Osteonevus of Nanta—A Rare Case Report of a Cellular Blue Nevus with Ossification
Abstract
1. Introduction and Clinical Significance
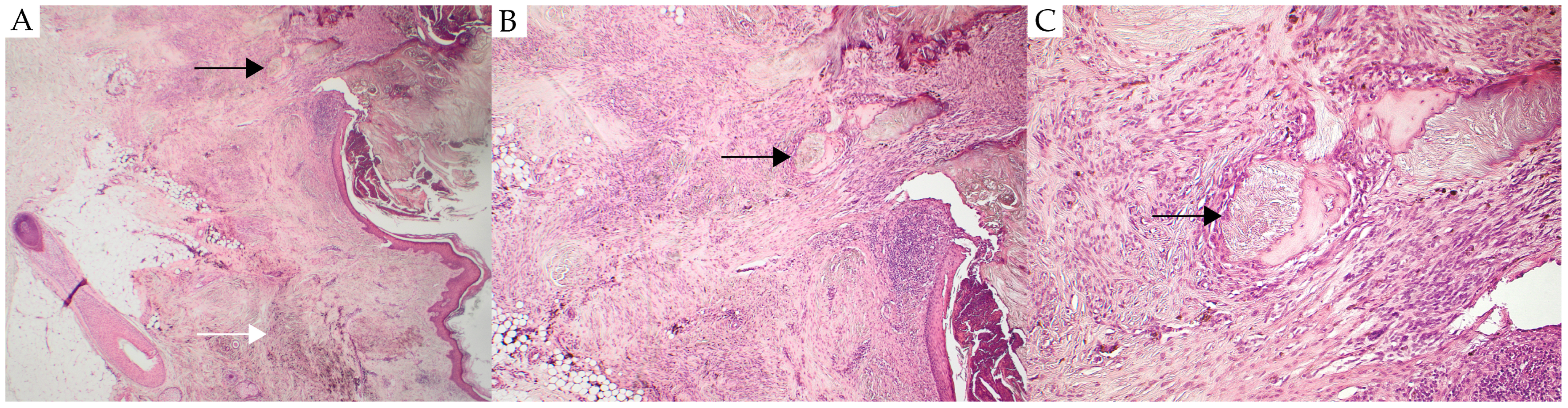
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- López-Robles, J.; Pérez-Plaza, A.; Luis Requena, C.S. Osteoma Cutis Arising in Common Blue Nevus (Blue Osteonevus): A Clinicopathologic, Immunohistochemical, and Dermoscopic Study. Am. J. Dermatopathol. 2019, 41, e19–e21. [Google Scholar] [CrossRef] [PubMed]
- Bezić, J.; Karaman, I.; Tomaš, S.Z.; Živković, P.M.; Božić, J. Osteonevus of Nanta Revisited: Clinicopathological Features of 33 Cases. Am. J. Dermatopathol 2016, 38, 859–861. [Google Scholar] [CrossRef] [PubMed]
- Breunig, J.A.; Breunig, A.A.; Lovatto, L.; Duquia, R.P.; Almeida, H.L., Jr. Dermoscopy of an osteonevus of Nanta. Int. J. Dermatol. 2014, 53, e212. [Google Scholar] [CrossRef] [PubMed]
- Moulin, G.; Souquet, D.; Balme, B. Pigmented nevus and cutaneous ossifications. Apropos of 125 cases of osteonevi. Ann. Dermatol. Venereol. 1991, 118, 199–204. [Google Scholar] [PubMed]
- Baran, L.; Civatte, J. Un osteonaevus de Nanta aux caracteres inusites. Bull. Soc. Fr. Dermatol. Syphiligr. 1959, 67, 611–615. [Google Scholar]
- Collina, G.; Annessi, G.; Gregorio, C.D. Cellular blue naevus associated with osteoma cutis. Histopathology 1991, 19, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Culver, W.; Burgdorf, W.H. Malignant melanoma arising in a nevus of Nanta. J. Cutan. Pathol. 1993, 20, 375–377. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, S.; Mitsuhashi, Y.; Ito, Y. Osteo-nevus of Nanta: A case report and review of the Japanese literature. J. Dermatol. 1999, 26, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Conlin, P.A.; Jimenez-Quintero, L.P.; Rapini, R.P. Osteomas of the skin revisited: A clinicopathologic review of 74 cases. Am. J. Dermatopathol. 2002, 24, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, J.; Ciolfi, C.; Sartor, E.; Caroppo, F.; Salmaso, R.; Del Forno, B.; Fortina, A.B. Osteonevus of Nanta in a 3-year-old child with dermatoscopic characterization. JAAD Case Rep. 2023, 38, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Zembowicz, A.; Phadke, P.A. Blue nevi and variants: An update. Arch. Pathol. Lab. Med. 2011, 135, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Cesare, A.D.; Sera, F.; Gulia, A.; Coletti, G.; Micantonio, T.; Fargnoli, M.C.; Peris, K. The spectrum of dermatoscopic patterns in blue nevi. J. Am. Acad. Dermatol. 2012, 67, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Gronbeck, C.; Kerr, P.E. Nodular melanoma. Clin. Dermatol. 2025, 43, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Reiter, O.; Mimouni, I.; Dusza, S.; Halpern, A.C.; Leshem, Y.A.; Marghoob, A.A. Dermoscopic features of basal cell carcinoma and its subtypes: A systematic review. J. Am. Acad. Dermatol. 2021, 85, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Paver, E.C.; Ahmed, T.; Burke, H.; Saw, R.P.M.; Stretch, J.R.; Spillane, A.J.; Shannon, K.F.; Vergara, I.A.; Elder, D.E.; Lo, S.N.; et al. Prognostic Significance of Incipient Ulceration in Primary Cutaneous Melanoma. JAMA Dermatol. 2023, 159, 1359–1367. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kristiansen, C.S.; Norling, A.L.; Bols, B.; Lang, C.L. Osteonevus of Nanta—A Rare Case Report of a Cellular Blue Nevus with Ossification. Reports 2025, 8, 139. https://doi.org/10.3390/reports8030139
Kristiansen CS, Norling AL, Bols B, Lang CL. Osteonevus of Nanta—A Rare Case Report of a Cellular Blue Nevus with Ossification. Reports. 2025; 8(3):139. https://doi.org/10.3390/reports8030139
Chicago/Turabian StyleKristiansen, Camilla Soendergaard, Anna Louise Norling, Birgitte Bols, and Christian Lyngsaa Lang. 2025. "Osteonevus of Nanta—A Rare Case Report of a Cellular Blue Nevus with Ossification" Reports 8, no. 3: 139. https://doi.org/10.3390/reports8030139
APA StyleKristiansen, C. S., Norling, A. L., Bols, B., & Lang, C. L. (2025). Osteonevus of Nanta—A Rare Case Report of a Cellular Blue Nevus with Ossification. Reports, 8(3), 139. https://doi.org/10.3390/reports8030139





