpromazine, using an in vitro model of the blood–brain barrier. Pharmacol. Res. 2007, 56, 11–17. [Google Scholar] [CrossRef]
- Bateman, D.N.; Rawlins, M.D.; Simpson, J.M. Extrapyramidal reactions with metoclopramide. BMJ 1985, 291, 930–932. [Google Scholar] [CrossRef]
- Tianyi, F.-L.; Agbor, V.N.; Njim, T. Metoclopramide induced acute dystonic reaction: A case report. BMC Res. Notes 2017, 10, 32. [Google Scholar] [CrossRef]
- Jankovic, J. Medical therapy and botulinum toxin in dystonia. Adv. Neurol. 1998, 78, 169–183. [Google Scholar]
- Dressler, D.; Saberi, F.A. Botulinum Toxin: Mechanisms of Action. Eur. Neurol. 2005, 53, 3–9. [Google Scholar] [CrossRef]
- Chauhan, G.; Nayar, P.; Kashyap, C. Metoclopramide-induced akathisia. J. Anaesthesiol. Clin. Pharmacol. 2012, 28, 548–549. [Google Scholar] [CrossRef]
- Sachdev, P.; Kruk, J. Clinical Characteristics and Predisposing Factors in Acute Drug-Induced Akathisia. Arch. Gen. Psychiatry 1994, 51, 963–974. [Google Scholar] [CrossRef]
- Yin, J.; Barr, A.M.; Ramos-Miguel, A.; Procyshyn, R.M. Antipsychotic Induced Dopamine Supersensitivity Psychosis: A Comprehensive Review. Curr. Neuropharmacol. 2017, 15, 174–183. [Google Scholar] [CrossRef]
- Sharma, A. Propranolol Treatment for Neuroleptic-Induced Akathisia. Prim. Care Companion J. Clin. Psychiatry 2005, 7, 202–203. [Google Scholar] [CrossRef]
- Adler, L.; Angrist, B.; Peselow, E.; Corwin, J.; Rotrosen, J. Efficacy of propranolol in neuroleptic-induced akathesia. J. Clin. Psychopharmacol. 1985, 5, 164–166. [Google Scholar] [CrossRef]
- Regan, L.A.; Hoffman, R.S.; Nelson, L.S. Slower infusion of metoclopramide decreases the rate of akathisia. Am. J. Emerg. Med. 2009, 27, 475–480. [Google Scholar] [CrossRef]
- Ganzini, L.; Casey, D.E.; Hoffman, W.F.; McCall, A.L. The prevalence of metoclopramide-induced tardive dyskinesia and acute extrapyramidal movement disorders. Arch. Intern. Med. 1993, 153, 1469–1475. [Google Scholar] [CrossRef]
- Avorn, J.; Gurwitz, J.H.; Bohn, R.L.; Mogun, H.; Monane, M.; Walker, A. Increased incidence of levodopa therapy following metoclopramide use. JAMA 1995, 274, 1780–1782. [Google Scholar] [CrossRef]
- Rao, A.S.; Camilleri, M. Review article: Metoclopramide and tardive dyskinesia. Aliment. Pharmacol. Ther. 2010, 31, 11–19. [Google Scholar] [CrossRef] [PubMed]
- E Wiholm, B.; Mortimer, O.; Boethius, G.; E Haggstrom, J. Tardive dyskinesia associated with metoclopramide. BMJ 1984, 288, 545–547. [Google Scholar] [CrossRef] [PubMed]
- Sewell, D.D.; Kodsi, A.B.; Caligiuri, M.P.; Jeste, D.V. Metoclopramide and Tardive Dyskinesia. Biol. Psychiatry 1994, 36, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Kenney, C.; Hunter, C.; Davidson, A.; Jankovic, J.; Hunter, C.; Bs, A.D. Metoclopramide, an Increasingly Recognized Cause of Tardive Dyskinesia. J. Clin. Pharmacol. 2008, 48, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Merrill, R.M.; Lyon, J.L.; Matiaco, P.M. Tardive and spontaneous dyskinesia incidence in the general population. BMC Psychiatry 2013, 13, 152–159. [Google Scholar] [CrossRef]
- McCallum, R.W.; Parkman, H.P.; Kunkel, D.C.; Nguyen, L.A.B.; Wright, B.A.; Kalas, M.A.; Ramamoorthy, B.; Donders, J.; Quesenberry, C.; Hyde, B.B. Revisiting the risk of tardive dyskinesia with metoclopramide use: A real-world data driven epidemiologicy study from 2011-2021. Gastroenterology 2022, 162, s368. [Google Scholar] [CrossRef]
- De Keyser, J. Excitotoxic Mechanisms May Be Involved in the Pathophysiology of Tardive Dyskinesia. Clin. Neuropharmacol. 1991, 14, 562–566. [Google Scholar] [CrossRef]
- Camilleri, M.; Kuo, B.; Nguyen, L.; Vaughn, V.M.; Petrey, J.; Greer, K.; Yadlapati, R.; Abell, T.L. ACG Clinical Guideline: Gastroparesis. Am. J. Gastroenterol. 2022, 117, 1197–1220. [Google Scholar] [CrossRef]
- Pasricha, P.J.; Pehlivanov, N.; Sugumar, A.; Jankovic, J. Drug Insight: From disturbed motility to disordered movement—A review of the clinical benefits and medicolegal risks of metoclopramide. Nat. Clin. Pr. Gastroenterol. Hepatol. 2006, 3, 138–148. [Google Scholar] [CrossRef]
- Bergman, H.; Rathbone, J.; Agarwal, V.; Soares-Weiser, K. Antipsychotic reduction and/or cessation and antipsychotics as specific treatments for tardive dyskinesia. Cochrane Database Syst. Rev. 2018, 2018, CD000459. [Google Scholar] [CrossRef]
- Mentzel, C.L.; Bakker, P.R.; van Os, J.; Drukker, M.; Matroos, G.E.; Hoek, H.W.; Tijssen, M.A.J.; van Harten, P.N. Effect of Antipsychotic Type and Dose Changes on Tardive Dyskinesia and Parkinsonism Severity in Patients with a Serious Mental Illness: The Curaçao Extrapyramidal Syndromes Study XI. J. Clin. Psychiatry 2017, 78, e279–e285. [Google Scholar] [CrossRef]
- Arya, D.; Khan, T.; Margolius, A.J.; Fernandez, H.H. Tardive Dyskinesia: Treatment Update. Curr. Neurol. Neurosci. Rep. 2019, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Mentzel, C.L.; Tenback, D.E.; Tijssen, M.A.J.; Visser-Vandewalle, V.E.R.M.; van Harten, P.N. Efficacy and Safety of Deep Brain Stimulation in Patients with Medication-Induced Tardive Dyskinesia and/or Dystonia: A systematic review. J. Clin. Psychiatry 2012, 73, 1434–1438. [Google Scholar] [CrossRef]
- Zhang, W.-F.; Tan, Y.-L.; Zhang, X.-Y.; Chan, R.C.K.; Wu, H.-R.; Zhou, D.-F. Extract of Ginkgo biloba Treatment for Tardive Dyskinesia in Schizophrenia: A randomized, double-blind, placebo-controlled trial. J. Clin. Psychiatry 2010, 72, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Homko, C.J.; Duffy, F.; Friedenberg, F.K.; Boden, G.; Parkman, H.P. Effect of dietary fat and food consistency on gastroparesis symptoms in patients with gastroparesis. Neurogastroenterol. Motil. 2015, 27, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Goyal, R.K. Gastric Emptying Abnormalities in Diabetes Mellitus. N. Engl. J. Med. 2021, 384, 1742–1751. [Google Scholar] [CrossRef]
- Schey, R.; Saadi, M.; Midani, D.; Roberts, A.C.; Parupalli, R.; Parkman, H.P. Domperidone to Treat Symptoms of Gastroparesis: Benefits and Side Effects from a Large Single-Center Cohort. Dig. Dis. Sci. 2016, 61, 3545–3551. [Google Scholar] [CrossRef]
- Patterson, D.; Abell, T.; Rothstein, R.; Koch, K.; Barnett, J. A Double-Blind Multicenter Comparison of Domperidone and Metoclopramide in The Treatment of Diabetic Patients with Symptoms of Gastroparesis. Am. J. Gastroenterol. 1999, 94, 1230–1234. [Google Scholar] [CrossRef]
- Abell, T.L.; Bernstein, V.K.; Cutts, T.; Farrugia, G.; Forster, J.; Hasler, W.L.; Mccallum, R.W.; Olden, K.W.; Parkman, H.P.; Parrish, C.R.; et al. Treatment of gastroparesis: A multidisciplinary clinical review. Neurogastroenterol. Motil. 2006, 18, 263–283. [Google Scholar] [CrossRef]
- McCallum, R.W.; Bashashati, M.; Gonzalez, Z.; Padilla, O.; Torabi, A.; Espino, K.; Davis, B.R.; Sarosiek, I. Pathophysiological evidence provided by gastric smooth muscle biopsies supporting pyloric interventions in patients with refractory gastroparesis: A single center experience. Gastroenterology 2021, 160, S491–S492. [Google Scholar] [CrossRef]
| Predisposing Factors for Extrapyramidal Side Effects |
|---|
| Elderly population (age > 60) |
| Pediatric population–acute dystonia |
| Female sex |
| Use of neuroleptic medications (e.g., 1st generation antipsychotics) |
| Treatment duration > 12 weeks |
| Total dose > 30 mg daily |
| Diabetes mellitus |
| Renal or hepatic dysfunction |
| Use of CYP2D6 inhibitors (e.g., fluoxetine, paroxetine, and bupropion) |
| Genetic (decreased CYP2D6 metabolism) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalas, M.A.; Trivedi, B.; Kalas, M.; Chavez, L.O.; McCallum, R.W. Metoclopramide in Gastroparesis: Its Mechanism of Action and Safety Profile. Gastrointest. Disord. 2023, 5, 317-328. https://doi.org/10.3390/gidisord5030026
Kalas MA, Trivedi B, Kalas M, Chavez LO, McCallum RW. Metoclopramide in Gastroparesis: Its Mechanism of Action and Safety Profile. Gastrointestinal Disorders. 2023; 5(3):317-328. https://doi.org/10.3390/gidisord5030026
Chicago/Turabian StyleKalas, M Ammar, Bhavi Trivedi, Mutaz Kalas, Luis O. Chavez, and Richard W. McCallum. 2023. "Metoclopramide in Gastroparesis: Its Mechanism of Action and Safety Profile" Gastrointestinal Disorders 5, no. 3: 317-328. https://doi.org/10.3390/gidisord5030026
APA StyleKalas, M. A., Trivedi, B., Kalas, M., Chavez, L. O., & McCallum, R. W. (2023). Metoclopramide in Gastroparesis: Its Mechanism of Action and Safety Profile. Gastrointestinal Disorders, 5(3), 317-328. https://doi.org/10.3390/gidisord5030026







