Abstract
Sleep health inequalities represent an increasing public health concern. Among multiple determinants affecting sleep health, there is people’s socioeconomic status (SES), and no systematic review on the relationship between SES and sleep health has been previously conducted in Iran and Saudi Arabia. Following the Prisma protocol, ten articles were selected. Findings revealed that the combined number of participants was N = 37,455 participants, including 73.23% of children and adolescents (n = 27,670) and 26.77% of adults (n = 10,026). The smallest sample was N = 715 and the larger was N = 13,486. In all these studies, sleep variables were assessed using self-reported questionnaires. The studies conducted in Iran assessed the risk of obstructive sleep apnea (OSA), while those in Saudi Arabia were interested in sleep duration, nap time, bedtime, rise time and insomnia. The studies performed on adult populations in Iran and Saudi Arabia concluded that there is no significant association between SES determinants and sleep components in adult populations. One study in Iran found a significant association between parent’s low SES and children and adolescent insomnia; and one study in Saudi Arabia found a significant association between the father’s education and the longer sleep duration of their children. More longitudinal studies are necessary to establish a causal relationship between public health policies and sleep health inequalities. An extension of the investigation to more sleep disturbances is required to cover the entirety of sleep health inequalities in Iran and Saudi Arabia.
1. Introduction
Health inequalities are associated with economic and societal impact on every government, regardless of GDP and the global well-being of an entire population [1,2,3,4,5,6,7,8]. Health inequalities can be observed with the cardiovascular system [9], respiratory system [10] or sleep mechanisms [1,2]. Sleep is a multifactorial process that may be disturbed by a wide range of environmental, sociological, physiological stimuli and socioeconomic status (SES) [4,5,11]. The concept of sleep health provides a positive holistic framing of multiple sleep characteristics, including sleep duration, continuity, timing, alertness and satisfaction [4]. Sleep health inequalities represent a public health concern similar to public health issues previously reported for cardiovascular, mental health and metabolic diseases [12], while SES is a latent multidimensional concept of an individual’s economic and socioecological situation, also associated to public health inequalities at different levels such as community or country [5,11]. Thus, sleep health disparity is a complex assessment of socio-ideological and theoretical constructs measured in a variety of ways, usually considering several determinants such as employment, income, education, occupation and social position [3,11,12,13].
An extensive screening of the empirical literature revealed that no systematic review on the relationship between SES and sleep health has been previously conducted in Iran and Saudi Arabia. It is pertinent to understand whether public health inequalities in terms of sleep disturbances that are observed elsewhere are the same as in these two important countries, especially considering the crossover of different continents and different ethnocultural populations. This systematic review aims to document the determinants of sleep health inequalities in Iran and Saudi Arabia.
2. Results
2.1. Characteristics of Studies Selected
Descriptive synthesis. Ten articles [14,15,16,17,18,19,20,21,22,23] were included in the final sample (Table 1). They were all cross-sectional studies and published between 2006 and 2019. Among these studies, 50% (n = 5) were performed in Saudi Arabia and 50% (n = 5) in Iran. The combined number of participants was N = 39,550 participants, composed of 69.35% children and adolescents (n = 27,429, mean age = 9.8 years old) and 30.65% adults (n = 12,121, mean age = 46.3 years old). The smallest sample was N = 715 and the largest were N = 13,486. The socioeconomic indicators used were perceived SES/composite indices, education, income, marital status and employment/occupation. In all the studies, sleep variables were reported using self-reported questionnaires. The studies conducted in Iran assessed principally the risk of obstructive sleep apnea (OSA), while those in Saudi Arabia were interested in sleep duration, nap time, bedtime, rise time and insomnia.

Table 1.
Characteristics of included studies investigating determinants of sleep health inequalities in Saudi Arabia and Iran.
Sleep fragmentation. Four cross-sectional studies [18,21,22,23] have studied the association between education (not educated, high school or less and university) with the outcome of the risk of obstructive sleep apnea disorder and insomnia. Amra et al. [18] (adults from the general population aged from 18 to 70 years old) and Seyedmehdi et al. [21] (staff employees at a hospital with mean age at 33.5 years old +/− 7.65) were rated as good quality articles and used the Berlin Questionnaire. Foroughi et al. [22] (adults from the general population with mean age at 40.88 +/− 15.4) had used the Stop Bang. It was rated as a poor-quality study. Ahmed et al. [23] used the ICD-2 instrument to assess insomnia symptoms. No significant result in the multivariate analysis was found in all three articles.
Sleep latency. One cross-sectional study [23] was performed on adults (mean age at 42.3 years +/− 15.5). It had used the ICD-2 criteria to test the association between education and having insomnia, defined by the presence of any of the following symptoms: (1) early morning awakening, (2) difficulty initiating sleep, (3) frequent awakening, (4) feeling tired and (5) sleep loss affects mood. This study was rated as fair. Overall, uneducated people had more risk of insomnia than those attended university. Those who attended high school had a lower risk of insomnia compared to those who attended university. This study concluded that insomnia is most prevalent among females and the elderly population.
Total sleep time. The cross-sectional study of Althakafi et al. [16] had been conducted using an online questionnaire. The mean age of participants was 21.8 years +/− 10.7. It was rated as having a good quality. It had studied the association between education and the duration of sleep and found no significant association.
2.2. Determinants of Sleep Health Inequalities in Iran
Four cross-sectional studies assessed the relationship between SES and subjective sleep measurement. One of these was conducted on children and adolescents (mean age = 12.47 years old) and the others with adults.
For the study conducted on children and adolescents, SES was measured by a SES score summarized by parents’ education and occupation, possessing a private car, school type (public/private), home type (private/rented) and having a personal computer at home. Sleep variables were sleep duration and insomnia assessed by a non-specific questionnaire administered both to parents and children by interviewers.
For those conducted on adults, the SES measurement was the educational level. Sleep variables were risks for obstructive sleep apnea assessed by the self-reported Berlin questionnaire in two studies and the Stop Bang questionnaire in one study. One of these studies assessed, additionally, the quality of sleep summarized by difficulty falling asleep, difficulty staying asleep and waking up too early.
Overall, there was no association between SES and sleep variables. Specifically, only the study conducted in children and adolescents reported an association between low socioeconomic conditions of parents and insomnia. The association between sleep duration and SES was not assessed in this study. In adults, no association between educational level and self-reported risk of OSA was found.
2.3. Determinants of Sleep Health Inequalities in Saudi Arabia
Among the five studies conducted in Saudi Arabia, two were conducted on children, one on adolescents and two on adults. For those conducted on children, SES was measured by the educational level of parents, job status of mothers and family income. For the one conducted on adolescents, the SES measurement was self-reported perceived socio-economic status. For the last two articles on adults, SES was measured by educational level, marital status, occupation and job status. Sleep variables were principally night sleep duration. In one study conducted on children nap duration, bedtime and rise time were also measured. For the studies conducted on adolescents and adults, sleep duration was used to characterize sleep deprivation which was defined by sleeping less than 7 h daily.
Overall, no association was found between SES and sleep duration or sleep deprivation. Only one study conducted on children reported that a high educational level of fathers was associated with longer sleep duration.
3. Discussion
3.1. Summary of Findings
All these ten studies were cross-sectional studies including a total number of 39,550 participants, an average of 55.94% of women in Iran and 52.92% of women in Saudi Arabia. The majority of participants were children and adolescents (N = 27,670, 73.23%). The SES indicators used were perceived SES/composite indices, education, income and employment/occupation. Sleep components were reported using self-reported questionnaires. Studies conducted in Iran assessed principally the risk of obstructive sleep apnea while those in Saudi Arabia were interested in sleep duration, and additionally in nap time, bedtime, rise time and insomnia. The studies performed on adult populations in Iran and Saudi Arabia concluded that there is no significant association between SES and sleep components in adult populations. One study in Iran found a significant association between the parent’s low SES and children and adolescent insomnia, and one study in Saudi Arabia found a significant association between the father’s education and longer sleep duration of their children.
3.2. Relation with Current Knowledge
The novelty and the significance of this work is the epidemiological investigation of health determinants in a world region not well documented in the field of health inequities and sleep science. The current findings in this research are mitigated because they confirm an association between the parent’s SES and sleep disturbances, but they reported no association between SES and sleep health for adult populations. The majority of studies investigating sleep health inequalities found, until now, an important trend in favor of an association between SES and sleep inequalities [2,3,12,24,25,26,27,28]. Most of them seem to support the hypothesis stating that low SES is associated with an increase in sleep disturbances for children, adolescents and adults [1,10,25,29,30,31,32], while a moderate or a high SES is associated with a decrease in sleep disturbances for the same sub-groups of the general population [2,4,10,11,12]. One reason explaining this empirical discrepancy is the small quantity of research on sleep health inequalities. As revealed by this review, the empirical literature included peer review papers published from 2006 to 2019. It seems relatively new compared to sleep science or public health research related to sleep in other countries, where a few studies on the same subject were published almost twenty years before the first study included in this systematic review [33,34]. Another potential reason explaining the current findings is the experimental design, which is essentially cross-sectional. It is commonly admitted and demonstrated that a cross-sectional study is one of the best experimental designs to rigorously collect data and quickly release pertinent results on a subject [35]. At the same time, it is missing a lot of causal information and correlation, which is very often available with longitudinal study design [36]. It is difficult to establish the causal effects of SES on sleep disturbances in these circumstances. The third reason hypothesized is the incomplete conceptualization of SES in this public health literature. The majority of these articles employed education as a key component to assess the health inequalities of their sample. Education alone cannot capture the complexity of socioeconomic determinants of health inequalities in general and sleep health inequalities in particular [5,6,11,12,37]. It is important to analyze other indicators such as income and employment to understand how far sleep disturbances are important for public health in the countries concerned.
3.3. Recommendations for Future Research
The first recommendation is to perform longitudinal studies to capture the effect of time in the relationship between SES, public health and sleep. Life conditions are markers of health status variance in time and with changes in demography and lifestyle in certain subgroups of the general population, it might be interesting to observe how sleep patterns evolve negatively or positively for future public health policies.
The second recommendation is to use a quantitative measure of sleep components to collect unbiased data. Using actigraphy or polysomnography will add an additional layer of evidence in support of future appropriate public health programs.
The third recommendation is to extend the scope of future research by investigating other sleep disorders. The current literature in Iran and Saudi Arabia focuses on insomnia and OSA, even if a few general sleep parameters such as sleep quality and sleep duration were also explored. Sleep science is very wide and multidisciplinary. An integration of different conceptualizations and theoretical models developed by sleep scientists based on inputs from sociology, psychology or health economics are a few examples of possible actions to improve future research and clinical practice.
3.4. Limitations of This Review
There was no objective sleep measurement in all studies included. The self-assessment of sleep outcomes is very often used in cross-sectional studies, but it was recently demonstrated that the SES influence on health can be observed with quantitative methods [1,2,38]. So, future studies in this region should consider moving forward the knowledge by using an objective measure of sleep to verify trends reported by local authors. There are also a lot of sleep disorders not studied, while a few such as OSA can be linked to other sleep disorders such as excessive daytime sleepiness [8,39,40], and thus have to be studied. Finally, the heterogeneity of SES involved a deep consideration of the sociological approaches and psychological theories in biomedical research, in order to be able to accurately capture this complex concept.
4. Methods
4.1. Literature Search
The relevant citations for this review were identified by searching the databases Web of Science, PubMed/Medline and Google Scholar between January 2000 and July 2022. A combination of the search terms “socioeconomic”, “socio-economic”, “social position”, “social class”, “socioeconomic position”, “determinant*”, “health inequalities”, “sleep”, “sleep disorders”, “sleep disturbances”, “sleep complains”, “sleep outcome”, “sleep health”, “Iran*”, “Saudi Arabia” was used. All included articles were identified following the PRISMA guidelines detailed in Figure 1 [41].
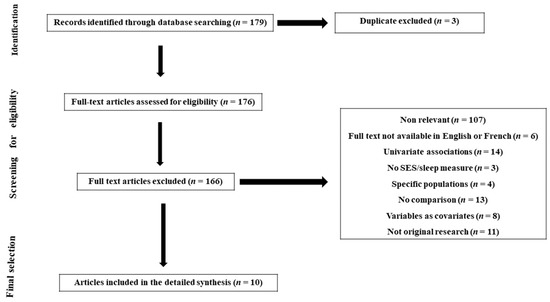
Figure 1.
Prisma flowchart of study selection process.
4.2. Inclusion and Excusion Criteria
Empirical studies were defined as being of any design (cross-sectional, retrospective or longitudinal) that evaluated humans of any age, gender or race/ethnicity from the general populations of Iran and Saudi Arabia. The article should include an objective or a subjective measure of SES, such as education, income, assets, occupation, employment status, perceived SES or self-reported by participants. Indirect measures of SES, such as area deprivation or social class, were also included when individual data were not available. For studies examining children or adolescents, perceived family SES measures such as parental education, parental profession or annual household income were used instead. Studies were excluded based on the following criteria: (1) they were interventional trials, reviews or meta-analyses, case series or case reports, commentary, editorial or did not present original research; (2) they were not written in English, French or Arabic; (3) the full text was not accessible; (4) authors/researchers recruited participants that already presented specific conditions at the beginning of the study (for example, pregnant women or people with chronic sleep disturbances, those taking medication such as sleep aid, etc.); (5) they did not provide statistical significance in cases where either SES or sleep were evaluated as covariates or mediators.
Author Contributions
Conceptualization: F.A.E.S. Methodology, F.A.E.S. Validation: F.A.E.S., C.N. and Y.A.; Formal Analysis: F.A.E.S., C.N. and Y.A.; Writing—Original Draft Preparation, F.A.E.S., C.N. and Y.A.; Writing—Review & Editing, F.A.E.S., C.N. and Y.A.; Visualization, F.A.E.S.; Supervision, F.A.E.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
Thanks to the librarians involved in building the search strategy and validating the keywords used for this review.
Conflicts of Interest
The authors reports no conflict of interest.
References
- Etindele Sosso, F.A. Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings. Clocks Sleep 2022, 4, 80–87. [Google Scholar] [CrossRef]
- Etindele Sosso, F.A.; Holmes, S.D.; Weinstein, A.A. Influence of socioeconomic status on objective sleep measurement: A systematic review and meta-analysis of actigraphy studies. Sleep Health 2021, 7, 417–428. [Google Scholar] [CrossRef]
- Papadopoulos, D.; Sosso, F.E.; Khoury, T.; Surani, S.R. Sleep Disturbances Are Mediators between Socioeconomic Status and Health: A Scoping Review. Int. J. Ment. Health Addict. 2020, 20, 480–504. [Google Scholar] [CrossRef]
- Hale, L.; Troxel, W.; Buysse, D.J. Sleep Health: An Opportunity for Public Health to Address Health Equity. Annu. Rev. Public Health 2020, 41, 81–99. [Google Scholar] [CrossRef]
- Berwick, D.M. The Moral Determinants of Health. JAMA 2020, 324, 225–226. [Google Scholar] [CrossRef]
- Rodriguez, J.M.; Karlamangla, A.S.; Gruenewald, T.L.; Miller-Martinez, D.; Merkin, S.S.; Seeman, T.E. Social stratification and allostatic load: Shapes of health differences in the MIDUS study in the United States. J. Biosoc. Sci. 2019, 51, 627–644. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, D.; Etindele Sosso, F.A. Socioeconomic status and sleep health: A narrative synthesis of three decades of empirical research. J. Clin. Sleep Med. 2022, 19. [Google Scholar] [CrossRef] [PubMed]
- Bendaoud, I.; Etindele Sosso, F.A. Socioeconomic Position and Excessive Daytime Sleepiness: A Systematic Review of Social Epidemiological Studies. Clocks Sleep 2022, 4, 240–259. [Google Scholar] [CrossRef]
- Meneton, P.; Hoertel, N.; Wiernik, E.; Lemogne, C.; Ribet, C.; Bonenfant, S.; Ménard, J.; Goldberg, M.; Zins, M. Work environment mediates a large part of social inequalities in the incidence of several common cardiovascular risk factors: Findings from the Gazel cohort. Soc. Sci. Med. 2018, 216, 59–66. [Google Scholar] [CrossRef]
- Petrovic, D.; Haba-Rubio, J.; Carmeli, C.; Vollenweider, P.; Heinzer, R.; Stringhini, S. Social inequalities in sleep-disordered breathing: Evidence from the CoLaus|HypnoLaus study. J. Sleep Res. 2019, 28, e12799. [Google Scholar] [CrossRef]
- Grandner, M.A. (Ed.) Chapter 5—Social-Ecological Model of Sleep Health. In Sleep and Health; Academic Press: Cambridge, MA, USA, 2019; pp. 45–53. [Google Scholar]
- Sosso, F.A.E.; Kreidlmayer, M.; Pearson, D.; Bendaoud, I. Towards A Socioeconomic Model of Sleep Health among the Canadian Population: A Systematic Review of the Relationship between Age, Income, Employment, Education, Social Class, Socioeconomic Status and Sleep Disparities. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1143–1167. [Google Scholar]
- Ribeiro, A.I.; Amaro, J.; Lisi, C.; Fraga, S. Neighborhood Socioeconomic Deprivation and Allostatic Load: A Scoping Review. Int. J. Environ. Res. Public Health 2018, 15, 1092. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Bahammam, A.; Bin Saeed, A.; Al-Faris, E.; Shaikh, S. Sleep duration and its correlates in a sample of Saudi elementary school children. Singap. Med. J. 2006, 47, 875–881. [Google Scholar]
- Al-Hazzaa, H.M.; Alhussain, M.H.; Alhowikan, A.M.; Obeid, O.A. Insufficient Sleep Duration and Its Association with Breakfast Intake, Overweight/Obesity, Socio-Demographics and Selected Lifestyle Behaviors among Saudi School Children. Nat. Sci. Sleep 2019, 11, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazzaa, H.M.; Al-Hussain, M.H.; Alhowikan, A.M.; Obeid, O.A. Prevalence of short sleep duration and effect of co-morbid medical conditions—A cross-sectional study in Saudi Arabia. J. Fam. Med. Prim. Care 2019, 8, 3334–3339. [Google Scholar]
- Nasim, M.; Saade, M.; AlBuhairan, F. Sleep deprivation: Prevalence and associated factors among adolescents in Saudi Arabia. Sleep Med. 2019, 53, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Amra, B.; Farajzadegan, Z.; Golshan, M.; Fietze, I.; Penzel, T. Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath 2011, 15, 425–429. [Google Scholar] [CrossRef]
- Hassani, S.; Rahnama, N.; Seyedmehdi, S.M.; Yazdanparast, T.; Roozbahani, R.; Attarchi, M.; Naghan, P.A.; Jamaati, H. Association between Occupational Accidents and Sleep Apnea in Hospital Staff. Tanaffos 2015, 14, 201–207. [Google Scholar]
- Heshmat, R.; Qorbani, M.; Ghoreshi, B.; Djalalinia, S.; Tabatabaie, O.R.; Safiri, S.; Noroozi, M.; Motlagh, M.E.; Ahadi, Z.; Asayesh, H.; et al. Association of socioeconomic status with psychiatric problems and violent behaviours in a nationally representative sample of Iranian children and adolescents: The CASPIAN-IV study. BMJ Open 2016, 6, e011615. [Google Scholar] [CrossRef]
- Seyedmehdi, S.M.; Rahnama, N.; Yazdanparast, T.; Jamaati, H.; Attarchi, M.; Naghan, P.A.; Hassani, S. Prevalence of snoring and the risk of sleep apnea in hospital staff. Work 2016, 55, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Foroughi, M.; Malekmohammad, M.; Sharafkhaneh, A.; Emami, H.; Adimi, P.; Khoundabi, B. Prevalence of Obstructive Sleep Apnea in a High-Risk Population Using the Stop-Bang Questionnaire in Tehran, Iran. Tanaffos 2017, 16, 217–224. [Google Scholar]
- Ahmed, A.E.; Al-Jahdali, H.; Fatani, A.; Al-Rouqi, K.; Al-Jahdali, F.; Al-Harbi, A.; Baharoon, S.; Ali, Y.Z.; Khan, M.; Rumayyan, A. The effects of age and gender on the prevalence of insomnia in a sample of the Saudi population. Ethn. Health 2017, 22, 285–294. [Google Scholar] [CrossRef]
- van de Straat, V.; Cheval, B.; Schmidt, R.E.; Sieber, S.; Courvoisier, D.; Kliegel, M.; Burton-Jeangros, C.; Cullati, S.; Bracke, P. Early predictors of impaired sleep: A study on life course socioeconomic conditions and sleeping problems in older adults. Aging Ment. Health 2018, 24, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Sim, C.S.; Sung, J.H.; Lee, J.; Ahn, J.H.; Choe, Y.M.; Park, J. Low Income as a Vulnerable Factor to the Effect of Noise on Insomnia. Psychiatry Investig. 2018, 15, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Matthews, K.A.; Jennings, J.R.; Lee, L. Socioeconomic status in childhood predicts sleep continuity in adult Black and White men. Sleep Health 2018, 4, 49–55. [Google Scholar] [CrossRef]
- Seo, W.H.; Kwon, J.H.; Eun, S.-H.; Kim, G.; Han, K.; Choi, B.M. Effect of socio-economic status on sleep. J. Paediatr. Child Health 2017, 53, 592–597. [Google Scholar] [CrossRef]
- Hawkins, S.S.; Takeuchi, D.T. Social determinants of inadequate sleep in US children and adolescents. Public Health 2016, 138, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Kolla, B.P.; He, J.-P.; Mansukhani, M.; Frye, M.A.; Merikangas, K. Excessive sleepiness and associated symptoms in the U.S. adult population: Prevalence, correlates, and comorbidity. Sleep Health 2020, 6, 79–87. [Google Scholar] [CrossRef]
- Wu, W.; Wang, W.; Dong, Z.; Xie, Y.; Gu, Y.; Zhang, Y.; Li, M.; Tan, X. Sleep Quality and Its Associated Factors among Low-Income Adults in a Rural Area of China: A Population-Based Study. Int. J. Environ. Res. Public Health 2018, 15, 2055. [Google Scholar] [CrossRef]
- Doane, L.D.; Breitenstein, R.S.; Beekman, C.; Clifford, S.; Smith, T.J.; Lemery-Chalfant, K. Early Life Socioeconomic Disparities in Children’s Sleep: The Mediating Role of the Current Home Environment. J. Youth Adolesc. 2018, 48, 56–70. [Google Scholar] [CrossRef] [PubMed]
- Counts, C.J.; Grubin, F.C.; John-Henderson, N.A. Childhood socioeconomic status and risk in early family environments: Predictors of global sleep quality in college students. Sleep Health 2018, 4, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Habte-Gabr, E.; Wallace, R.B.; Colsher, P.L.; Hulbert, J.R.; White, L.R.; Smith, I.M. Sleep patterns in rural elders: Demographic, health, and psychobehavioral correlates. J. Clin. Epidemiol. 1991, 44, 5–13. [Google Scholar] [CrossRef]
- Touitou, Y.; Motohashi, Y.; Reinberg, A.; Bourdeleau, P.; Bogdan, A. Effect of shift work on the night-time secretory patterns of melatonin, prolactin, cortisol and testosterone. Eur. J. Appl. Physiol. Occup. Physiol. 1990, 60, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cheng, Z. Cross-Sectional Studies: Strengths, Weaknesses, and Recommendations. Chest 2020, 158 (Suppl. 1), S65–S71. [Google Scholar] [CrossRef]
- Caruana, E.J.; Roman, M.; Hernández-Sánchez, J.; Solli, P. Longitudinal studies. J. Thorac. Dis. 2015, 7, E537–E540. [Google Scholar]
- Vermeiren, A.P.; Willeboordse, M.; Oosterhoff, M.; Bartelink, N.; Muris, P.; Bosma, H. Socioeconomic multi-domain health inequalities in Dutch primary school children. Eur. J. Public Health 2018, 28, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Wendt, A.; da Silva, I.C.M.; Gonçalves, H.; Assunção, M.C.F.; Menezes, A.M.B.; Wehrmeister, F.C. Sleep parameters measured by accelerometry: Descriptive analyses from the 22-year follow-up of the Pelotas 1993 birth cohort. Sleep Med. 2020, 67, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Etindele-Sosso, F.A. Insomnia, excessive daytime sleepiness, anxiety, depression and socioeconomic status among customer service employees in Canada. Sleep Sci. 2020, 13, 54–64. [Google Scholar] [PubMed]
- Chami, H.A.; Ghandour, B.; Isma’Eel, H.; Nasreddine, L.; Nasrallah, M.; Tamim, H. Sleepless in Beirut: Sleep duration and associated subjective sleep insufficiency, daytime fatigue, and sleep debt in an urban environment. Sleep Breath 2020, 24, 357–367. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).