Effects of One Night of Forced Wakefulness on Morning Resting Blood Pressure in Humans: The Role of Biological Sex and Weight Status
Abstract
1. Introduction
2. Results
2.1. Cohort Characteristics
2.2. Main Effects of Experimental Condition, Biological Sex, and Weight Group Status on Morning Resting BP
2.3. Sex-Specific Effects of Forced Overnight Wakefulness on BP
2.4. Weight Group-Specific Effects of Forced Overnight Wakefulness on BP
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Design and Procedure
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Madeira, S.G.; Fernandes, C.; Paiva, T.; Moreira, C.S.; Caldeira, D. The Impact of Different Types of Shift Work on Blood Pressure and Hypertension: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6738. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Li, J.; Feng, D.; Liu, J.; Hao, Y.; Zhen, Y.; Hao, X.; Liu, F.; Zuo, A.; Yang, X.; et al. Effect of frequency and pattern of night shift on hypertension risk in female nurses: A cross-sectional study. J. Hypertens. 2021, 39, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Xu, C.; Liu, Q.; Yan, Q.; Liang, J.; Weng, Z.; Zhang, X.; Xu, J.; Hang, D.; Gu, A. Night Shift Work, Genetic Risk, and Hypertension. Mayo Clin. Proc. 2022. [Google Scholar] [CrossRef]
- Mancia, G.; Ferrari, A.; Gregorini, L.; Parati, G.; Pomidossi, G.; Bertinieri, G.; Grassi, G.; di Rienzo, M.; Pedotti, A.; Zanchetti, A. Blood pressure and heart rate variabilities in normotensive and hypertensive human beings. Circ. Res. 1983, 53, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.E. Circadian variation in cardiovascular events. Am. J. Hypertens. 1999, 12 Pt 2, 35S–42S. [Google Scholar] [CrossRef][Green Version]
- Reckelhoff, J.F. Gender Differences in the Regulation of Blood Pressure. Hypertension 2001, 37, 1199–1208. [Google Scholar] [CrossRef]
- Wiinberg, N.; Høegholm, A.; Christensen, H.R.; Bang, L.E.; Mikkelsen, K.L.; Nielsen, P.E.; Svendsen, T.L.; Kampmann, J.P.; Madsen, N.H.; Bentzon, M.W. 24-h ambulatory blood pressure in 352 normal Danish subjects, related to age and gender. Am. J. Hypertens. 1995, 8 Pt 1, 978–986. [Google Scholar] [CrossRef]
- Siani, A.; Cappuccio, F.P.; Barba, G.; Trevisan, M.; Farinaro, E.; Iacone, R.; Russo, O.; Russo, P.; Mancini, M.; Strazzullo, P. The relationship of waist circumference to blood pressure: The Olivetti heart studyAm. J. Hypertens. 2002, 15, 780–786. [Google Scholar] [CrossRef]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight#:~:text=Facts%20about%20overweight%20and%20obesity&text=In%202016%2C%2039%25%20of%20adults,tripled%20between%201975%20and%202016 (accessed on 24 August 2022).
- Resnick, H.E.; Lindsay, R.S.; McDermott, M.M.; Devereux, R.B.; Jones, K.L.; Fabsitz, R.R.; Howard, B.V. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: The Strong Heart Study. Circulation 2004, 109, 733–739. [Google Scholar] [CrossRef]
- Niiranen, T.J.; Hänninen, M.R.; Johansson, J.; Reunanen, A.; Jula, A.M. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: The Finn-Home study. Hypertension 2010, 55, 1346–1351. [Google Scholar] [CrossRef]
- Zavada, A.; Gordijn, M.C.; Beersma, D.G.; Daan, S.; Roenneberg, T. Comparison of the Munich Chronotype Questionnaire with the Horne-Ostberg's Morningness-Eveningness Score. Chronobiol. Int. 2005, 22, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Adekolu, O.; Zinchuk, A. Sleep Deficiency in Obstructive Sleep Apnea. Clin. Chest Med. 2022, 43, 353–371. [Google Scholar] [CrossRef] [PubMed]
- Kario, K. Obstructive sleep apnea syndrome and hypertension: Mechanism of the linkage and 24-h blood pressure control. Hypertens. Res. 2009, 32, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Varghese, L.; Rebekah, G.; Priya, N.; Oliver, A.; Kurien, R. Oxygen desaturation index as alternative parameter in screening patients with severe obstructive sleep apnea. Sleep Sci. 2022, 15, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 24 August 2022).
- Aatola, H.; Kähönen, N.; Juonala, M.; Viikari, J.S.; Hulkkonen, J.; Laitinen, T.; Taittonen, L.; Lehtimäki, T.; Raitakari, O.T.; Kahonen, M. Lifetime risk factors and arterial pulse wave velocity in adulthood: The cardiovascular risk in young Finns study. Hypertension 2010, 55, 806–811. [Google Scholar] [CrossRef]
- Manohar, S.; Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Herrmann, S.M. Associations of rotational shift work and night shift status with hypertension: A systematic review and meta-analysis. J. Hypertens. 2017, 35, 1929–1937. [Google Scholar] [CrossRef]
- Ferguson, J.; Costello, S.; Neophytou, A.M.; Balmes, J.R.; Bradshaw, P.T.; Cullen, M.; Eisen, E.A. Night and rotational work exposure within the last 12 months and risk of incident hypertension. Scand. J. Work. Environ. Health 2019, 45, 256–266. [Google Scholar] [CrossRef]
- Ogawa, Y.; Kanbayashi, T.; Saito, Y.; Takahashi, Y.; Kitajima, T.; Takahashi, K.; Hishikawa, Y.; Shimizu, T. Total Sleep Deprivation Elevates Blood Pressure Through Arterial Baroreflex Resetting: A Study with Microneurographic Technique. Sleep 2003, 26, 986–989. [Google Scholar] [CrossRef]
- Wei, T.; Li, C.; Heng, Y.; Gao, X.; Zhang, G.; Wang, H.; Zhao, X.; Meng, Z.; Zhang, Y.; Hou, H. Association between night-shift work and level of melatonin: Systematic review and meta-analysis. Sleep Med. 2020, 75, 502–509. [Google Scholar] [CrossRef]
- Paulis, L.; Šimko, F. Blood pressure modulation and cardiovascular protection by melatonin: Potential mechanisms behind. Physiol. Res. 2007, 56, 671–684. [Google Scholar] [CrossRef]
- Baker, J.; Kimpinski, K. Role of melatonin in blood pressure regulation: An adjunct anti-hypertensive agent. Clin. Exp. Pharmacol. Physiol. 2018, 45, 755–766. [Google Scholar] [CrossRef] [PubMed]
- Scheer, F.; Van Montfrans, G.A.; Van Someren, E.J.W.; Mairuhu, G.; Buijs, R.M. Daily Nighttime Melatonin Reduces Blood Pressure in Male Patients With Essential Hypertension. Hypertension 2004, 43, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Gubin, D.; Gubin, G.D.; Gapon, L.I.; Weinert, D. Daily Melatonin Administration Attenuates Age-Dependent Disturbances of Cardiovascular Rhythms. Curr. Aging Sci. 2016, 9, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.R.; Haas, E.; Barton, M. Gender differences of cardiovascular disease: New perspectives for estrogen receptor signaling. Hypertension 2006, 47, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Dubey, R.K.; Oparil, S.; Imthurn, B.; Jackson, E.K. Sex hormones and hypertension. Cardiovasc. Res. 2002, 53, 688–708. [Google Scholar] [CrossRef]
- Millar-Craig, M.W.; Bishop, C.N.; Raftery, E.B. Circadian variation of blood-pressure. Lancet 1978, 1, 795–797. [Google Scholar] [CrossRef]
- van Egmond, L.T.; Meth, E.M.; Bukhari, S.; Engström, J.; Ilemosoglou, M.; Keller, J.A.; Zhou, S.; Schiöth, H.B.; Benedict, C. How Sleep-Deprived People See and Evaluate Others’ Faces: An Experimental Study. Nat. Sci. Sleep 2022, 14, 867–876. [Google Scholar] [CrossRef]
- van Egmond, L.T.; Bukhari, S.; Benedet, A.L.; Ashton, N.J.; Meth, E.M.S.; Boukas, A.; Engström, J.; Ilemosoglou, M.; Blennow, K.; Henrik Zetterberg, H.; et al. Acute sleep loss increases CNS health biomarkers and compromises the ability to stay awake in a sex-and weight-specific manner. Transl. Psychiatry 2022. accepted. [Google Scholar] [CrossRef]
- Tamaki, M.; Bang, J.W.; Watanabe, T.; Sasaki, Y. Night Watch in One Brain Hemisphere during Sleep Associated with the First-Night Effect in Humans. Curr. Biol. 2016, 26, 1190–1194. [Google Scholar] [CrossRef]
- The AASM Manual for the Scoring of Sleep and Associated Events. Available online: https://aasm.org/resources/pdf/scoring-manual-preface.pdf (accessed on 24 August 2022).
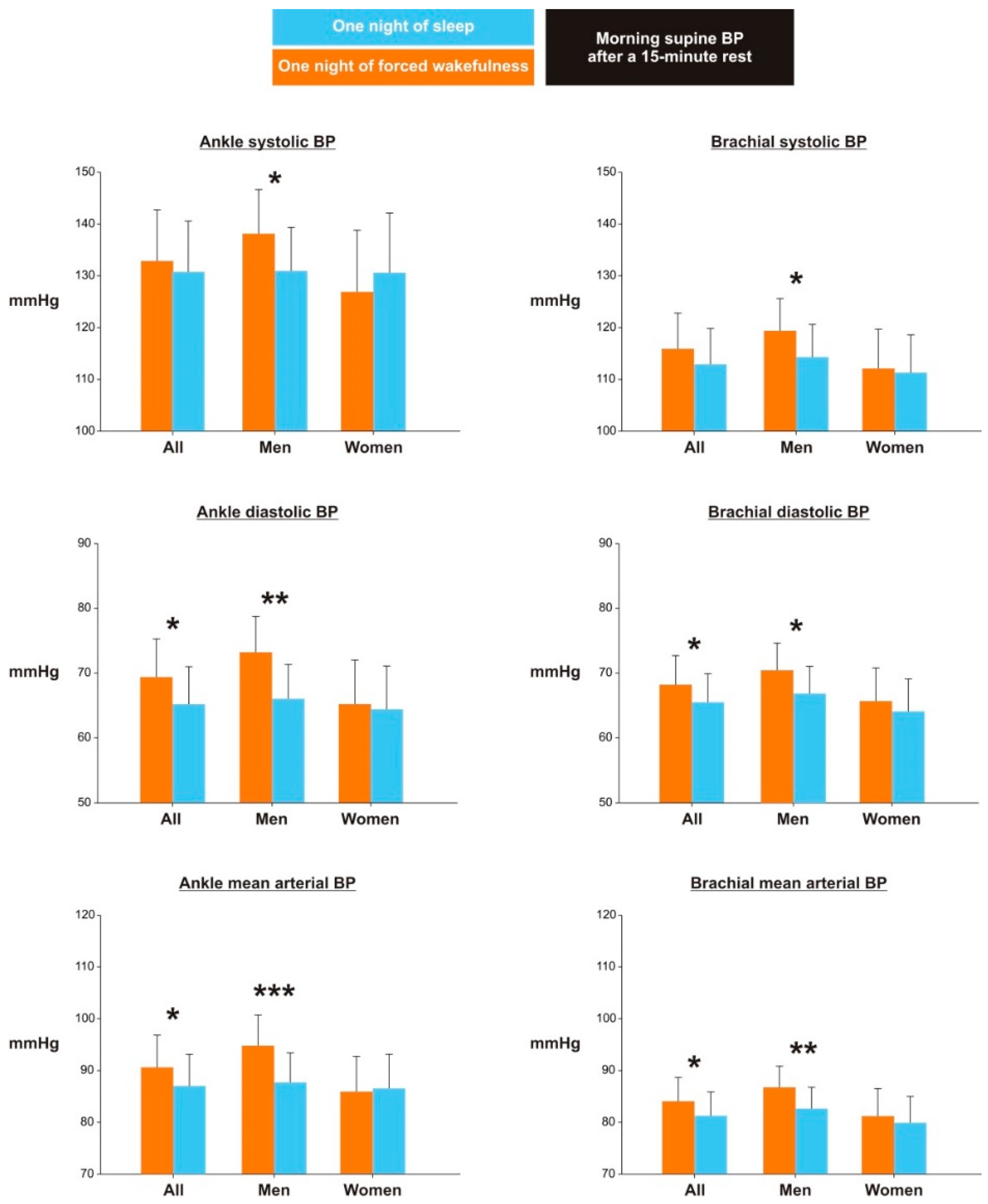
| Outcome | Experimental Condition (Co) | Biological Sex (Sex) | Weight Group (W) | p for Interaction | ||||
|---|---|---|---|---|---|---|---|---|
| Wakefulness | Sleep | Men | Women | Obesity | Normal Weight | Co*Sex | Co*W | |
| No. of participants | 47 | 45 | 26 | 21 | 22 | 25 | -- | -- |
| No. of women | 21 | 21 | 0 | 21 | 10 | 11 | -- | -- |
| No. of participants with obesity | 22 | 20 | 12 | 10 | 22 | 0 | -- | -- |
| Ankle site | ||||||||
| Systolic BP, mmHg | 132.9 ± 9.9 | 130.8 ± 9.8 | 133.5 ± 9.9 | 130.2 ± 9.9 | 134.9 ± 9.9 * | 128.8 ± 9.9 | 0.019 | 0.470 |
| Diastolic BP, mmHg | 69.4 ± 5.9 * | 65.2 ± 5.8 | 69.4 ± 5.9 ** | 65.3 ± 5.9 | 68.5 ± 5.9 | 66.1 ± 5.9 | 0.076 | 0.567 |
| Mean arterial BP, mmHg | 90.7 ± 6.2 * | 87.1 ± 6.1 | 90.5 ± 6.1 | 87.3 ± 6.2 | 90.8 ± 6.2 * | 86.9 ± 6.1 | 0.018 | 0.476 |
| Brachial site | ||||||||
| Systolic BP, mmHg | 115.9 ± 6.9 | 112.9 ± 6.9 | 117.1 ± 6.9 * | 111.7 ± 7.0 | 117.3 ± 7.0 ** | 111.5 ± 6.9 | 0.245 | 0.299 |
| Diastolic BP, mmHg | 68.2 ± 4.5 * | 65.5 ± 4.4 | 68.8 ± 4.5 ** | 65.0 ± 4.5 | 68.9 ± 4.5 *** | 64.9 ± 4.4 | 0.453 | 0.564 |
| Mean arterial BP, mmHg | 84.1 ± 4.6 * | 81.3 ± 4.6 | 84.9 ± 4.6 *** | 80.6 ± 4.6 | 85.0 ± 4.6 *** | 80.5 ± 4.6 | 0.298 | 0.927 |
| Outcome | Men (§) | Women (§) | Normal Weight (†) | Obesity (†) | ||||
|---|---|---|---|---|---|---|---|---|
| Wakefulness | Sleep | Wakefulness | Sleep | Wakefulness | Sleep | Wakefulness | Sleep | |
| Ankle site | ||||||||
| Systolic BP, mmHg | 138.1 ± 8.5 * | 130.9 ± 8.4 | 126.9 ± 11.9 | 130.6 ± 11.5 | 130.8 ± 7.1 | 127.0 ± 7.0 | 134.7 ± 13.6 | 134.4 ± 13.1 |
| Diastolic BP, mmHg | 73.2 ± 5.5 *** | 66.0 ± 5.3 | 65.2 ± 6.8 | 64.4 ± 6.7 | 68.8 ± 6.4 * | 63.6 ± 6.1 | 69.7 ± 5.8 | 67.2 ± 5.9 |
| Mean arterial BP, mmHg | 94.8 ± 5.9 *** | 87.7 ± 5.7 | 85.9 ± 6.8 | 86.5 ± 6.6 | 89.5 ± 6.0 * | 84.8 ± 5.7 | 91.6 ± 7.1 | 89.3 ± 6.9 |
| Brachial site | ||||||||
| Systolic BP, mmHg | 119.4 ± 6.2 * | 114.3 ± 6.3 | 112.1 ± 7.6 | 111.3 ± 7.3 | 111.8 ± 6.8 | 110.4 ± 6.8 | 120.2 ± 6.9 | 115.0 ± 6.9 |
| Diastolic BP, mmHg | 70.5 ± 4.2 * | 66.9 ± 4.2 | 65.7 ± 5.1 | 64.1 ± 5.0 | 66.6 ± 4.0 * | 63.2 ± 3.9 | 69.8 ± 5.3 | 67.8 ± 5.3 |
| Mean arterial BP, mmHg | 86.8 ± 4.1 ** | 82.7 ± 4.1 | 81.2 ± 5.3 | 79.9 ± 5.1 | 81.6 ± 4.3 | 78.9 ± 4.2 | 86.5 ± 5.2 | 83.7 ± 5.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Egmond, L.T.; Xue, P.; Meth, E.M.S.; Ilemosoglou, M.; Engström, J.; Benedict, C. Effects of One Night of Forced Wakefulness on Morning Resting Blood Pressure in Humans: The Role of Biological Sex and Weight Status. Clocks & Sleep 2022, 4, 458-465. https://doi.org/10.3390/clockssleep4030036
van Egmond LT, Xue P, Meth EMS, Ilemosoglou M, Engström J, Benedict C. Effects of One Night of Forced Wakefulness on Morning Resting Blood Pressure in Humans: The Role of Biological Sex and Weight Status. Clocks & Sleep. 2022; 4(3):458-465. https://doi.org/10.3390/clockssleep4030036
Chicago/Turabian Stylevan Egmond, Lieve T., Pei Xue, Elisa M. S. Meth, Maria Ilemosoglou, Joachim Engström, and Christian Benedict. 2022. "Effects of One Night of Forced Wakefulness on Morning Resting Blood Pressure in Humans: The Role of Biological Sex and Weight Status" Clocks & Sleep 4, no. 3: 458-465. https://doi.org/10.3390/clockssleep4030036
APA Stylevan Egmond, L. T., Xue, P., Meth, E. M. S., Ilemosoglou, M., Engström, J., & Benedict, C. (2022). Effects of One Night of Forced Wakefulness on Morning Resting Blood Pressure in Humans: The Role of Biological Sex and Weight Status. Clocks & Sleep, 4(3), 458-465. https://doi.org/10.3390/clockssleep4030036






