Adult Small Intestinal Intussusception Due to Bleeding Lipoma: A Rare Case Report (with Video)
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alhammadi, F.; Prakash, A.; Alhashimi, F.M.; Jaffar, M.; Ikram, F.; AlBastaki, S. From an incidental lipoma to ileo-ileal intussusception in an adult: A case report. Int. J. Surg. Case Rep. 2024, 123, 110164. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mar, A.; Yiallourou, A.; Samanides, L.; Dafnios, N.; Anastasopoulos, G.; Vassiliou, I.; Theodosopoulos, T. Intussusception of the bowel in adults: A review. World J. Gastroenterol. 2009, 15, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Honjo, H.; Mike, M.; Kusanagi, H.; Kano, N. Adult intussusception: A retrospective review. World J. Surg. 2015, 239, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Martin-Lorenzo, J.G.; Torralba-Martinez, A.; Liron-Ruiz, R.; Flores-Pastor, B.; Miguel-Perello, J.; Aguilar-Jimenez, J.; Aguayo-Albasini, J.L. Intestinal invagination in adults: Preoperative diagnosis and management. Int. J. Color. Dis. 2004, 19, 68–72. [Google Scholar] [CrossRef]
- Hong, K.D.; Kim, J.; Ji, W.; Wexner, S.D. Adult intussusception: A systematic review and meta-analysis. Tech. Coloproctol. 2019, 23, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, M.; Gojwari, T.A.; Shah, O.A.; Nazir, N. “Sausage” sign intussusception. Abdom. Radiol. 2019, 44, 2947–2948. [Google Scholar] [CrossRef]
- Begos, D.G.; Sandor, A.; Modlin, I.M. The diagnosis and management of adult intussusception. Am. J. Surg. 1997, 173, 88–94. [Google Scholar] [CrossRef]
- 8. Sohrabi, C.G.; Mathew, G.; Maria, N.; Kerwan, A.; Franchi, T.; Agha, R.A. The SCARE 2023 guideline: Updating consensus. Surgical CAse Report (SCARE) guidelines. Int. J. Surg. 2023, 109, 1136. [Google Scholar] [CrossRef]
- Panzera, F.; Di Venere, B.; Rizzi, M.; Biscaglia, A.; Prat, C.A.; Nasti, G.; Mardighian, A.; Nunes, T.F.; Inchingolo, R. Bowel intussusception in adult: Prevalence, diagnostic tools and therapy. World J. Methodol. 2021, 11, 81–87. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Álvarez-Baut, F.E.; Moctezuma-Velázquez, P.; Pimienta-Ibarra, A.S.; Vergara-Fernández, O.; Salgado-Nesme, N. Adult intussusception: Still a challenging diagnosis for the surgeon. Rev. Gastroenterol. Mex. 2023, 88, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Chand, J.T.; Rakesh, R.; Ganesh, M.S. Adult intussusception: A systematic review of current literature. Langenbecks Arch. Surg. 2024, 409, 235. [Google Scholar] [CrossRef] [PubMed]
- Mouaqit, O.; Hasnai, H.; Chbani, L.; Benjelloun, B.; Bouhaddouti, H.; Majdoub, K.I.; Toughrai, I.; Laalim, S.A.; Oussaden, A.; Maazaz, K.; et al. Adult intussusceptions caused by a lipoma in the jejunum: Report of a case and review of the literature. World J. Emerg. Surg. 2012, 7, 28. [Google Scholar] [CrossRef] [PubMed]
- Jiang, R.D.; Zhi, X.T.; Zhang, B.; Chen, Z.Q.; Li, T. Submucosal Lipoma: A rare cause of recurrent intestinal obstruction and intestinal intussusception. J. Gastrointest. Surg. 2015, 19, 1733–1735. [Google Scholar] [CrossRef] [PubMed]
- Konik, R.D.; Rhodes, R.A. Complete small bowel obstruction without intussusception due to a submucosal lipoma. J. Surg. Case Rep. 2018, 2018, rjy155. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, S. Adult Intussusception: A case series and review. World J. Gastroentest. Endosc. 2017, 9, 220–227. [Google Scholar] [CrossRef]
- Luke, N.; She, T.; Roy, D.; Sonoda, T.; Katz, S. Jejunal lipoma-induced intussusception mimicking Crohn’s disease: A case report. Case Rep. Gastroenterol. 2025, 19, 282–288. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Basukala, S.; Karki, S.; Maharjan, S.; Banmala, S.; Shrestha, M.; Jayswal, M.; Shrestha, K. Small bowel intussusception in an adult secondary to gastrointestinal stromal tumor: A rare case report. Ann. Med. Surg. 2023, 85, 1952–1955. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Siow, S.L.; Goo, Z.Q.; Mahendran, H.A.; Wong, C.M. Laparoscopic versus open management of. adult intussusception. Surg. Endosc. 2020, 34, 4429–4435. [Google Scholar] [CrossRef] [PubMed]
- Charles, T.; Penninga, L.; Reurings, J.C.; Berry, M.C. Intussusception in children: A clinical review. Acta Chir. Belg. 2015, 115, 327–333. [Google Scholar] [CrossRef]
- Al Zaabi, A.H.Y.; Al Janahi, J.A.; Alremeithi, S.N.; Qayyum, H. Jejunojejunal intussusception in an adult: A rare presententation of abdominal. pain in the emergency. department. BMJ Case Rep. 2021, 14, e243787. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grbavac, M.; Bakula, B.; Romic, I.; Bogut, A.; Bakula, M. Jejunal lipoma causing intussusception in an adult. J. Coll. Physicians Surg. Pak. 2022, 32, 108–110. [Google Scholar] [PubMed]
- Karampa, A.; Stefanou, C.K.; Stefanou, S.K.; Tepelenis, K.; Tsoumanis, P.; Ntalapa, K.M.; Giannouli, P.; Pappas-Gogos, G.; Vlachos, K. Jejunal intussusception due to an atypical lipomatous tumor: A rare case report. J. Surg. Case Rep. 2022, 8, rjab624. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Waack, A.; Nandwani, S.; Kolisetty, K.; Vattipally, V. Lipoma lead point intussusception in an adult: A case report. Radiol. Case Rep. 2022, 17, 4907–4910. [Google Scholar] [CrossRef] [PubMed]
- Winfield, F.J.; Nasim, S. Adult ileocaecal intussusception caused by lipoma managed in a remote western Australian hospital. BMJ Case Rep. 2024, 17, e259963. [Google Scholar] [CrossRef] [PubMed]
- Eisen, L.K.; Cunningham, J.D.; Aufses, A.H., Jr. Intussusception in adults: Institutional review. J. Am. Coll. Surg. 1999, 188, 390–395. [Google Scholar] [CrossRef]
- Santacruz, C.C.; García Septiem, J. Adult intestinal intussusception: Practical issues and concerns. Dis. Colon. Rectum. 2021, 64, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Tarchouli, M.; Ait Ali, A. Adult intussusception: An uncommon condition and challenging management. Visc. Med. 2021, 37, 120–127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lianos, G.; Xeropotam, N.; Bali, C.; Baltoggiannis, G.; Ignatiadou, E. Adult bowel intussusception: Presentation, location, etiology diagnosis and treatment. G. Chir. 2013, 34, 280–283. [Google Scholar]


| Date/Day | Clinical Event | Details |
|---|---|---|
| Day 0—Emergency department—H15:00 | Presentation admission | 55-year-old female. Symptoms: melena, diffuse abdominal pain, weakness, and palpitations. Medical history: Shone’s syndrome, atrial fibrillation, chronic heart failure and hypothyroidism. |
| Day 0—H15:14 | Laboratory tests | Severe anemia (Hb 6.8 g/dL), INR 3.66, lactate 2.6 mmol/L. Blood transfusions administered. |
| Day 0—H18:00 | Upper endoscopy | No evidence of active or recent bleeding. |
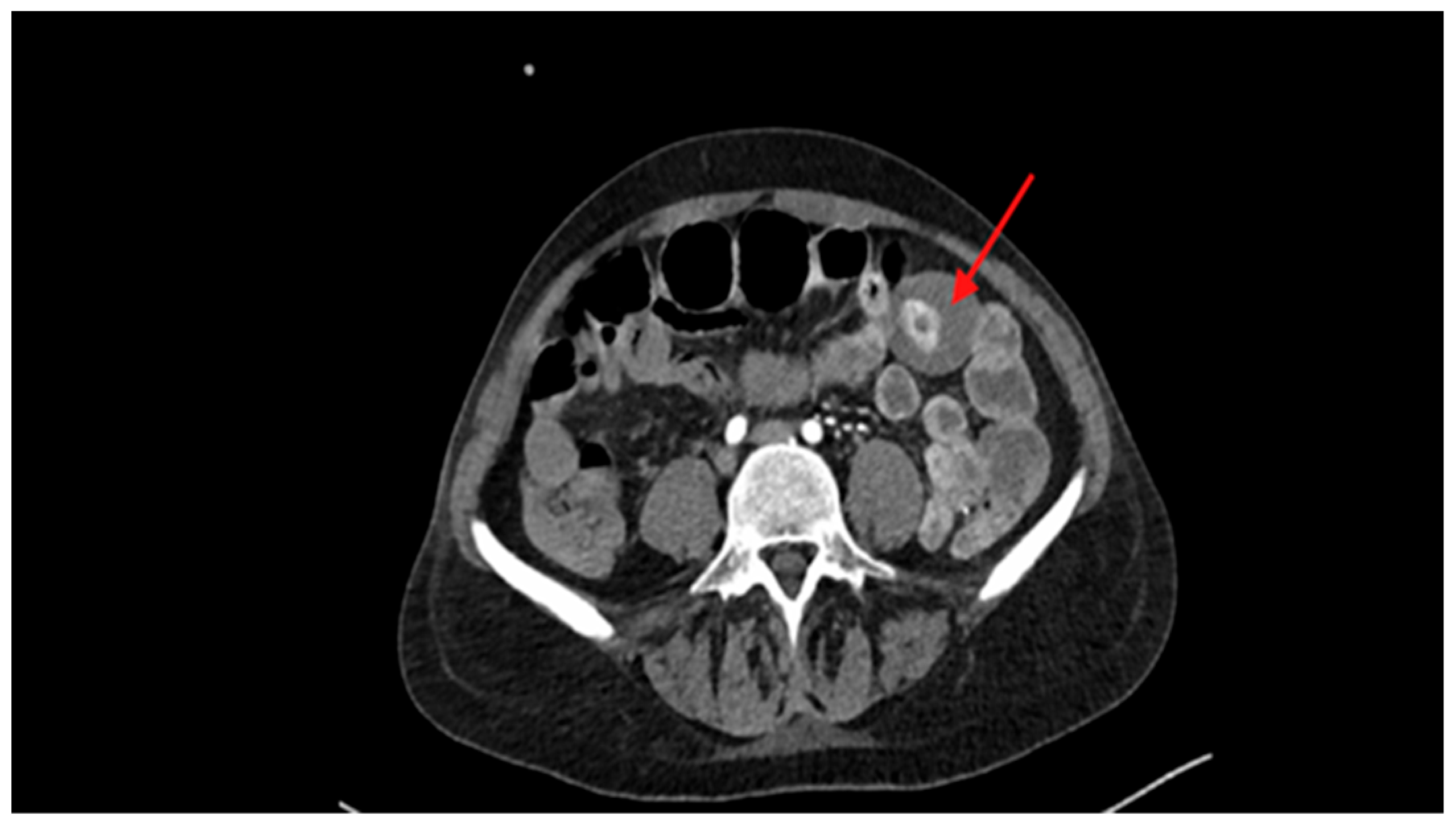
| Day 0—H20:45 | CT scan | Hyperdense intraluminal lesion in the small intestine, suspicious of bleeding lipoma. |
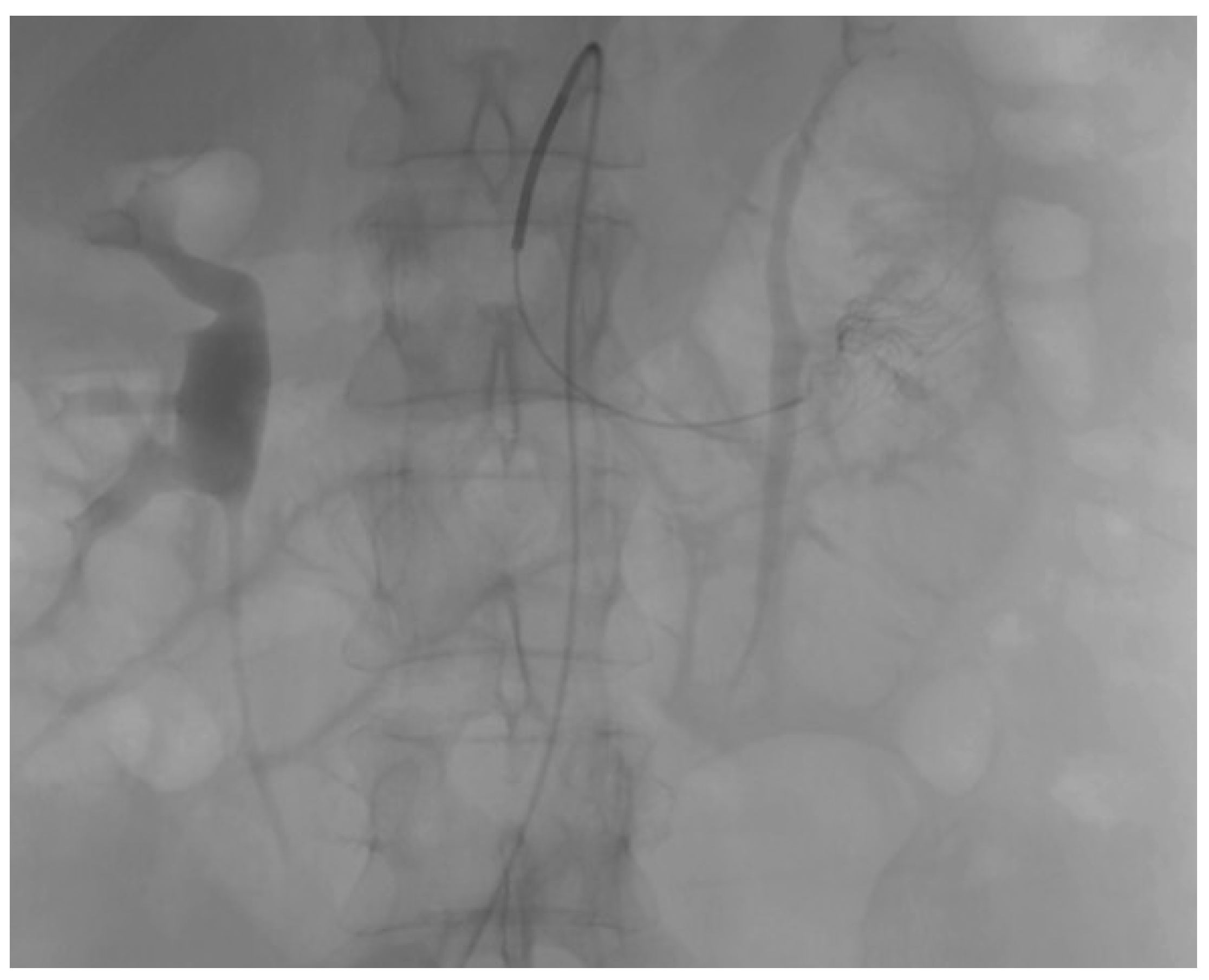
| Day 0—H23:30 | Angiography | Active contrast extravasation from ileocolic branches → selective embolization performed. |
| Day +1—H00:00 | Clinical evolution | Persistent anemia and onset of acute obstructive abdominal condition. |
| Day +1—H4:00 | Urgent surgery | Midline laparotomy revealed ischemic tract and intussusception ~50 cm from Treitz. En-bloc Resection of ~50 cm segment with lateral–lateral jejunal-jejunal anastomosis. |
| POD 1 | Early complications | Recurrence of atrial fibrillation and anemia, managed with medication and transfusions. |
| POD 3–4 | Recovery of nutrition | Transition from parenteral nutrition to liquids and then soft diet. |
| POD 6 | Discharge | Clinical and laboratory improvement with stable hemoglobin levels. |
| 2-week follow-up | Outpatient evaluation | Patient asymptomatic, hemoglobin stable and complete symptom resolution. |
| Histology | Final diagnosis | Submucosal intestinal lipoma. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valeriani, M.; De Martino, C.; Capuano, M.; Fernicola, A.; Cerfolio, F.; Aprea, G.; Palomba, G. Adult Small Intestinal Intussusception Due to Bleeding Lipoma: A Rare Case Report (with Video). Reports 2025, 8, 221. https://doi.org/10.3390/reports8040221
Valeriani M, De Martino C, Capuano M, Fernicola A, Cerfolio F, Aprea G, Palomba G. Adult Small Intestinal Intussusception Due to Bleeding Lipoma: A Rare Case Report (with Video). Reports. 2025; 8(4):221. https://doi.org/10.3390/reports8040221
Chicago/Turabian StyleValeriani, Mariafelicia, Ciro De Martino, Marianna Capuano, Agostino Fernicola, Francesco Cerfolio, Giovanni Aprea, and Giuseppe Palomba. 2025. "Adult Small Intestinal Intussusception Due to Bleeding Lipoma: A Rare Case Report (with Video)" Reports 8, no. 4: 221. https://doi.org/10.3390/reports8040221
APA StyleValeriani, M., De Martino, C., Capuano, M., Fernicola, A., Cerfolio, F., Aprea, G., & Palomba, G. (2025). Adult Small Intestinal Intussusception Due to Bleeding Lipoma: A Rare Case Report (with Video). Reports, 8(4), 221. https://doi.org/10.3390/reports8040221







