An Evaluation of Psychological Well-Being among Physicians and Nurses in Makkah’s Major Hospitals
Abstract
1. Introduction
2. Materials and Methods
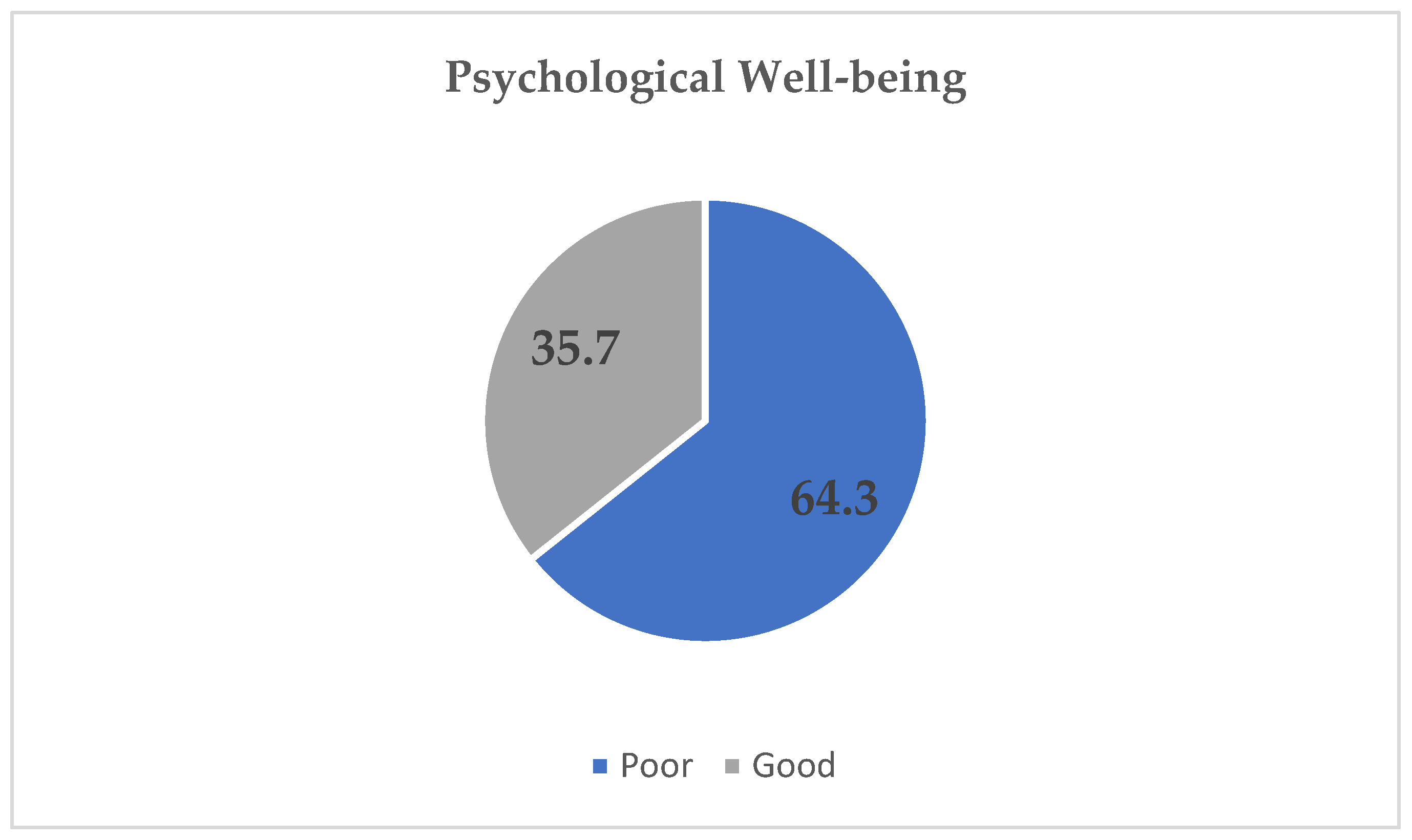
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Strengthening mental health promotion: Mental health is not just the absence of mental disorder. In Strengthening Mental Health Promotion: Mental Health Is Not Just the Absence of Mental Disorder; WHO: Geneva, Switzerland, 1999; p. 2001. [Google Scholar]
- World Health Organization (WHO). The world health report 2001: Mental health: New understanding. In New Hope: World Health Organization; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Schmitz, N.; Kruse, J.; Tress, W. Psychometric properties of the general health questionnaire (GHQ)-12) in a German primary care. Acta. Psychiatr. Scand. 1999, 100, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Employee Assistance Professionals Association (EAPA). EAPA Standards and Professional Guidelines for Employee Assistance Programs. 2010. Available online: https://www.easna.org/wp-content/uploads/2010/08/EASNA-PURCHSERS-GUIDE-TO-EAPs-FINAL-102209.pdf (accessed on 5 May 2021).
- Nunes, A.P.; Richmond, M.K.; Pampel, F.C.; Wood, R.C. The effect of employee assistance services on reductions in employee absenteeism. J. Bus. Psychol. 2017, 33, 699–709. [Google Scholar] [CrossRef]
- Brigham, T.; Barden, C.; Dopp, A.L.; Hengerer, A.; Kaplan, J.; Malone, B.; Nora, L.M. A journey to construct an all-encompassing conceptual model of factors affecting clinician well-being and resilience. NAM Perspect. 2018, 8, 10–31478. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; Alghamdi, A.H.; Aladwani, B.S.; Kazim, S.N.; Almufleh, A.S. Work-related stress and stress-coping strategies in residents and administrative employees working in a tertiary care hospital in KSA. J. Taibah Univ. Medic. Sci. 2016, 11, 32–40. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; Alawad, H.S.; Alamri, A.K.; Saeed, A.I.; Aljuaydi, K.A.; Alotaibi, A.S.; Alfaris, E.A. Stress and coping among consultant physicians working in Saudi Arabia. Ann. Saudi Med. 2018, 38, 214–224. [Google Scholar] [CrossRef]
- Lesener, T.; Gusy, B.; Wolter, C. The job demands-resources model: A meta-analytic review of longitudinal studies. Work Stress 2019, 33, 76–103. [Google Scholar] [CrossRef]
- Seaman, J.B.; Cohen, T.R.; White, D.B. Reducing the stress on clinicians working in the ICU. JAMA 2018, 320, 1981–1982. [Google Scholar] [CrossRef]
- El-Metwally, A.; Javed, S.; Razzak, H.A.; Aldossari, K.K.; Aldiab, A.; Al-Ghamdi, S.H.; Al-Zahrani, J.M. The factor structure of the general health questionnaire (GHQ12) in Saudi Arabia. BMC Health Serv. Res. 2018, 18, 1–11. [Google Scholar] [CrossRef]
- El-Rufaie, O.E.; Daradkeh, T.K. Validation of the Arabic versions of the thirty-and twelve-item general health questionnaires in primary care patients. Br. J. Psychiatry. 1996, 169, 662–664. [Google Scholar] [CrossRef]
- Daradkeh, T.K.; Ghubash, R.; ElRufaie, O.E.F. Reliability, validity, and factor structure of the Arabic version of the 12-item general health questionnaire. Psychol. Rep. 2001, 89, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Emmanuel Olatunde, B.; Odusanya, O. Job satisfaction and psychological well-being among mental health nurses. Int. J. Trans. Comm. Med. 2015, 3, 64–70. [Google Scholar]
- De Sio, S.; La Torre, G.; Buomprisco, G.; Lapteva, E.; Perri, R.; Corbosiero, P.; Cedrone, F. Consequences of COVID19-pandemic lockdown on Italian occupational physicians’ psychosocial health. PLoS ONE 2021, 16, e0243194. [Google Scholar] [CrossRef] [PubMed]
- Pelissier, C.; Fontana, L.; Fort, E.; Vohito, M.; Sellier, B.; Perrier, C.; Charbotel, B. Impaired mental well-being and psychosocial risk: A cross-sectional study in female nursing home direct staff. BMJ Open 2015, 5, e007190. [Google Scholar] [CrossRef]
- Renzi, C.; Di Pietro, C.; Tabolli, S. Psychiatric morbidity and emotional exhaustion among hospital physicians and nurses: Association with perceived job-related factors. Arch. Environ. Occup. Health 2012, 67, 117–123. [Google Scholar] [CrossRef]
- Gao, F.; Luo, N.; Thumboo, J.; Fones, C.; Li, S.C.; Cheung, Y.B. Does the 12-item General Health Questionnaire contain multiple factors and do we need them? Health Qual. Life Outcomes 2004, 2, 1–7. [Google Scholar] [CrossRef][Green Version]
- Tomás, J.M.; Gutiérrez, M.; Sancho, P. Factorial validity of the General Health Questionnaire 12 in an Angolan sample. Eur. J. Psychol. Assess. 2017, 33, 116. [Google Scholar] [CrossRef]
- Liang, Y.; Wang, L.; Yin, X. The factor structure of the 12-item general health questionnaire (GHQ-12) in young Chinese civil servants. Health Qual. Life Outcomes 2016, 14, 1–9. [Google Scholar]
- Alqutub, S.; Mahmoud, M.; Baksh, T. Psychological impact of COVID-19 on frontline healthcare workers in Saudi Arabia. Cureus 2021, 13, e15300. [Google Scholar] [CrossRef]
- Altwaijri, Y.; Bilal, L.; Almeharish, A.; BinMuammar, A.; DeVol, E.; Hyder, S.; Almatrafi, R. Psychological distress reported by healthcare workers in Saudi Arabia during the COVID-19 pandemic: A cross-sectional study. PLoS ONE 2022, 17, e0268976. [Google Scholar] [CrossRef]
- Al Ammari, M.; Sultana, K.; Thomas, A.; Al Swaidan, L.; Al Harthi, N. Mental health outcomes amongst health care workers during COVID 19 pandemic in Saudi Arabia. Front. Psychiatry 2021, 11, 619540. [Google Scholar] [CrossRef] [PubMed]
- Alyami, H.; Krägeloh, C.U.; Medvedev, O.N.; Alghamdi, S.; Alyami, M.; Althagafi, J.; Hill, A.G. Investigating Predictors of Psychological Distress for Healthcare Workers in a Major Saudi COVID-19 Center. Int. J. Environ. Res. Public Health 2022, 19, 4459. [Google Scholar] [CrossRef] [PubMed]
- Rutledge, T.; Stucky, E.; Dollarhide, A.; Shively, M.; Jain, S.; Wolfson, T.; Dresselhaus, T. A real-time assessment of work stress in physicians and nurses. J. Health Psychol. 2009, 28, 194. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Kelly, S.A.; Stephens, J.; Dhakal, K.; McGovern, C.; Tucker, S.; Bird, S.B. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: A systematic review. Am. J. Health Promot. 2020, 34, 929–941. [Google Scholar] [CrossRef] [PubMed]
- Saki, K.; Kaikhavani, S. Mental health of Ilam medical university students. JIUMS 2002, 10, 11–15. [Google Scholar]
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 225 | 49.2 |
| Female | 232 | 50.8 |
| Nationality | ||
| Saudi | 291 | 63.7 |
| Non-Saudi | 166 | 36.3 |
| Profession | ||
| Physician | 187 | 40.9 |
| Nurse | 270 | 59.1 |
| Experience, Mean (SD) | 12.04 (7.73) | |
| ≤15 years | 342 | 74.8 |
| >15 Years | 115 | 25.2 |
| Department | ||
| Surgical wards | 73 | 16.0 |
| Medical wards | 98 | 21.4 |
| Emergency department | 85 | 18.6 |
| Intensive care unit (ICU) | 73 | 16.0 |
| Outpatient department | 39 | 8.5 |
| Allied health services department | 89 | 19.5 |
| Hospital name | ||
| Alnoor | 131 | 28.7 |
| Maternity | 54 | 11.8 |
| King Faisal | 50 | 10.9 |
| Hera Hospital | 61 | 13.3 |
| Ajyad | 17 | 3.7 |
| King Abdul-Aziz | 93 | 20.4 |
| King Abdullah Medical City | 51 | 11.2 |
| Have you attended any psychological support sessions? | ||
| Yes | 33 | 7.2 |
| No | 424 | 92.8 |
| Have you visited any psychological clinics? | ||
| Yes | 56 | 12.3 |
| No | 401 | 87.7 |
| Questionnaire Item | Mean (SD a) | Type of Item | * Response Frequencies (%) | ||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||||
| GHQ-1 | Able to concentrate | 1.14 (0.77) | Positive | 86 (18.8) | 243 (53.2) | 107 (23.4) | 21 (4.6) |
| GHQ-2 | Lost much sleep | 1.49 (1.02) | Negative | 90 (19.7) | 146 (31.9) | 129 (28.2) | 92 (20.1) |
| GHQ-3 | Playing a useful part | 1.11 (0.80) | Positive | 91 (19.9) | 259 (56.7) | 73 (16.0) | 34 (7.4) |
| GHQ-4 | Capable of making decisions | 1.02 (0.73) | Positive | 100 (21.9) | 269 (58.9) | 69 (15.1) | 19 (4.2) |
| GHQ-5 | Under stress | 1.79 (0.98) | Negative | 50 (10.9) | 127 (27.8) | 149 (32.6) | 131 (28.7) |
| GHQ-6 | Could not overcome difficulties | 1.12 (0.80) | Negative | 98 (21.4) | 233 (51.0) | 101 (22.1) | 25 (5.5) |
| GHQ-7 | Enjoy your day-to-day activities | 1.62 (0.88) | Positive | 35 (7.7) | 192 (42.0) | 143 (31.3) | 87 (19.0) |
| GHQ-8 | Face up to problems | 1.60 (0.77) | Positive | 33 (7.2) | 161 (35.2) | 217 (47.5) | 46 (10.1) |
| GHQ-9 | Feeling unhappy and depressed | 1.34 (1.057) | Negative | 121 (26.5) | 140 (30.6) | 114 (24.9) | 82 (17.9) |
| GHQ-10 | Losing confidence | 0.75 (0.91) | Negative | 236 (51.6) | 119 (26.0) | 80 (17.5) | 22 (4.8) |
| GHQ-11 | Thinking of self as worthless | 0.59 (0.88) | Negative | 284 (62.1) | 101 (22.1) | 48 (10.5) | 24 (5.3) |
| GHQ-12 | Feeling reasonably happy | 1.39 (0.84) | Positive | 52 (11.4) | 228 (49.9) | 124 (27.1) | 53 (11.6) |
| Mean GHQ-12 score b | 14.95 (6.40) | Range (2–34) | |||||
| Variables | Mean | (SD) | Test Statistic | |
|---|---|---|---|---|
| t/F | p-Value | |||
| Gender | ||||
| Male | 15.10 | 6.43 | 0.443 a | 0.658 |
| Female | 14.82 | 6.39 | ||
| Nationality | ||||
| Saudi | 15.45 | 6.48 | 2.203 a | 0.028 * |
| Non-Saudi | 14.10 | 6.21 | ||
| Profession | ||||
| Physician | 15.50 | 6.27 | 1.467 a | 0.143 |
| Nurse | 14.59 | 6.49 | ||
| Experience | ||||
| ≤15 years | 15.54 | 6.45 | 3.349 a | 0.001 * |
| >15 Years | 13.24 | 5.99 | ||
| Department | ||||
| Surgical wards | 14.47 | 6.39 | 0.949 b | 0.449 |
| Medical wards | 15.74 | 6.41 | ||
| Emergency department | 17.74 | 7.06 | ||
| Intensive care unit (ICU) | 13.95 | 4.83 | ||
| Outpatient department | 12.82 | 5.96 | ||
| Allied health services department | 14.25 | 6.95 | ||
| Hospital name | 15.88 | 5.81 | ||
| Alnoor | 2.848 b | 0.010 * | ||
| Maternity | 14.97 | 5.64 | ||
| King Faisal | 15.97 | 6.56 | ||
| Hera Hospital | 15.27 | 7.29 | ||
| Ajyad | 14.67 | 6.67 | ||
| King Abdul-Aziz | 14.05 | 5.50 | ||
| King Abdullah Medical City | 14.18 | 6.05 | ||
| Have you attended any psychological support sessions? | ||||
| Yes | 12.82 | 5.74 | 2.082 a | 0.038 * |
| No | 15.13 | 6.43 | ||
| Have you visited any psychological clinics? | ||||
| Yes | 18.82 | 6.28 | −4.949 a | <0.001 * |
| No | 14.42 | 6.24 | ||
| (I) Hospital Name | (J) Hospital Name | Mean Difference (I-J) | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Alnoor | Maternity | −1.29036 | −4.3199 | 1.7392 | 0.869 |
| King Faisal | −3.28962 * | −6.4038 | −0.1754 | 0.031 | |
| Hera hospital | 0.49956 | −2.4043 | 3.4034 | 0.999 | |
| Ajyad | 1.62685 | −3.2026 | 6.4563 | 0.954 | |
| King Abdul-Aziz | 0.20307 | −2.3372 | 2.7433 | 1.000 | |
| King Abdullah Medical City | −1.43197 | −4.5240 | 1.6601 | 0.817 | |
| Maternity | Alnoor | 1.29036 | −1.7392 | 4.3199 | 0.869 |
| King Faisal | −1.99926 | −5.6760 | 1.6775 | 0.676 | |
| Hera hospital | 1.78992 | −1.7105 | 5.2903 | 0.736 | |
| Ajyad | 2.91721 | −2.2928 | 8.1272 | 0.644 | |
| King Abdul-Aziz | 1.49343 | −1.7117 | 4.6986 | 0.812 | |
| King Abdullah Medical City | −0.14161 | −3.7996 | 3.5164 | 1.000 | |
| King Faisal | Alnoor | 3.28962 * | 0.1754 | 6.4038 | 0.031 |
| Maternity | 1.99926 | −1.6775 | 5.6760 | 0.676 | |
| Hera hospital | 3.78918 * | 0.2153 | 7.3631 | 0.030 | |
| Ajyad | 4.91647 | −0.3432 | 10.1761 | 0.084 | |
| King Abdul-Aziz | 3.49269 * | 0.2074 | 6.7780 | 0.029 | |
| King Abdullah Medical City | 1.85765 | −1.8707 | 5.5860 | 0.759 | |
| Hera hospital | Alnoor | −0.49956 | −3.4034 | 2.4043 | 0.999 |
| Maternity | −1.78992 | −5.2903 | 1.7105 | 0.736 | |
| King Faisal | −3.78918 * | −7.3631 | −0.2153 | 0.030 | |
| Ajyad | 1.12729 | −4.0106 | 6.2652 | 0.995 | |
| King Abdul-Aziz | −0.29649 | −3.3831 | 2.7901 | 1.000 | |
| King Abdullah Medical City | −1.93153 | −5.4861 | 1.6230 | 0.676 | |
| Ajyad | Alnoor | −1.62685 | −6.4563 | 3.2026 | 0.954 |
| Maternity | −2.91721 | −8.1272 | 2.2928 | 0.644 | |
| King Faisal | −4.91647 | −10.1761 | 0.3432 | 0.084 | |
| Hera hospital | −1.12729 | −6.2652 | 4.0106 | 0.995 | |
| King Abdul-Aziz | −1.42378 | −6.3653 | 3.5177 | 0.979 | |
| King Abdullah Medical City | −3.05882 | −8.3054 | 2.1877 | 0.598 | |
| King Abdul-Aziz | Alnoor | −0.20307 | −2.7433 | 2.3372 | 1.000 |
| Maternity | −1.49343 | −4.6986 | 1.7117 | 0.812 | |
| King Faisal | −3.49269 * | −6.7780 | −0.2074 | 0.029 | |
| Hera hospital | 0.29649 | −2.7901 | 3.3831 | 1.000 | |
| Ajyad | 1.42378 | −3.5177 | 6.3653 | 0.979 | |
| King Abdullah Medical City | −1.63504 | −4.8993 | 1.6292 | 0.755 | |
| King Abdullah Medical City | Alnoor | 1.43197 | −1.6601 | 4.5240 | 0.817 |
| Maternity | 0.14161 | −3.5164 | 3.7996 | 1.000 | |
| King Faisal | −1.85765 | −5.5860 | 1.8707 | 0.759 | |
| Hera hospital | 1.93153 | −1.6230 | 5.4861 | 0.676 | |
| Ajyad | 3.05882 | −2.1877 | 8.3054 | 0.598 | |
| King Abdul-Aziz | 1.63504 | −1.6292 | 4.8993 | 0.755 | |
| Variables | Social Dysfunction Factor | Anxiety/Depression Factor | Loss of Confidence Factor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| t/F | DF | p Value | t/F | DF | p Value | t/F | DF | p Value | |
| Gender | 2.284 | 455 | 0.023 * | −0.800 | 455 | 0.424 | −0.524 | 455 | 0.600 |
| Profession | 1.900 | 455 | 0.058 | 1.829 | 455 | 0.068 | −0.760 | 455 | 0.448 |
| Nationality | 3.165 | 455 | 0.002 * | 1.266 | 455 | 0.206 | 1.058 | 455 | 0.291 |
| Experience | 2.427 | 455 | 0.016 * | 3.265 | 455 | 0.001 * | 2.985 | 455 | 0.003 * |
| Department | 1.990 | 5 | 0.079 | 2.667 | 5 | 0.022 * | 1.114 | 5 | 0.352 |
| Hospital | 2.037 | 6 | 0.059 | 2.662 | 6 | 0.015 * | 3.133 | 6 | 0.005 * |
| Have you attended any psychological support sessions? | 2.960 | 455 | 0.003 * | 1.875 | 455 | 0.061 | −0.181 | 455 | 0.856 |
| Have you visited any psychological clinics? | −3.156 | 455 | 0.002 * | −4.808 | 455 | <0.001 * | −5.106 | 455 | <0.001 * |
| Variables | 2.284 | 455 | 0.023 * | −0.800 | 455 | 0.424 | −0.524 | 455 | 0.600 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alghamdi, H.; Almalki, A.; Alshaikh, M. An Evaluation of Psychological Well-Being among Physicians and Nurses in Makkah’s Major Hospitals. J 2022, 5, 369-379. https://doi.org/10.3390/j5030025
Alghamdi H, Almalki A, Alshaikh M. An Evaluation of Psychological Well-Being among Physicians and Nurses in Makkah’s Major Hospitals. J. 2022; 5(3):369-379. https://doi.org/10.3390/j5030025
Chicago/Turabian StyleAlghamdi, Huda, Abdullah Almalki, and Maha Alshaikh. 2022. "An Evaluation of Psychological Well-Being among Physicians and Nurses in Makkah’s Major Hospitals" J 5, no. 3: 369-379. https://doi.org/10.3390/j5030025
APA StyleAlghamdi, H., Almalki, A., & Alshaikh, M. (2022). An Evaluation of Psychological Well-Being among Physicians and Nurses in Makkah’s Major Hospitals. J, 5(3), 369-379. https://doi.org/10.3390/j5030025






