Rapidly Progressive Buccal Hematoma Following Local Anesthetic Injection: A Case Report
Abstract
1. Introduction and Clinical Significance
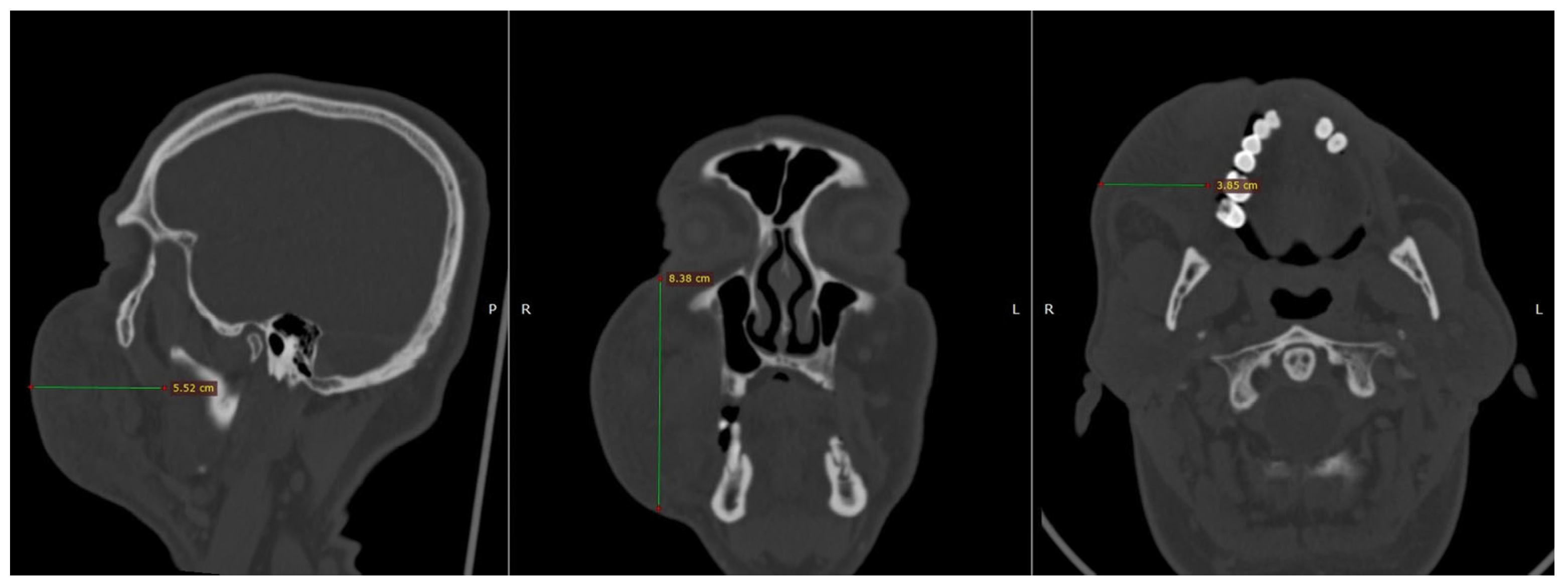
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ICU | Intensive care unit |
References
- Calatayud, J.; González, Á. History of the Development and Evolution of Local Anesthesia since the Coca Leaf. Anesthesiology 2003, 98, 1503–1508. [Google Scholar] [CrossRef] [PubMed]
- Keskin Yalcin, B. Complications Associated with Local Anesthesia in Oral and Maxillofacial Surgery. In Topics in Local Anesthetics; Whizar-Lugo, V.M., Hernández-Cortez, E., Eds.; IntechOpen: London, UK, 2020. [Google Scholar] [CrossRef]
- Säkkinen, J.; Huppunen, M.; Suuronen, R. Complications Following Local Anaesthesia. Nor. Tann. Tid. 2005, 115, 48–52. [Google Scholar] [CrossRef]
- Boon Tat, Y.; Muniandy, R.K.; Ng Mooi Hang, L. Denture Induced Submandibular Hematoma in a Patient on Warfarin. Case Rep. Anesth. 2018, 2018, 4245809. [Google Scholar] [CrossRef]
- Bajkin, B.V.; Todorovic, L.M. Safety of Local Anaesthesia in Dental Patients Taking Oral Anticoagulants: Is It Still Controversial? Br. J. Oral Maxillofac. Surg. 2012, 50, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Matsuzaki, Y.; Kogou, T.; Kato, H.; Ohno, K.; Watanabe, A.; Akashi, Y.; Takano, M. A Rare Case of Organized Hematoma in the Cheek. J. Oral Maxillofac. Surg. Med. Pathol. 2021, 33, 443–447. [Google Scholar] [CrossRef]
- Singh, K. Hematoma—A Complication of Posterior Superior Alveolar Nerve Block. J. Dent. Probl. Solut. 2015, 2, 015–016. [Google Scholar] [CrossRef]
- Barrientos-Lezcano, F.; Corchero-Martín, G.; González-Núñez, A.; Soler-Presas, F. Life-Threatening Sublingual Hematoma after Mandibular Implant Placement—A Case Report. Ann. Maxillofac. Surg. 2021, 11, 169–172. [Google Scholar] [CrossRef]
- Moghadam, H.G.; Caminiti, M.F. Life-Threatening Hemorrhage after Extraction of Third Molars: Case Report and Management Protocol. J. Can. Dent. Assoc. 2002, 68, 670–674. [Google Scholar]
- Kawashima, W.; Hatake, K.; Morimura, Y.; Kudo, R.; Nakanishi, M.; Tamaki, S.; Kasuda, S.; Yuui, K.; Ishitani, A. Asphyxial Death Related to Postextraction Hematoma in an Elderly Man. Forensic Sci. Int. 2013, 228, e47–e49. [Google Scholar] [CrossRef]
- Funayama, M.; Kumagai, T.; Saito, K.; Watanabe, T. Asphyxial Death Caused by Postextraction Hematoma. Am. J. Forensic Med. Pathol. 1994, 15, 87–90. [Google Scholar] [CrossRef]
- Zhu, W.; Gyamfi, J.; Niu, L.; Schoeffel, G.J.; Liu, S.; Santarcangelo, F.; Khan, S.; Tay, K.C.-Y.; Pashley, D.H.; Tay, F.R. Anatomy of Sodium Hypochlorite Accidents Involving Facial Ecchymosis—A Review. J. Dent. 2013, 41, 935–948. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.L.N.; Figueroba, S.R.; Mafra, M.A.T.; Groppo, F.C. Edema and Hematoma after Local Anesthesia via Posterior Superior Alveolar Nerve Block: A Case Report. J. Dent. Anesth. Pain Med. 2022, 22, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Mardinger, O.; Manor, Y.; Mijiritsky, E.; Hirshberg, A. Lingual Perimandibular Vessels Associated with Life-Threatening Bleeding: An Anatomic Study. Int. J. Oral. Maxillofac. Implant. 2007, 22, 127–131. [Google Scholar]
- Benjelloun, L.; Taleb, B. Facial Hematoma of Endodontic Origin: A Case Report. Ann. Med. Surg. 2022, 81, 104484. [Google Scholar] [CrossRef]
- Mehra, P.; Clancy, C.; Wu, J. Formation of a Facial Hematoma during Endodontic Therapy. J. Am. Dent. Assoc. 2000, 131, 67–71. [Google Scholar] [CrossRef]
- Tribovane, D.C.; Tortajada Bustelo, J.C.; Cañellas, Á.R. Sodium Hypochlorite-Induced Facial Hematoma Following Root Canal Treatment. Iran. Endod. J. 2024, 19, 46–49. [Google Scholar] [CrossRef]
- Stanley, F. Malamed Handbook of Local Anesthesia, 7th ed.; Elsevier: St Louis, MO, USA, 2020; ISBN 9780323676861. [Google Scholar]
- Weinstock, R.J.; Clarkson, E. Risk of Airway Embarrassment during Root Canal Therapy. J. Am. Dent. Assoc. 2013, 144, 1144–1147. [Google Scholar] [CrossRef]
- Ho, K.; Hutter, J.J.; Eskridge, J.; Khan, U.; Boorer, C.J.; Hopper, R.A.; Deva, A.K. The Management of Life-Threatening Haemorrhage Following Blunt Facial Trauma. J. Plast. Reconstr. Aesthet. Surg. 2006, 59, 1257–1262. [Google Scholar] [CrossRef]
- Smatt, Y.; Browaeys, H.; Genay, A.; Raoul, G.; Ferri, J. Iatrogenic Pneumomediastinum and Facial Emphysema after Endodontic Treatment. Br. J. Oral Maxillofac. Surg. 2004, 42, 160–162. [Google Scholar] [CrossRef]
- Biočić, J.; Brajdić, D.; Perić, B.; Danić, P.; Salarić, I.; Macan, D. A Large Cheek Hematoma as a Complication of Local Anesthesia: Case Report. Acta Stomatol. Croat. 2018, 52, 156–159. [Google Scholar] [CrossRef]
- Singh, N.R.; Behera, R.; Pattnaik, S. Hematoma Following Nerve Block of a Branch of Maxillary Nerve: A Case Report. Indian J. Forensic Med. Toxicol. 2020, 14, 8490–8492. [Google Scholar] [CrossRef]
- Kraus, C.K.; Katz, K.D. Extensive Facial Hematoma Following Third Molar Removal. Am. J. Emerg. Med. 2014, 32, 1153.e5–1153.e6. [Google Scholar] [CrossRef] [PubMed]
- Hirshi, T.S.; Gupta, S. Posterior Superior Alveolar Nerve Block, a Dilemma for Dental Practitioners—A Case Report. J. Cont. Med. Dent. 2016, 4, 45–48. [Google Scholar]
- Penna, K.J.; Neshat, K. Cervicofacial Subcutaneous Emphysema after Lower Root Canal Therapy. N. Y. State Dent. J. 2001, 67, 28–29. [Google Scholar]
- Engdahl, R.; Nassiri, N.; Mina, B.; Drury, J.; Rosen, R. Superselective Microcatheter Embolization of Hemorrhage after Buccal Lipectomy. Aesthetic Plast. Surg. 2012, 36, 742–745. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Politis, S.; Tatsis, D.; Antoniou, A.; Louizakis, A.; Paraskevopoulos, K. Rapidly Progressive Buccal Hematoma Following Local Anesthetic Injection: A Case Report. Reports 2025, 8, 88. https://doi.org/10.3390/reports8020088
Politis S, Tatsis D, Antoniou A, Louizakis A, Paraskevopoulos K. Rapidly Progressive Buccal Hematoma Following Local Anesthetic Injection: A Case Report. Reports. 2025; 8(2):88. https://doi.org/10.3390/reports8020088
Chicago/Turabian StylePolitis, Solon, Dimitris Tatsis, Asterios Antoniou, Alexandros Louizakis, and Konstantinos Paraskevopoulos. 2025. "Rapidly Progressive Buccal Hematoma Following Local Anesthetic Injection: A Case Report" Reports 8, no. 2: 88. https://doi.org/10.3390/reports8020088
APA StylePolitis, S., Tatsis, D., Antoniou, A., Louizakis, A., & Paraskevopoulos, K. (2025). Rapidly Progressive Buccal Hematoma Following Local Anesthetic Injection: A Case Report. Reports, 8(2), 88. https://doi.org/10.3390/reports8020088






