Sleep Quality Assessment in Intensive Care Units: Comparing Actigraphy and the Richards Campbell Sleep Questionnaire—A Pilot Study in the Moroccan Context
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Population and Sampling
4.3. Data Collection
4.4. Nurse Training and Clinical Setting
4.5. Assessment Tools
4.5.1. AM-RCSQ
4.5.2. Actigraphy
4.6. Sleep Quality
4.7. Ethical Approval
4.8. Data Analysis
5. Conclusions
Strengths and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Halvorsen, K.; Jensen, J.F.; Collet, M.O.; Olausson, S.; Lindahl, B.; Sætre Hansen, B.; Lind, R.; Eriksson, T. Patients’ experiences of well-being when being cared for in the intensive care unit—An integrative review. J. Clin. Nurs. 2022, 31, 3–19. [Google Scholar] [CrossRef]
- Alegria, L.; Brockmann, P.; Repetto, P.; Leonard, D.; Cadiz, R.; Paredes, F.; Rojas, I.; Moya, A.; Oviedo, V.; Garcia, P.; et al. Improve sleep in critically ill patients: Study protocol for a randomized controlled trial for a multi-component intervention of environment control in the ICU. PLoS ONE 2023, 18, e0286180. [Google Scholar] [CrossRef] [PubMed]
- Burman, D.; Muzumdar, H. Sleep architecture and physiology. In Management of Sleep Disorders in Psychiatry New York; Oxford University Press: New York, NY, USA, 2020; pp. 12–22. [Google Scholar]
- Daou, M.; Telias, I.; Younes, M.; Brochard, L.; Wilcox, M.E. Abnormal sleep, circadian rhythm disruption, and delirium in the ICU: Are they related? Front. Neurol. 2020, 11, 549908. [Google Scholar] [CrossRef] [PubMed]
- Mart, M.F.; Roberson, S.W.; Salas, B.; Pandharipande, P.P.; Ely, E.W. (Eds.) Prevention and management of delirium in the intensive care unit. In Seminars in Respiratory and Critical Care Medicine; Thieme Medical Publishers, Inc.: New York, NY, USA, 2021. [Google Scholar]
- Voiriot, G.; Oualha, M.; Pierre, A.; Salmon-Gandonniere, C.; Gaudet, A.; Jouan, Y.; Kallel, H.; Radermacher, P.; Vodovar, D.; Sarton, B.; et al. Chronic critical illness and post-intensive care syndrome: From pathophysiology to clinical challenges. Ann. Intensive Care 2022, 12, 58. [Google Scholar] [CrossRef] [PubMed]
- Gupta, L.; Subair, M.N.; Munjal, J.; Singh, B.; Bansal, V.; Gupta, V.; Jain, R. Beyond survival: Understanding post-intensive care syndrome. Acute Crit. Care 2024, 39, 226–233. [Google Scholar] [CrossRef]
- Hussain, Z.; Sheng, Q.Z.; Zhang, W.E.; Ortiz, J.; Pouriyeh, S. Non-invasive techniques for monitoring different aspects of sleep: A comprehensive review. ACM Trans. Comput. Healthc. (HEALTH) 2022, 3, 1–26. [Google Scholar]
- Malhotra, R.; Kirsch, D.; Kristo, D.; Olson, E.; Aurora, R.; Carden, K.; Chervin, R.; Martin, J.; Ramar, K.; Rosen, C. American Academy of Sleep Medicine Board of Directors. Polysomnography for obstructive sleep apnea should include arousal-based scoring: An American Academy of Sleep Medicine position statement. J. Clin. Sleep Med. 2018, 14, 1245–1247. [Google Scholar] [CrossRef]
- Delaney, L.; Litton, E.; Melehan, K.; Huang, H.-C.C.; Lopez, V.; Van Haren, F. The feasibility and reliability of actigraphy to monitor sleep in intensive care patients: An observational study. Crit. Care 2021, 25, 42. [Google Scholar] [CrossRef]
- Bigué, J.L.; Duclos, C.; Dumont, M.; Paquet, J.; Blais, H.; Menon, D.K.; Bernard, F.; Gosselin, N. Validity of actigraphy for nighttime sleep monitoring in hospitalized patients with traumatic injuries. J. Clin. Sleep Med. 2020, 16, 185–192. [Google Scholar] [CrossRef]
- Rahimi-Eichi, H.; Coombs Iii, G.; Vidal Bustamante, C.M.; Onnela, J.P.; Baker, J.T.; Buckner, R.L. Open-source Longitudinal Sleep Analysis From Accelerometer Data (DPSleep): Algorithm Development and Validation. JMIR Mhealth Uhealth 2021, 9, e29849. [Google Scholar] [CrossRef]
- Richards, K.C.; O’Sullivan, P.S.; Phillips, R.L. Measurement of sleep in critically ill patients. J. Nurs. Meas. 2000, 8, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Dorsch, J.J.; Martin, J.L.; Malhotra, A.; Owens, R.L.; Kamdar, B.B. (Eds.) Sleep in the intensive care unit: Strategies for improvement. In Seminars in Respiratory and Critical Care Medicine; Thieme Medical Publishers: New York, NY, USA, 2019. [Google Scholar]
- Birdja, D.; Özcan, E. Better sleep experience for the critically Ill: A comprehensive strategy for designing hospital soundscapes. Multimodal Technol. Interact. 2019, 3, 36. [Google Scholar] [CrossRef]
- Naik, R.D.; Gupta, K.; Soneja, M.; Elavarasi, A.; Sreenivas, V.; Sinha, S. Sleep quality and quantity in intensive care unit patients: A cross-sectional study. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2018, 22, 408. [Google Scholar]
- Christina-Athanasia, S.; Georgios, K.; Athanasia, L.; Papageorgiou, D. Sleep Quality and Circadian Rhythm Disruption in Critically Ill Patients in Intensive Care Unit. Health Res. J. 2025, 11, 154–166. [Google Scholar]
- Zhang, Y.; Zhang, Y.; Teng, M.; Wang, B.; Cheng, M.; Zhong, S.; Zhang, X.; Ding, X.; Liu, C.; Ma, J. Study on the sleep quality classification and influencing factors of adult icu awake patients based on latent profile analysis: A cross-sectional survey. Nat. Sci. Sleep 2023, 15, 861–871. [Google Scholar] [CrossRef]
- Talvacchia, K. Implementation of a Nonpharmacological Sleep Bundle in a Surgical Intensive Care Unit. Ph.D. Thesis, West Chester University, West Chester, PA, USA, 2024. [Google Scholar]
- Strobel, T.M.; Nguyen, C.; Riggs, T.; Horst, S.N.; Motley, A.; Upadhyaya, S.; Campbell, S.; Spring, E.; Dalal, R.L.; Scoville, E.; et al. Functional medicine approach to patient care improves sleep, fatigue, and quality of life in patients with inflammatory bowel disease. Crohn’s Colitis 2022, 4, 360. [Google Scholar]
- Nilius, G.; Richter, M.; Schroeder, M. Updated perspectives on the management of sleep disorders in the intensive care unit. Nat. Sci. Sleep 2021, 13, 751–762. [Google Scholar] [CrossRef]
- Romagnoli, S.; Villa, G.; Fontanarosa, L.; Tofani, L.; Pinelli, F.; De Gaudio, A.R.; Ricci, Z. Sleep duration and architecture in non-intubated intensive care unit patients: An observational study. Sleep Med. 2020, 70, 79–87. [Google Scholar] [CrossRef]
- Boyko, Y.; Jennum, P.; Toft, P. Sleep quality and circadian rhythm disruption in the intensive care unit: A review. Nat. Sci. Sleep 2017, 9, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Conley, S.; Knies, A.; Batten, J.; Ash, G.; Miner, B.; Hwang, Y.; Jeon, S.; Redeker, N.S. Agreement between actigraphic and polysomnographic measures of sleep in adults with and without chronic conditions: A systematic review and meta-analysis. Sleep Med. Rev. 2019, 46, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Figorilli, M.; Velluzzi, F.; Redolfi, S. Obesity and sleep disorders: A bidirectional relationship. Nutr. Metab. Cardiovasc. Dis. 2025, 35, 104014. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, G.; Zanella, M.T. Obesity metabolic and hormonal disorders associated with obstructive sleep apnea and their impact on the risk of cardiovascular events. Metabolism 2018, 84, 76–84. [Google Scholar] [CrossRef]
- Altman, M.T.; Knauert, M.P.; Pisani, M.A. Sleep disturbance after hospitalization and critical illness: A systematic review. Ann. Am. Thorac. Soc. 2017, 14, 1457–1468. [Google Scholar] [CrossRef]
- Lkoul, A.; Oum’barek, K.; Baba, M.A.; Jniene, A.; Dendane, T. Translation and Validation of the Richards-Campbell Sleep Questionnaire for Intensive Care Unit Patients in Morocco: Reliability and Validity Assessment. Clocks Sleep 2025, 7, 31. [Google Scholar] [CrossRef]
- Edouard, P.; Campo, D.; Bartet, P.; Yang, R.Y.; Bruyneel, M.; Roisman, G.; Escourrou, P. Validation of the Withings Sleep Analyzer, an under-the-mattress device for the detection of moderate-severe sleep apnea syndrome. J. Clin. Sleep Med. 2021, 17, 1217–1227. [Google Scholar] [CrossRef]
- Locihová, H.; Axmann, K.; Žiaková, K.; Šerková, D.; Černochová, S. Sleep quality assessment in intensive care: Actigraphy vs. Richards-Campbell sleep questionnaire. Sleep Sci. 2020, 13, 235–241. [Google Scholar] [PubMed]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
| Variables | Mean ± SD | |
|---|---|---|
| Patients | Age [Years] | 54.25 ± 16.76 |
| BMI [kg/m2] | 23.13 ± 4.86 | |
| Pain-score VAS (Visual Analogue Scale) | 4.07 ± 3.24 | |
| Charlson score | 1.25 ± 1.37 | |
| SOFA score | 0.73 ± 0.85 | |
| APACHE II score | 10.66 ± 5.76 | |
| Length of Stay [Days] | 5.44 ± 2.53 | |
| AM-RCSQ | Sleep Depth [Score] | 39.03 ± 22.43 |
| Sleep Latency [Score] | 35.71 ± 21.44 | |
| Number of Sleep Interruptions | 40.32 ± 20.03 | |
| Return to Sleep After Awakening [Score] | 38.88 ± 18.81 | |
| Perceived Sleep Quality [Score] | 38.93 ± 17.12 | |
| Noise [Score] | 33.23 ± 17.72 | |
| RCSQ Total [Score] | 38.16 ± 17.09 | |
| Actigraphy | Sleep Onset Latency [min] | 39.23 ± 22.09 |
| Total Sleep Time [min] | 198.15 ± 128.42 | |
| Number of Sleep Interruptions | 52.28 ± 24.85 | |
| Overall Sleep Quality [score] | 37.03 ± 19.2 |
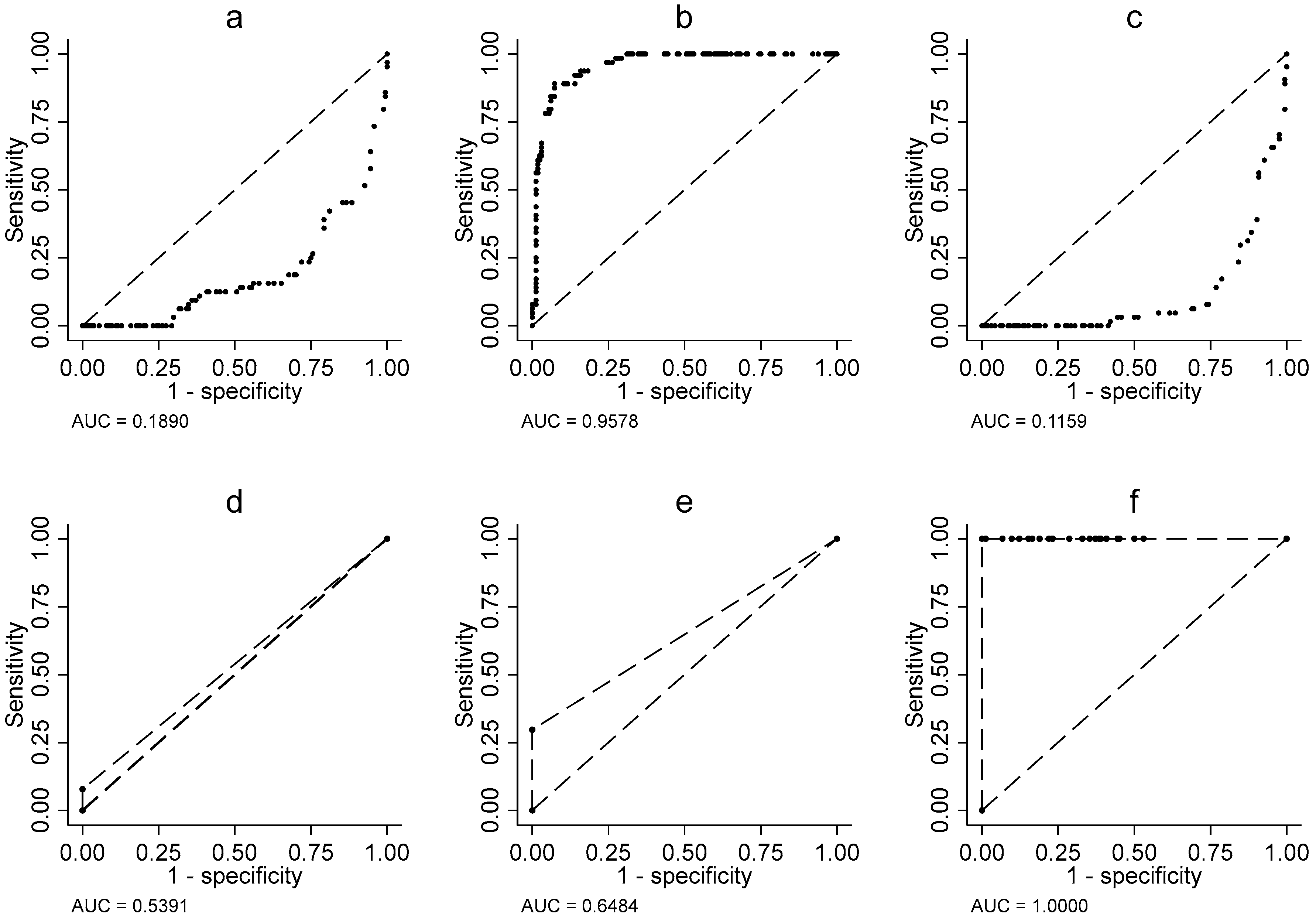
| Variable | Cut-Off Value a | Youden’s Statistic | AUC (SD) b | p-Value c | Sensitivity (%) | Specificity (%) | Accuracy (%) | |
|---|---|---|---|---|---|---|---|---|
| AM-RCSQ | Sleep Depth | 53 | 0.6711 | 0.84 (0.0204) | <0.001 | 82.00 | 85.00 | 82.46 |
| Sleep Latency | 43 | 0.7173 | 0.86 (0.0130) | <0.001 | 92.00 | 80.00 | 82.02 | |
| Number of Awakenings | 57 | 0.6940 | 0.85 (0.0257) | <0.001 | 76.00 | 94.00 | 89.04 | |
| Return to Sleep After Awakening | 53 | 0.6341 | 0.82 (0.0276) | <0.001 | 73.00 | 90.00 | 84.65 | |
| Perceived Sleep Quality | 38 | 0.6575 | 0.83 (0.0215) | <0.001 | 96.00 | 70.00 | 74.12 | |
| Noise | 40 | 0.6540 | 0.83 (0.0196) | <0.001 | 82.00 | 84.00 | 73.25 | |
| Total AM-RCSQ Score | 49.4 | 1.0000 | 1.00 (0.00) | <0.001 | 100.00 | 100.00 | 99.56 | |
| Actigraphy | Sleep Latency | 97 | 0.0000 | 0.5 (0.0314) | <0.001 | 0.00 | 100.00 | 71.49 |
| Total Sleep Duration | 277 | 0.817 | 0.91 (0.0124) | <0.001 | 89.00 | 93.00 | 89.47 | |
| Number of Sleep Interruptions | 124 | 0.0000 | 0.50 (0.0223) | <0.001 | 0.00 | 100.00 | 71.49 | |
| Sleep Depth | 0 | 0.078 | 0.54 (0.0169) | <0.020 | 08.00 | 100.00 | 0.00 | |
| Sleep Efficiency | 0 | 0.297 | 0.65 (0.2878) | <0.001 | 30.00 | 100.00 | 0.00 | |
| Total Score (Sleep Quality) | 49 | 1.000 | 1.00 (0.0) | <0.001 | 100.00 | 100.00 | 99.12 |
| Variables | Mean ± SD | p | |
|---|---|---|---|
| Poor Sleep Quality n = 164 (% = 71.9) | Good Sleep Quality n = 64 (% = 28.1) | ||
| Gender | <0.001 a | ||
| Female (n = 107, % = 46.9) | 94 (87.85) | 13 (12.15) | - |
| Male (n = 121, % = 53.1) | 70 (57.85) | 51 (42.15) | - |
| Age [Years] | 56.09 ± 16.19 | 49.52 ± 17.4 | 0.010 b |
| BMI [kg/m2] | 23.23 ± 4.96 | 22.89 ± 4.63 | 0.764 b |
| Pain VAS score | 4.79 ± 3.12 | 2.22 ± 2.78 | <0.001 b |
| Charlson score | 1.45 ± 1.36 | 0.77 ± 1.26 | <0.001 b |
| SOFA score | 0.82 ± 0.86 | 0.5 ± 0.8 | 0.004 b |
| APACHE II score | 11.65 ± 5.65 | 8.14 ± 5.26 | <0.001 b |
| Length of Stay [Days] | 5.77 ± 2.64 | 4.59 ± 1.99 | <0.001 b |
| Sleep Onset Latency [min] | 45.2 ± 22.01 | 23.94 ± 13.21 | <0.001 b |
| Total Sleep Time [min] | 143.07 ± 103.14 | 339.3 ± 61.34 | <0.001 b |
| Number of Sleep Interruptions | 60.33 ± 24.35 | 31.66 ± 9.48 | <0.001 b |
| Overall Sleep Quality [score] | 28.1 ± 13.91 | 59.92 ± 9.39 | <0.001 b |
| Actigraphy Parameters | Unit | Definition |
|---|---|---|
| Sleep onset latency | Minutes | The elapsed time between wakefulness inhibition and sleep onset |
| Total sleep time | Minutes | The total time spent sleeping, from sleep onset to final awakening. |
| Number of awakenings | Episodes | The number of awakenings during the night. |
| Sleep depth | Score | Duration of the deep sleep phase (NREM Stage 3) |
| Sleep efficiency | Score | The proportion of time spent sleeping relative to time spent in bed. |
| Global sleep quality score | Score | Sleep quality, rated on a scale of 0 to 100. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lkoul, A.; Oumbarek, K.; Bouchriti, Y.; Jniene, A.; Dendane, T. Sleep Quality Assessment in Intensive Care Units: Comparing Actigraphy and the Richards Campbell Sleep Questionnaire—A Pilot Study in the Moroccan Context. Clocks & Sleep 2025, 7, 49. https://doi.org/10.3390/clockssleep7030049
Lkoul A, Oumbarek K, Bouchriti Y, Jniene A, Dendane T. Sleep Quality Assessment in Intensive Care Units: Comparing Actigraphy and the Richards Campbell Sleep Questionnaire—A Pilot Study in the Moroccan Context. Clocks & Sleep. 2025; 7(3):49. https://doi.org/10.3390/clockssleep7030049
Chicago/Turabian StyleLkoul, Abdelmajid, Keltouma Oumbarek, Youssef Bouchriti, Asmaa Jniene, and Tarek Dendane. 2025. "Sleep Quality Assessment in Intensive Care Units: Comparing Actigraphy and the Richards Campbell Sleep Questionnaire—A Pilot Study in the Moroccan Context" Clocks & Sleep 7, no. 3: 49. https://doi.org/10.3390/clockssleep7030049
APA StyleLkoul, A., Oumbarek, K., Bouchriti, Y., Jniene, A., & Dendane, T. (2025). Sleep Quality Assessment in Intensive Care Units: Comparing Actigraphy and the Richards Campbell Sleep Questionnaire—A Pilot Study in the Moroccan Context. Clocks & Sleep, 7(3), 49. https://doi.org/10.3390/clockssleep7030049






