Predictors of Excessive Daytime Sleepiness in Medical Students: A Meta-Regression
Abstract
1. Introduction
2. Materials and Methods
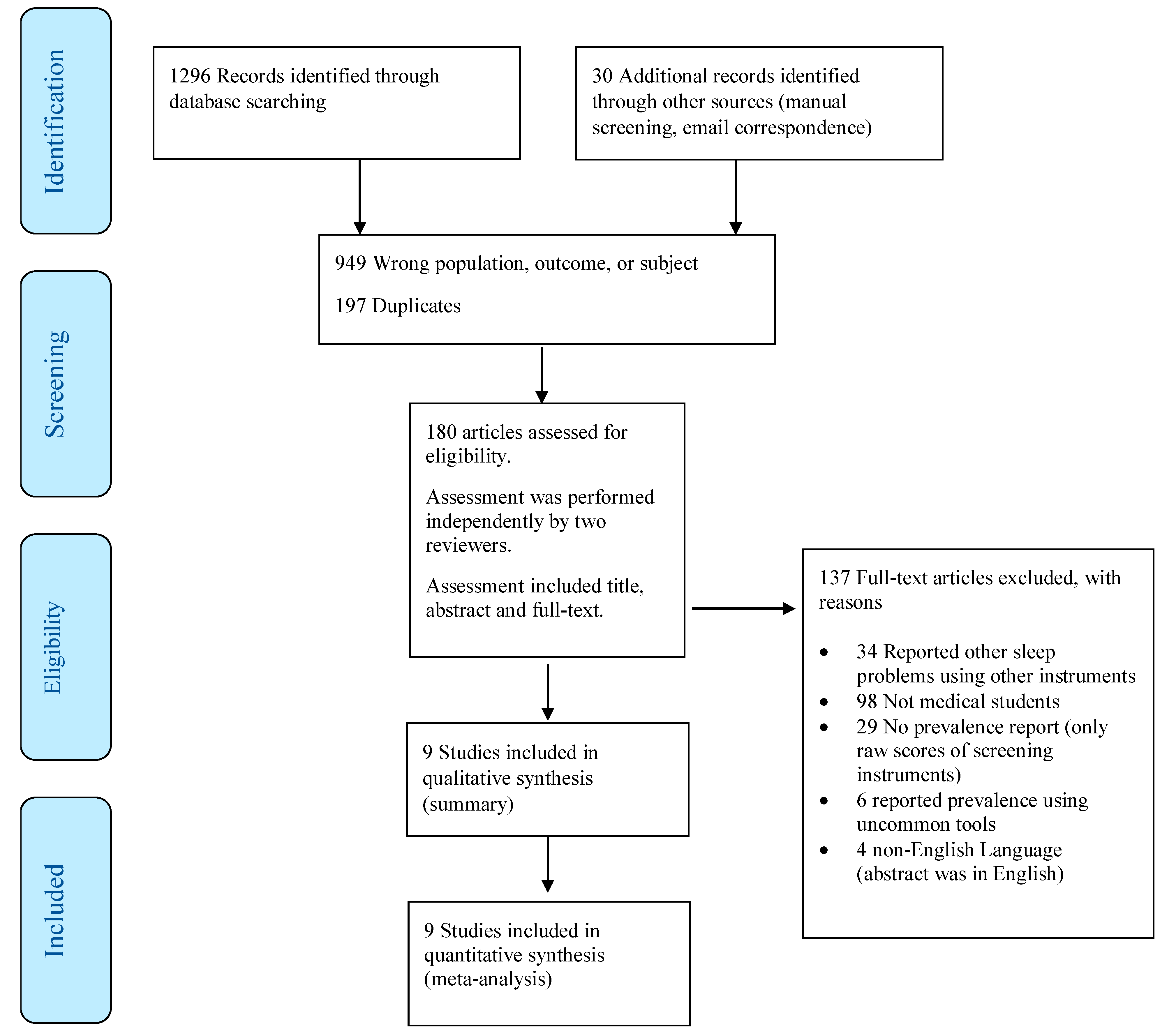
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Outcomes and Specific Measures
2.4. Data Extraction and Coding
2.5. Data Synthesis and Analysis
2.6. Ethical Considerations
3. Results
3.1. Study Characteristics
3.2. Prevalence of EDS in Medical Students
3.3. Predictors of EDS in Medical Students
4. Discussion
5. Conclusion
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PSQI | Pittsburg sleep quality index |
| EDS | Excessive daytime sleepiness |
| ESS | Epworth sleepiness scale |
References
- Slater, G.; Steier, J. Excessive daytime sleepiness in sleep disorders. J. Thorac. Dis. 2012, 4, 608–616. [Google Scholar] [PubMed]
- Ward, K.L.; Hillman, D.R.; James, A.; Bremner, A.P.; Simpson, L.; Cooper, M.N.; Palmer, L.J.; Fedson, A.C.; Mukherjee, S. Excessive Daytime Sleepiness Increases the Risk of Motor Vehicle Crash in Obstructive Sleep Apnea. J. Clin. Sleep Med. 2013, 9, 1013–1021. [Google Scholar] [CrossRef]
- Özer, C.; Etcibaşı, Ş.; Öztürk, L. Daytime sleepiness and sleep habits as risk factors of traffic accidents in a group of Turkish public transport drivers. Int. J. Clin. Exp. Med. 2014, 7, 268–273. [Google Scholar]
- Haavisto, M.-L.; Porkka-Heiskanen, T.; Hublin, C.; Härmä, M.; Mutanen, P.; Müller, K.; Virkkala, J.; Sallinen, M. Sleep restriction for the duration of a work week impairs multitasking performance. J. Sleep Res. 2010, 19, 444–454. [Google Scholar] [CrossRef]
- Azad, M.C.; Fraser, K.; Rumana, N.; Abdullah, A.F.; Shahana, N.; Hanly, P.J.; Turin, T.C. Sleep Disturbances among Medical Students: A Global Perspective. J. Clin. Sleep Med. 2015, 11, 69–74. [Google Scholar] [CrossRef]
- Alhola, P.; Polo-Kantola, P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr Dis. Treat 2007, 3, 553–567. [Google Scholar]
- Al Lawati, N.M.; Patel, S.R.; Ayas, N.T. Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Prog. Cardiovasc. Dis. 2009, 51, 285–293. [Google Scholar] [CrossRef]
- Roth, T.; Roehrs, T.A. Etiologies and sequelae of excessive daytime sleepiness. Clin. Ther. 1996, 18, 562–576; discussion 561. [Google Scholar] [CrossRef]
- Carvalho, D.Z.; St Louis, E.K.; Knopman, D.S.; Boeve, B.F.; Lowe, V.J.; Roberts, R.O.; Mielke, M.M.; Przybelski, S.A.; Machulda, M.M.; Petersen, R.C.; et al. Association of Excessive Daytime Sleepiness With Longitudinal β-Amyloid Accumulation in Elderly Persons Without Dementia. JAMA Neurol. 2018, 75, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Barger, L.K.; Ayas, N.T.; Cade, B.E.; Cronin, J.W.; Rosner, B.; Speizer, F.E.; Czeisler, C.A. Impact of Extended-Duration Shifts on Medical Errors, Adverse Events, and Attentional Failures. PLoS Med. 2006, 3, e487. [Google Scholar] [CrossRef] [PubMed]
- Howard, S.K. Sleep deprivation and physician performance: Why should I care? Proc. (Bayl. Univ. Med. Cent.) 2005, 18, 108–112. [Google Scholar] [CrossRef]
- Weaver, M.D.; Vetter, C.; Rajaratnam, S.M.W.; O’Brien, C.S.; Qadri, S.; Benca, R.M.; Rogers, A.E.; Leary, E.B.; Walsh, J.K.; Czeisler, C.A.; et al. Sleep disorders, depression and anxiety are associated with adverse safety outcomes in healthcare workers: A prospective cohort study. J. Sleep Res. 2018, 27, e12722. [Google Scholar] [CrossRef]
- Mahmood, M.; Kushida, C.A. Chapter 50—Excessive daytime sleepiness. In Handbook of Clinical Neurology; Montagna, P., Chokroverty, S., Eds.; Sleep Disorders Part II; Elsevier: San Francisco, CA, USA, 2011; Volume 99, pp. 825–831. [Google Scholar]
- Guilleminault, C.; Brooks, S.N. Excessive daytime sleepiness: A challenge for the practising neurologist. Brain 2001, 124, 1482–1491. [Google Scholar] [CrossRef]
- Stroe, A.F.; Roth, T.; Jefferson, C.; Hudgel, D.W.; Roehrs, T.; Moss, K.; Drake, C.L. Comparative Levels of Excessive Daytime Sleepiness in Common Medical Disorders. Sleep Med. 2010, 11, 890–896. [Google Scholar] [CrossRef]
- Maugeri, A.; Medina-Inojosa, J.R.; Kunzova, S.; Agodi, A.; Barchitta, M.; Sochor, O.; Lopez-Jimenez, F.; Geda, Y.E.; Vinciguerra, M. Sleep Duration and Excessive Daytime Sleepiness Are Associated with Obesity Independent of Diet and Physical Activity. Nutrients 2018, 10, 1219. [Google Scholar] [CrossRef]
- Mollayeva, T.; Kendzerska, T.; Colantonio, A. Self-report instruments for assessing sleep dysfunction in an adult traumatic brain injury population: A systematic review. Sleep Med. Rev. 2013, 17, 411–423. [Google Scholar] [CrossRef]
- Gradisar, M.; Lack, L.; Richards, H.; Harris, J.; Gallasch, J.; Boundy, M.; Johnston, A. The Flinders Fatigue Scale: Preliminary Psychometric Properties and Clinical Sensitivity of a New Scale for Measuring Daytime Fatigue associated with Insomnia. J. Clin. Sleep Med. 2007, 3, 722–728. [Google Scholar]
- Hayley, A.C.; Williams, L.J.; Kennedy, G.A.; Berk, M.; Brennan, S.L.; Pasco, J.A. Prevalence of excessive daytime sleepiness in a sample of the Australian adult population. Sleep Med. 2014, 15, 348–354. [Google Scholar] [CrossRef]
- Oginska, H.; Pokorski, J. Fatigue and mood correlates of sleep length in three age-social groups: School children, students, and employees. Chronobiol. Int. 2006, 23, 1317–1328. [Google Scholar] [CrossRef]
- Hershner, S.D.; Chervin, R.D. Causes and consequences of sleepiness among college students. Nat. Sci. Sleep 2014, 6, 73–84. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Johns, M.W. Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the epworth sleepiness scale: failure of the MSLT as a gold standard. J. Sleep Res. 2000, 9, 5–11. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2011; ISBN 978-1-119-96437-7. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 15, StataCorp LLC: College Station, TX, USA, 2017.
- OpenMeta[Analyst]—CEBM @ Brown. Available online: http://www.cebm.brown.edu/openmeta/index.html (accessed on 26 January 2018).
- Pagnin, D.; de Queiroz, V.; Carvalho, Y.T.M.S.; Dutra, A.S.S.; Amaral, M.B.; Queiroz, T.T. The relation between burnout and sleep disorders in medical students. Acad. Psychiatry 2014, 38, 438–444. [Google Scholar] [CrossRef]
- Kang, J.-H.; Chen, S.-C. Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health 2009, 9, 248. [Google Scholar] [CrossRef]
- Giri, P.A.; Baviskar, M.P.; Phalke, D.B. Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann. Med. and Health Sci. Res. 2013, 3, 51–54. [Google Scholar] [CrossRef]
- Rique, G.L.N.; Fernandes Filho, G.M.C.; Ferreira, A.D.C.; de Sousa-Muñoz, R.L. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014, 7, 96–102. [Google Scholar] [CrossRef]
- Surani, A.A.; Zahid, S.; Surani, A.; Ali, S.; Mubeen, M.; Khan, R.H. Sleep quality among medical students of Karachi, Pakistan. J. Pak. Med. Assoc. 2015, 65, 380–382. [Google Scholar]
- Alsaggaf, M.A.; Wali, S.O.; Merdad, R.A.; Merdad, L.A. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med. J. 2016, 37, 173–182. [Google Scholar] [CrossRef]
- Saygın, M.; Öztürk, Ö.; Gonca, T.; Has, M.; Hayri, U.B.; Kurt, Y.; Yağlı, M.A.; Çalışkan, S.; Akkaya, A.; Öztürk, M. Investigation of Sleep Quality and Sleep Disorders in Students of Medicine. Turk. Thorac. J. 2016, 17, 132–140. [Google Scholar] [CrossRef]
- Ibrahim, N.; Badawi, F.; Mansouri, Y.; Ainousa, A.; Jambi, S.; Fatani, A.; Andijani, R. Sleep Quality among Medical Students at King Abdulaziz University: A Cross-sectional Study. J. Community Med. Health Educ. 2017, 7, 1–6. [Google Scholar]
- Priya, J.; Singh, J.; Kumari, S. Study of the factors associated with poor sleep among medical students. Indian J. Basic and Appl. Med Res. 2017, 6, 422–429. [Google Scholar]
- Mirghani, H.O. The effect of chronotype (morningness/eveningness) on medical students’ academic achievement in Sudan. J. Taibah Univ. Med Sci. 2017, 12, 512–516. [Google Scholar] [CrossRef]
- Brown, C.A.; Qin, P.; Esmail, S. “Sleep? Maybe Later…” A Cross-Campus Survey of University Students and Sleep Practices. Educ. Sci. 2017, 7, 66. [Google Scholar] [CrossRef]
- Chang, Y.-J.; Peng, C.-Y.; Lan, Y.-C. Consumption of Energy Drinks among Undergraduate Students in Taiwan: Related Factors and Associations with Substance Use. Int. J. Environ. Res. Public Health 2017, 14, 954. [Google Scholar] [CrossRef]
- Touitou, Y.; Reinberg, A.; Touitou, D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017, 173, 94–106. [Google Scholar] [CrossRef]
- Corrêa, C.d.C.; de Oliveira, F.K.; Pizzamiglio, D.S.; Ortolan, E.V.P.; Weber, S.A.T. Sleep quality in medical students: a comparison across the various phases of the medical course. J. Bras. Pneumol. 2017, 43, 285–289. [Google Scholar] [CrossRef]
- Gordon, R.; McDermott, L.; Stead, M.; Angus, K. The effectiveness of social marketing interventions for health improvement: what’s the evidence? Public Health 2006, 120, 1133–1139. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Miller, M.A.; Lockley, S.W.; Rajaratnam, S.M.W. Sleep, Health, and Society: From Aetiology to Public Health; Oxford University Press: Oxford, UK, 2018; ISBN 978-0-19-108410-2. [Google Scholar]
- Barnes, C.M.; Gunia, B.C.; Wagner, D.T. Sleep and moral awareness. J. Sleep Res. 2015, 24, 181–188. [Google Scholar] [CrossRef]
- Zailinawati, A.H.; Teng, C.L.; Chung, Y.C.; Teow, T.L.; Lee, P.N.; Jagmohni, K.S. Daytime sleepiness and sleep quality among Malaysian medical students. Med. J. Malaysia 2009, 64, 108–110. [Google Scholar]
- Rodrigues, R.N.D.; Viegas, C.A.A.; Abreu E Silva, A.A.A.; Tavares, P. Daytime sleepiness and academic performance in medical students. Arq. Neuropsiquiatr. 2002, 60, 6–11. [Google Scholar] [CrossRef][Green Version]
- Doi, Y.; Minowa, M. Gender differences in excessive daytime sleepiness among Japanese workers. Soc. Sci. Med. 2003, 56, 883–894. [Google Scholar] [CrossRef]
- Fatani, A.; Al-Rouqi, K.; Al Towairky, J.; Ahmed, A.E.; Al-Jahdali, S.; Ali, Y.; Al-Shimemeri, A.; Al-Harbi, A.; Baharoon, S.; Khan, M.; et al. Effect of age and gender in the prevalence of excessive daytime sleepiness among a sample of the Saudi population. J. Epidemiol. Glob. Health 2015, 5, S59–S66. [Google Scholar] [CrossRef]
- Data—OECD. Available online: http://www.oecd.org/gender/data/women-make-up-most-of-the-health-sector-workers-but-they-are-under-represented-in-high-skilled-jobs.htm (accessed on 30 November 2018).
- Kabrita, C.S.; Hajjar-Muça, T.A. Sex-specific sleep patterns among university students in Lebanon: Impact on depression and academic performance. Nat. Sci. Sleep 2016, 8, 189–196. [Google Scholar] [CrossRef]
| Study | Country | Design; Sampling; Response Rate | Number of Respondents | Number of Cases with EDS † | Age * (years) | Male % | Sleep Duration (hours/night) * | Sleep Quality Index * |
|---|---|---|---|---|---|---|---|---|
| Kang and Chen et al., 2009 | China | Cross-sectional; Probability; 81.2% | 160 | 23 | 20.3 ± 1.9 | 50.62 | 6.7 ± 1.3 | 4.9 ± NR |
| Giri et al., 2013 | India | Cross-sectional; Convenient; NR | 50 | 10 | 22.4 ± 0.5 | 40.00 | 6.3 ** | 6.5 ± NR |
| Rique et al., 2013 | Brazil | Cross-sectional; Convenient; 86.7% | 221 | 93 | 22.3 ± 3.8 | 55.66 | 6.3 ** | 6.3 ± 2.6 |
| Pagnin et al., 2014 | Brazil | Cross-sectional; Convenient; NR | 127 | 80 | 21.3 ± 2.3 | 44.88 | 6.3 ** | 6.99 ± 3.0 |
| Surani et al., 2015 | Pakistan | Cross-sectional; Convenient; 77.7% | 504 | 52 | 20 ± 1.4 | 40.48 | 6.4 ± 1.5 | 4.9 ± 2.3 |
| Alsaggaf et al., 2016 | Saudi Arabia | Cross-sectional; Convenient; 95% | 305 | 118 | 22 ± 1.3 | 41.64 | 5.5 ± 2.0 | 6.3 ± NR |
| Saygin et al., 2016 | Turkey | Cross-sectional; Probability; 46.8% | 337 | 54 | 21.3 ± 2.1 | 42.09 | 6.6 ± 1.3 | 9.03 ± 4.21 |
| Ibrahim et al., 2017 | Saudi Arabia | Cross-sectional; Probability; NR | 576 | 403 | 21 ± 1.46 | 35.76 | 6.3 ** | 7.23 ± 2.97 |
| Priya et al., 2017 | India | Cross-sectional; Convenient; NR | 307 | 114 | 20.5 ± NR | 76.54 | 6.3 ** | 6.3 ± NR |
| Predictive Factor | β (SE) | 95% CI | p-Value | |
|---|---|---|---|---|
| 1 | Age (Years) | 0.058 (0.080) | −0.100–0.215 | 0.606 |
| Intercept | −0.879 (1.704) | −4.218–2.461 | 0.472 | |
| 2 | Sex (Proportion of male subjects) | 0.056 (0.578) | −1.188–1.076 | 0.923 |
| Intercept | 0.373 (0.283) | −0.181–0.927 | 0.188 | |
| 3 | Sleep duration (Hours per night) | −0.216 (0.201) | −0.610–0.178 | 0.282 |
| Intercept | 1.707 (1.268) | −0.778–4.191 | 0.178 | |
| 4 | Sleep quality index (PSQI † Scale) | 0.059 (0.051) | −0.042–0.160 | 0.254 |
| Intercept | −0.029 (0.335) | −0.685–0.627 | 0.931 | |
| 5 | Sleep duration | −0.224 (0.140) | −0.587–0.140 | 0.227 |
| Sleep quality index | 0.061 (0.048) | −0.330–0.154 | 0.205 | |
| Intercept | 1.371 (1.199) | −0.980–3.721 | 0.253 | |
| 6 | Sleep duration | 4.756 (1.479) | 1.857–7.655 | 0.001 * |
| Sleep quality index | 5.245 (1.535) | 2.237–8.253 | 0.001 * | |
| Sleep duration × Sleep quality index | −0.793 (0.235) | −1.253–−0.333 | 0.001 * | |
| Intercept | −31.182 (9.671) | −50.137–−12.228 | 0.001 * | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jahrami, H.; Alshomili, H.; Almannai, N.; Althani, N.; Aloffi, A.; Algahtani, H.; Brown, C.A. Predictors of Excessive Daytime Sleepiness in Medical Students: A Meta-Regression. Clocks & Sleep 2019, 1, 209-219. https://doi.org/10.3390/clockssleep1020018
Jahrami H, Alshomili H, Almannai N, Althani N, Aloffi A, Algahtani H, Brown CA. Predictors of Excessive Daytime Sleepiness in Medical Students: A Meta-Regression. Clocks & Sleep. 2019; 1(2):209-219. https://doi.org/10.3390/clockssleep1020018
Chicago/Turabian StyleJahrami, Haitham, Hajar Alshomili, Noora Almannai, Noora Althani, Adel Aloffi, Haifa Algahtani, and Cary A. Brown. 2019. "Predictors of Excessive Daytime Sleepiness in Medical Students: A Meta-Regression" Clocks & Sleep 1, no. 2: 209-219. https://doi.org/10.3390/clockssleep1020018
APA StyleJahrami, H., Alshomili, H., Almannai, N., Althani, N., Aloffi, A., Algahtani, H., & Brown, C. A. (2019). Predictors of Excessive Daytime Sleepiness in Medical Students: A Meta-Regression. Clocks & Sleep, 1(2), 209-219. https://doi.org/10.3390/clockssleep1020018






