The Effect of Bright Light Treatment on Rest–Activity Rhythms in People with Dementia: A 24-Week Cluster Randomized Controlled Trial
Abstract
:1. Introduction
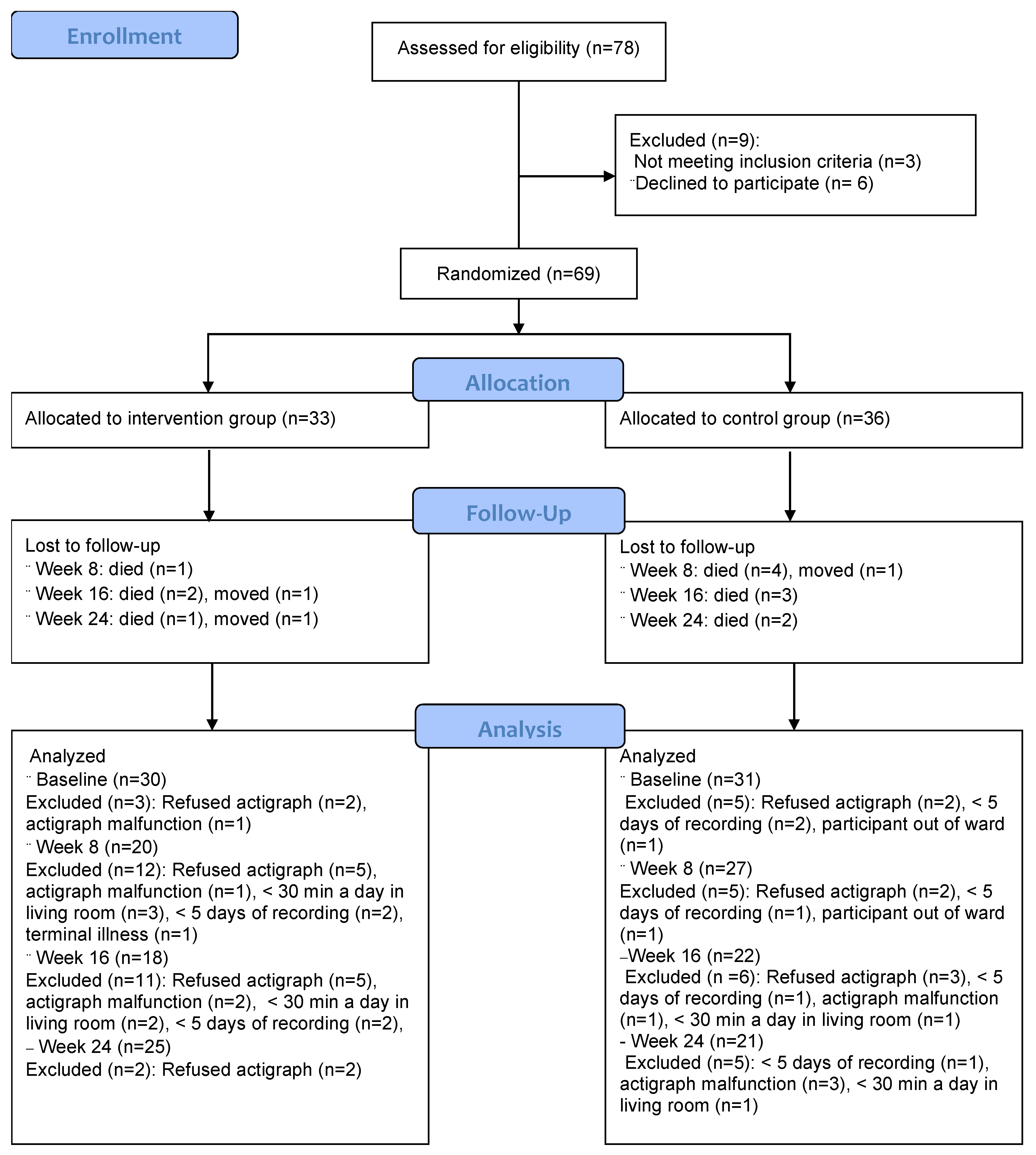
2. Materials and Methods
2.1. Participants
2.2. Sample Size and Power Calculation
2.3. Delivery of the Intervention
2.4. Group Allocation and Blinding
2.5. Measurements
2.5.1. Rest–Activity Rhythms
2.5.2. Light Measurements
2.5.3. Other Measurements
2.6. Data Management and Statistical Analyses
2.7. Ethical Considerations
3. Results
3.1. Sample Descriptive Statistics
3.2. Adherence
3.3. Light Measurements
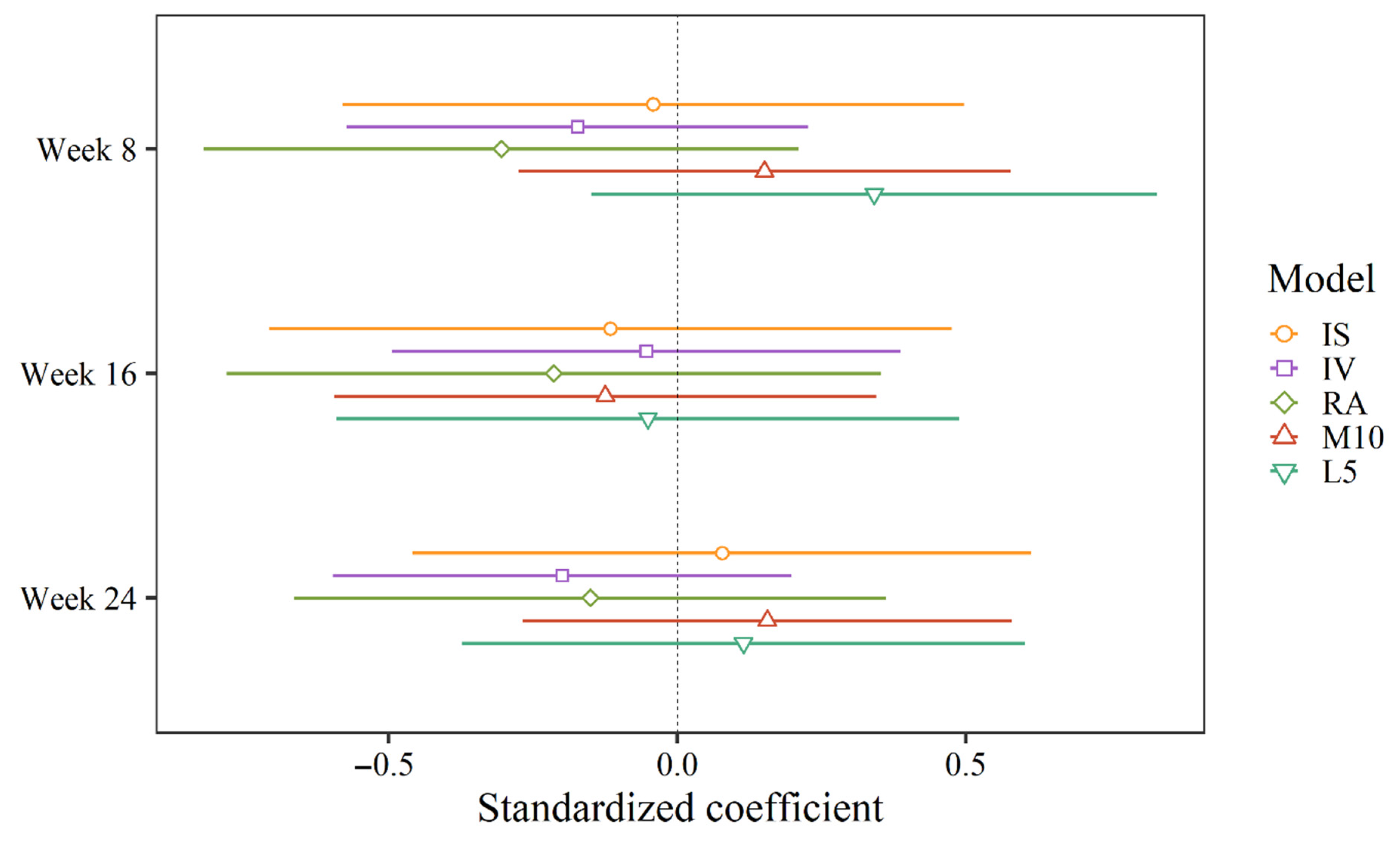
3.4. Rest–Activity Rhythms
Correlations between Circadian Rhythm Outcomes at Baseline
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ancoli-Israel, S.; Cole, R.; Alessi, C.; Chambers, M.; Moorcroft, W.; Pollak, C.P. The role of actigraphy in the study of sleep and circadian rhythms. Sleep 2003, 26, 342–392. [Google Scholar] [CrossRef] [Green Version]
- Smagula, S.F.; Gujral, S.; Capps, C.S.; Krafty, R.T. A Systematic Review of Evidence for a Role of Rest-Activity Rhythms in Dementia. Front. Psychiatry 2019, 10, 778. [Google Scholar] [CrossRef] [PubMed]
- Pat-Horenczyk, R.; Klauber, M.R.; Shochat, T.; Ancoli-Israel, S. Hourly profiles of sleep and wakefulness in severely versus mild-moderately demented nursing home patients. Aging 1998, 10, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Hofman, M.A.; Swaab, D.F. Living by the clock: The circadian pacemaker in older people. Ageing Res. Rev. 2006, 5, 33–51. [Google Scholar] [CrossRef] [PubMed]
- Reppert, S.M.; Weaver, D.R. Coordination of circadian timing in mammals. Nature 2002, 418, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Leng, Y.; Musiek, E.S.; Hu, K.; Cappuccio, F.P.; Yaffe, K. Association between circadian rhythms and neurodegenerative diseases. Lancet Neurol. 2019, 18, 307–318. [Google Scholar] [CrossRef]
- Baron, K.G.; Reid, K.J. Circadian misalignment and health. Int. Rev. Psychiatry 2014, 26, 139–154. [Google Scholar] [CrossRef] [Green Version]
- Duffy, J.F.; Zitting, K.M.; Chinoy, E.D. Aging and Circadian Rhythms. Sleep Med. Clin. 2015, 10, 423–434. [Google Scholar] [CrossRef] [Green Version]
- Saito, Y.; Kume, Y.; Kodama, A.; Sato, K.; Yasuba, M. The association between circadian rest-activity patterns and the behavioral and psychological symptoms depending on the cognitive status in Japanese nursing-home residents. Chronobiol. Int. 2018, 35, 1670–1679. [Google Scholar] [CrossRef]
- Martin, J.; Marler, M.; Shochat, T.; Ancoli-Israel, S. Circadian rhythms of agitation in institutionalized patients with Alzheimer’s disease. Chronobiol. Int. 2000, 17, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Hofman, M.A. The human circadian clock and aging. Chronobiol. Int. 2000, 17, 245–259. [Google Scholar] [CrossRef] [PubMed]
- Duffy, J.F.; Kronauer, R.E.; Czeisler, C.A. Phase-shifting human circadian rhythms: Influence of sleep timing, social contact and light exposure. J. Physiol. 1996, 495 Pt 1, 289–297. [Google Scholar] [CrossRef]
- Thapan, K.; Arendt, J.; Skene, D.J. An action spectrum for melatonin suppression: Evidence for a novel non-rod, non-cone photoreceptor system in humans. J. Physiol. 2001, 535, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.L.; Mainster, M.A. Circadian photoreception: Ageing and the eye’s important role in systemic health. Br. J. Ophthalmol. 2008, 92, 1439–1444. [Google Scholar] [CrossRef]
- Mishima, K.; Okawa, M.; Shimizu, T.; Hishikawa, Y. Diminished melatonin secretion in the elderly caused by insufficient environmental illumination. J. Clin. Endocrinol. Metab. 2001, 86, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Kolberg, E.; Pallesen, S.; Hjetland, G.J.; Nordhus, I.H.; Thun, E.; Flo-Groeneboom, E. Insufficient melanopic equivalent daylight illuminance in nursing home dementia units across seasons and gaze directions. Light Res. Technol. 2021. [Google Scholar] [CrossRef]
- Campbell, S.S.; Kripke, D.F.; Gillin, J.C.; Hrubovcak, J.C. Exposure to light in healthy elderly subjects and Alzheimer’s patients. Physiol. Behav. 1988, 42, 141–144. [Google Scholar] [CrossRef]
- Shochat, T.; Martin, J.; Marler, M.; Ancoli-Israel, S. Illumination levels in nursing home patients: Effects on sleep and activity rhythms. J. Sleep Res. 2000, 9, 373–379. [Google Scholar] [CrossRef]
- Dodson, E.R.; Zee, P.C. Therapeutics for Circadian Rhythm Sleep Disorders. Sleep Med. Clin. 2010, 5, 701–715. [Google Scholar] [CrossRef] [Green Version]
- Van Maanen, A.; Meijer, A.M.; van der Heijden, K.B.; Oort, F.J. The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 29, 52–62. [Google Scholar] [CrossRef]
- Riemersma-van der Lek, R.F.; Swaab, D.F.; Twisk, J.; Hol, E.M.; Hoogendijk, W.J.; Van Someren, E.J. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: A randomized controlled trial. JAMA 2008, 299, 2642–2655. [Google Scholar] [CrossRef]
- Van Someren, E.J.; Kessler, A.; Mirmiran, M.; Swaab, D.F. Indirect bright light improves circadian rest-activity rhythm disturbances in demented patients. Biol. Psychiatry 1997, 41, 955–963. [Google Scholar] [CrossRef] [Green Version]
- Onega, L.L.; Pierce, T.W.; Epperly, L. Effect of Bright Light Exposure on Depression and Agitation in Older Adults with Dementia. Issues Ment. Health Nurs. 2016, 37, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Munch, M.; Schmieder, M.; Bieler, K.; Goldbach, R.; Fuhrmann, T.; Zumstein, N.; Vonmoos, P.; Scartezzini, J.L.; Wirz-Justice, A.; Cajochen, C. Bright Light Delights: Effects of Daily Light Exposure on Emotions, Restactivity Cycles, Sleep and Melatonin Secretion in Severely Demented Patients. Curr. Alzheimer Res. 2017, 14, 1063–1075. [Google Scholar] [CrossRef]
- Fetveit, A.; Bjorvatn, B. The effects of bright-light therapy on actigraphical measured sleep last for several weeks post-treatment. A study in a nursing home population. J. Sleep Res. 2004, 13, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Ancoli-Israel, S.; Gehrman, P.; Martin, J.L.; Shochat, T.; Marler, M.; Corey-Bloom, J.; Levi, L. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behav. Sleep Med. 2003, 1, 22–36. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Hunter, C.M.; Higgins, P.; Hornick, T.; Jones, G.E.; Plitnick, B.; Brons, J.; Rea, M.S. Tailored Lighting Intervention for Persons with Dementia and Caregivers Living at Home. Sleep Health 2015, 1, 322–330. [Google Scholar] [CrossRef] [Green Version]
- Figueiro, M.G.; Plitnick, B.A.; Lok, A.; Jones, G.E.; Higgins, P.; Hornick, T.R.; Rea, M.S. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin. Interv. Aging 2014, 9, 1527–1537. [Google Scholar] [CrossRef] [Green Version]
- Sloane, P.D.; Figueiro, M.; Garg, S.; Cohen, L.W.; Reed, D.; Williams, C.S.; Preisser, J.; Zimmerman, S. Effect of home-based light treatment on persons with dementia and their caregivers. Light Res. Technol. 2015, 47, 161–176. [Google Scholar] [CrossRef]
- Wahnschaffe, A.; Nowozin, C.; Haedel, S.; Rath, A.; Appelhof, S.; Münch, M.; Kunz, D. Implementation of dynamic lighting in a nursing home: Impact on agitation but not on rest-activity patterns. Curr. Alzheimer Res. 2017, 14, 1076–1083. [Google Scholar] [CrossRef]
- Sloane, P.D.; Williams, C.S.; Mitchell, C.M.; Preisser, J.S.; Wood, W.; Barrick, A.L.; Hickman, S.E.; Gill, K.S.; Connell, B.R.; Edinger, J.; et al. High-intensity environmental light in dementia: Effect on sleep and activity. J. Am. Geriatr. Soc. 2007, 55, 1524–1533. [Google Scholar] [CrossRef] [PubMed]
- Hjetland, G.J.; Pallesen, S.; Thun, E.; Kolberg, E.; Nordhus, I.H.; Flo, E. Light interventions and sleep, circadian, behavioral, and psychological disturbances in dementia: A systematic review of methods and outcomes. Sleep Med. Rev. 2020, 52, 101310. [Google Scholar] [CrossRef] [PubMed]
- Mitolo, M.; Tonon, C.; La Morgia, C.; Testa, C.; Carelli, V.; Lodi, R. Effects of Light Treatment on Sleep, Cognition, Mood, and Behavior in Alzheimer’s Disease: A Systematic Review. Dement. Geriatr. Cogn. Disord. 2018, 46, 371–384. [Google Scholar] [CrossRef]
- Forbes, D.; Blake, C.M.; Thiessen, E.J.; Peacock, S.; Hawranik, P. Light therapy for improving cognition, activities of daily living, sleep, challenging behaviour, and psychiatric disturbances in dementia. Cochrane Database Syst. Rev. 2014, 2, CD003946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Donner, A. Some aspects of the design and analysis of cluster randomization trials. J. R. Stat. Soc. Ser. C. 2002, 47, 95–113. [Google Scholar] [CrossRef]
- Peyvandi, S.; Hernandez-Andres, J.; Olmo, F.J.; Nieves, J.L.; Romero, J. Colorimetric analysis of outdoor illumination across varieties of atmospheric conditions. J. Opt. Soc. Am. Opt. Image Sci. Vis. 2016, 33, 1049–1059. [Google Scholar] [CrossRef] [Green Version]
- Camargos, E.F.; Louzada, F.M.; Nobrega, O.T. Wrist actigraphy for measuring sleep in intervention studies with Alzheimer’s disease patients: Application, usefulness, and challenges. Sleep Med. Rev. 2013, 17, 475–488. [Google Scholar] [CrossRef]
- Neikrug, A.B.; Chen, I.Y.; Palmer, J.R.; McCurry, S.M.; Von Korff, M.; Perlis, M.; Vitiello, M.V. Characterizing Behavioral Activity Rhythms in Older Adults Using Actigraphy. Sensors 2020, 20, 549. [Google Scholar] [CrossRef] [Green Version]
- Van Someren, E.J.; Swaab, D.F.; Colenda, C.C.; Cohen, W.; McCall, W.V.; Rosenquist, P.B. Bright light therapy: Improved sensitivity to its effects on rest-activity rhythms in Alzheimer patients by application of nonparametric methods. Chronobiol. Int. 1999, 16, 505–518. [Google Scholar] [CrossRef]
- Marler, M.R.; Gehrman, P.; Martin, J.L.; Ancoli-Israel, S. The sigmoidally transformed cosine curve: A mathematical model for circadian rhythms with symmetric non-sinusoidal shapes. Stat. Med. 2006, 25, 3893–3904. [Google Scholar] [CrossRef] [PubMed]
- Witting, W.; Kwa, I.H.; Eikelenboom, P.; Mirmiran, M.; Swaab, D.F. Alterations in the circadian rest-activity rhythm in aging and Alzheimer’s disease. Biol. Psychiatry 1990, 27, 563–572. [Google Scholar] [CrossRef] [Green Version]
- Van Someren, E.J.; Hagebeuk, E.E.; Lijzenga, C.; Scheltens, P.; de Rooij, S.E.; Jonker, C.; Pot, A.M.; Mirmiran, M.; Swaab, D.F. Circadian rest-activity rhythm disturbances in Alzheimer’s disease. Biol. Psychiatry 1996, 40, 259–270. [Google Scholar] [CrossRef] [Green Version]
- Hatfield, C.F.; Herbert, J.; van Someren, E.J.; Hodges, J.R.; Hastings, M.H. Disrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer’s dementia. Brain 2004, 127, 1061–1074. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oosterman, J.M.; van Someren, E.J.; Vogels, R.L.; Van Harten, B.; Scherder, E.J. Fragmentation of the rest-activity rhythm correlates with age-related cognitive deficits. J. Sleep Res. 2009, 18, 129–135. [Google Scholar] [CrossRef]
- Carvalho-Bos, S.S.; Riemersma-van der Lek, R.F.; Waterhouse, J.; Reilly, T.; Van Someren, E.J. Strong association of the rest-activity rhythm with well-being in demented elderly women. Am. J. Geriatr. Psychiatry 2007, 15, 92–100. [Google Scholar] [CrossRef] [Green Version]
- Kume, Y.; Kodama, A.; Sato, K.; Kurosawa, S.; Ishikawa, T.; Ishikawa, S. Sleep/awake status throughout the night and circadian motor activity patterns in older nursing-home residents with or without dementia, and older community-dwelling people without dementia. Int. Psychogeriatr. 2016, 28, 2001–2008. [Google Scholar] [CrossRef] [PubMed]
- Blume, C.; Santhi, N.; Schabus, M. ‘nparACT’ package for R: A free software tool for the non-parametric analysis of actigraphy data. MethodsX 2016, 3, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Gehrman, P.; Marler, M.; Martin, J.L.; Shochat, T.; Corey-Bloom, J.; Ancoli-Israel, S. The relationship between dementia severity and rest/activity circadian rhythms. Neuropsychiatr. Dis. Treat. 2005, 1, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Ancoli-Israel, S.; Martin, J.L.; Kripke, D.F.; Marler, M.; Klauber, M.R. Effect of light treatment on sleep and circadian rhythms in demented nursing home patients. J. Am. Geriatr. Soc. 2002, 50, 282–289. [Google Scholar] [CrossRef]
- Tranah, G.J.; Blackwell, T.; Stone, K.L.; Ancoli-Israel, S.; Paudel, M.L.; Ensrud, K.E.; Cauley, J.A.; Redline, S.; Hillier, T.A.; Cummings, S.R.; et al. Circadian activity rhythms and risk of incident dementia and mild cognitive impairment in older women. Ann. Neurol. 2011, 70, 722–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graves, J.L. RAR. Available online: https://github.com/JessLGraves/RAR (accessed on 15 November 2020).
- Spitschan, M.; Stefani, O.; Blattner, P.; Gronfier, C.; Lockley, S.W.; Lucas, R.J. How to Report Light Exposure in Human Chronobiology and Sleep Research Experiments. Clocks Sleep 2019, 1, 24. [Google Scholar] [CrossRef] [Green Version]
- International Commission on Illumination. Available online: http://cie.co.at/publications/cie-system-metrology-optical-radiation-iprgc-influenced-responses-light-0 (accessed on 3 September 2020).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef] [PubMed]
- Reisberg, B. Functional assessment staging (FAST). Psychopharmacol. Bull. 1988, 24, 653–659. [Google Scholar]
- Sclan, S.G.; Reisberg, B. Functional assessment staging (FAST) in Alzheimer’s disease: Reliability, validity, and ordinality. Int. Psychogeriatr. 1992, 4 (Suppl. 1), 55–69. [Google Scholar] [CrossRef]
- Bates, D.; Machler, M.; Bolker, B.M.; Walker, S.C. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate—A Practical and Powerful Approach to Multiple Testing. J. R. Soc. Ser. B Stat. Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Gehrman, P.; Marler, M.; Martin, J.L.; Shochat, T.; Corey-Bloom, J.; Ancoli-Israel, S. The timing of activity rhythms in patients with dementia is related to survival. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 1050–1055. [Google Scholar] [CrossRef] [Green Version]
- Van Someren, E.J.; Riemersma-Van Der Lek, R.F. Live to the rhythm, slave to the rhythm. Sleep Med. Rev. 2007, 11, 465–484. [Google Scholar] [CrossRef] [PubMed]
- Duffy, J.F.; Czeisler, C.A. Effect of Light on Human Circadian Physiology. Sleep Med. Clin. 2009, 4, 165–177. [Google Scholar] [CrossRef] [Green Version]
- Skjerve, A.; Holsten, F.; Aarsland, D.; Bjorvatn, B.; Nygaard, H.A.; Johansen, I.M. Improvement in behavioral symptoms and advance of activity acrophase after short-term bright light treatment in severe dementia. Psychiatry Clin. Neurosci. 2004, 58, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Dowling, G.A.; Mastick, J.; Hubbard, E.M.; Luxenberg, J.S.; Burr, R.L. Effect of timed bright light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s disease. Int. J. Geriatr. Psychiatry 2005, 20, 738–743. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, C.A.; Kronauer, R.E.; Allan, J.S.; Duffy, J.F.; Jewett, M.E.; Brown, E.N.; Ronda, J.M. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science 1989, 244, 1328–1333. [Google Scholar] [CrossRef]
- Volicer, L.; Harper, D.G.; Manning, B.C.; Goldstein, R.; Satlin, A. Sundowning and circadian rhythms in Alzheimer’s disease. Am. J. Psychiatry 2001, 158, 704–711. [Google Scholar] [CrossRef]
- Duffy, J.F.; Dijk, D.J.; Klerman, E.B.; Czeisler, C.A. Later endogenous circadian temperature nadir relative to an earlier wake time in older people. Am. J. Physiol. 1998, 275, R1478–R1487. [Google Scholar] [CrossRef]
- Duffy, J.F.; Zeitzer, J.M.; Rimmer, D.W.; Klerman, E.B.; Dijk, D.J.; Czeisler, C.A. Peak of circadian melatonin rhythm occurs later within the sleep of older subjects. Am. J. Physiol. Endocrinol. Metab. 2002, 282, E297–E303. [Google Scholar] [CrossRef] [Green Version]
- Yoon, I.Y.; Kripke, D.F.; Elliott, J.A.; Youngstedt, S.D.; Rex, K.M.; Hauger, R.L. Age-related changes of circadian rhythms and sleep-wake cycles. J. Am. Geriatr. Soc. 2003, 51, 1085–1091. [Google Scholar] [CrossRef]
- Paudel, M.L.; Taylor, B.C.; Ancoli-Israel, S.; Blackwell, T.; Stone, K.L.; Tranah, G.; Redline, S.; Cummings, S.R.; Ensrud, K.E.; Osteoporotic Fractures in Men, S. Rest/activity rhythms and mortality rates in older men: MrOS Sleep Study. Chronobiol. Int. 2010, 27, 363–377. [Google Scholar] [CrossRef] [Green Version]
- Tranah, G.J.; Blackwell, T.; Ancoli-Israel, S.; Paudel, M.L.; Ensrud, K.E.; Cauley, J.A.; Redline, S.; Hillier, T.A.; Cummings, S.R.; Stone, K.L.; et al. Circadian activity rhythms and mortality: The study of osteoporotic fractures. J. Am. Geriatr. Soc. 2010, 58, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Smagula, S.F.; Boudreau, R.M.; Stone, K.; Reynolds, C.F., 3rd; Bromberger, J.T.; Ancoli-Israel, S.; Dam, T.T.; Barrett-Connor, E.; Cauley, J.A. Latent activity rhythm disturbance sub-groups and longitudinal change in depression symptoms among older men. Chronobiol. Int. 2015, 32, 1427–1437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers-Soeder, T.S.; Blackwell, T.; Yaffe, K.; Ancoli-Israel, S.; Redline, S.; Cauley, J.A.; Ensrud, K.E.; Paudel, M.; Barrett-Connor, E.; LeBlanc, E.; et al. Rest-Activity Rhythms and Cognitive Decline in Older Men: The Osteoporotic Fractures in Men Sleep Study. J. Am. Geriatr. Soc. 2018, 66, 2136–2143. [Google Scholar] [CrossRef]
- Satlin, A.; Volicer, L.; Ross, V.; Herz, L.; Campbell, S. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am. J. Psychiatry 1992, 149, 1028–1032. [Google Scholar] [CrossRef]
- Yamadera, H.; Ito, T.; Suzuki, H.; Asayama, K.; Ito, R.; Endo, S. Effects of bright light on cognitive and sleep-wake (circadian) rhythm disturbances in Alzheimer-type dementia. Psychiatry Clin. Neurosci. 2000, 54, 352–353. [Google Scholar] [CrossRef] [PubMed]
- Hjetland, G.J.; Kolberg, E.; Pallesen, S.; Thun, E.; Nordhus, I.H.; Bjorvatn, B.; Flo-Groeneboom, E. Ambient bright light treatment improved proxy-rated sleep but not sleep measured by actigraphy in nursing home patients with dementia: A placebo-controlled randomised trial. BMC Geriatr. 2021, 21, 312. [Google Scholar] [CrossRef] [PubMed]
- Kolberg, E.; Hjetland, G.J.; Thun, E.; Pallesen, S.; Nordhus, I.H.; Husebo, B.S.; Flo-Groeneboom, E. The effects of bright light treatment on affective symptoms in people with dementia: A 24-week cluster randomized controlled trial. BMC Psychiatry 2021, 21, 377. [Google Scholar] [CrossRef]
- Satlin, A.; Volicer, L.; Stopa, E.G.; Harper, D. Circadian locomotor activity and core-body temperature rhythms in Alzheimer’s disease. Neurobiol. Aging 1995, 16, 765–771. [Google Scholar] [CrossRef]
- Martin, J.L.; Marler, M.R.; Harker, J.O.; Josephson, K.R.; Alessi, C.A. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 67–72. [Google Scholar] [CrossRef]
- McCurry, S.M.; Pike, K.C.; Vitiello, M.V.; Logsdon, R.G.; Larson, E.B.; Teri, L. Increasing walking and bright light exposure to improve sleep in community-dwelling persons with Alzheimer’s disease: Results of a randomized, controlled trial. J. Am. Geriatr. Soc. 2011, 59, 1393–1402. [Google Scholar] [CrossRef]
- Musiek, E.S.; Bhimasani, M.; Zangrilli, M.A.; Morris, J.C.; Holtzman, D.M.; Ju, Y.S. Circadian Rest-Activity Pattern Changes in Aging and Preclinical Alzheimer Disease. JAMA Neurol. 2018, 75, 582–590. [Google Scholar] [CrossRef] [PubMed]



| Participants Were Eligible If They: | Patients Were Not Eligible If They: |
|---|---|
|
|
| Control (N = 31) | Intervention (N = 30) | Total (N = 61) | |
|---|---|---|---|
| Female | 20 (64.5%) | 23 (76.7%) | 43 (70.5%) |
| Age—M (Q1, Q3) | 82.0 (78.5, 87.5) | 86.0 (83.0, 88.8) | 84.0 (79.0, 88.0) |
| FAST | |||
| 4 | 0 (0.0%) | 2 (6.7%) | 2 (3.3%) |
| 5 | 1 (3.3%) | 1 (3.3%) | 2 (3.3%) |
| 6 | 21 (70.0%) | 24 (80.0%) | 45 (75.0%) |
| 7 | 8 (26.7%) | 3 (10.0%) | 11 (18.3%) |
| CCI—M (Q1, Q3) | 1.0 (1.0, 2.0) | 2.0 (1.0, 2.0) | 1.0 (1.0, 2.0) |
| MMSE—M (Q1, Q3) | 4.0 (2.0, 9.0) | 4.0 (1.0, 11.0) | 4.0 (1.0, 10.0) |
| Psychotropic med. *—M (Q1, Q3) | 3.0 (2.0, 3.0) | 3.0 (2.0, 4.0) | 3.0 (2.0, 4.0) |
| No. using hypnotics/sedatives † | 10 (32.3%) | 12 (40.0%) | 22 (36.1%) |
| No. with eye disease | 6 (19.4%) | 4 (13.3%) | 10 (16.4%) |
| Dementia diagnoses | |||
| Alzheimer’s | 17 (55%) | 16 (53%) | 33 (54%) |
| Vascular | 1 (3%) | 2 (7%) | 3 (5%) |
| Lewy body | 1 (3%) | 0 (0%) | 1 (2%) |
| Other | 1 (3%) | 1 (3%) | 2 (3%) |
| Unknown | 9 (29%) | 10 (33%) | 19 (31%) |
| IS | IV | RA | M10 | L5 | |
|---|---|---|---|---|---|
| Amplitude | 0.66 **** | −0.52 **** | 0.6 **** | 0.46 **** | −0.29 * |
| MESOR | 0.11 | −0.21 | −0.19 | 0.67 **** | 0.54 * |
| Alpha | 0.06 * | −0.26 | 0.15 * | −0.02 | −0.11 **** |
| Beta | −0.18 * | 0.26 **** | −0.10 | 0.00 * | 0.02 |
| F-statistic | 0.81 **** | −0.58 **** | 0.82 **** | 0.48 **** | −0.49 **** |
| Acrophase | 0.14 * | −0.23 * | −0.03 | 0.09 **** | 0.09 |
| Nadir | −0.41 **** | 0.32 **** | −0.62 **** | 0.18 | 0.66 **** |
| Week 8 × Intervention B (95 % CI) | Week 16 × Intervention B (95 % CI) | Week 24 × Intervention B (95 % CI) | N | N (id) | R2 (Fixed) | R2 (Total) | ICC | |
|---|---|---|---|---|---|---|---|---|
| Non-Parametric Indicators | ||||||||
| IS | −0.01(−0.12–0.10) | −0.02(−0.15–0.10) | 0.02(−0.10–0.13) | 187 | 64 | 0.04 | 0.57 | 0.55 |
| IV | −0.07(−0.22–0.09) | −0.02(−0.19–0.15) | −0.08(−0.23–0.07) | 187 | 64 | 0.01 | 0.77 | 0.77 |
| RA | −0.07(−0.19–0.05) | −0.05(−0.18–0.08) | −0.04(−0.16–0.09) | 187 | 64 | 0.04 | 0.61 | 0.59 |
| M10 | 11.3(−20.62–43.22) | −9.34(−44.51–25.83) | 11.68(−20.04–43.40) | 187 | 64 | 0.13 | 0.75 | 0.71 |
| L5 | 8.47(−3.70–20.64) | −1.26(−14.65–12.13) | 2.85(−9.25–14.94) | 187 | 64 | 0.03 | 0.67 | 0.66 |
| Extended Cosine Model | ||||||||
| Amplitude (ln) | −0.82(−1.81–0.17) | −0.41(−1.52–0.70) | −0.26(−1.28–0.75) | 166 | 61 | 0.02 | 0.32 | 0.31 |
| MESOR (ln) | −0.01(−0.44–0.43) | −0.21(−0.70–0.28) | −0.19(−0.64–0.25) | 166 | 61 | 0.05 | 0.45 | 0.42 |
| Acrophase * | −0.51(−1.39–0.37) | −1.02(−2.00–−0.05) † | −0.59(−1.49–0.30) | 163 | 61 | 0.10 | 0.63 | 0.59 |
| Nadir * | 0.41(−0.02–0.84) | 0.01(−0.47–0.50) | −0.06(−0.50–0.38) | 166 | 60 | 0.04 | 0.52 | 0.49 |
| Alpha | −0.12(−0.38–0.14) | −0.14(−0.44–0.16) | −0.19(−0.46–0.08) | 166 | 61 | 0.05 | 0.51 | 0.48 |
| Beta (ln) | 0.29(−0.65–1.24) | 0.48(−0.57–1.53) | 0.57(−0.40–1.54) | 165 | 61 | 0.03 | 0.08 | 0.05 |
| F-statistic (ln) | −0.4(−0.82–0.03) | −0.01(−0.49–0.47) | −0.06(−0.50–0.38) | 166 | 61 | 0.05 | 0.78 | 0.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolberg, E.; Pallesen, S.; Hjetland, G.J.; Nordhus, I.H.; Flo-Groeneboom, E. The Effect of Bright Light Treatment on Rest–Activity Rhythms in People with Dementia: A 24-Week Cluster Randomized Controlled Trial. Clocks & Sleep 2021, 3, 449-464. https://doi.org/10.3390/clockssleep3030032
Kolberg E, Pallesen S, Hjetland GJ, Nordhus IH, Flo-Groeneboom E. The Effect of Bright Light Treatment on Rest–Activity Rhythms in People with Dementia: A 24-Week Cluster Randomized Controlled Trial. Clocks & Sleep. 2021; 3(3):449-464. https://doi.org/10.3390/clockssleep3030032
Chicago/Turabian StyleKolberg, Eirin, Ståle Pallesen, Gunnhild Johnsen Hjetland, Inger Hilde Nordhus, and Elisabeth Flo-Groeneboom. 2021. "The Effect of Bright Light Treatment on Rest–Activity Rhythms in People with Dementia: A 24-Week Cluster Randomized Controlled Trial" Clocks & Sleep 3, no. 3: 449-464. https://doi.org/10.3390/clockssleep3030032
APA StyleKolberg, E., Pallesen, S., Hjetland, G. J., Nordhus, I. H., & Flo-Groeneboom, E. (2021). The Effect of Bright Light Treatment on Rest–Activity Rhythms in People with Dementia: A 24-Week Cluster Randomized Controlled Trial. Clocks & Sleep, 3(3), 449-464. https://doi.org/10.3390/clockssleep3030032






