Abstract
In patients with reccurent lateral and medial patellar instability, isolated medial patellofemoral ligament (MPFL) reconstruction may be insufficient due to poor lateral retinacular tissue quality. In this report, we describe a case of a patient that underwent simultaneous MPFL and lateral patellofemoral ligament (LPFL) reconstruction on the left knee due to chronic bidirectional patellar instability. A 29-year-old female patient presented with first-time lateral patellar dislocation five years ago due to acute strain. She underwent a tibial tuberosity transposition in another hospital. After the surgery, she suffered from recurrent medial and lateral patellar dislocation and presented to our center. MPFL and concomitant LPFL reconstruction on the left knee was simultaneously performed due to bilateral patellar dislocation. The patella was stable postoperatively, and the patient underwent physiotherapy with successful results to date. Single-time patellar dislocation should be treated conservatively. Surgical treatment after the first episode of dislocation can magnitude the risk of postoperative complications. The simultaneous reconstructing of the LPFL yields patellar fixation indistinguishable from the native LPFL. These grafts provide separate tensioning depending on body anatomy, allowing for individualized stability. Anatomical MPFL reconstruction is supported by well-established high-quality research. Reconstructing the LPFL anatomically yields patellar fixation indistinguishable from the native LPFL.
1. Introduction
In sports medicine, patellar instability (PI) is prevalent, especially among younger, more physically active patients. PI is common in those with more than two dislocations. Other important factors contributing to patellar dislocation are the Q angle, the weakness of the medialis obliquus, medial retinaculum lesions, and a high tibial tuberosity trochlear groove (TTTG) distance [1]. Patellar restraint is supported laterally and medially by the lateral patellofemoral ligament (LPFL) and the medial patellofemoral ligament (MPFL), respectively, especially during the first 20 degrees of flexion [2].
In the past, lateral retinacular release (LRR) has been utilized to treat lateral PI byreleasing an overly tight lateral retinaculum, either alone or in combination with an MPFL repair or reconstruction [3]. However, LRRs have been linked to a higher risk of iatrogenic medial instability. They may promote lateral patellar displacement [4]. A lateral reconstruction may be required in this scenario. If a patient with repeated lateral and medial instability does not improve with conservative therapy, then the simultaneous reconstruction of medial and lateral patellar restraints may be essential. These patients may not benefit from intraoperative stability with isolated MPFL reconstruction [5]. In addition, the risk of postoperative re-dislocation may be reduced by assessing any abnormal anatomy related to PI, for example, a tibial tubercle–trochlea groove distance of more than 20 mm or a Caton–Deschamp index of more than 1.4 [6].
In this report, we describe a case of a patient that underwent simultaneous MPFL and LPFL reconstruction on the left knee due to PI.
Presentation of Case: A 29-year-old otherwise healthy female presented to our center in 2018 due to recurrent painful PI in the left knee. Initially, she suffered from PIof the left knee for two years as a result of a single acute strain while playing volleyball. The treated surgeon decided to perform a tibial tuberosity transposition without MPFL reconstruction to achieve better stability. However, since the operation, she has suffered from recurrent painful PI that prevented her from active physical activity due to a fear of dislocation. Upon examination, the left knee showed no signs of inflammation or effusion, with no pain. The range of motion of the left knee was 0–130°. The patella was hypermobile both medially and laterally. The apprehension test for medial and lateral subluxation was positive. The collateral ligaments were firm and Lachmann’s test was negative. The X-ray for patella instability, according to Lyon’s protocol (anteroposterior and lateral view in 30 degrees of flexion with superimposed femoral condyles), was conducted preoperatively and postoperatively (Figure 1). The X-ray in this position showed an adequate height of the patella and the groove of the trochlea. In our facility, we do not perform other X-rays in flexion or extension.

Figure 1.
The X-ray for patella instability according to Lyon’s protocol made preoperatively (above) and postoperatively (below). The X-ray in this position showed an adequate height of the patella (CD index 1.1) and no trohlear dysplasia.
The next preoperative procedure was a computed tomography (CT) scan, which showed patellofemoral instability (posterior bicondylar line angle = 28° on the right and 14° on the left) and the subluxation of the patella (Figure 2). Magnetic resonance imaging (MRI) showed the medialization of the tibial tuberosity on the left knee (Figure 3).
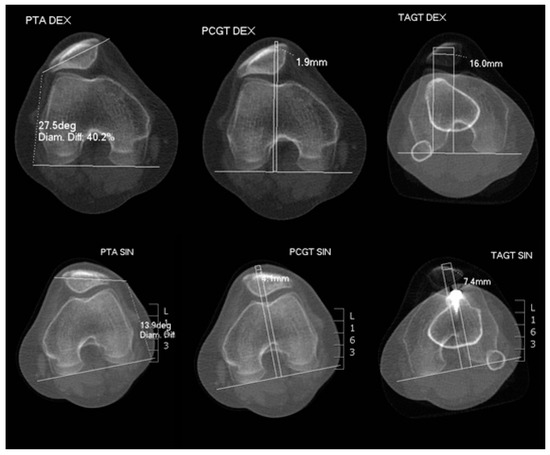
Figure 2.
CT scan after tibial tuberosity transposition without MPFL reconstruction showing patellofemoral instability on the left (posterior bicondylar line angle = 28° on the right and 14° on the left) and the subluxation of the patella. Clinically speaking, the left patella was hypermobile both medially and laterally.
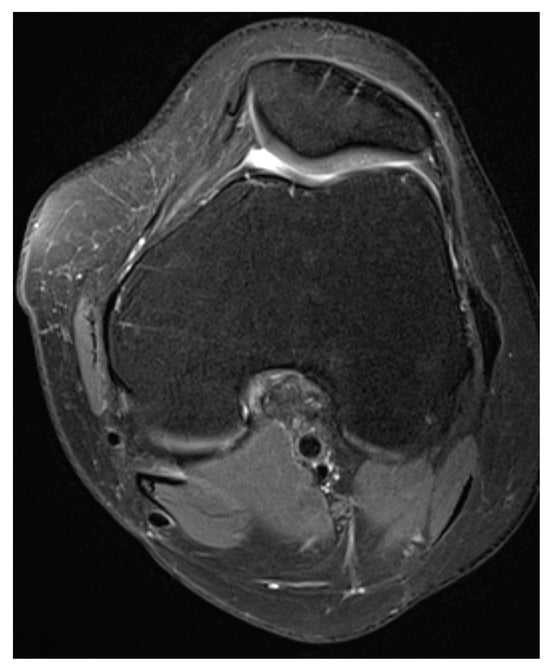
Figure 3.
Preoperative MRI showed the centralization of the left patella with no exact signs of medial or lateral instability. Clinically speaking, the left patella was hypermobile both medially and laterally.
Based on these findings, in November 2021, we decided to perform MPFL reconstruction and concomitant LPFL with the semitendinosus and gracilis tendon on the left knee. The procedure was performed under spinal anesthesia, while the patient was in the supine position using tourniquet bloodles state. Intraoperative arthroscopy showed an unstable patella medially and laterally, with minor cartilage damage in the central part of the patella. A small skin incision was made at the origin of the gracilis tendon and semitendinosus tendon, which were removed using a stripper to prepare two grafts. The tibial screws from the previous tibial tuberositywere removed. Another small incision was made at the medial border of the patella. The MPFL was fixed to the patella using three suture anchors to place the gracilis tendon longitudinally and fix the graft to the proximal half of the patella with sliding sutures and knots. The tendon was also fixed to the femoral epicondyle with an interference 6 × 25 screw to position the tendon isometrically. We never use smaller screws because of their fragility. In this case, the gracilis tendon was used for the MPFL and the semitendinosus tendon was used for LPFL reconstruction. However, there is no inherent designation of one being “weaker” and the other being “stronger” in the context of MPFL and LPFL reconstruction [5]. A longitudinal incision was made over the lateral side of the patella to expose the iliotibial tract next to the lateral epicondyle and the area where the quadriceps tendon was inserted on the patella. Another three incisions were made next to the patella in the distal part of the quadriceps. The semitendinosus tendon was pulled through the incision and fixed to the LPFL, which was sewn back onto the graft. This was followed by the additional suturing of the graft to the patellar ligament, the quadriceps, and the iliotibial tract (Figure 4). We fixed both grafts in 60-degree knee flexions under fluoroscopic control to find the isometric point with the adequate tension on the patella. After the fixation of both grafts, the patella was located in between both trochlear facets.
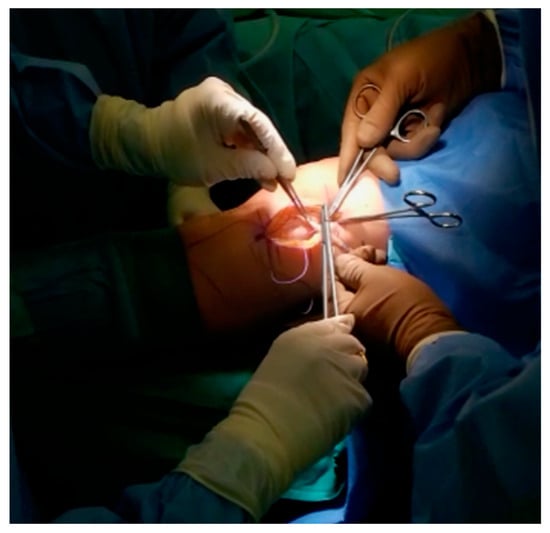
Figure 4.
Sewing the LPFL under adequate tension. The semitendinosus tendon was pulled through the incision and fixed to the LPFL, which was sewn back onto the graft. This was followed by the additional suturing of the graft to the patellar ligament, the quadriceps, and the iliotibial tract.
The operation was uneventful, and the patella was stable postoperatively. The patient was put in an extension brace and was afforded partial weight bearing for 6 weeks. No postoperative complications were recorded. The patella was stable on the follow-up visit, and the patient underwent physiotherapy.
2. Discussion
The simultaneous reconstruction of the MPFL and LPFL aims to establish comprehensive patellar stability, effectively addressing both medial and lateral aspects of patellar instability [5]. The decision to undergo this combined procedure is personalized and contingent upon the unique characteristics and requirements of each patient. Patellar hypermobility can manifest in various symptoms, including pain, recurrent dislocations, and difficulties with activities involving knee bending or extension. Increased mobility may result from ligament laxity, muscle strength imbalances, or other anatomical factors [1].
Typically, gracilis is utilized as an autograft in MPFL reconstruction [5]. Hence, we opted to use gracilis for MPFL reconstruction and semitendinosus for LPFL reconstruction. However, there is no inherent designation of one being “weaker” and the other being “stronger” in the context of MPFL and LPFL reconstruction. The choice between using gracilis or semitendinosus grafts for MPFL or LPFL reconstruction depends on various factors, including the surgeon’s preference, patient characteristics, and specific surgical considerations. Both tendons can provide suitable grafts for ligament reconstruction.
Initial patellar dislocations are often treated conservatively, which involves resolving any swelling, reconditioning the vastus medialis oblique (VMO) muscle, and allowing for the return of a normal range of motion and function [7,8]. Studies have shown that VMO reconditioning can be beneficial in this regard [9]. Patellar taping and stabilization braces can also help reduce subjective feelings of patellar instability [10,11,12,13]. However, in cases where conservative management fails, patients may experience recurrent patellar apprehension, which may be indicative of residual micro-instability with subluxations without frank dislocations. Further diagnostic imaging and a discussion of operative interventions may be required in such cases. If the dislocation does recur, surgery is often necessary [14]. One surgical approach is MPFL reconstruction, which involves replacing the torn ligament with a graft from the patient’s own body or a donor. It is recommended that MPFL reconstruction is performed if patellofemoral instability is present after two or more events of patellar dislocation, while MPFL repair after the first episode of dislocation can increase the risk of postoperative complications [15], which was highlighted in this case.
MPFL reconstruction is the mainstay of proximal soft tissue stabilization procedures and can greatly reduce subjective instability and dislocations [16,17]. The indications for an isolated MPFL reconstruction include a normal tibial tubercle–trochlear groove (TTTG), a normal or Dejour type A trochlea, a Caton–Deschamps index (CDI) of <1.2 indicating no patella alta, and a patellar tilt measurement of <20° [18,19]. MPFL reconstruction is an effective surgical technique that can significantly reduce recurrent dislocations. Studies have shown low re-dislocation rates and excellent functional outcome scores in patients treated using this technique [20,21]. Compared to medial imbrication or MPFL repair, MPFL reconstruction is far superior. However, the procedure can lead to complications, such as patella fractures, with an overall complication rate of 20.3% [22]. To avoid patellar fixation complications, drilling smaller tunnels, avoiding transverse drilling, or using suture anchors or interference screws is recommended. A small percentage of patients may still experience continued patellar instability and subjective feelings of apprehension [23].
The transposition of the tuberosity of the tibia (TTT) is a surgical technique used to correct patellar instability. Indications for TTT include patellar instability with lateral patellar maltracking, patella alta, and patellar chondromalacia with or without extensor mechanism realignment [24]. Recurrent patellar instability, persistent pain, and the subluxation or dislocation of the patella after previous surgery are also indications of TTT [25]. In cases of recurrence or failure after TTT, revision surgery may be necessary. The appropriate management depends on the specific cause of failure or recurrence. If the transfer was not performed correctly, revision surgery might involve repeating the transfer or performing a different procedure. If the initial transfer was successful, but a subsequent injury or trauma caused the recurrence, the underlying cause may need to be addressed before revision surgery is performed. Other potential causes of failure or recurrence, such as incomplete or inadequate rehabilitation, may need to be addressed before considering revision surgery [26]. The type of revision surgery performed will depend on the underlying cause of the failure or recurrence.
In patients with repeated lateral and medial patellar instability, the MPFL procedure may not be sufficient due to poor lateral retinacular tissue quality. The lateral retinaculum is a complex of multiple structures that include the lateral patellofemoral ligament, the iliotibial band, and the lateral patellotibial ligament [27]. It provides lateral stabilization to the patella. In patients with repeated lateral and medial patellar instability, the lateral retinacular tissue quality may be compromised due to previous surgeries or chronic instability, leading to a weakened and stretched lateral patellar retinaculum [5]. In these cases, isolated MPFL reconstruction may not provide adequate lateral stabilization and may result in persistent lateral patellar instability.
To address this issue, a combination of MPFL and LPFL reconstruction may be necessary. Lateral retinacular reconstruction may be performed using autograft or allograft tissue. This combined approach provides a more comprehensive stabilization of the patella and may reduce the risk of recurrent instability [28].
Functional rehabilitation may be greatly enhanced with surgical treatment using MPFL and LPFL reconstruction in individuals with combined medial and lateral PI who have not responded to non-operative therapy. To have a technically successful operation with the best possible results, a comprehensive preoperative workup and assessment under anesthesia are required. Along with the ligamentous reconstruction, it is essential to treat any underlying modifiable risk factors, whether local, regional, or systemic. For MPFL reconstruction, several surgical strategies have been reported in the past, including fixation, tensioning, and graft alternatives, among various other methods [29]. MPFL reconstruction has become a reliable procedure as our understanding of the underlying pathophysiology has improved, but there is still debate surrounding the best surgical approaches. MPFL reconstruction has been consistently deemed a very effective procedure for restoring stability and enhancing knee function under optimal conditions [30]. Few surgical procedures for LPFL reconstruction have been reported, in contrast to those for MPFL reconstruction.
The choice of graft for MPFL reconstruction is not clearly supported by evidence, but hamstring tendons are commonly used. For young patients with wide-open physes, a medial quadriceps turndown in the form of a local autograft may be considered to limit the use of femoral bone tunnels [31]. The proper positioning of the graft on the femur is critical for success, and Schöttle et al.’s point is a useful intraoperative radiographic location. The knee flexion angle for graft fixation should be carefully considered to avoid malpositioned femoral tunnel placement, and over-tensioning the graft should be avoided to prevent potential complications [32]. Beckert et al. used a hamstring allograft with suspensory femoral and sutured patellar fixation in 19 knees [33]. Their findings demonstrated positive results, in terms of osteoarthritis and knee injury outcome scores, with no postoperative anxiety. While these findings are promising, further studies are required to establish best practices and assess long-term benefits. The results of LPFL reconstruction have only been studied in a few retrospective investigations. After two years, patients in a case series published by Moatshe et al. reported an average satisfaction score of 8.2 out of 10 and a reduction in pain and swelling [34]. Similar postoperative improvements in Lysholm scores and psychometrics were reported by Sanchis-Alfonso et al. for 17 knees treated with ITB autograft at 18–48 months [35].
In light of these limitations, it is possible that unconventional surgical approaches might help patients with medial and lateral patellar instability achieve the best possible functional results. The simultaneous reconstruction of both MPFLs and LPFLs has only been accomplished once in the literature. Parvaresh et al. have developed their method based on prior assessments of the MPFL and LPFL; the foundations of their method were developed with anatomical reconstruction in mind [5]. Their patellar attachment locations for the MPFL were comparable to those mentioned by Steensen et al. [36], who discovered that the MPFL covers 38.8% of the patellar length and begins 6 mm distal to the superior pole on average. The radiographic landmarks reported by Schöttle et al. [37] serve as the basis for their femoral insertion, and an isometry is validated prior to fixation, as described by Bollier et al. [38]. The restoration of the LPFL, based on anatomical studies, restored the most robust component of the lateral retinaculum [39].
Given the limited literature on the combined operative reconstruction of MPFLs and LFPLs, we find it crucial to assess the feasibility and effectiveness of such a procedure in our own practice. A notable limitation of our case report is the absence of patient outcome measures, and we acknowledge that potential variations could arise if different graft choices, such as using the semitendinosus tendon for MPFL reconstruction and the gracilis tendon for LPFL reconstruction, were considered. Furthermore, we are aware of the fact that it is difficult to draw any conclusions regarding the success of this operative intervention based on a single case. However, it is worth highlighting the strength of our case in the absence of any complications.
Nevertheless, while we have not yet conducted a formal assessment of post-rehabilitation outcomes in this particular case, it is worth noting that the patient expressed satisfaction during routine check-ups. This report stands to provide valuable insights for others contemplating a similar surgical approach.
3. Conclusions
In conclusion, isolated medial patellofemoral ligament (MPFL) reconstruction may be insufficient in patients with repeated lateral and medial patellar instability due to poor lateral retinacular tissue quality.
We describe a case of a patient that underwent simultaneous MPFL and lateral patellofemoral ligament (LPFL) reconstruction on the left knee due to chronic bilateral patellar instability.
Anatomical MPFL reconstruction is supported by well-established high-quality research. Reconstructing the LPFL anatomically yields patellar fixation indistinguishable from the native LPFL. These grafts provide separate tensioning depending on body anatomy, allowing for individualized stability. We anticipate better patient outcomes as a result of this method; however, additional research is needed to confirm its efficacy.
Author Contributions
Conceptualization, J.M. and M.S.; methodology, J.M. and M.S.; software, J.M. and M.S.; validation, J.M. and M.S.; formal analysis, J.M. and M.S.; investigation, J.M. and M.S.; resources, J.M. and M.S.; data curation, J.M. and M.S.; writing—original draft preparation, J.M. and M.S.; writing—review and editing, J.M. and M.S.; visualization, J.M. and M.S.; supervision, J.M. and M.S.; project administration, J.M. and M.S.; funding acquisition, J.M. and M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or non-profit sectors.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Orthopedic Hospital Valdoltra (protocol code 1/2024 and date of approval 10 January 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data used in this study are not available online. However, interested parties may contact corresponding author for inquiries regarding the data.
Conflicts of Interest
Jakob Merkač is employed by Orthopaedic Hospital Valdoltra. Mateja Sirše is employed by Private Hospital Lassnitzhöhe. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Frosch, S.; Balcarek, P.; Walde, T.; Schüttrumpf, J.; Wachowski, M.; Ferleman, K.-G.; Stürmer, K.; Frosch, K.-H. The treatment of patellar dislocation: A systematic review. Z. Orthop. Unfall. 2011, 149, 630–645. [Google Scholar] [CrossRef]
- Desio, S.M.; Burks, R.T.; Bachus, K.N. Soft Tissue Restraints to Lateral Patellar Translation in the Human Knee. Am. J. Sports Med. 1998, 26, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Casteleyn, P.P.; Handelberg, F. Arthroscopy in the diagnosis of occult dislocation of the patella. Acta Orthop. Belg. 1989, 55, 381–383. [Google Scholar] [PubMed]
- Cancienne, J.M.; Christian, D.R.; Redondo, M.L.; Huddleston, H.P.; Shewman, E.F.; Farr, J.; Cole, B.J.; Yanke, A.B. The Biomechanical Effects of Limited Lateral Retinacular and Capsular Release on Lateral Patellar Translation at Various Flexion Angles in Cadaveric Specimens. Arthrosc. Sports Med. Rehabil. 2019, 1, e137–e144. [Google Scholar] [CrossRef] [PubMed]
- Parvaresh, K.; Huddleston, H.P.; Yanke, A.B. Medial Patellofemoral Ligament Reconstruction with Concomitant Lateral Patellofemoral Reconstruction for Patellar Instability. Arthrosc. Tech. 2021, 10, e2099–e2106. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Staroseletz, Y.; Zenkova, M.A.; Bichenkova, E.V. 85 Developing a new generation of peptidyl-oligonucleotide conjugates with desired biocatalytic properties against biologically relevant RNA. J. Biomol. Struct. Dyn. 2015, 33, 55–56. [Google Scholar] [CrossRef][Green Version]
- Lewallen, L.; McIntosh, A.; Dahm, D. First-Time Patellofemoral Dislocation: Risk Factors for Recurrent Instability. J. Knee Surg. 2015, 28, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Lewallen, L.W.; McIntosh, A.L.; Dahm, D.L. Predictors of Recurrent Instability After Acute Patellofemoral Dislocation in Pediatric and Adolescent Patients. Am. J. Sports Med. 2013, 41, 575–581. [Google Scholar] [CrossRef]
- Palmu, S.; E Kallio, P.; Donell, S.T.; Helenius, I.; Nietosvaara, Y. Acute Patellar Dislocation in Children and Adolescents: A Randomized Clinical Trial. J. Bone Jt. Surg. Am. Vol. 2008, 90, 463–470. [Google Scholar] [CrossRef]
- McConnell, J. Rehabilitation and Nonoperative Treatment of Patellar Instability. Sports Med. Arthrosc. Rev. 2007, 15, 95–104. [Google Scholar] [CrossRef]
- Lee, S.-E.; Cho, S.-H. The effect of McConnell taping on vastus medialis and lateralis activity during squatting in adults with patellofemoral pain syndrome. J. Exerc. Rehabil. 2013, 9, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Colvin, A.C.; West, R.V. Patellar Instability. J. Bone Jt. Surg. Am. Vol. 2008, 90, 2751–2762. [Google Scholar] [CrossRef] [PubMed]
- Khormaee, S.; Kramer, D.E.; Yen, Y.-M.; Heyworth, B.E. Evaluation and Management of Patellar Instability in Pediatric and Adolescent Athletes. Sports Health 2015, 7, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Nietosvaara, Y.; Aalto, K.; Kallio, P.E. Acute Patellar Dislocation in Children: Incidence and Associated Osteochondral Fractures. J. Pediatr. Orthop. 1994, 14, 513–515. [Google Scholar] [CrossRef] [PubMed]
- Dall’Oca, C.; Elena, N.; Lunardelli, E.; Ulgelmo, M.; Magnan, B. MPFL reconstruction: Indications and results. Acta Biomed. 2020, 91, 128–135. [Google Scholar] [CrossRef]
- Astur, D.C.; Gouveia, G.B.; de Souza Borges, J.H.; Astur, N.; Arliani, G.G.; Kaleka, C.C.; Cohen, M. Medial Patellofemoral Ligament Reconstruction: A Longitudinal Study Comparison of 2 Techniques with 2 and 5-Years Follow-Up. Open Orthop. J. 2015, 9, 198–203. [Google Scholar] [CrossRef]
- Latt, L.D.; Fornalski, S.; Raiszadeh, K.; Inacio, M.C.; Fithian, D.C.; Csintalan, R.P. Medial Patellofemoral Ligament (MPFL) Reconstruction for the Treatment of Patellofemoral Instability. J. Knee Surg. 2014, 27, 139–146. [Google Scholar] [CrossRef]
- Biedert, R.M.; Albrecht, S. The patellotrochlear index: A new index for assessing patellar height. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 707–712. [Google Scholar] [CrossRef]
- Hopper, G.P.; Leach, W.J.; Rooney, B.P.; Walker, C.R.; Blyth, M.J. Does Degree of Trochlear Dysplasia and Position of Femoral Tunnel Influence Outcome After Medial Patellofemoral Ligament Reconstruction? Am. J. Sports Med. 2014, 42, 716–722. [Google Scholar] [CrossRef]
- Kita, K.; Tanaka, Y.; Toritsuka, Y.; Amano, H.; Uchida, R.; Takao, R.; Horibe, S. Factors Affecting the Outcomes of Double-Bundle Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocations Evaluated by Multivariate Analysis. Am. J. Sports Med. 2015, 43, 2988–2996. [Google Scholar] [CrossRef]
- Hinterwimmer, S.; Imhoff, A.B.; Minzlaff, P.; Saier, T.; Rosenstiel, N.; Hawe, W.; Feucht, M.J. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: Technical note and preliminary results. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2147–2154. [Google Scholar] [CrossRef] [PubMed]
- Schiphouwer, L.; Rood, A.; Tigchelaar, S.; Koëter, S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 245–250. [Google Scholar] [CrossRef]
- Shah, J.N.; Howard, J.S.; Flanigan, D.C.; Brophy, R.H.; Carey, J.L.; Lattermann, C. A Systematic Review of Complications and Failures Associated with Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocation. Am. J. Sports Med. 2012, 40, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- An, V.V.; Sivakumar, B.S.; Phan, K.; A Fritsch, B.; Sher, D. Isolated versus combined medial patellofemoral ligament reconstruction for lateral instability of the patella. J. Orthop. Surg. 2019, 27, 2309499018820698. [Google Scholar] [CrossRef] [PubMed]
- Servien, E.; Verdonk, P.C.; Neyret, P. Tibial Tuberosity Transfer for Episodic Patellar Dislocation. Sports Med. Arthrosc. 2007, 15, 61–67. [Google Scholar] [CrossRef]
- Laidlaw, M.S.; Diduch, D.R. Current Concepts in the Management of Patellar Instability. Indian J. Orthop. 2017, 51, 493–504. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N.; Eschweiler, J.; Quack, V.; Tingart, M.; Driessen, A. Lateral retinacular release combined with MPFL reconstruction for patellofemoral instability: A systematic review. Arch. Orthop. Trauma Surg. 2021, 141, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, T.; Moatshe, G.; Arendt, E.; Feller, J.; Getgood, A. Combined Medial Patellofemoral Ligament and Medial Patellotibial Ligament Reconstruction for Recurrent Lateral Patellar Dislocation in Flexion. Arthrosc. Tech. 2021, 10, e385–e395. [Google Scholar] [CrossRef]
- Fink, C.; Veselko, M.; Herbort, M.; Hoser, C. MPFL reconstruction using a quadriceps tendon graft. Knee 2014, 21, 1175–1179. [Google Scholar] [CrossRef]
- Schneider, D.K.; Grawe, B.; Magnussen, R.A.; Ceasar, A.; Parikh, S.N.; Wall, E.J.; Colosimo, A.J.; Kaeding, C.C.; Myer, G.D. Outcomes After Isolated Medial Patellofemoral Ligament Reconstruction for the Treatment of Recurrent Lateral Patellar Dislocations. Am. J. Sports Med. 2016, 44, 2993–3005. [Google Scholar] [CrossRef]
- Mountney, J.; Senavongse, W.; Amis, A.A.; Thomas, N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J. Bone Jt. Surg. 2005, 87, 36–40. [Google Scholar] [CrossRef]
- Russo, F.; Doan, J.; Chase, D.C.; Farnsworth, C.L.; Pennock, A.T. Medial Patellofemoral Ligament Reconstruction: Fixation Technique Biomechanics. J. Knee Surg. 2016, 29, 303–309. [Google Scholar] [CrossRef]
- Beckert, M.; Crebs, D.; Nieto, M.; Gao, Y.; Albright, J. Lateral patellofemoral ligament reconstruction to restore functional capacity in patients previously undergoing lateral retinacular release. World J. Clin. Cases 2016, 4, 202–206. [Google Scholar] [CrossRef]
- Moatshe, G.; Cram, T.R.; Chahla, J.; Cinque, M.E.; Godin, J.A.; LaPrade, R.F. Medial Patellar Instability: Treatment and Outcomes. Orthop. J. Sports Med. 2017, 5, 2325967117699816. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Montesinos-Berry, E.; Monllau, J.C.; Merchant, A.C. Results of Isolated Lateral Retinacular Reconstruction for Iatrogenic Medial Patellar Instability. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Steensen, R.N.; Dopirak, R.M.; Mcdonald, W.G. The Anatomy and Isometry of Themedial Patellofemoral Ligament. Am. J. Sports Med. 2004, 32, 1509–1513. [Google Scholar] [CrossRef] [PubMed]
- Schöttle, P.B.; Schmeling, A.; Rosenstiel, N.; Weiler, A. Radiographic Landmarks for Femoral Tunnel Placement in Medial Patellofemoral Ligament Reconstruction. Am. J. Sports Med. 2007, 35, 801–804. [Google Scholar] [CrossRef] [PubMed]
- Bollier, M.; Fulkerson, J.; Cosgarea, A.; Tanaka, M. Technical Failure of Medial Patellofemoral Ligament Reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Merican, A.M.; Sanghavi, S.; Iranpour, F.; Amis, A.A. The structural properties of the lateral retinaculum and capsular complex of the knee. J. Biomech. 2009, 42, 2323–2329. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).