Surgical Management of an Impacted Mandibular Second Premolar in Close Proximity to the Mental Foramen: A Case Report
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
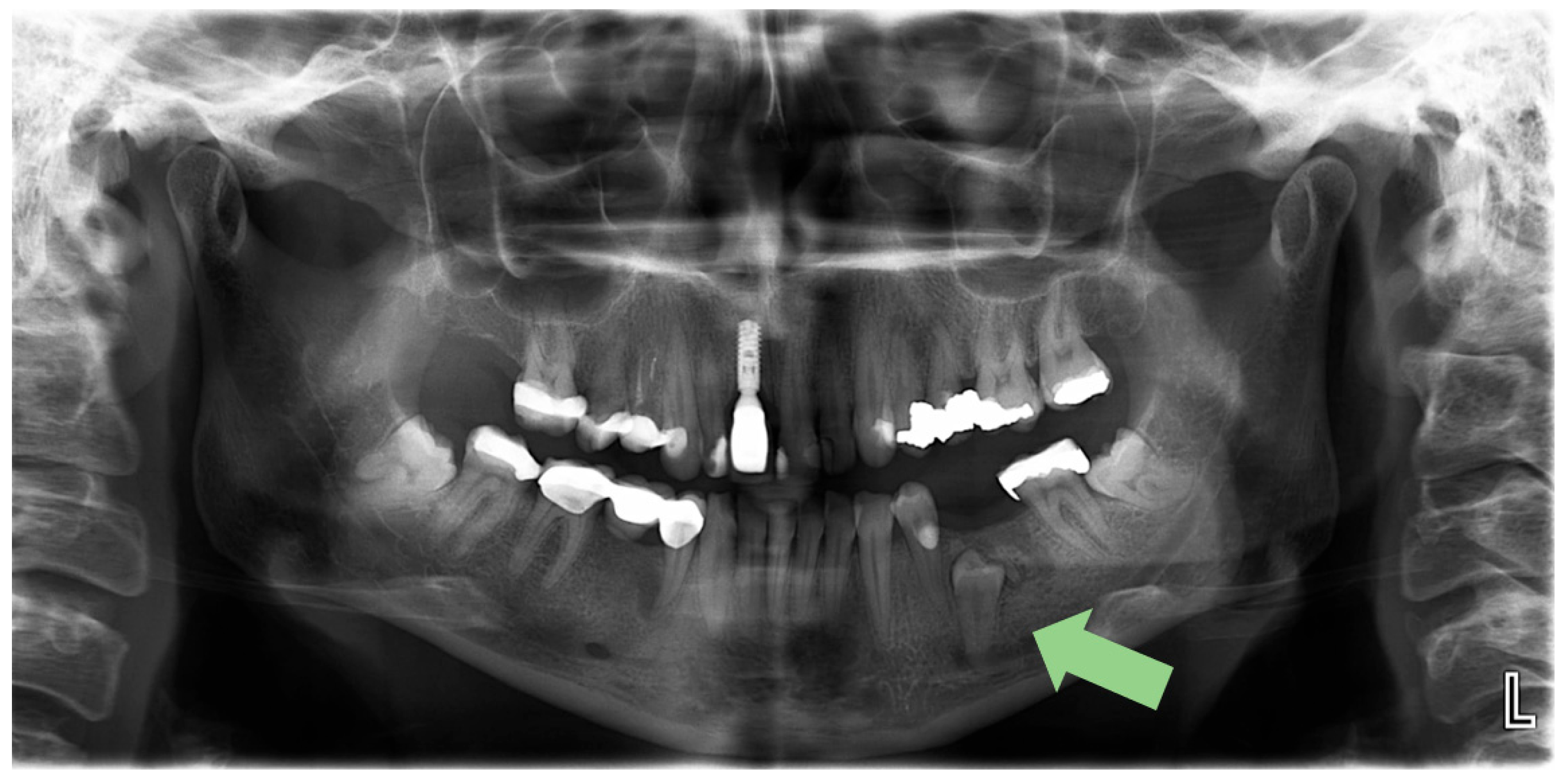
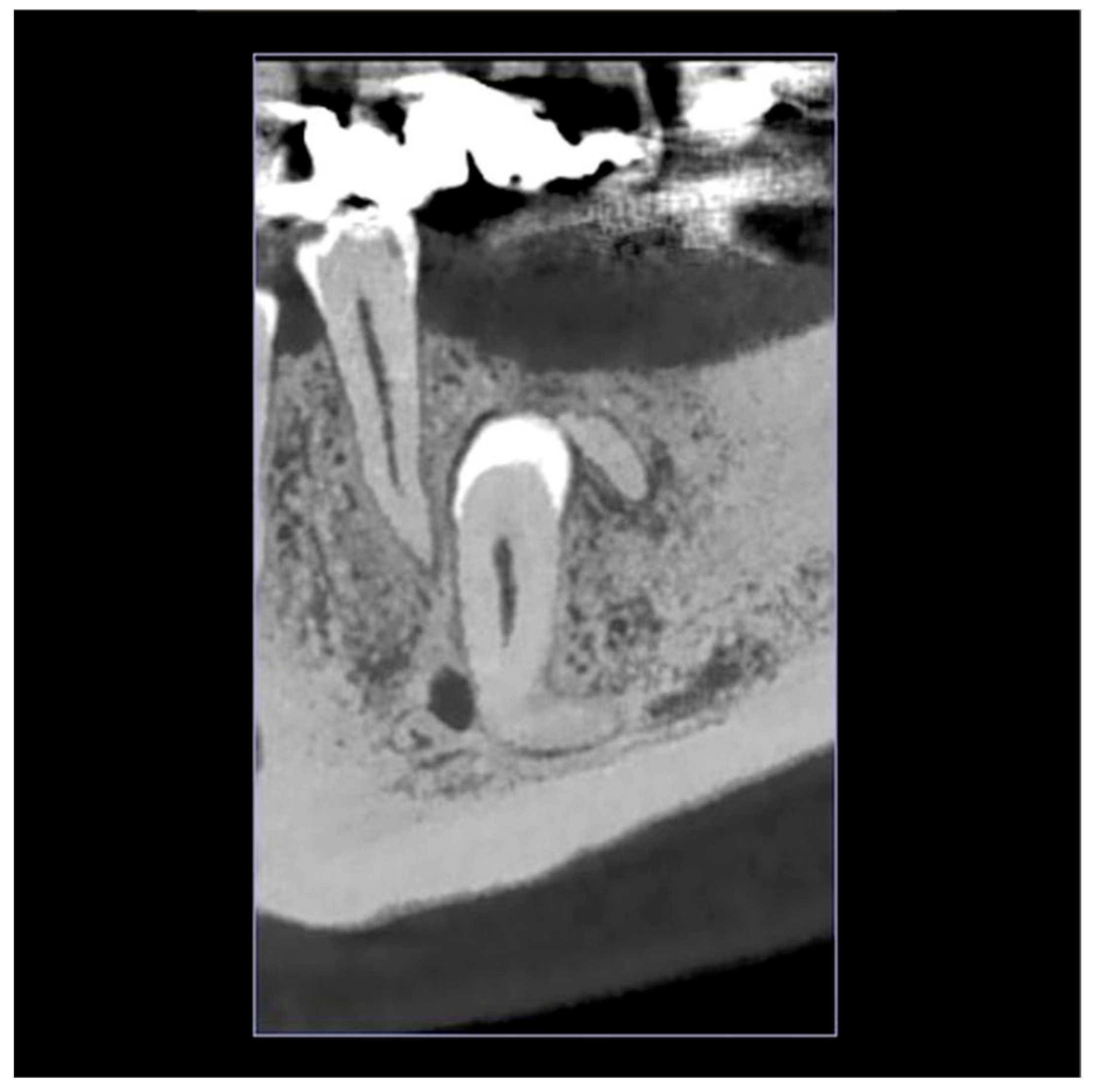
2.1. Initial Visit, Radiographic Evaluation and Diagnosis
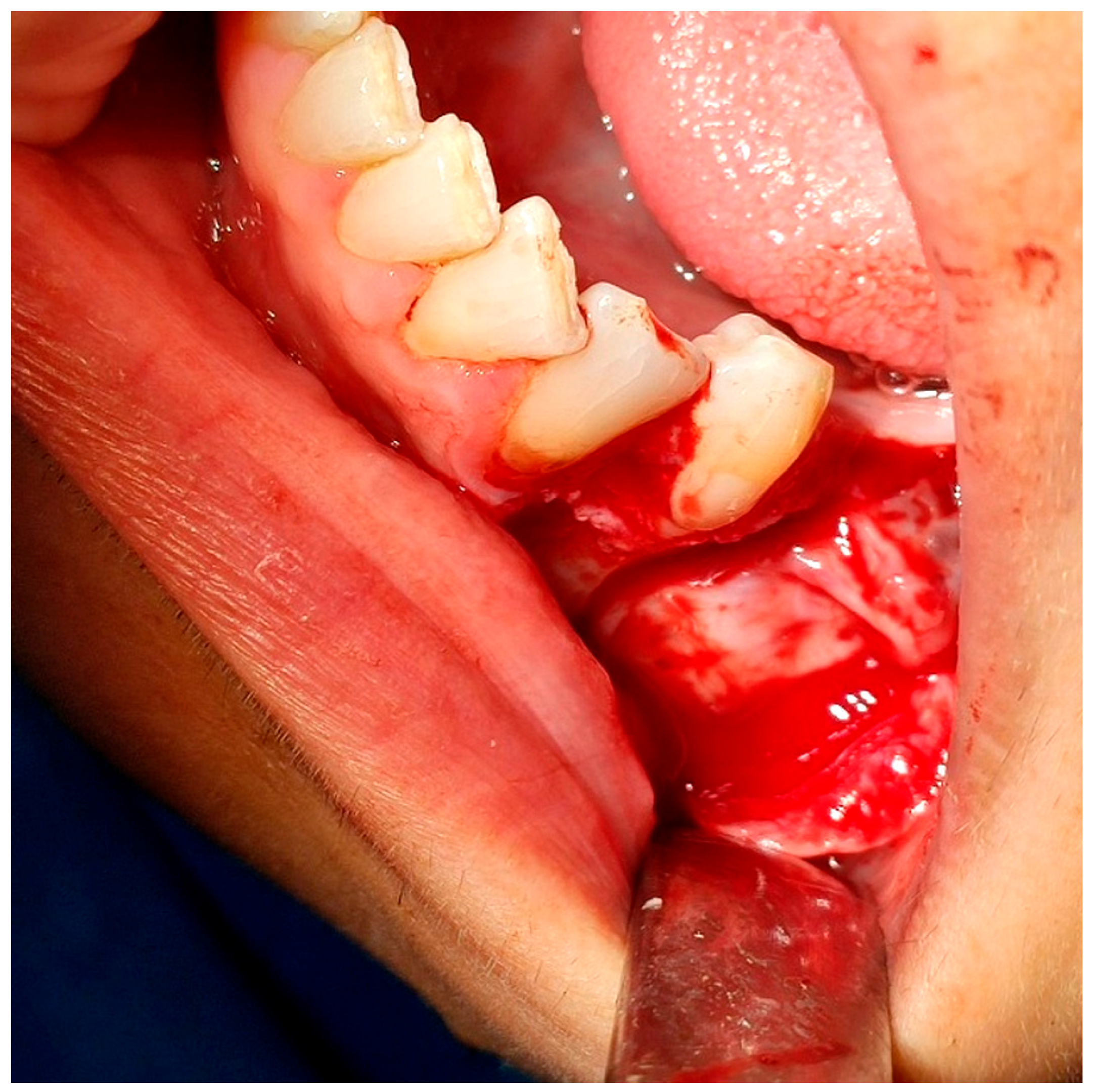
2.2. Surgical Intervention
2.3. Postoperative Management
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OPG | Orthopantomogram |
| CBCT | Cone-Beam Computed Tomography |
| PRF | Platelet-Rich Fibrin |
| PRP | Platelet-Rich Plasma |
References
- Rathee, M.; Jain, P. Embryology, Teeth. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Huang, X.-F.; Chai, Y. Molecular regulatory mechanism of tooth root development. Int. J. Oral Sci. 2012, 4, 177–181. [Google Scholar] [CrossRef]
- Roulias, P.; Kalantzis, N.; Doukaki, D.; Pachiou, A.; Karamesinis, K.; Damanakis, G.; Gizani, S.; Tsolakis, A.I. Teeth Eruption Disorders: A Critical Review. Children 2022, 9, 771. [Google Scholar] [CrossRef]
- Chen, H.M.; Hwang, M.J.; Chiang, C.P. Risk factors and treatments for impacted permanent second molars. J. Dent. Sci. 2024, 19, 1174–1181. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Korkmaz, V.-C.; Chhatwani, S.; Danesh, G. General correlation between neonatal factors, primary and permanent tooth eruption and their interrelation in a population in German orthodontic practices. BMC Oral Health 2023, 23, 437. [Google Scholar] [CrossRef] [PubMed]
- Siotou, K.; Kouskouki, M.-P.; Christopoulou, I.; Tsolakis, A.I.; Tsolakis, I.A. Frequency and Local Etiological Factors of Impaction of Permanent Teeth among 1400 Patients in a Greek Population. Dent. J. 2022, 10, 150. [Google Scholar] [CrossRef] [PubMed]
- Alalola, B.S.; Almasoud, F.S.; Alghamdi, K.B.; Almalki, L.M.; Alodan, Y.A.; Alotaibi, S.N.; Alali, S.R. Comparing the prevalence of impacted teeth through radiographic evidence among orthodontic and general populations: A secondary data analysis. Saudi Dent. J. 2023, 35, 1053–1057. [Google Scholar] [CrossRef]
- Kaczor-Urbanowicz, K.; Zadurska, M.; Czochrowska, E. Impacted Teeth: An Interdisciplinary Perspective. Adv. Clin. Exp. Med. 2016, 25, 575–585. [Google Scholar] [CrossRef]
- Shekhar, M.G.; Pavankumar, P.S.; Chowdary, V.J.; Shivappa, A.B. Bucco-lingual Impaction of Mandibular Second Premolar: Case Report and Review of Literature. Eur. J. Dent. Oral Heal. 2020, 1. [Google Scholar] [CrossRef]
- Janosy, A.M.; Moca, A.E.; Juncar, R.I. Early Diagnosis and Treatment of Mandibular Second Premolar Impaction: A Case Report. Diagnostics 2024, 14, 1610. [Google Scholar] [CrossRef]
- Chu, F.C.; Li, T.K.; Lui, V.K.; Newsome, P.R.; Chow, R.L.; Cheung, L.K. Prevalence of impacted teeth and associated pathologies—A radiographic study of the Hong Kong Chinese population. Hong Kong Med. J. Xianggang Yi Xue Za Zhi 2003, 9, 158–163. [Google Scholar]
- Vandana, S.; Muthu, M.S.; Kandaswamy, D.; Narayanan, M.A. Proposal for a grading system to determine the clinical status and sequence of permanent teeth eruption: A pilot study. J. Oral Biol. Craniofacial Res. 2024, 14, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Santosh, P. Impacted Mandibular Third Molars: Review of Literature and a Proposal of a Combined Clinical and Radiological Classification. Ann. Med. Health Sci. Res. 2015, 5, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Mahdey, H.M.; Wei, M.; Muzaffar, D.; Ramachandra, S.S.; Jameel, R.A.; Tanwir, F.; Hashmi, S. Transient Paresthesia after Surgical Removal of Embedded Supernumerary Tooth. Periodontics Prosthodont. 2016, 2, 1–4. [Google Scholar] [CrossRef]
- Kasapoğlu, Ç.; Brkić, A.; Gürkan-Köseoğlu, B.; Koçak-Berberoğlu, H. Complications Following Surgery of Impacted Teeth and Their Management. In A Textbook of Advanced Oral and Maxillofacial Surgery; InTech: London, UK, 2013. [Google Scholar] [CrossRef]
- Goswami, P.; Chaudhary, V.; Arya, A.; Verma, R.; Vijayakumar, G.; Bhavani, M. Platelet-Rich Fibrin (PRF) and its Application in Dentistry: A Literature Review. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. 1), S5–S7. [Google Scholar] [CrossRef]
- Hajibagheri, P.; Basirat, M.; Tabari-Khomeiran, Z.; Asadi-Aria, A. The efficacy of platelet-rich fibrin (PRF) in post-extraction hard and soft tissue healing and associated complications: A systematic review and meta-analysis of split-mouth randomized clinical trials. BMC Oral Health 2025, 25, 869. [Google Scholar] [CrossRef]
- Ye, L.; He, Y.; Ma, W.; Zhou, F.; Liu, J. Effect of platelet-rich fibrin on the recovery after third molar surgery: A systematic review and meta-analysis. J. Cranio-Maxillofac. Surg. 2024, 52, 1095–1108. [Google Scholar] [CrossRef]
- Yin, Y.; Shuai, F.; Liu, X.; Zhao, Y.; Han, X.; Zhao, H. Biomaterials and therapeutic strategies designed for tooth extraction socket healing. Biomaterials 2025, 316, 122975. [Google Scholar] [CrossRef]
- Dohan Ehrenfest, D.M.; Pinto, N.R.; Pereda, A.; Jiménez, P.; Del Corso, M.; Kang, B.-S.; Nally, M.; Lanata, N.; Wang, H.-L.; Quirynen, M. The impact of the centrifuge characteristics and centrifugation protocols on the cells, growth factors, and fibrin architecture of a leukocyte- and platelet-rich fibrin (L-PRF) clot and membrane. Platelets 2018, 29, 171–184. [Google Scholar] [CrossRef]
- Al-Abdallah, M.; AlHadidi, A.; Hammad, M.; Dar-Odeh, N. What factors affect the severity of permanent tooth impaction? BMC Oral Health 2018, 18, 184. [Google Scholar] [CrossRef]
- Aziz, S.R.; Pulse, C.; Dourmas, M.A.; Roser, S.M. Inferior alveolar nerve paresthesia associated with a mandibular dentigerous cyst. J. Oral Maxillofac. Surg. 2002, 60, 457–459. [Google Scholar] [CrossRef]
- McNamara, C.; McNamara, T.G. Mandibular Premolar Impaction: 2 Case Reports. J. Can. Dent. Assoc. 2005, 71, 859–863. [Google Scholar]
- Abu-Hussein, M.; Watted, N.; Emodi, O.; Awadi, O. Management of Lower Second Premolar Impaction. J. Dent. Coll. Azamgarh. 2015, 1, 1–9. [Google Scholar]
- Bokelund, M.; Andreasen, J.O.; Christensen, S.S.A.; Kjær, I. Autotransplantation of maxillary second premolars to mandibular recipient sites where the primary second molars were impacted, predisposes for complications. Acta Odontol. Scand. 2013, 71, 1464–1468. [Google Scholar] [CrossRef]
- Choi, J.F.; Park, D.Y.; Williams, S.L.; Chang, P. Oral Surgery, Extraction of Unerupted Teeth. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Davidopoulou, S. Surgical Exposure of Impacted Mandibular Second Premolar. Int. J. Clin. Stud. Med. Case Rep. 2021, 14. [Google Scholar] [CrossRef]
- Nimčenko, T.; Omerca, G.; Varinauskas, V.; Bramanti, E.; Signorino, F.; Cicciù, M. Tooth auto-transplantation as an alternative treatment option: A literature review. Dent. Res. J. 2013, 10, 1–6. [Google Scholar]
- Saccomanno, S.; Valeri, C.; Di Giandomenico, D.; Fani, E.; Marzo, G.; Quinzi, V. What is the impact of autotransplantation on the longterm stability and patient satisfaction of impacted canines? A Systematic Review. Saudi Dent. J. 2024, 36, 1268–1277. [Google Scholar] [CrossRef]
- Ye, Z.-X.; Qian, W.-H.; Wu, Y.-B.; Yang, C. Pathologies associated with the mandibular third molar impaction. Sci. Prog. 2021, 104, 368504211013247. [Google Scholar] [CrossRef]
- Gojayeva, G.; Tekin, G.; Kose, N.S.; Dereci, O.; Kosar, Y.C.; Caliskan, G. Evaluation of complications and quality of life of patient after surgical extraction of mandibular impacted third molar teeth. BMC Oral Health 2024, 24, 131. [Google Scholar] [CrossRef]
- Yadav, R.; Verma, U.; Dixit, M.; Gupta, A. Platelet-rich Fibrin: A Paradigm in Periodontal Therapy—A Systematic Review. J. Int. Soc. Prev. Community Dent. 2017, 7, 227–233. [Google Scholar] [CrossRef]
- Egierska, D.; Perszke, M.; Mazur, M.; Duś-Ilnicka, I. Platelet-rich plasma and platelet-rich fibrin in oral surgery: A narrative review. Dent. Med. Probl. 2023, 60, 177–186. [Google Scholar] [CrossRef]
- Al-Maawi, S.; Becker, K.; Schwarz, F.; Sader, R.; Ghanaati, S. Efficacy of platelet-rich fibrin in promoting the healing of extraction sockets: A systematic review. Int. J. Implant Dent. 2021, 7, 1–27. [Google Scholar] [CrossRef]
- Ucer, C.; Khan, R.S. Extraction Socket Augmentation with Autologous Platelet-Rich Fibrin (PRF): The Rationale for Socket Augmentation. Dent. J. 2023, 11, 196. [Google Scholar] [CrossRef]
- Logvynenko, I.; Bursova, V. Inferior alveolar nerve injury after sagittal split osteotomy of the mandible: A literature review. Chin. J. Plast. Reconstr. Surg. 2024, 6, 219–227. [Google Scholar] [CrossRef]
- Tabrizi, R.; Pourdanesh, F.; Jafari, S.; Behnia, P. Can platelet-rich fibrin accelerate neurosensory recovery following sagittal split osteotomy? A double-blind, split-mouth, randomized clinical trial. Int. J. Oral Maxillofac. Surg. 2018, 47, 1011–1014. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Bornstein, M.M.; Lambrichts, I.; Yu, H.Y.; Politis, C.; Jacobs, R. Platelet-rich plasma for regeneration of neural feedback pathways around dental implants: A concise review and outlook on future possibilities. Int. J. Oral Sci. 2017, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Franchini, M.; Cruciani, M.; Mengoli, C.; Masiello, F.; Marano, G.; D‘Aloja, E.; Dell’Aringa, C.; Pati, I.; Veropalumbo, E.; Pupella, S.; et al. The use of platelet-rich plasma in oral surgery: A systematic review and meta-analysis. Blood Transfus. 2019, 17, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Chaushu, S. Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 509–514. [Google Scholar] [CrossRef]
- AlAli, A.M.; AlAnzi, T.H. Inferior alveolar nerve damage secondary to orthodontic treatment: A systematic scoping review. Int. J. Risk Saf. Med. 2021, 32, 175–191. [Google Scholar] [CrossRef]
- Rajanikanth, K.; Bhola, N.; Shukla, D. Concurrent Impaction of the Mandibular Primary Second Molar and Second Premolar in Close Approximation to the Mental Nerve: A Case Report. Cureus 2024, 16, e57934. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blouchou, A.; Peitsinis, P.R.; Makrygiannis, I.H.; Venetis, G.; Tilaveridis, I. Surgical Management of an Impacted Mandibular Second Premolar in Close Proximity to the Mental Foramen: A Case Report. Reports 2025, 8, 177. https://doi.org/10.3390/reports8030177
Blouchou A, Peitsinis PR, Makrygiannis IH, Venetis G, Tilaveridis I. Surgical Management of an Impacted Mandibular Second Premolar in Close Proximity to the Mental Foramen: A Case Report. Reports. 2025; 8(3):177. https://doi.org/10.3390/reports8030177
Chicago/Turabian StyleBlouchou, Aikaterini, Panagiotis Rafail Peitsinis, Ioannis H. Makrygiannis, Gregory Venetis, and Ioannis Tilaveridis. 2025. "Surgical Management of an Impacted Mandibular Second Premolar in Close Proximity to the Mental Foramen: A Case Report" Reports 8, no. 3: 177. https://doi.org/10.3390/reports8030177
APA StyleBlouchou, A., Peitsinis, P. R., Makrygiannis, I. H., Venetis, G., & Tilaveridis, I. (2025). Surgical Management of an Impacted Mandibular Second Premolar in Close Proximity to the Mental Foramen: A Case Report. Reports, 8(3), 177. https://doi.org/10.3390/reports8030177





